Short-Term Outcomes After Transtibial Repair of Medial Meniscus Posterior Root Tears: A Case Series
Abstract
1. Introduction
2. Materials and Methods
2.1. Patient Selection
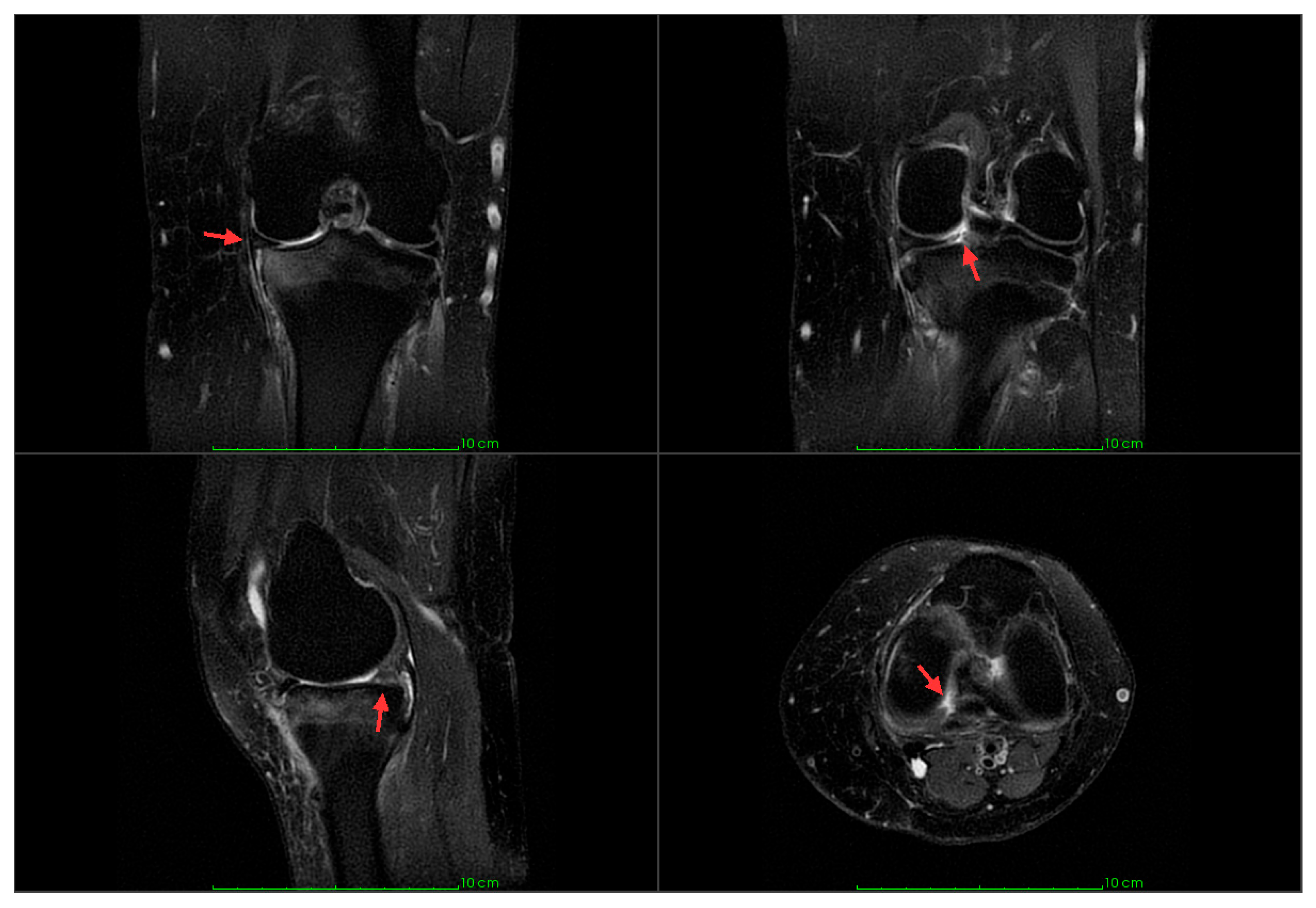
2.2. Surgical Technique
2.3. Postoperative Rehabilitation and Follow-Up
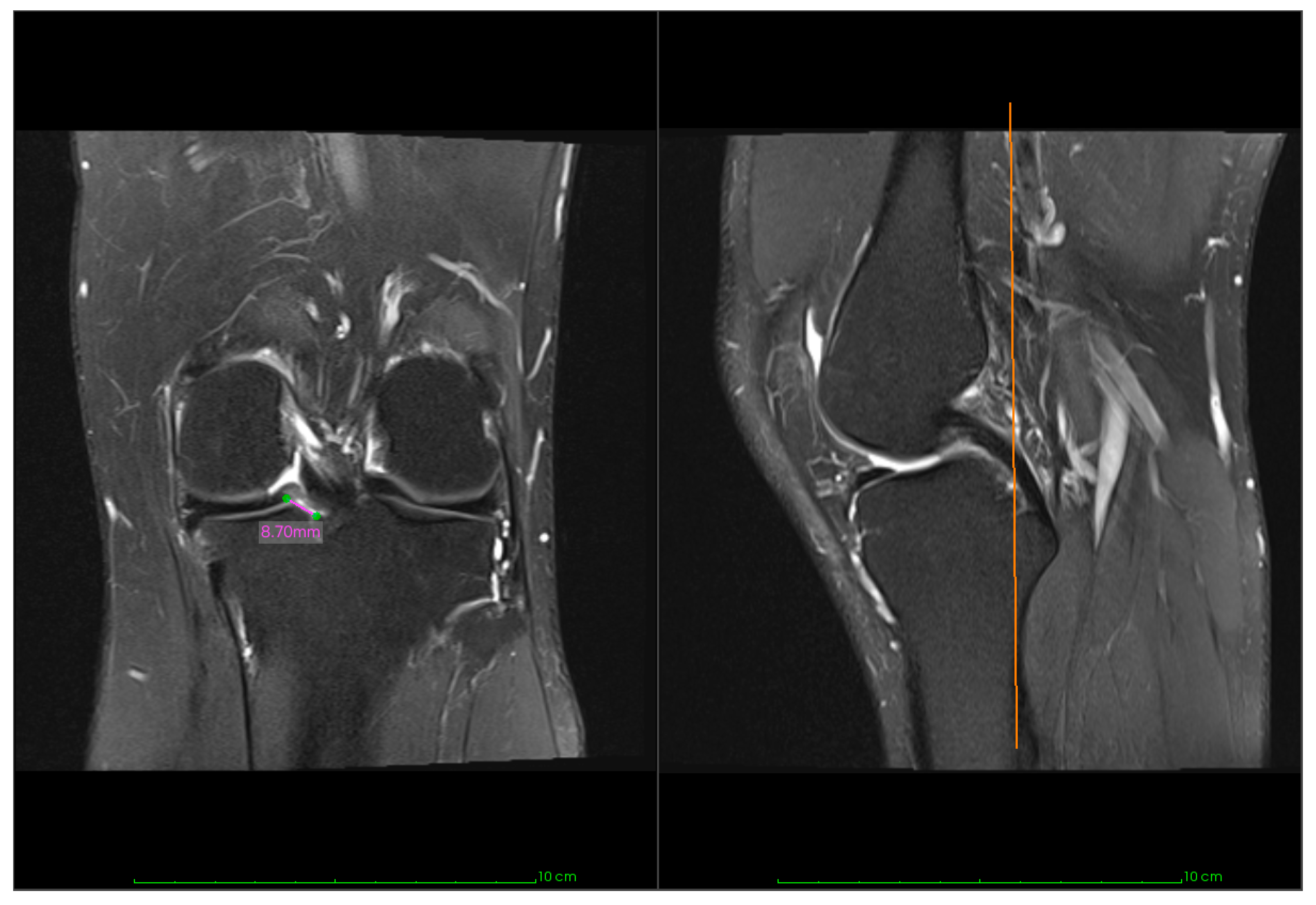
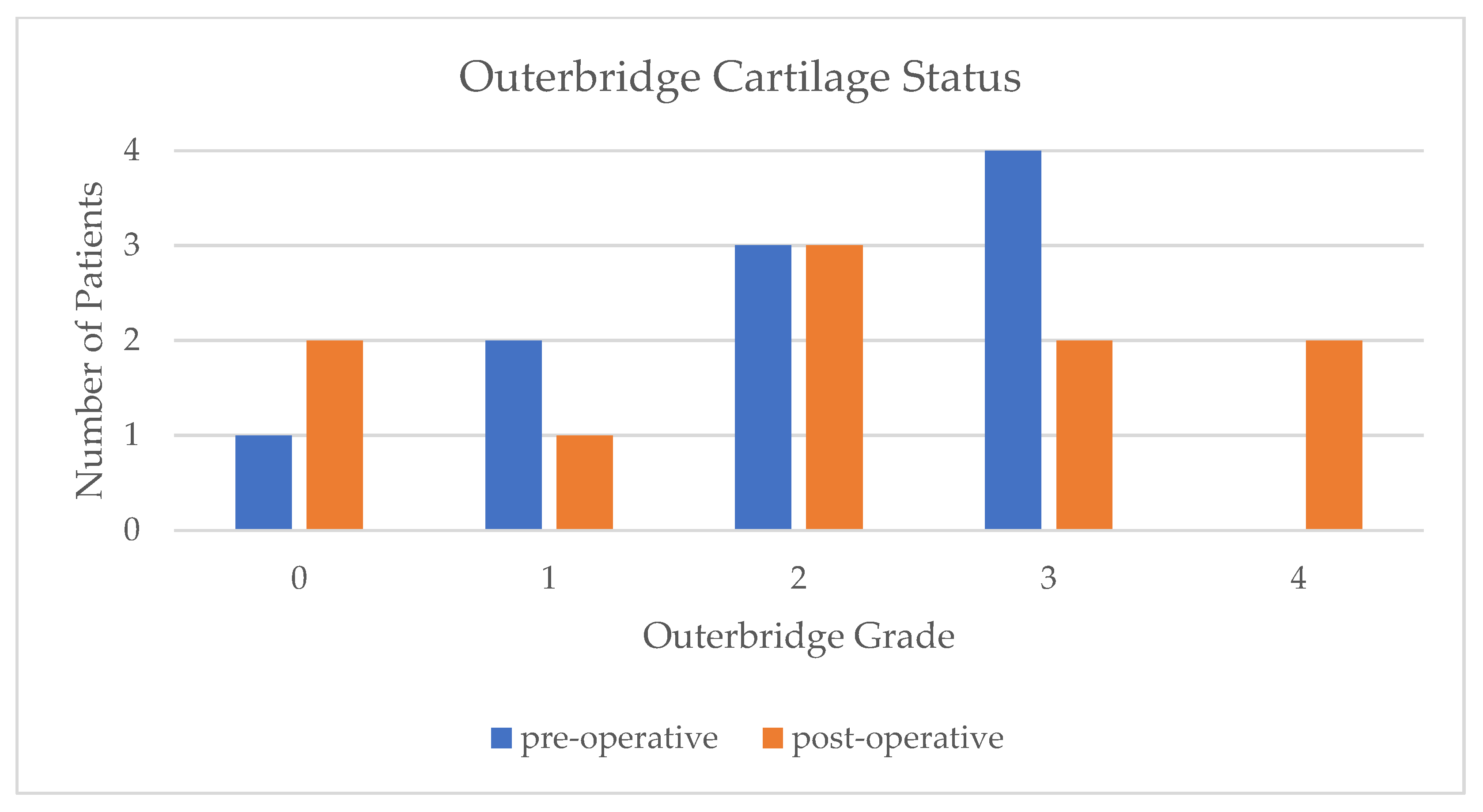
2.4. Clinical Outcomes and Imaging
2.5. Statistical Analysis
3. Results
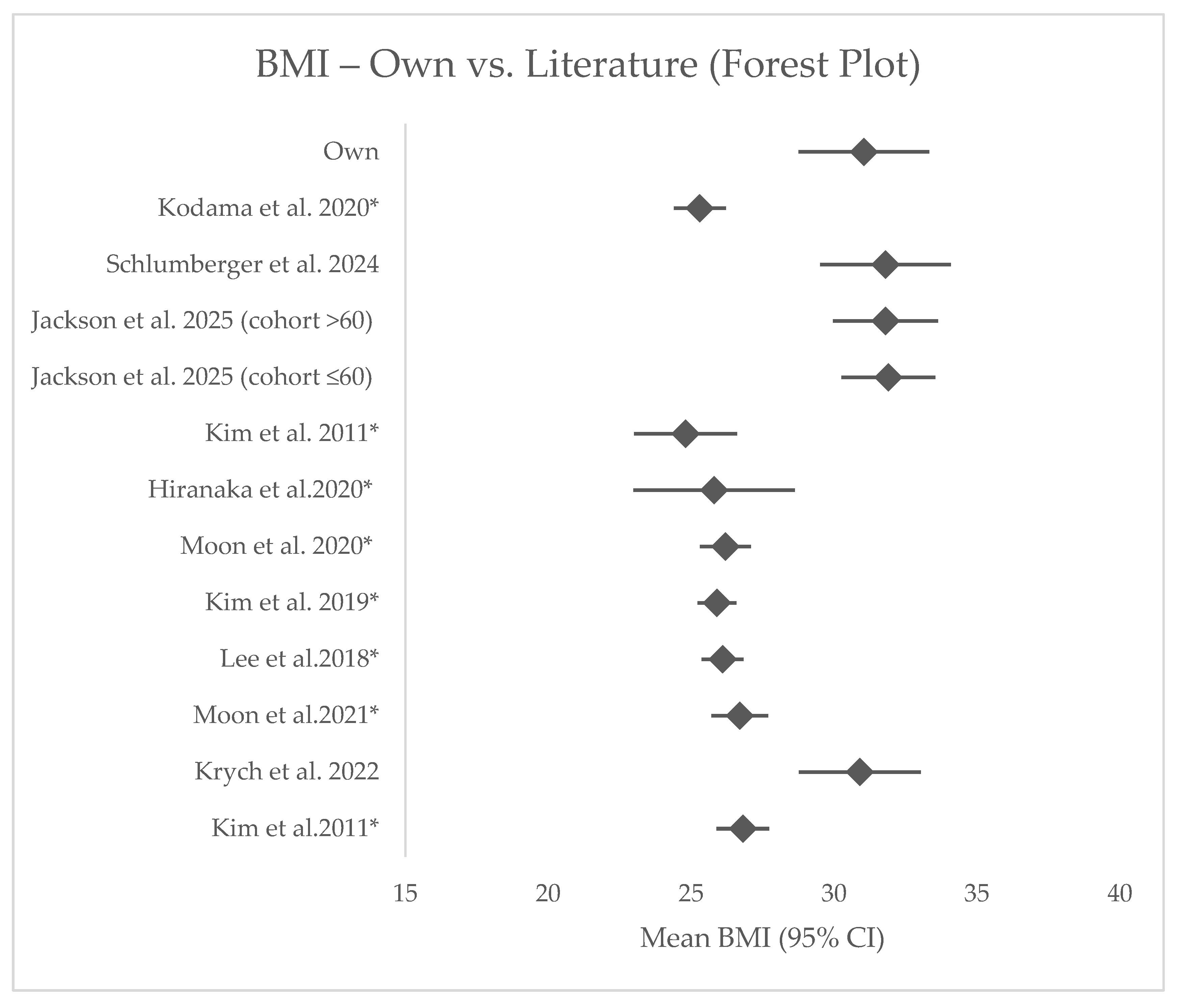
3.1. Comparative Results
3.2. Within-Cohort Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| BMI | Body mass index |
| IKDC | International Knee Documentation Committee |
| ME | Meniscal extrusion |
| MMPRT | Medial meniscus posterior root tear |
| NWB | Non-weight bearing |
| OA | Osteoarthritis |
| PD-FS | Proton density-weighted fat-saturated |
| PROM | Patient-reported outcome measure |
| PRP/PRG | Platelet-rich plasma/gel |
| PT | Physiotherapy |
| RCT | Randomized controlled trial |
| ROM | Range of motion |
| SAR | Suture anchor repair |
| SF-36 | 36-Item Short Form Survey |
| TPO | Transtibial pull-out technique |
| VAS | Visual analog scale |
| WOMET | Western Ontario Meniscal Evaluation Tool |
References
- Mameri, E.S.; Dasari, S.P.; Fortier, L.M.; Verdejo, F.G.; Gursoy, S.; Yanke, A.B.; Chahla, J. Review of Meniscus Anatomy and Biomechanics. Curr. Rev. Musculoskelet. Med. 2022, 15, 323–335. [Google Scholar] [CrossRef] [PubMed]
- Hantouly, A.T.; Aminake, G.; Khan, A.S.; Ayyan, M.; Olory, B.; Zikria, B.; Al-Khelaifi, K. Meniscus root tears: State of the art. Int. Orthop. 2024, 48, 955–964. [Google Scholar] [CrossRef] [PubMed]
- Allaire, R.; Muriuki, M.; Gilbertson, L.; Harner, C.D. Biomechanical consequences of a tear of the posterior root of the medial meniscus: Similar to total meniscectomy. J. Bone Jt. Surg. 2008, 90, 1922–1931. [Google Scholar] [CrossRef]
