1. Introduction
Trabeculectomy is considered the gold standard for drainage surgery in glaucoma. It is an effective procedure for lowering intraocular pressure (IOP) and reducing the need for post-operative medication. However, due to its invasive nature, trabeculectomy surgery carries a risk of sight-threatening post-operative complications. These complications prolong recovery and may even require surgical revision. Surgeons also require a high level of skill and expertise to perform trabeculectomy surgery [
1,
2,
3,
4,
5].
There has been a shift towards less invasive surgical procedures, such as the PreserFlo MicroShunt (PF) (Santen, Osaka, Japan). This device aims to avoid the need to create a scleral flap, sclerostomy, and pre-placed nylon sutures, as well as to reduce post-operative complications and follow-up review requirements. The reduced intra-operative trauma results in less post-operative inflammation and potentially better preservation of tissues for future surgery [
1,
2,
3,
4,
5].
This study aimed to compare the effectiveness and safety of PF to trabeculectomy in the management of glaucoma.
2. Materials and Methods
This is a retrospective cohort analysis of consecutive patients undergoing glaucoma drainage surgery at a single-center private ophthalmology practice by a single surgeon (G.A.L.) in Brisbane, Australia. Surgeries were conducted between November 2017 and October 2022 for trabeculectomy patients and between May 2022 and January 2024 for PF patients. Written consent for surgery was obtained from all patients with institutional ethical approval (Royal Australian and New Zealand College of Ophthalmology 195.25). The inclusion criteria involved patients aged ≥18 years with mild to advanced glaucoma, which was uncontrolled on maximally tolerated medication.
Data was retrospectively collected pre-operatively as well as post-operatively on day 1, week 1, and at 3, 6, and 12 months. Information on the patient’s age, sex, ethnicity, type of glaucoma, and past ocular history was recorded. Primary outcome measures included IOP and the number of IOP-lowering medications. Secondary outcome measures included best-corrected visual acuity (BCVA), visual field mean deviation (MD), retinal nerve fiber layer thickness, and intraluminal stent removal (for PF patients). The severity of glaucoma was based on the Hodapp–Parrish–Anderson classification of MD with mild ≥ −6 dB, moderate between −6–−12 dB and severe ≤ −12 dB. Data was also collected on any post-operative complications, including the need for revision surgery.
