1. Introduction
Breast cancer is the most common cancer in women [
1], and its diagnosis and treatment represent a significant physical and emotional challenge. Like the disease itself, changes in the physical appearance of the breast after surgery can disrupt psychological well-being, body image, and overall quality of life [
2,
3,
4]. Tumor location within the breast further influences surgical planning, cosmetic outcomes, and patient satisfaction. Breast cancers are most frequently located in the upper outer quadrant (45%), followed by the upper inner quadrant (15%), lower outer quadrant (10%), and lower inner quadrant (5%) [
5]. Breast-conserving surgery (BCS) aims to remove the tumor with clear oncological margins while preserving as much healthy breast tissue as possible, and it has become a widely accepted standard due to its ability to maintain breast esthetics without compromising oncological safety [
6].
Over the years, there has been a continuous search for alternatives to classical incisions in breast-conserving surgery, motivated by the need to optimize both oncological outcomes and cosmetic results. Tan et al. introduced the Boomerang incision in 2007 [
7] and subsequently modified it in 2015 [
8], offering better adaptability for tumors in specific quadrants. Nevertheless, these incisions often had limitations in terms of breast size, tumor location, and closure complexity, and no single incision was available that could be safely applied to all quadrants and breast volumes.
To overcome these challenges, we developed the Sparrow (Modified Lazy-S) incision, which incorporates a curved design with a central skin islet, allowing for precise tumor excision with safe margins while minimizing distortion of the breast contour. This incision is versatile, applicable in all four quadrants, and particularly advantageous for tumors located near the skin, where anterior margin positivity is a concern. Furthermore, the Sparrow incision is straightforward to perform, does not require specialized training, and can be safely applied in small- and medium-volume breasts, making it a practical technique for general surgeons and in settings with limited oncoplastic support [
9,
10,
11,
12].
This study aimed to present our experience with the Sparrow (Modified Lazy-S) incision in breast-conserving surgery, evaluating its oncological safety, cosmetic outcomes, complication rates, and patient satisfaction. Additionally, we aimed to assess whether this technique could provide a simple, versatile, and reproducible alternative to classical incisions for level 1 oncoplastic procedures.
2. Materials and Methods
This study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Istanbul University-Cerrahpasa, Cerrahpasa Medical Faculty Clinical Research Ethics Committee (number of approval: 56390; Date: 22 April 2020). Informed consents were obtained from all patients.
A total of 57 patients who underwent the Sparrow incision were included in the study. Patients who were admitted to the Istanbul University-Cerrahpaşa, Cerrahpaşa Medical Faculty Breast Clinic with a diagnosis of invasive carcinoma and decided to have breast-conserving surgery, who are candidates for resection of less than 20% percent of the breast tissue (level 1 oncoplastic surgery) at the multidisciplinary breast council, were screened between January 2017 and January 2020.
The patient’s age, tumor localization, tumor size, complications, and comorbidity data were retrospectively analyzed from the surgical, epicrisis, and pathology reports. In all cases, intraoperative pathological evaluation of the surgical margins was performed routinely. To evaluate the new incision, the BREAST-Q™ Breast Cancer Core Scale and the BCT Module Version 2.0 Psychosocial Well-Being and Satisfaction with Breasts modules were administered [
13].
The Sparrow (Modified Lazy-S) incision was applied consecutively to all eligible patients who met the inclusion criteria during the study period. No patients were selectively excluded based on breast volume or degree of ptosis, as the technique was designed to be suitable for both small-volume and ptotic breasts.
2.1. Inclusion and Exclusion Criteria
The women who had multifocal tumors that were more than 4 cm away or had multicentric tumors, women for whom radiotherapy is contraindicated, centrally localized tumors in which the nipple areola complex is invaded, and women for whom breast conserving therapy is contraindicated are excluded from the study. Women who are candidates for level 1 oncoplastic surgery (less than 20% of breast tissue is removed) are included in the study.