- Feucht, M.J.; Grande, E.; Brunhuber, J.; Rosenstiel, N.; Burgkart, R.; Imhoff, A.B.; Braun, S. Biomechanical comparison between suture anchor and transtibial pull-out repair for posterior medial meniscus root tears. Am. J. Sports Med. 2013, 42, 187–193. [Google Scholar] [CrossRef]
- Moon, H.-S.; Choi, C.-H.; Jung, M.; Chung, K.; Jung, S.-H.; Kim, Y.-H.; Kim, S.-H. Medial Meniscus Posterior Root Tear: How Far Have We Come and What Remains? Medicina 2023, 59, 1181. [Google Scholar] [CrossRef]
- Krych, A.J.; Song, B.M.; Nauert, R.F.; Cook, C.S.; Levy, B.A.; Camp, C.L.; Stuart, M.J.; Smith, P.A. Prospective Consecutive Clinical Outcomes After Transtibial Root Repair for Posterior Meniscal Root Tears: A Multicenter Study. Orthop. J. Sports Med. 2022, 10, 23259671221079794. [Google Scholar] [CrossRef]
- Kim, J.S.; Lee, M.K.; Choi, M.Y.; Kong, D.H.; Ha, J.K.; Kim, J.G.; Chung, K.S. Rehabilitation after Repair of Medial Meniscus Posterior Root Tears: A Systematic Review of the Literature. Clin. Orthop. Surg. 2023, 15, 740–751. [Google Scholar] [CrossRef]
- Kattan, A.E.; AlHemsi, H.B.; AlKhawashki, A.M.; AlFadel, F.B.; Almoosa, S.M.; Mokhtar, A.M.; Alasmari, B.A. Patient Compliance With Physical Therapy Following Orthopedic Surgery and Its Outcomes. Cureus 2023, 15, e37217. [Google Scholar] [CrossRef]
- Naqvi, A.A.; Hassali, M.A.; Naqvi, S.B.S.; Shakeel, S.; Zia, M.; Fatima, M.; Iffat, W.; Khan, I.; Jahangir, A.; Nadir, M.N. Development and validation of the General Rehabilitation Adherence Scale (GRAS) in patients attending physical therapy clinics for musculoskeletal disorders. BMC Musculoskelet. Disord. 2020, 21, 65. [Google Scholar] [CrossRef] [PubMed]