The criteria for complete success were an IOP between 6 mmHg and 15 mmHg, with a ≥20% reduction in IOP from baseline, no requirement for post-operative IOP-lowering medication, and no subsequent procedures, revisions, or additional glaucoma surgeries. Qualified success was defined as an IOP between 6 mmHg and 15 mmHg, with a ≥20% reduction in IOP from baseline, regardless of the use of adjunct medication (but not including acetazolamide), and no further glaucoma procedures or surgeries. Any additional glaucoma surgery, except for needling with 5-fluoruracil, during the follow-up period was defined as a failure.
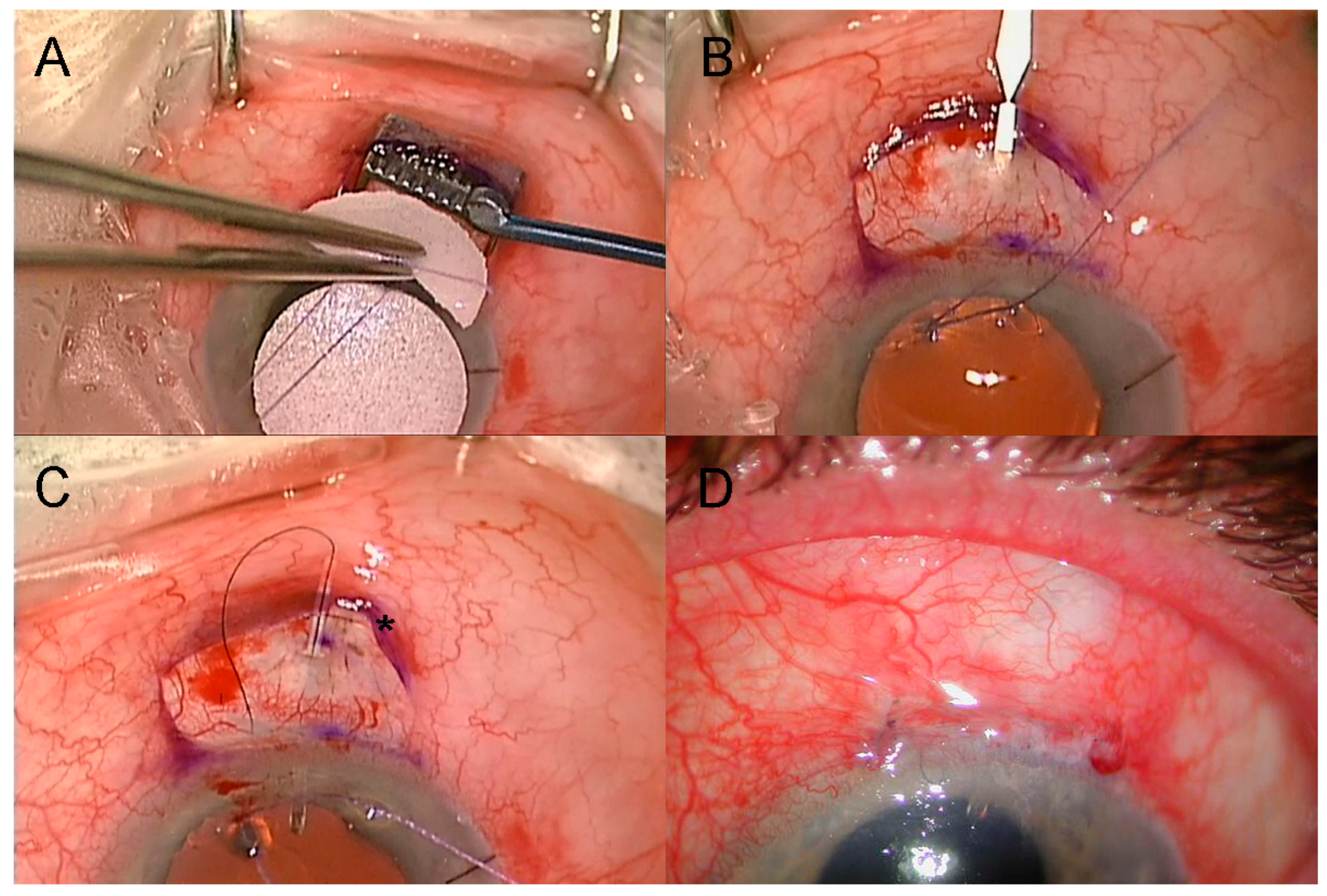
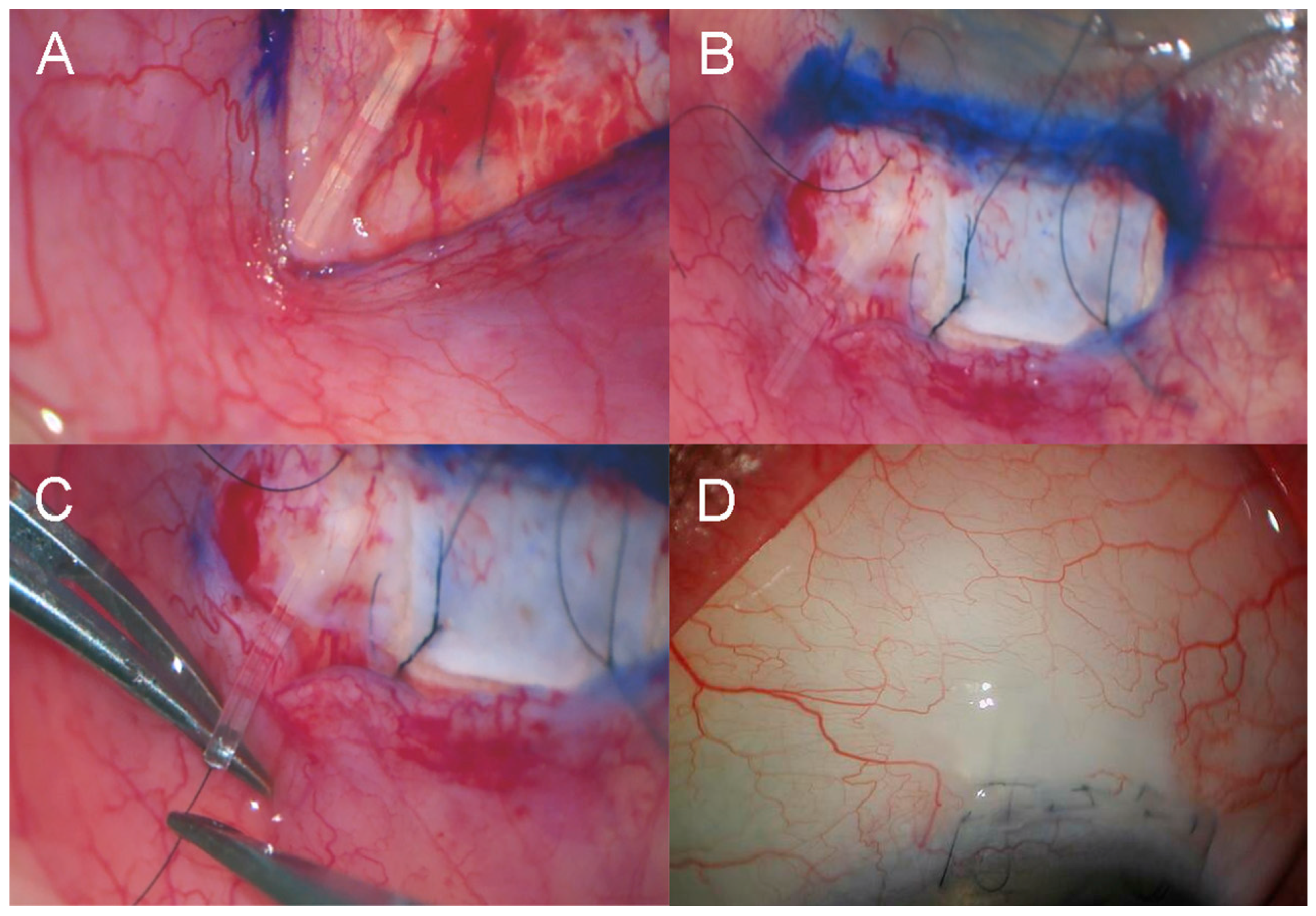
For the PF surgery, the procedure was performed with a fornix-based conjunctival flap, followed by the application of Mitomycin C (MMC) at 0.01–0.04% for 2–3 min (
Figure 1A), depending on the state of the conjunctiva and Tenon’s capsule as determined by the surgeon (G.A.L.). The device was placed ab externo with the formation of the sclerostomy using a two-step knife (Mani, Tochigi, Japan), commencing 4 mm behind the scleral limbus (
Figure 1B). A buried releasable 10/0 nylon intraluminal stent was placed after the first eight eyes that had PF insertion (
Figure 1C). The conjunctiva was closed with four buried 9/0 polyglactin 910 (Vicryl, Ethicon, Inc., Raritan, NJ, USA) buried horizontal mattress sutures (
Figure 1D). Subconjunctival dexamethasone and cefazolin were injected.
For the trabeculectomy surgery, a fornix-based conjunctival flap was created, followed by a scleral flap (4 mm × 3 mm × 300 microns thick), and then the application of MMC at 0.01–0.04% for 2–3 min, depending on the state of the conjunctiva and Tenon’s capsule as determined by the surgeon (G.A.L.). A peripheral iridectomy was performed in all phakic patients and in pseudophakic patients if the iris base was occluding the sclerostomy. The flap was closed with two or three triple-throw buried releasable 10/0 nylon sutures, and the conjunctiva was closed with a combination of two purse-string and 3–4 10/0 nylon buried horizontal mattress sutures. A Seidel test was performed to confirm no leaks. Subconjunctival dexamethasone and cefazolin were injected.
Post-operatively, patients were commenced on topical prednisolone acetate 1% and antibiotic eye drops six times per day. The topical antibiotic was ceased after 1–2 weeks, and the topical steroids were gradually tapered over 4–6 months. IOP-lowering medication was not administered unless indicated.