2.2. Surgical Technique
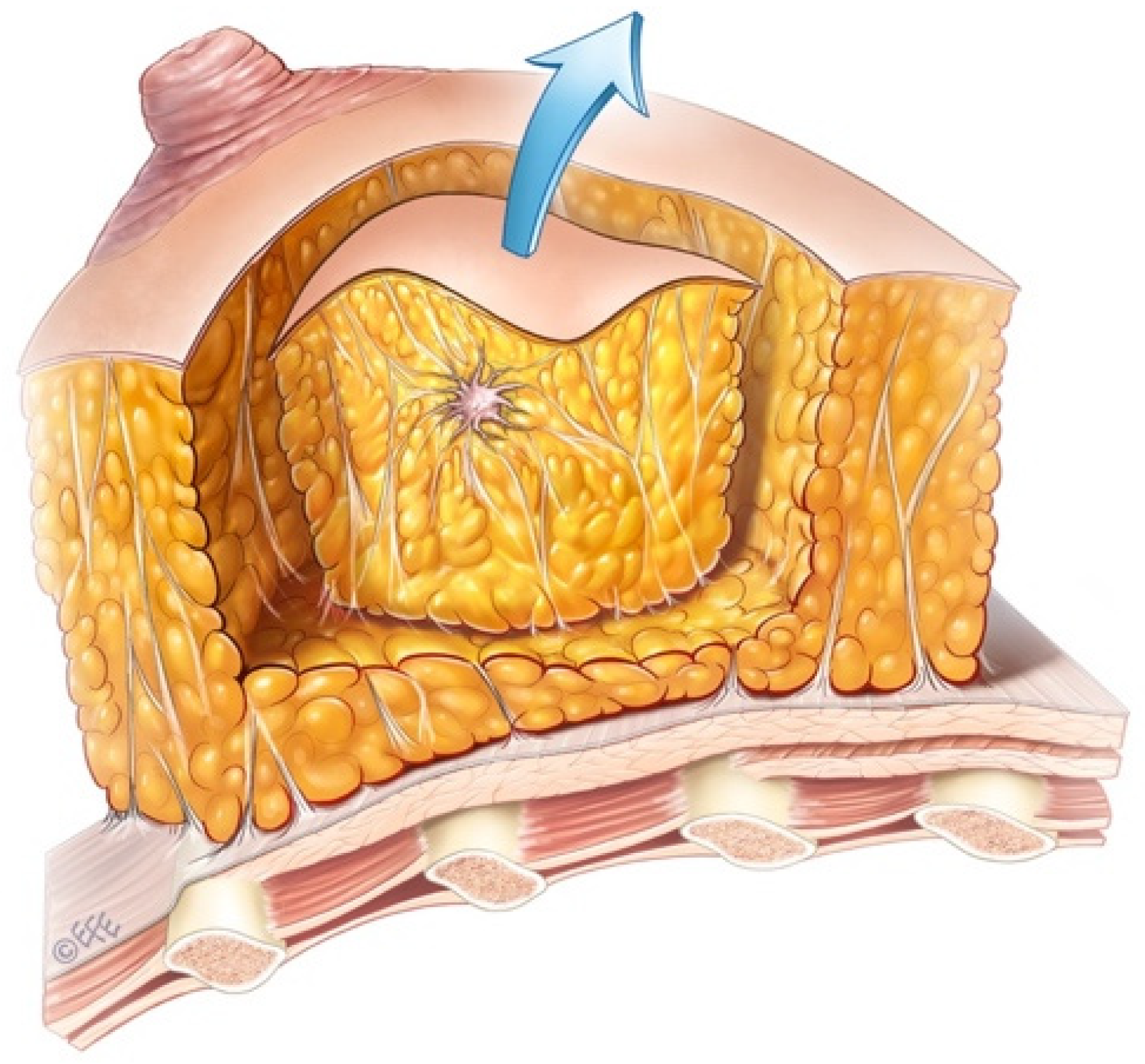
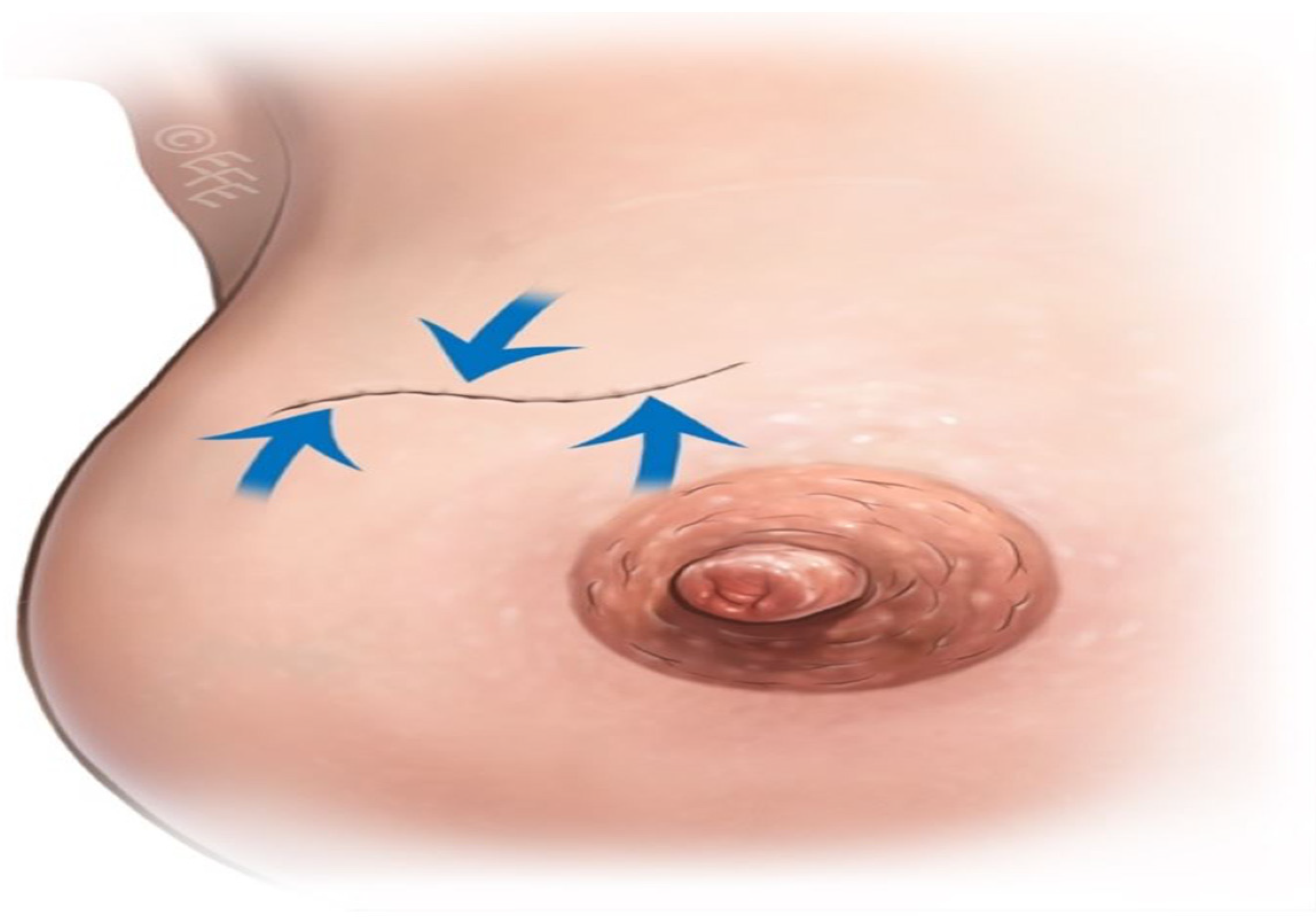
Sparrow (Modified Lazy-S) incision is a versatile technique that can be applied to tumors in any quadrant during breast-conserving surgery. It provides a safe surgical margin, and a central skin islet is excised only when the tumor is close to the skin, resulting in minimal asymmetry and distortion. After tumor excision, the remaining tissue defect is typically closed by approximating the tissues over the pectoralis major fascia and beneath the skin. While other incisions vary according to the quadrant (radial or circular), the Sparrow (Modified Lazy-S) incision serves as an alternative to classical approaches, suitable for different quadrants, breast sizes, and tumor dimensions. Unlike the standard Lazy-S incision, both ends of the Sparrow incision are more curved, and a skin islet is preserved in the center of the excised tissue. It can be safely used horizontally or vertically in all four quadrants. Additionally, when indicated, the incision may include a large anterior skin islet, particularly for large or superficial tumors, which reduces the risk of anterior margin positivity. This approach achieves the goal of providing the most benefit with the least intervention (
Figure 1). This novel technique (Sparrow), developed by our team, has not been previously reported in the literature.