- Slattery, C.; Kweon, C.Y. Classifications in Brief: Outerbridge Classification of Chondral Lesions. Clin. Orthop. Relat. Res. 2018, 476, 2101–2104. [Google Scholar] [CrossRef]
- Kim, S.B.; Ha, J.K.; Lee, S.W.; Kim, D.W.; Shim, J.C.; Kim, J.G.; Lee, M.Y. Medial meniscus root tear refixation: Comparison of clinical, radiologic, and arthroscopic findings with medial meniscectomy. Arthrosc. J. Arthrosc. Relat. Surg. 2011, 27, 346–354. [Google Scholar] [CrossRef]
- Kim, J.-H.; Chung, J.-H.; Lee, D.-H.; Lee, Y.-S.; Kim, J.-R.; Ryu, K.-J. Arthroscopic suture anchor repair versus pullout suture repair in posterior root tear of the medial meniscus: A prospective comparison study. Arthrosc. J. Arthrosc. Relat. Surg. 2011, 27, 1644–1653. [Google Scholar] [CrossRef]
- Schlumberger, M.; Michalski, S.; Beel, W.; Mayer, P.; Schuster, P.; Immendörfer, M.; Mayr, R.; Richter, J. Short-term results of tibial interference screw fixation for transtibial medial meniscus posterior root pull-out repair. J. Orthop. 2024, 50, 155–161. [Google Scholar] [CrossRef] [PubMed]
- Jackson, G.R.; Knapik, D.M.; Khan, Z.A.; Jawanda, H.; Obioha, O.A.; Kaplan, D.J.; McCormick, J.R.; Sugrañes, J.; Batra, A.; Mameri, E.S.; et al. Outcomes After Isolated Medial Meniscus Posterior Root Repairs Using an Anatomic Transtibial Pullout Technique in Patients Older Than 60 Years: A Matched Cohort Study. Orthop. J. Sports Med. 2025, 13, 23259671241274136. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.-S.; Ahn, J.H.; Kim, J.H.; Kyung, B.S.; Wang, J.H. Evaluation of Healing After Medial Meniscal Root Repair Using Second-Look Arthroscopy, Clinical, and Radiological Criteria. Am. J. Sports Med. 2018, 46, 2661–2668. [Google Scholar] [CrossRef]