Statistical analyses were conducted using Stata version 18 (StataCorp LLC, College Station, TX, USA). Differences in means between groups were analyzed with an independent t-test. Between-group differences in proportions and differences in categorical distributions between treatment groups were analyzed using Fisher’s exact test or the Chi-squared test. To account for the inherent correlation between repeated measurements within individual eyes and the inclusion of both eyes from the same patient, multilevel mixed-effects linear or Poisson regression models were employed, controlling for age, pre-operative IOP, number of glaucoma medications, and MD. Inverse probability of treatment weighting (IPTW) was applied using propensity scores estimated from the same covariates included in the regression models to mitigate potential selection bias between groups. The hazards of failure to achieve success criteria and of ceasing steroid use were analyzed using IPTW-Cox proportional hazard modelling, controlling for age, pre-operative IOP, the number of glaucoma medications, and MD. p < 0.05 indicated statistical significance.
3. Results
A total of 95 eyes (48 PF and 47 trabeculectomy) in 83 patients (44 PF and 39 trabeculectomy) were included in the study. The groups had comparable characteristics with a few exceptions (
Table 1). The PF group was older, with a mean ± standard deviation age of 72.9 ± 9.6 years compared to 65.3 ± 13.8 years in the trabeculectomy group (
p = 0.002). The MD was worse in the PF group at −11.1 ± 7.8 dB compared to −7.3 ± 6.6 dB in the trabeculectomy group (
p = 0.014). The initial eight PF procedures were performed without the placement of an intra-operative intraluminal 10/0 nylon stent. In the subsequent 40 cases, stents were placed, with 31 (77.5%) of these removed within three months post-operatively. The PF group received slightly higher doses of MMC, with 29 (60.4%) receiving a concentration of 0.03% for 3 min, compared to 20 (42.6%) in the trabeculectomy group (
p = 0.131).
Outcome analysis was conducted using the IPWA results to balance out differences between the groups without reducing the sample size. Standardized mean differences were close to zero, with a range of weighted standard differences between −0.04 and 0.01, indicating excellent covariate balance, and variance ratios were within the acceptable range of between 0.6 and 1.4.
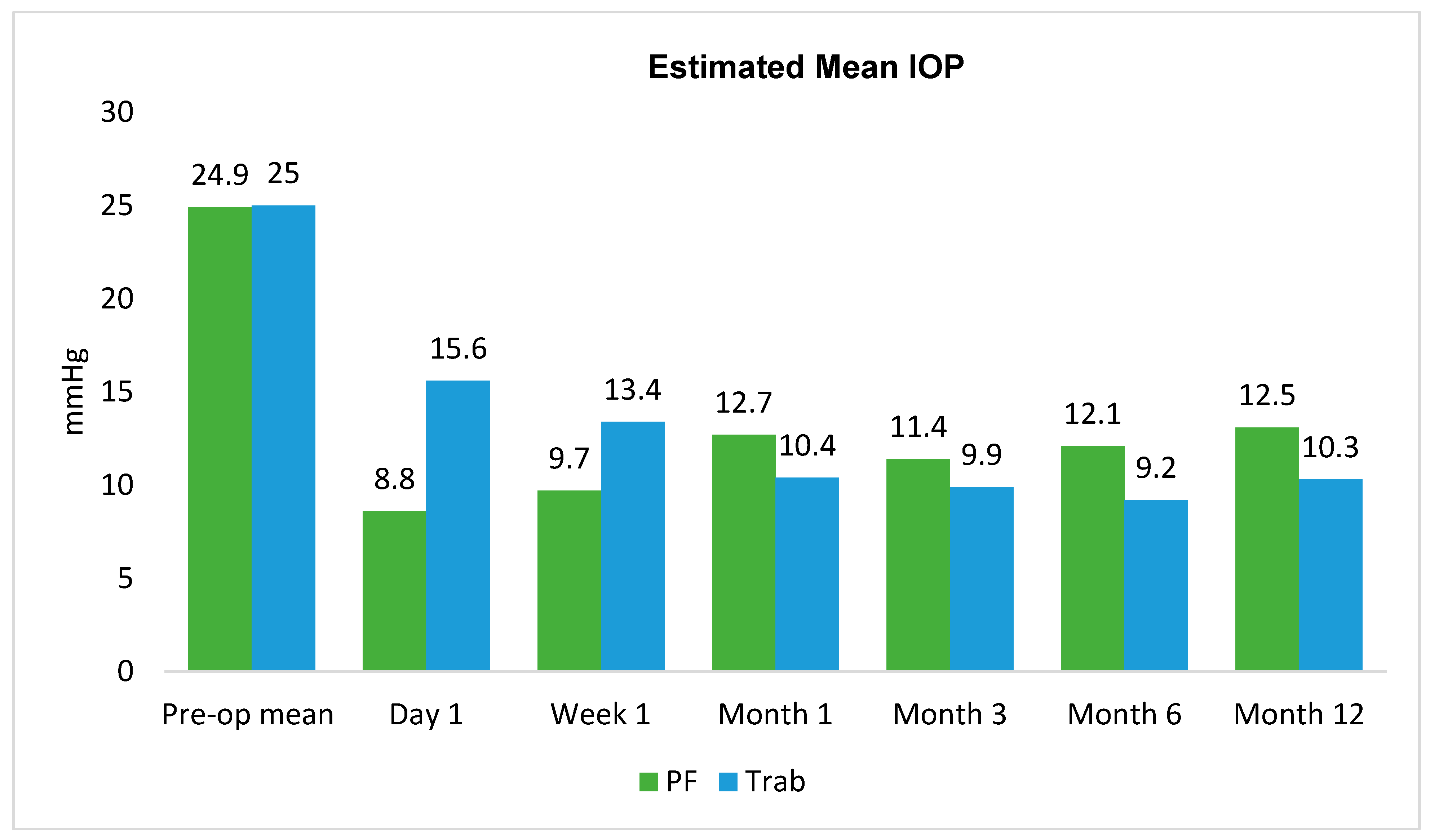
The mean IPWA-adjusted pre-operative IOP was 24.9 mmHg in the PF group and 25.0 mmHg in the trabeculectomy group (
Table 2,
Figure 2). The difference in mean IOP reduction from baseline was statistically significantly greater in the PF group at day 1 and week 1, with no significant differences between groups at subsequent time points. At Month 12, the mean IOP was 13.1 mmHg in the PF group, resulting in an IOP reduction of −11.8 mmHg from baseline. In the trabeculectomy group, the mean IOP was 10.3 mmHg, with a reduction of −14.7 mmHg. The between-group difference in IOP reduction was 2.9 mmHg (95%CI: −2.0, 7.9;
p = 0.246).