The incision is closed following its natural curvature rather than in a straight line, which distributes tension across multiple vectors. Compared with standard linear incision or simple elliptical excision, it provides better mobilization and control of breast tissue, reduces distortion, and maintains oncological safety. This design is well tolerated during adjuvant radiotherapy and does not interfere with treatment planning. The Sparrow incision also provides adequate exposure of the glandular breast tissue, facilitating safe tumor excision and enabling placement of drains if required, ensuring proper postoperative drainage of the operative site.
Patient-Reported Outcomes
The Breast-Q™ questionnaires were administered once postoperatively, after completion of all adjuvant treatments, including radiotherapy, to assess the patients’ final cosmetic and psychosocial outcomes [
13]. We acknowledge that including a comparison group undergoing lumpectomy through a standard incision would have strengthened the study; however, as this was a retrospective, single-arm analysis, no such control group was available.
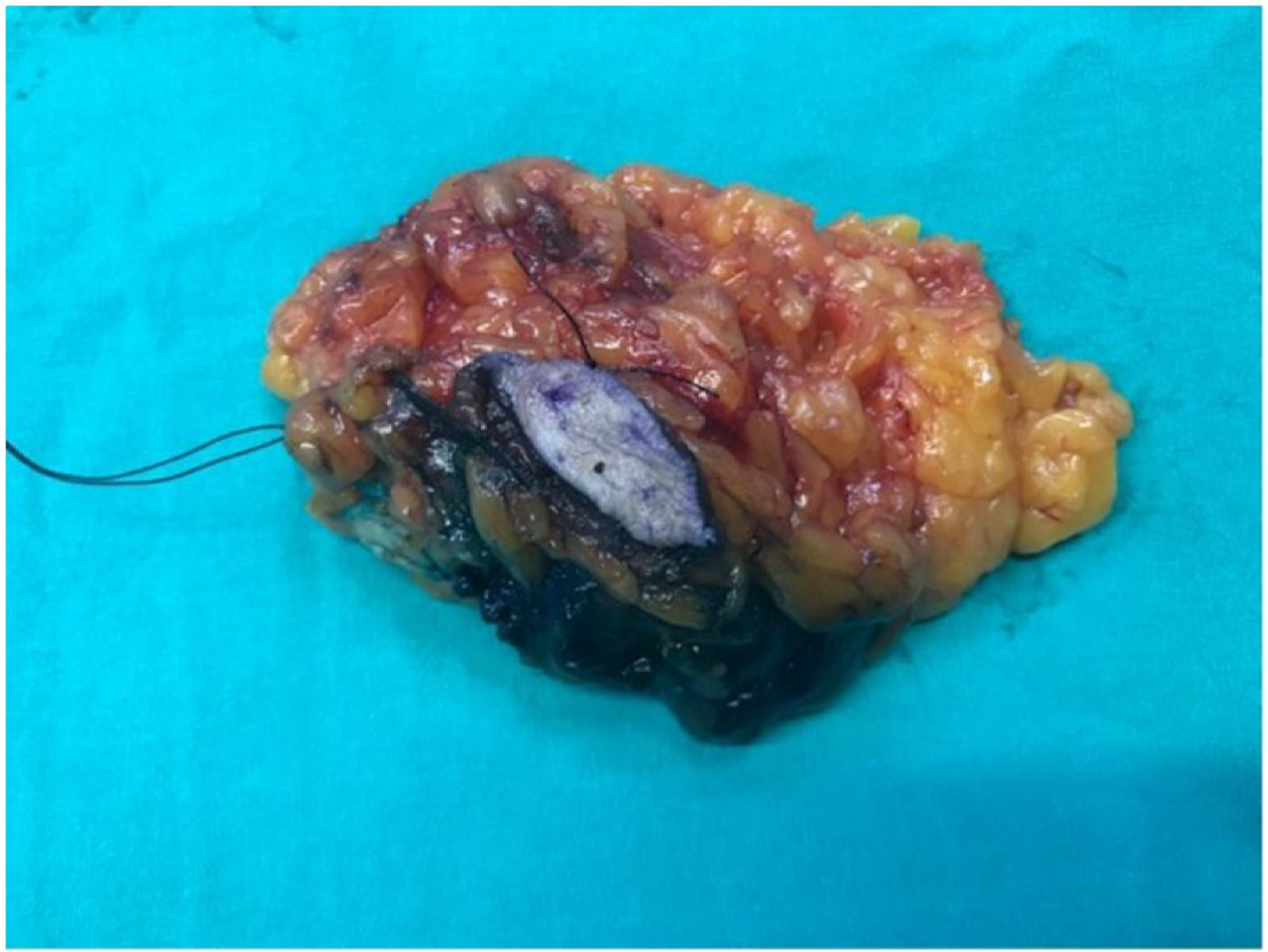
With the long axis of the tumor forming the main body of the sparrow, Sparrow incision can be applied in all quadrants in all directions, 360 degrees. When a skin islet excision is required, its direction and length are determined according to the tumor’s extension and longitudinal diameter. It is a technique that can be used in breast-conserving surgery. It is named “Sparrow” (
Figure 2a) because it resembles a sparrow in appearance (
Figure 2b).