- Moon, H.-S.; Choi, C.-H.; Jung, M.; Lee, D.-Y.; Hong, S.-P.; Kim, S.-H. Early Surgical Repair of Medial Meniscus Posterior Root Tear Minimizes the Progression of Meniscal Extrusion: 2-Year Follow-up of Clinical and Radiographic Parameters After Arthroscopic Transtibial Pull-out Repair. Am. J. Sports Med. 2020, 48, 2692–2702. [Google Scholar] [CrossRef]
- Hiranaka, T.; Furumatsu, T.; Kamatsuki, Y.; Miyazawa, S.; Okazaki, Y.; Masuda, S.; Okazaki, Y.; Kodama, Y.; Ozaki, T. The distance between the tibial tunnel aperture and meniscal root attachment is correlated with meniscal healing status following transtibial pullout repair for medial meniscus posterior root tear. Knee 2020, 27, 899–905. [Google Scholar] [CrossRef]
- Kodama, Y.; Furumatsu, T.; Masuda, S.; Okazaki, Y.; Kamatsuki, Y.; Okazaki, Y.; Hiranaka, T.; Miyazawa, S.; Yasumitsu, M.; Ozaki, T. Transtibial fixation for medial meniscus posterior root tear reduces posterior extrusion and physiological translation of the medial meniscus in middle-aged and elderly patients. Knee Surg. Sports Traumatol. Arthrosc. 2020, 28, 3416–3425. [Google Scholar] [CrossRef]
- Kim, C.-W.; Lee, C.-R.; Gwak, H.-C.; Kim, J.-H.; Park, D.-H.; Kwon, Y.-U.; Jung, S.-H. Clinical and Radiologic Outcomes of Patients With Lax Healing After Medial Meniscal Root Repair: Comparison With Subtotal Meniscectomy. Arthrosc. J. Arthrosc. Relat. Surg. 2019, 35, 3079–3086. [Google Scholar] [CrossRef]
- Moon, H.-S.; Choi, C.-H.; Yoo, J.-H.; Jung, M.; Lee, T.-H.; Jeon, B.-H.; Kim, S.-H. Mild to Moderate Varus Alignment in Relation to Surgical Repair of a Medial Meniscus Root Tear: A Matched-Cohort Controlled Study With 2 Years of Follow-up. Am. J. Sports Med. 2021, 49, 1005–1016. [Google Scholar] [CrossRef] [PubMed]