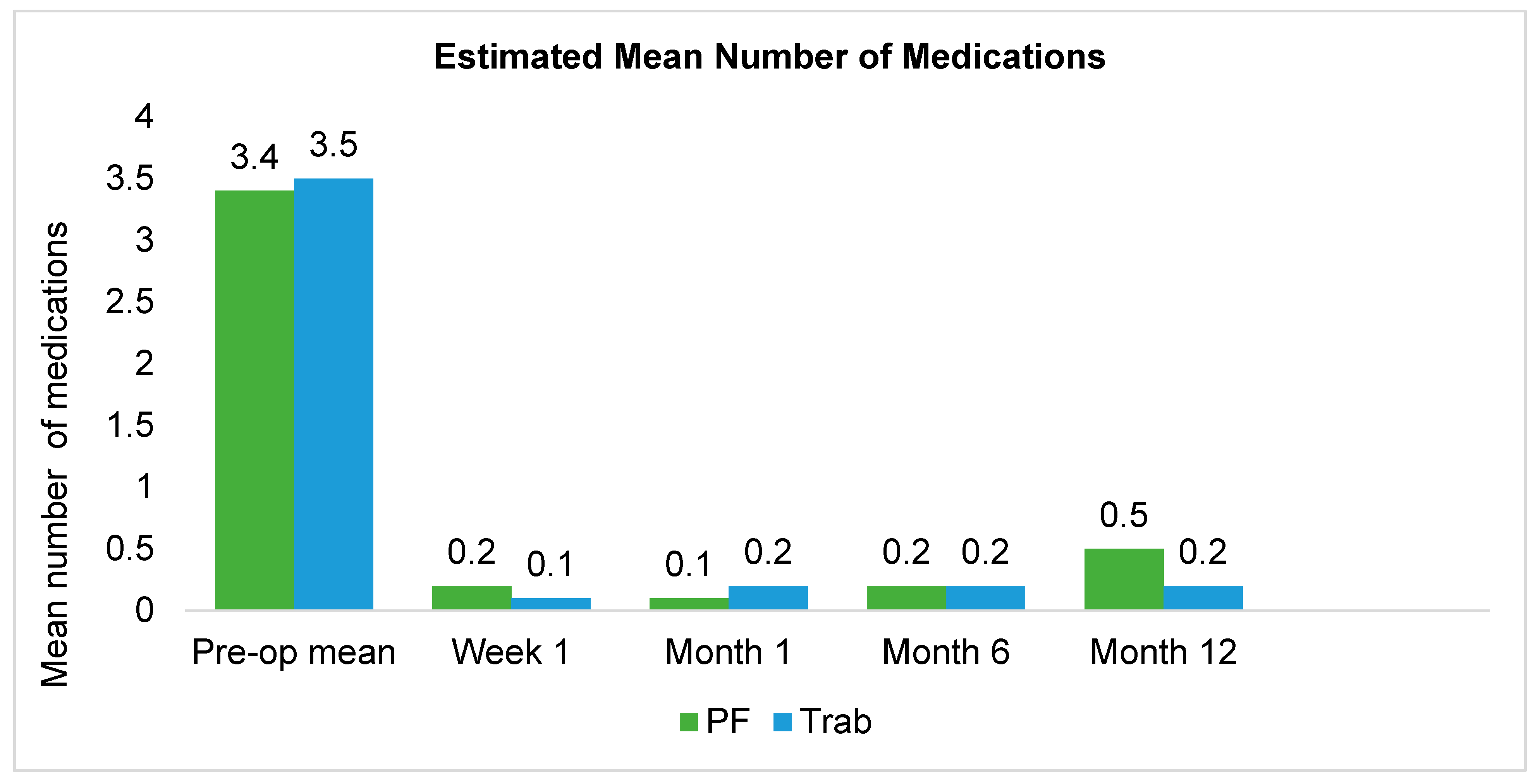
Over the 12-month study period, on average, the PF group exhibited a reduction of 2.9 medications, whilst the trabeculectomy group had a reduction of 3.3 medications, resulting in a between-group difference in medication reduction of 0.4 (95%CI: −0.13, 0.96;
p = 0.138). At 12 months, the mean number of post-operative medications for the PF group was 0.5 and 0.2 medications in the trabeculectomy group (
Figure 3,
Table 3).
The IPWA-adjusted mean BCVA in the PF and trabeculectomy eyes pre-operatively were both 0.76, and by 12 months post-operatively, the PF eyes had the same mean BCVA at 0.76, whereas the trabeculectomy group was 0.73 (between-group differences: 0.03; 95%CI: −0.1, 0.2; p = 0.710).
Six of the eight (75.0%) non-stented PF eyes developed early (≤1 month) post-operative numerical hypotony. This prompted the subsequent 40 eyes to have intra-operative placement of a 10/0 nylon intraluminal stent, with no further episodes of hypotony. Among the non-stented eyes, one eye (12.5%) experienced clinically significant hypotony requiring re-stenting at one month. Further complications are detailed in
Table 4. In the trabeculectomy eyes (
n = 47), early post-operative complications included numerical hypotony in six eyes (12.8%), macroscopic hyphema in one eye (2.1%), peripheral iris incarceration in one eye (2.1%), and bleb leak in two eyes (4.7%).
Bleb needling with 5% 5-fluorouracil was required in both treatment groups, with 16 (33.3%) PF eyes and 13 (27.7%) trabeculectomy eyes. Needling was performed at a mean of 2.6 months post-operatively in the PF eyes and 1.9 months post-operatively in trabeculectomy eyes, suggesting a requirement for earlier post-operative bleb management in the trabeculectomy group (
Table 4).
The cessation of topical steroids (based on clinical observation of bleb appearance, such as vascularity, extent, and height) in PF was 6.3 times (95%CI: 2.8, 14.5; p < 0.001) more likely than in trabeculectomy, indicating faster resolution of post-operative inflammation following PF surgery. The estimated cumulative probability of continued steroid use at Months 6 and 12 was 48.3% and 10.5% in the PF group, compared with 89.2% and 70.1% in the trabeculectomy group, respectively.