2.3. Statistical Analysis
SPSS 21 was used to conduct statistical analyses. Qualitative data were given as numbers (n) and percentages (%), while quantitative data were presented as mean ± SD.
3. Results
Between January 2017 and January 2020, 57 patients who underwent breast-conserving surgery using the Sparrow (Modified Lazy-S) incision were retrospectively analyzed. The mean follow-up was 25 ± 10.06 months (range, 6–42 months). The mean age of the patients was 55.74 ± 12.18 years (range, 25–80 years). Tumors were in the right breast at 43.9% (n = 25) and in the left breast in 56.1% (n = 32). Regarding tumor quadrant, 50.9% (n = 29) were in the upper outer quadrant, 19.3% (n = 11) in the upper inner quadrant, 14.0% (n = 8) in the lower outer quadrant, and 15.8% (n = 9) in the lower inner quadrant (
Figure 3 and
Figure 4). The mean surgical margin was 0.43 ± 0.25 cm (range 0.1–0.9 cm) in the remaining 32 patients. For clarity, the previously stated 0.3 cm referred specifically to a single patient with the closest anterior margin. The overall anterior margin in the cohort ranged from 0.1 to 0.9 cm.
All patients received standard surgical management, including sentinel lymph node sampling, with axillary dissection performed when clinically indicated. The majority of patients had drains placed postoperatively, and the overall complication rate was low. Only two patients required reoperation due to concerns regarding surgical margins, highlighting the oncological safety of the Sparrow incision.
Comorbidities and demographic characteristics varied among patients, yet the technique was successfully applied across different breast volumes and tumor locations, including patients with ptotic or small breasts. Neoadjuvant therapy was administered selectively to patients with larger tumors to facilitate optimal breast conservation.
Overall, the Sparrow (Modified Lazy-S) incision was associated with low complication rates, effective tumor excision, and broad applicability in diverse patient populations. A detailed summary of patient demographics, tumor characteristics, comorbidities, and postoperative complications is presented in
Table 1.
4. Discussion
With the advances in imaging, screening programs, and patient awareness, early and rapid diagnosis and treatment of breast cancer can be achieved [
14], increasing the feasibility of breast-conserving surgery. The Sparrow (Modified Lazy-S) incision, developed from the classical Lazy-S design, provides an oncologically safe approach, particularly for tumors located near the skin. When indicated, inclusion of a selective anterior skin islet allows for safe margin control while improving esthetic outcomes by reducing wound tension and distortion (
Figure 5 and
Figure 6).
In small breasts or cases with large tumors, extensive glandular flaps or level I reconstruction may cause displacement of the tumor bed and increase the distance between the skin incision and the original tumor site, creating challenges for adjuvant radiotherapy [
15,
16]. This can complicate radiotherapy planning, increase the required boost dose, and inadvertently irradiate healthy tissue, potentially affecting cosmetic outcomes [
15,
17,
18]. The Sparrow (Modified Lazy-S) incision, closed along its natural curvature, distributes tension across multiple vectors, allowing for better mobilization and control of breast tissue, reducing distortion, and maintaining oncological safety. Because the incision preserves the tumor’s original location, it facilitates adjuvant treatment and radiotherapy planning. The Sparrow incision may offer potential advantages, as it does not require specialized instruments, prostheses, or additional operative time [
19,
20]. While a formal economic analysis was not performed in this retrospective study, future prospective studies could objectively assess its financial advantages compared with standard incisions.