- LaPrade, R.F.; Matheny, L.M.; Moulton, S.G.; James, E.W.; Dean, C.S. Posterior Meniscal Root Repairs: Outcomes of an Anatomic Transtibial Pull-Out Technique. Am. J. Sports Med. 2017, 45, 884–891. [Google Scholar] [CrossRef]
- Chung, K.S.; Ha, J.K.; Ra, H.J.; Lee, H.S.; Lee, D.W.; Park, J.H.; Kim, D.H.; Kim, J.G. Pullout fixation for medial meniscus posterior root tears: Clinical results were not age-dependent, but osteoarthritis progressed. Knee Surg. Sports Traumatol. Arthrosc. 2019, 27, 189–196. [Google Scholar] [CrossRef]
- Jiang, E.X.; Abouljoud, M.M.; Everhart, J.S.; DiBartola, A.C.; Kaeding, C.C.; Magnussen, R.A.; Flanigan, D.C. Clinical factors associated with successful meniscal root repairs: A systematic review. Knee 2019, 26, 285–291. [Google Scholar] [CrossRef]
- Krivicich, L.M.; Kunze, K.N.; Parvaresh, K.C.; Jan, K.; DeVinney, A.; Vadhera, A.; LaPrade, R.F.; Chahla, J. Comparison of Long-term Radiographic Outcomes and Rate and Time for Conversion to Total Knee Arthroplasty Between Repair and Meniscectomy for Medial Meniscus Posterior Root Tears: A Systematic Review and Meta-analysis. Am. J. Sports Med. 2022, 50, 2023–2031. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Zhang, K.; Liu, X.; Liu, Z.; Yi, Q.; Jiang, J.; Xia, Y. The efficacy of meniscus posterior root tears repair: A systematic review and meta-analysis. J. Orthop. Surg. 2021, 29, 23094990211003350. [Google Scholar] [CrossRef] [PubMed]
- Ro, K.-H.; Kim, J.-H.; Heo, J.-W.; Lee, D.-H. Clinical and Radiological Outcomes of Meniscal Repair Versus Partial Meniscectomy for Medial Meniscus Root Tears: A Systematic Review and Meta-analysis. Orthop. J. Sports Med. 2020, 8, 2325967120962078. [Google Scholar] [CrossRef] [PubMed]