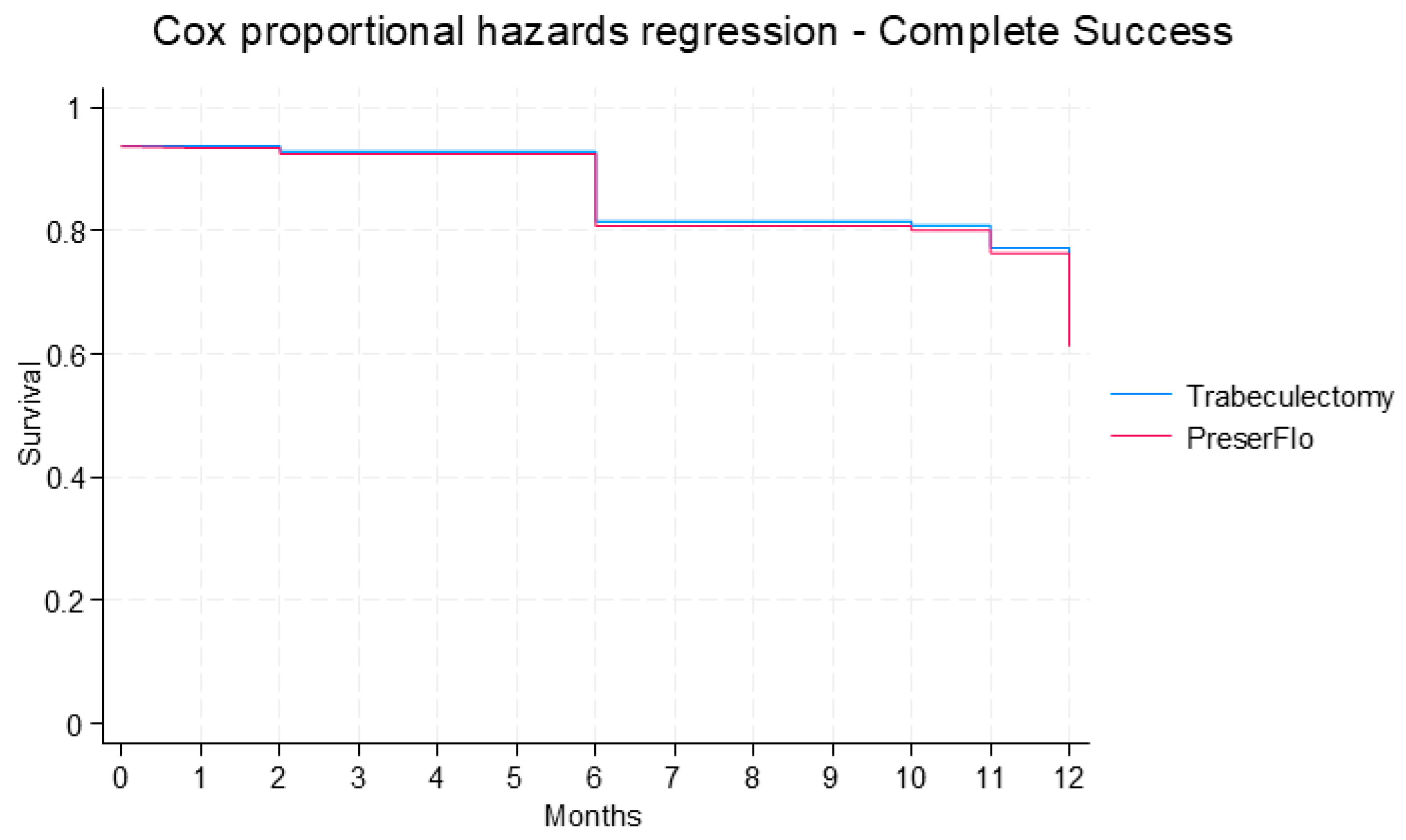
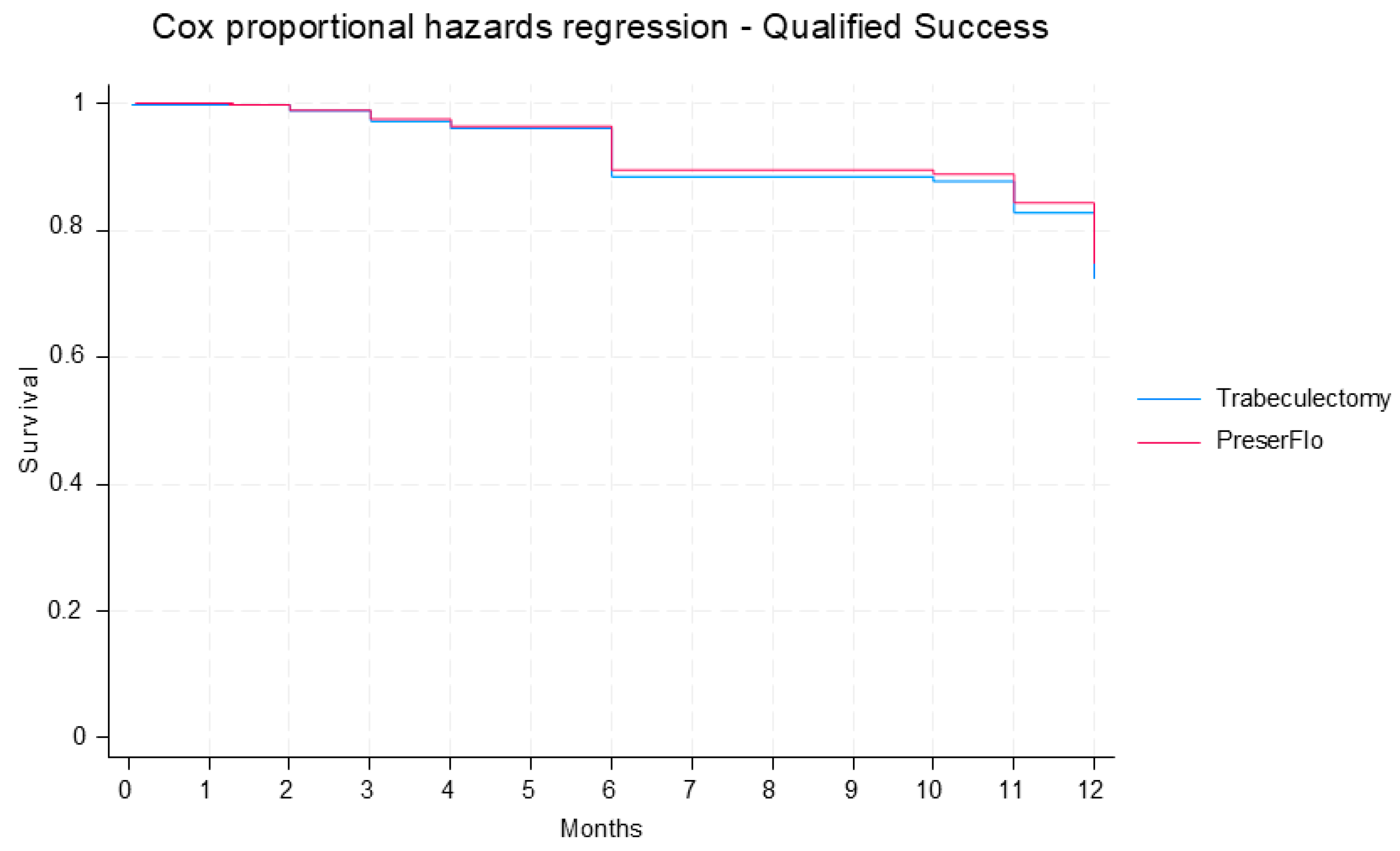
Complete and qualified success did not differ significantly between groups. The cumulative probability of complete success was estimated to be 61.3% in the PF group and 62.7% in the trabeculectomy group at 12 months post-operatively [hazard ratio (HR): 1.0; 95% CI: 0.5, 2.2;
p = 0.984) (
Figure 4). The cumulative probability of qualified success was predicted to be 74.9% in the PF group and 72.5% in the trabeculectomy group at 12 months post-operatively (HR: 0.9; 95% CI: 0.4, 2.2;
p = 0.813) (
Figure 5).
In PF eyes, 7 (14.6%) required surgical revision. One eye (2.1%) underwent Paul tube implantation, and the other six (12.5%) had open revision with trabeculectomy/MMC (
Figure 6). Two (4.2%) occurred between 2 and 3 months, with the remaining five (10.4%) having between 11 and 13 months post-operatively. Late trabeculectomy complications included numerical hypotony in five eyes (10.6%), clinically significant hypotony in one eye (2.1%), and blebitis/endophthalmitis in one eye (2.1%). One eye (2.1%) underwent Baerveldt tube implantation with concurrent phacoemulsification and posterior chamber intraocular lens (PCIOL) insertion, and the other one (2.1%) required sequential CyPass implantation, phacoemulsification/PCIOL, and placement of a Baerveldt tube (
Table 4).
4. Discussion
This retrospective cohort analysis compares the effectiveness and safety of PF and trabeculectomy for surgical glaucoma management. The findings indicate that both procedures reduce IOP and the need for medication.
Early post-operative hypotony, primarily occurring within the first two weeks, was common in PF eyes that did not receive an intraluminal 10/0 nylon suture. While most cases were asymptomatic and resolved spontaneously, some patients experienced complications like choroidal detachment and reduced visual acuity. To address this, the use of 10/0 nylon stenting was systematically adopted in the remaining 40 PF eyes, which effectively prevented early hypotony. Although approximately 75% of these stents were removed within three months, several cases maintained adequate IOP control with the stents in place. This suggests that without the stent, hypotony would have likely occurred. By the 12-month follow-up, no PF patients in this study had numerical hypotony. These results are consistent with the existing literature. Lupardi et al. reported no hypotony in stented PF eyes, while non-stented cases had a 28.6% incidence of hypotony and a 9.5% rate of choroidal detachment [
6]. Similarly, Chami et al. found significantly higher rates of both numerical and symptomatic hypotony in non-stented PF eyes compared to their stented counterparts (44% vs. 24%,
p = 0.007 and 28% vs. 13%,
p = 0.027, respectively) [