The inclusion of a skin islet is performed selectively based on the tumor’s proximity to the skin. In smaller-breasted women, especially when the tumor is near the skin, this approach can be safely applied, minimizing esthetic deformity while maintaining oncological safety. The Sparrow incision was used in small breasts, large tumors, and tumors close to the anterior margin, with skin islets excised according to the tumor’s size and location. For larger tumors, excision included the posterior fascia. In our series, the largest anterior skin islet measured approximately 4 × 3 cm, and cosmetic outcomes remained acceptable due to the incision’s design, which distributes tension vectors and minimizes breast contour distortion.
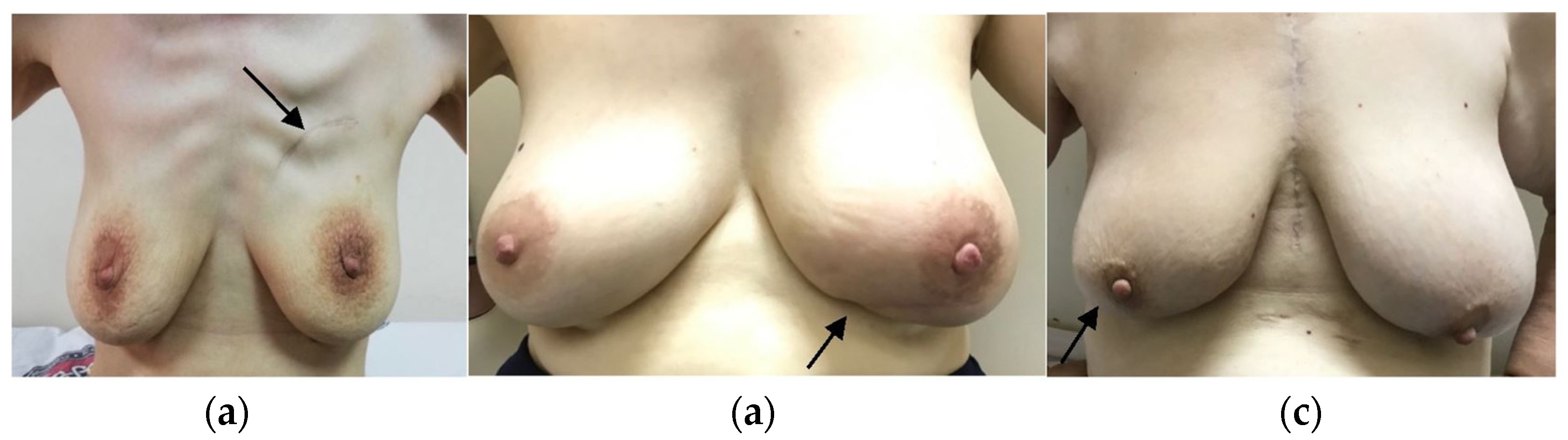
Breast cancers most commonly occur in the upper outer quadrant (45%), followed by the upper inner (15%), lower outer (10%), and lower inner quadrants (5%) [
5]. In our study, tumors were located in the upper outer quadrant in 50.9% (n = 29), upper inner in 19.3% (n = 11), lower outer in 14% (n = 8), and lower inner in 15.8% (n = 9), consistent with the literature. The Sparrow incision can be applied to all quadrants (
Figure 7a–c).
In a meta-analysis by Xiaopeng Cai et al., complications in breast-conserving surgery were reported at 10.97% [
21], while Serrurier et al. observed a rate of 9.8% [
14]. In our series, the complication rate was 5.3%, consistent with the literature.
The Sparrow incision adheres to oncological principles and is a potential advantage, as it does not prolong operative time or require additional instruments, including prostheses. It allows for excision of the previous biopsy site and can be safely applied in patients receiving neoadjuvant therapy or with multifocal tumors. Patient-reported outcomes, assessed using the Breast-Q™ questionnaire once postoperatively after completion of all adjuvant treatments, including radiotherapy [
13], demonstrated high satisfaction: psychosocial well-being was 90.33%, preoperative breast satisfaction was 86.47%, and postoperative breast satisfaction was 90.14%. These results reflect positive outcomes in psychosocial well-being, breast shape, symmetry, and contour.