- Chung, K.S.; Ha, J.K.; Ra, H.J.; Kim, J.G. A meta-analysis of clinical and radiographic outcomes of posterior horn medial meniscus root repairs. Knee Surg. Sports Traumatol. Arthrosc. 2016, 24, 1455–1468. [Google Scholar] [CrossRef] [PubMed]
- Faucett, S.C.; Geisler, B.P.; Chahla, J.; Krych, A.J.; Kurzweil, P.R.; Garner, A.M.; Liu, S.; LaPrade, R.F.; Pietzsch, J.B. Meniscus Root Repair vs Meniscectomy or Nonoperative Management to Prevent Knee Osteoarthritis After Medial Meniscus Root Tears: Clinical and Economic Effectiveness. Am. J. Sports Med. 2019, 47, 762–769. [Google Scholar] [CrossRef]
- Boksh, K.; Shepherd, D.E.; Espino, D.M.; Ghosh, A.; Aujla, R.; Boutefnouchet, T. Centralization reduces meniscal extrusion, improves joint mechanics and functional outcomes in patients undergoing meniscus surgery: A systematic review and meta-analysis. Knee Surg. Sports Traumatol. Arthrosc. 2024, 33, 888–906. [Google Scholar] [CrossRef]
- Chung, K.S.; Ha, J.K.; Ra, H.J.; Kim, J.G. Preoperative varus alignment and postoperative meniscus extrusion are the main long-term predictive factors of clinical failure of meniscal root repair. Knee Surg. Sports Traumatol. Arthrosc. 2021, 29, 4122–4130. [Google Scholar] [CrossRef]
- Feucht, M.J.; Kühle, J.; Bode, G.; Mehl, J.; Schmal, H.; Südkamp, N.P.; Niemeyer, P. Arthroscopic Transtibial Pullout Repair for Posterior Medial Meniscus Root Tears: A Systematic Review of Clinical, Radiographic, and Second-Look Arthroscopic Results. Arthrosc. J. Arthrosc. Relat. Surg. 2015, 31, 1808–1816. [Google Scholar] [CrossRef]
- Nishino, K.; Hashimoto, Y.; Kinoshita, T.; Iida, K.; Tsumoto, S.; Nakamura, H. Anterior bone tunnel position increases meniscus migration in medial meniscus posterior root repair: A cadaveric study of suture length changes. J. Exp. Orthop. 2024, 11, e70028. [Google Scholar] [CrossRef]