7]. Both studies advocate for the use of 10/0 nylon intraluminal stents to reduce hypotony. The use of 9/0 nylon, which provides total occlusion and must be removed to achieve drainage, has also been reported in the literature [
7].
The concentration of MMC used in this PF series aligns with the 0.3–0.4 mg/mL concentration recommended in most of the literature [
1,
4,
5,
8]. Previous studies, such as one by Beckers et al., have demonstrated that a higher dose (0.4 mg/mL) results in better outcomes, including a higher rate of medication-free patients (90.3% vs. 51.9% at 0.2 mg/mL) and superior IOP reduction [
9]. A recent study utilized sub-Tenon MMC administration over sponge-based application [
10]. In the current cohort, the surgeon (G.A.L.) assessed the appropriate MMC dose at the time of surgery, tailoring it to the integrity of the conjunctival and Tenon’s tissue. While crucial for surgical success, overdosing MMC can lead to complications such as avascular conjunctiva and blebitis, particularly in elderly Caucasian patients [
11,
12].
The PF procedure in this study positioned the pledgets more posteriorly than in trabeculectomy, a technique that aligns with the resulting posterior position of PF blebs [
11]. This may be a clinical advantage, as posterior bleb locations are associated with a lower risk of long-term complications like blebitis and endophthalmitis [
11,
12]. The findings indicated that fibrosis around the device tip in PF eyes may have limited the effectiveness of needling and potentially contributed to the requirement for open revision. In contrast, bleb needling for failed trabeculectomy can effectively puncture the Tenon’s cyst wall and fibrosis around the scleral flap, recreating the sclerotomy.
Trabeculectomy necessitates more frequent early post-operative visits (one to two weekly) to assess the need for 5-fluoruracil (5-FU) injections, massage of the scleral trapdoor, and potential suture removal. The less invasive nature of the PF procedure leads to less inflammation and fewer required clinical reviews, improving short-term patient quality of life [
4]. At 12 months, however, trabeculectomy resulted in greater IOP reduction, which is the more clinically beneficial outcome, although it did not reach statistical significance in this study. This is likely due to the higher outflow through the trapdoor and the absence of a stent foreign body. Overall, PF success rates range from 52% to 74% at one year [
5,
8,
9,
13]. Baker et al. found that the probability of success was significantly higher in the trabeculectomy group (72.7%) compared to the PF group (53.9%,
p < 0.01) [
14]. Fili et al. reported that 94% of trabeculectomy eyes had a >20% reduction in IOP without medication, compared to 81% of PF eyes [
1]. Similarly, Zweifel et al. found that trabeculectomy led to a greater IOP reduction (12 mmHg vs. 7 mmHg,
p = 0.01) [
15].