The Limitations of This Study
This study has several limitations, including its retrospective design, relatively small sample size, a lack of a comparator group (e.g., standard lumpectomy incision), limited oncological follow-up, and the inclusion of some patients with ptotic breasts, which may affect cosmetic outcomes and the generalizability of the results. Additionally, due to patient privacy and consent constraints, a complete set of preoperative, intraoperative, and postoperative photographs for each patient could not be included. However, representative images are provided (
Figure 1,
Figure 5,
Figure 6 and
Figure 7) to illustrate the surgical technique and outcomes. Future prospective studies should aim to obtain comprehensive photographic documentation with appropriate consent for all patients.
5. Conclusions
The Sparrow incision, a modification of the Lazy-S technique, provides oncologically safe margins and can be applied safely in both horizontal and vertical orientations across all four breast quadrants. It may offer potential advantages while also reducing operative time, hospital stay, and complications, and not requiring specialized training. Patient-reported outcomes using the Breast-Q™ modules demonstrate high levels of satisfaction. Our findings suggest that the Sparrow incision is a safe, effective, and versatile alternative to level 1 oncoplastic reconstruction in breast-conserving surgery.
Author Contributions
B.P. and M.V.: Contributed to the conception, writing, and proofreading of the manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
Institutional Review Board Statement
This study was approved by the Istanbul University-Cerrahpasa, Cerrahpasa Medical Faculty Clinical Research Ethics Committee (number of approval: 56390; Date: 22 April 2020). Informed consents were obtained from all patients.
Informed Consent Statement
Informed consent was obtained from all participants included in the study.
Data Availability Statement
The datasets generated and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Acknowledgments
We all thank Levent Efe, CMI, Medical Illustration Studios (Brunswick), for his valuable medical and surgical illustrations.
Conflicts of Interest
The author declares no conflicts of interest.
References
- Stewart, W.B.; Wild, C.P. Cancer worldwide. In The Global and Regional Burden of Cancer; World Cancer Report; World Health Organization: Lyon, France, 2014; p. 16. [Google Scholar]
- Kouwenberg, C.A.E.M.; de Ligt, K.M.; Kranenburg, L.W.; Rakhorst, H.M.; de Leeuw, D.M.; Siesling, S.; Busschbach, J.J.; Mureau, M.A.M.M. Long-Term Health-Related Quality of Life after Four Common Surgical Treatment Options for Breast Cancer and the Effect of Complications: A Retrospective Patient-Reported Survey among 1871 Patients. Plast. Reconstr. Surg. 2020, 146, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Mureau, M.A.M.; Breast Reconstruction Guideline Working Group. Dutch breast reconstruction guideline. J. Plast Reconstr. Aesthet. Surg. 2018, 71, 290–304. [Google Scholar] [CrossRef] [PubMed]
- Noguchi, M.; Yokoi-Noguchi, M.; Ohno, Y.; Morioka, E.; Nakano, Y.; Kosaka, T.; Kurita, T. Oncoplastic breast conserving surgery: Volume replacement vs. volume displacement. Eur. J. Surg. Oncol. 2016, 42, 926–934. [Google Scholar] [CrossRef] [PubMed]
- Jatoi, I.; Kaufmann, M.; Petit, J.Y. Atlas of Breast Surgery; Springer: Berlin/Heidelberg, Germany, 2006; p. 16. [Google Scholar]
- Veronesi, U.; Salvadori, B.; Luini, A.; Greco, M.; Saccozzi, R.; del Vecchio, M.; Mariani, L.; Zurrida, S.; Rilke, F. Breast conservation is a safe method in patients with small cancer of breast. Long-term results of three randomised trials on 1973 patients. Eur. J. Cancer 1995, 31, 1574–1579. [Google Scholar] [CrossRef] [PubMed]