- LaPrade, C.M.; Foad, A.; Smith, S.D.; Turnbull, T.L.; Dornan, G.J.; Engebretsen, L.; Wijdicks, C.A.; LaPrade, R.F. Biomechanical consequences of a nonanatomic posterior medial meniscal root repair. Am. J. Sports Med. 2015, 43, 912–920. [Google Scholar] [CrossRef]
- Robinson, J.R.; Frank, E.G.; Hunter, A.J.; Jermin, P.J.; Gill, H.S. The Strength of Transosseous Medial Meniscal Root Repair Using a Simple Suture Technique Is Dependent on Suture Material and Position. Am. J. Sports Med. 2018, 46, 924–932. [Google Scholar] [CrossRef]
- Jiang, E.X.; Everhart, J.S.; Abouljoud, M.; Kirven, J.C.; Magnussen, R.A.; Kaeding, C.C.; Flanigan, D.C. Biomechanical Properties of Posterior Meniscal Root Repairs: A Systematic Review. Arthrosc. J. Arthrosc. Relat. Surg. 2019, 35, 2189–2206.e2. [Google Scholar] [CrossRef] [PubMed]
- Tamura, M.; Furumatsu, T.; Yokoyama, Y.; Okazaki, Y.; Kawada, K.; Ozaki, T.; Kamatsuki, Y.; Hiranaka, T.; Al, E. Fast rehabilitation does not worsen clinical, radiological, and arthroscopic outcomes after medial meniscus posterior root repair: A retrospective comparative study. Asia-Pac. J. Sports Med. Arthrosc. Rehabilitation Technol. 2024, 38, 29–35. [Google Scholar] [CrossRef] [PubMed]
- Leatherwood, W.; Torres, A.; Perea, S.H.; Paulus, M. Demographic and Diagnostic Factors in Physical Therapy Attendance. Cureus 2024, 16, e55908. [Google Scholar] [CrossRef] [PubMed]
- ClinicalTrials.gov Identifier: NCT05985772. Operative vs. Non operative Management of Posterior Medial Meniscal Root Tears. n.d. Available online: https://ctv.veeva.com/study/operative-vs-non-operative-management-of-posterior-medial-meniscal-root-tears-a-randomized-multicen (accessed on 30 May 2025).