Postoperative inflammation is generally milder in PF patients, allowing for a more rapid steroid taper [
4]. However, ceasing topical steroids earlier might be a contributing factor to the increased rates of fibrosis observed in PF eyes. Early hypotony in PF is often due to peritubular leaks, most of which resolve spontaneously within one to two weeks, especially if the flange is well-positioned. However, persistent hypotony can cause complications like anterior chamber flattening and choroidal detachment, requiring surgical revision. This study showed a higher rate of long-term hypotony in the trabeculectomy group. Although this, by definition, was regarded as a failure, only one eye required scleral patching due to reduced vision from choroidal folds [
1,
3,
14,
16,
17].
PF eyes in this study showed a trend toward a higher rate (
p = 0.059) of open revision. At revision surgery, fibrosis was commonly found surrounding the tip of the tube. This was addressed by either removing the PF or re-stenting it with a buried releasable 10/0 nylon suture, as well as performing a trabeculectomy with MMC adjacent to the original site (
Figure 6). Other studies support open revision with MMC as a safe and effective alternative to device exchange or conversion to trabeculectomy [
18,
19]. Meta-analytic data have shown that PF patients, particularly those without prior glaucoma surgery, have increased re-intervention rates [
5]. This persistent fibrosis remains a significant obstacle to surgical success and highlights the need for further research into anti-fibrotic interventions and myofibroblast inhibition [
20].
When comparing trabeculectomy with the PF in a single-surgeon consecutive series, the surgeon’s consistent technique and patient selection offer a key advantage, minimizing the influence of inter-surgeon variability on outcomes. However, this study design is susceptible to significant biases. For example, the surgeon might initially perform PF on patients with less severe glaucoma or those with a higher chance of success, leading to a selection bias that could artificially inflate the new technique’s reported efficacy. Selection bias resulting from the PF cohort’s older age may explain their improved post-operative outcomes, which could be attributed to the reduced fibrotic response in this demographic. Furthermore, the predominantly Caucasian patient population in both cohorts limits the study findings and may have contributed to increased rates of success. A temporal bias is also present; any improvements in surgical instruments, technique or post-operative management protocols over time would benefit the later PF cohort, confounding the direct comparison with the earlier trabeculectomy group. As a result, the findings of this study may not be generalizable to other surgeons or provide a truly objective comparison of the two techniques that would be better achieved with a multi-center, multi-surgeon, randomized trial with larger sample sizes.
5. Conclusions
In conclusion, this study confirms that both PF and trabeculectomy are effective surgical options for glaucoma, significantly reducing IOP and medication dependency. The PF procedure was associated with less inflammation and a more rapid steroid taper. The adoption of intraoperative nylon stenting in PF surgery proved crucial in preventing early post-operative hypotony. However, PF eyes had a higher rate of open surgical revisions, often due to persistent fibrosis that limited the effectiveness of needling. Future research should focus on refining patient selection criteria for PF and exploring novel anti-fibrotic interventions to improve the long-term success rates.
Author Contributions
Conceptualization, A.N.K. and G.A.L.; data curation A.N.K. and G.A.L.; visualization A.N.K. and G.A.L.; resources A.N.K. and G.A.L.; validation A.N.K. and G.A.L.; writing original draft A.N.K. and G.A.L.; writing review and editing A.N.K. and G.A.L. Investigation (data collection) mainly by A.N.K.; supervision, project administration and methodology mainly by G.A.L. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Royal Australian and New Zealand College of Ophthalmologists (RANZCO) Human Research and Ethics Committee (reference number: 195.25), on the 23 June 2025.
Informed Consent Statement
The patient consent was waived due to this being a retrospective cohort study. The participants are not vulnerable groups, and the study is a minimally intrusive retrospective study which did not require contact with the patients. There were no psychological or physical risks to the patients. The data collected will not pose any ethical concerns as there was no coercion or deception required to obtain data from patients.
Data Availability Statement
Data can be made available from the authors if given reasonable written request.
Acknowledgments
Alice Chu (A.C.), Singapore, for conducting statistical analysis of the results, formal analysis and software.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| PF | PreserFlo MicroShunt |
| IOP | Intraocular Pressure |
| 5-FU | 5-Fluorouracil |
| MMC | Mitomycin C |
| VA | Visual Acuity |
| IPTW | Inverse probability of treatment weighting |
References
- Fili, S.; Boutsika, K.; Kokkali, S.; Patsoukis, A.; Patsouras, A.; Laspas, P.; Garnavou-Xirou, C.; Georgopoulos, G. PreserFlo™ MicroShunt Versus trabeculectomy in Patients with Moderate to Advanced Open-Angle Glaucoma: 12-Month Follow-Up of a Single-Center Prospective Study. Cureus 2022, 14, e28288. [Google Scholar] [CrossRef] [PubMed]