- Tan, M.P. The boomerang incision for periareolar breast malignancies. Am. J. Surg. 2007, 194, 690–693. [Google Scholar] [CrossRef] [PubMed]
- Tan, M.P.; Sitoh, N.Y.; Sitoh, Y.Y. Perspectives of Cosmesis following Breast Conservation for Multifocal and Multicentric Breast Cancers. Int. J. Breast Cancer 2015, 2015, 126793. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.K.; Kim, Y.S. The Lazy S Design: A Novel Skin Closure Design in Skin-Sparing Mastectomy for Implant-Based Breast Reconstruction. Arch. Plast. Surg. 2017, 44, 344–347. [Google Scholar] [CrossRef] [PubMed]
- Proano, E.; Perbeck, L.G. Influence of the site of skin incision on the circulation in the nipple-areola complex after subcutaneous mastectomy in breast cancer. Scand. J. Plast. Reconstr. Surg. Hand Surg. 1996, 30, 195–200. [Google Scholar] [CrossRef] [PubMed]
- Perbeck, L.; Proano, E.; Westerberg, L. The circulation in the nipple-areola complex following subcutaneous mastectomy in breast cancer. Scand. J. Plast. Reconstr. Surg. Hand Surg. 1992, 26, 217–221. [Google Scholar] [CrossRef] [PubMed]
- Glaumann, B. Investigation of 72 patients following subcutaneous mastectomy. A clinical evaluation of current surgical techniques. Scand. J. Plast. Reconstr. Surg. 1985, 19, 273–281. [Google Scholar] [CrossRef] [PubMed]
- Pusic, A.; Klassen, A.; Cano, S. BREAST-Q Version 2.0© Breast Conserving Therapy Module Pre- and Postoperative Scales; Memorial Sloan Kettering Cancer Center and The University of British Columbia: Vancouver, BC, Canada, 2017; pp. 3, 7, 9. [Google Scholar]
- Serrurier, L.C.J.; Rayne, S.; Venter, M.; Benn, C.A. Direct-to-Implant Breast Reconstruction without the Use of an Acellular Dermal Matrix Is Cost Effective and Oncologically Safe. Plast. Reconstr. Surg. 2017, 139, 809–817. [Google Scholar] [CrossRef] [PubMed]
- Tse, T.; Knowles, S.; Bélec, J.; Caudrelier, J.; Lock, M.; Brackstone, M.; Arnaout, A. Consensus statement on tumour bed localization for radiation after oncoplastic breast surgery. Curr. Oncol. 2020, 27, e326–e331. [Google Scholar] [CrossRef] [PubMed]
- Arnaout, A.; Ross, D.; Khayat, E.; Richardson, J.; Kapala, M.; Hanrahan, R.; Zhang, J.; Doherty, C.; Brackstone, M. Position statement on defining and standardizing an oncoplastic approach to breast-conserving surgery in Canada. Curr. Oncol. 2019, 26, e405–e409. [Google Scholar] [CrossRef] [PubMed]
- Lee, G.; Parmar, H.; Li, W.; Shessel, A. The Effect of Lumpectomy Cavity Changes on Planning Dose in Breast Radiotherapy Boost. J. Med. Imaging Radiat. Sci. 2019, 50, 317–322. [Google Scholar] [CrossRef] [PubMed]
- Pezner, R.D.; Tan, M.C.; Clancy, S.L.; Chen, Y.J.; Joseph, T.; Vora, N.L. Radiation therapy for breast cancer patients who undergo oncoplastic surgery: Localization of the tumor bed for the local boost. Am. J. Clin. Oncol. 2013, 36, 535–539. [Google Scholar] [CrossRef] [PubMed]
- Chatterjee, A.; Asban, A.; Jonczyk, M.; Chen, L.; Czerniecki, B.; Fisher, C.S. A cost-utility analysis comparing large volume displacement oncoplastic surgery to mastectomy with free flap reconstruction in the treatment of breast cancer. Am. J. Surg. 2019, 218, 597–604. [Google Scholar] [CrossRef] [PubMed]
- Jablonka, E.M.; Lamelas, A.M.; Kanchwala, S.K.; Rhemtulla, I.; Smith, M.L. A Simplified Cost-Utility Analysis of Inpatient Flap Monitoring after Microsurgical Breast Reconstruction and Implications for Hospital Length of Stay. Plast. Reconstr. Surg. 2019, 144, 540e–549e. [Google Scholar] [CrossRef] [PubMed]
- Cai, X.; Liu, X.; Yu, H.; Li, J.; Zheng, X. Breast-conserving therapy for early-stage breast cancer in Chinese women: A meta-analysis of case-control studies. Onkologie 2012, 35, 133–139. [Google Scholar] [CrossRef] [PubMed]
| Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).