- Sundararajan, S.R.; Ramakanth, R.; Rajasekaran, S. Meniscal Root Repair Along with Auxiliary Procedures for Joint Preservation: Current Concepts. Indian J. Orthop. 2021, 55, 237–251. [Google Scholar] [CrossRef] [PubMed]
- Bansal, S.; Floyd, E.R.; A Kowalski, M.; Aikman, E.; Elrod, P.; Burkey, K.; Chahla, J.; LaPrade, R.F.; Maher, S.A.; Robinson, J.L.; et al. Meniscal repair: The current state and recent advances in augmentation. J. Orthop. Res. 2021, 39, 1368–1382. [Google Scholar] [CrossRef]
- Kaminski, R.; Kulinski, K.; Kozar-Kaminska, K.; Wasko, M.K.; Langner, M.; Pomianowski, S. Repair Augmentation of Unstable, Complete Vertical Meniscal Tears with Bone Marrow Venting Procedure: A Prospective, Randomized, Double-Blind, Parallel-Group, Placebo-Controlled Study. Arthrosc. J. Arthrosc. Relat. Surg. 2019, 35, 1500–1508.e1. [Google Scholar] [CrossRef]
- Kaminski, R.; Kulinski, K.; Kozar-Kaminska, K.; Wielgus, M.; Langner, M.; Wasko, M.K.; Kowalczewski, J.; Pomianowski, S. A Prospective, Randomized, Double-Blind, Parallel-Group, Placebo-Controlled Study Evaluating Meniscal Healing, Clinical Outcomes, and Safety in Patients Undergoing Meniscal Repair of Unstable, Complete Vertical Meniscal Tears (Bucket Handle) Augmented with Platelet-Rich Plasma. BioMed Res. Int. 2018, 2018, 9315815. [Google Scholar] [CrossRef]
- Rocha de Faria, J.L.; Cruz, R.S.; Campos, A.L.S.; Souza, G.G.A.; Di Cavalcanti, Y.S.; Goes, R.A. Meniscal Root Repair Alone or Combined with Different Procedures After at Least 6 Months of Follow-Up: A Series of Cases. Open Access J. Sports Med. 2022, 13, 25–34. [Google Scholar] [CrossRef] [PubMed]
- Bernard, C.D.; Kennedy, N.I.; Tagliero, A.J.; Camp, C.L.; Saris, D.B.; Levy, B.A.; Stuart, M.J.; Krych, A.J. Medial Meniscus Posterior Root Tear Treatment: A Matched Cohort Comparison of Nonoperative Management, Partial Meniscectomy, and Repair. Am. J. Sports Med. 2020, 48, 128–132. [Google Scholar] [CrossRef] [PubMed]

| N | Mean ± SD | |
|---|---|---|
| Follow-up time (months) | 14 | 18 ± 8 |
| Age (years) | 14 | 59 ± 13 |
| BMI (kg/m2) | 14 | 31 ± 4 |
| Symptom-to-repair (days) | 14 | 215 ± 212 |
| ROM (degrees) | 14 | 121 ± 16 |
| ME preoperative (mm) | 10 | 3.32 ± 1.77 |
| ME postoperative (mm) | 10 | 3.94 ± 1.72 |
| Outcome | Mean ± SD |
|---|---|
| Pain (VAS) | 2.79 ± 3.22 |
| IKDC | 63.4 ± 18.8 |
| WOMET total aggregate | 62.6 ± 31.1 |
| SF-36 points | 80.7 ± 19.4 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nistor, D.V.; Piu, S.; Mihu, D.R.; von Mengershausen, R. Short-Term Outcomes After Transtibial Repair of Medial Meniscus Posterior Root Tears: A Case Series. J. Clin. Med. 2025, 14, 7440. https://doi.org/10.3390/jcm14207440
Nistor DV, Piu S, Mihu DR, von Mengershausen R. Short-Term Outcomes After Transtibial Repair of Medial Meniscus Posterior Root Tears: A Case Series. Journal of Clinical Medicine. 2025; 14(20):7440. https://doi.org/10.3390/jcm14207440
Chicago/Turabian StyleNistor, Dan Viorel, Samuel Piu, Diana Raluca Mihu, and Romana von Mengershausen. 2025. "Short-Term Outcomes After Transtibial Repair of Medial Meniscus Posterior Root Tears: A Case Series" Journal of Clinical Medicine 14, no. 20: 7440. https://doi.org/10.3390/jcm14207440
APA StyleNistor, D. V., Piu, S., Mihu, D. R., & von Mengershausen, R. (2025). Short-Term Outcomes After Transtibial Repair of Medial Meniscus Posterior Root Tears: A Case Series. Journal of Clinical Medicine, 14(20), 7440. https://doi.org/10.3390/jcm14207440