- Jamke, M.; Fritz, M.; Laspas, P.; Pfeiffer, N.; Grus, F.H.; Hoffmann, E.M. PRESERFLO™ MicroShunt versus trabeculectomy: 1-year results on efficacy and safety. Graefes Arch. Clin. Exp. Ophthalmol. 2023, 261, 2901–2915. [Google Scholar] [CrossRef] [PubMed]
- Pillunat, K.R.; Herber, R.; Jasper, C.; Berchner, J.; Pfeiffer, N.; Pillunat, L.E. PRESERFLO™ MicroShunt versus trabeculectomy: First results on efficacy and safety. Acta Ophthalmol. 2022, 100, 779–790. [Google Scholar] [CrossRef] [PubMed]
- Khan, A.; Khan, A.U. Comparing the safety and efficacy of PreserFlo Microshunt implantation and trabeculectomy for glaucoma: A systematic review and meta-analysis. Acta Ophthalmol. 2024, 102, 443–451. [Google Scholar] [CrossRef] [PubMed]
- Governatori, L.; Oliverio, L.; Mermoud, A.; Scampoli, A.; Sarati, F.; Carradori, A.; Catalani, R.; Monaco, C.; Caporossi, T.; Rizzo, S. PreserFlo MicroShunt versus trabeculectomy: An updated meta-analysis and systematic review. Graefes Arch. Clin. Exp. Ophthalmol. 2025, 263, 885–899. [Google Scholar] [CrossRef] [PubMed]
- Lupardi, E.; Laffi, G.L.; Moramarco, A.; Barboni, P.; Fontana, L. Systematic PreserFlo MicroShunt Intraluminal Stenting for Hypotony Prevention in Highly Myopic Patients: A Comparative Study. J. Clin. Med. 2023, 12, 1677. [Google Scholar] [CrossRef] [PubMed]
- Chami, J.; Tan, J.C.K.; Manning, D.; Weiss, J.; Schlenker, M.B.; Ahmed, I.I.K. Comparative Study of Early Safety and Effectiveness Outcomes of the PreserFlo MicroShunt with and without an Intraluminal Suture Stent. Ophthalmol. Glaucoma 2025, 8, 367–374. [Google Scholar] [CrossRef] [PubMed]
- Bhayani, R.; Jawla, S.; Trikha, S.; Mehta, R.; Ahir, B.K.; Lyall, D.A.M.; Chandra, A.; Ahmed, F.; Smith, H.B. Short-term safety and efficacy of PreserFlo™ Microshunt in glaucoma patients: A multicentre retrospective cohort study. Eye 2023, 37, 644–649. [Google Scholar] [CrossRef] [PubMed]
- Beckers, H.J.M.; Aptel, F.; Webers, C.A.B.; Bluwol, E.; Martinez-de-la-Casa, J.M.; Cordeiro, M.F.; Stalmans, I.; Vandewalle, E.; García-Feijoó, J. Safety and Effectiveness of the PRESERFLO® MicroShunt in Primary Open-Angle Glaucoma: Results from a 2-Year Multicenter Study. Ophthalmol. Glaucoma 2022, 5, 195–209. [Google Scholar] [CrossRef] [PubMed]
- Majtanova, N.; Takacova, A.; Kurilova, V.; Hejsek, L.; Majtan, J.; Kolar, P. One-Year Comparison of Efficacy and Safety of PreserFlo MicroShunt with Mitomycin C Applied by Sub-Tenon Injection Versus Sponge. Ophthalmol. Ther. 2025, 14, 153–167. [Google Scholar] [CrossRef]
- Ibarz Barberá, M.; López-Grau, N.S.; Amaro-Alcázar, A.; Morales-Fernandez, L.; García-Feijoó, J.; Martínez-de-la-Casa, J.M. Bleb geometry and morphology after PreserFlo Microshunt surgery: Risk factors for surgical failure. PLoS ONE 2023, 18, e0286884. [Google Scholar] [CrossRef] [PubMed]
- Hasan, S.M.; Theilig, T.; Meller, D. Comparison of Bleb Morphology following PRESERFLO® MicroShunt and trabeculectomy Using Anterior Segment OCT. Diagnostics 2023, 13, 3373. [Google Scholar] [CrossRef] [PubMed]
- Tanner, A.; Haddow, J.; Ahir, B.K.; Lyall, D.A.M.; Jawla, S.; Ahmed, F.; Chandra, A.; Bhayani, R. One-year surgical outcomes of the PreserFlo MicroShunt in glaucoma: A multicentre analysis. Br. J. Ophthalmol. 2023, 107, 1104–1111. [Google Scholar] [CrossRef] [PubMed]
- Baker, N.D.; Barnebey, H.S.; Moster, M.R.; Flowers, B.E.; Maslin, J.S.; Grover, D.S.; Panarelli, J.F.; Sarkisian, S.R.; Noecker, R.J.; Kahook, M.Y.; et al. Ab-Externo MicroShunt versus Trabeculectomy in Primary Open-Angle Glaucoma: One-Year Results from a 2-Year Randomized, Multicenter Study. Ophthalmology 2021, 128, 1710–1721. [Google Scholar] [CrossRef] [PubMed]
- Zweifel, L.A.B.; Storp, J.J.; Vietmeier, F.E.; Eter, N.; Brücher, V.C. PreserFlo MicroShunt versus Trabeculectomy: Efficacy and Surgical Success within a Heterogenous Patient Cohort. Life 2024, 14, 1171. [Google Scholar] [CrossRef] [PubMed]
- Nobl, M.; Grün, C.; Kassumeh , S.; Priglinger, S.; Mackert, M.J. One-Year Outcomes of PreserFlo™ MicroShunt Implantation versus trabeculectomy for Pseudoexfoliation Glaucoma. J. Clin. Med. 2023, 12, 3000. [Google Scholar] [CrossRef] [PubMed]
- Batlle, J.F.; Fantes, F.; Riss, I.; Pinchuk, L.; Alburquerque, R.; Kato, Y.P.; Arrieta, E.; Peralta, A.C.; Palmberg, P.; Parrish, R.K. Long-term Results of the PRESERFLO MicroShunt in Patients with Primary Open-angle Glaucoma from a Single-center Nonrandomized Study. J. Glaucoma 2021, 30, 281–286. [Google Scholar] [CrossRef] [PubMed]
- Sadruddin, O.; Pinchuk, L.; Angeles, R.; Palmberg, P.; Parrish, R.K.; Weber, B.A.; Mehra, K.S. Ab externo implantation of the MicroShunt, a poly (styrene-block-isobutylene-block-styrene) surgical device for the treatment of primary open-angle glaucoma: A review. Eye Vis. 2019, 6, 36. [Google Scholar] [CrossRef] [PubMed]
- Strzalkowska, A.; Al-Mugheiry, T.S.; Trikha, S.; Verma, S.; Stalmans, I.; Dick, A.D. Outcomes of Open Bleb Revision After PreserFlo MicroShunt Failure in Patients with Glaucoma. J. Glaucoma 2023, 32, 681–685. [Google Scholar] [CrossRef] [PubMed]
- Saeed, E.; Gołaszewska, K.; Dmuchowska, D.A.; Zalewska, R.; Konopińska, J. The PreserFlo MicroShunt in the Context of Minimally Invasive Glaucoma Surgery: A Narrative Review. Int. J. Environ. Res. Public Health 2023, 20, 2904. [Google Scholar] [CrossRef] [PubMed]
| Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).