Bridging the Gap: Do Patient-Reported Outcome Measures Reflect Objective Knee Function After Cartilage Repair?
Abstract
1. Introduction
2. Material and Methods
2.1. German Cartilage Registry (KnorpelRegister DGOU)
2.2. Study Design and Data Collection
2.3. IKDC and ICRS Score
2.4. Statistics
3. Results
3.1. Patient and Defect Characteristics
3.2. Patient-Reported Outcomes and Correlations with the Objective ICRS Score
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Heir, S.; Nerhus, T.K.; Røtterud, J.H.; Løken, S.; Ekeland, A.; Engebretsen, L.; Årøen, A. Focal Cartilage Defects in the Knee Impair Quality of Life as Much as Severe Osteoarthritis:A Comparison of Knee Injury and Osteoarthritis Outcome Score in 4 Patient Categories Scheduled for Knee Surgery. Am. J. Sports Med. 2010, 38, 231–237. [Google Scholar] [CrossRef] [PubMed]
- Newman, A.P. Articular Cartilage Repair. Am. J. Sports Med. 1998, 26, 309–324. [Google Scholar] [CrossRef] [PubMed]
- Cicuttini, F.; Ding, C.; Wluka, A.; Davis, S.; Ebeling, P.R.; Jones, G. Association of cartilage defects with loss of knee cartilage in healthy, middle-age adults: A prospective study. Arthritis Rheum. 2005, 52, 2033–2039. [Google Scholar] [CrossRef] [PubMed]
- Schinhan, M.; Gruber, M.; Vavken, P.; Dorotka, R.; Samouh, L.; Chiari, C.; Gruebl-Barabas, R.; Nehrer, S. Critical-size defect induces unicompartmental osteoarthritis in a stable ovine knee. J. Orthop. Res. 2012, 30, 214–220. [Google Scholar] [CrossRef]
- Gelber, A.C.; Hochberg, M.C.; Mead, L.A.; Wang, N.Y.; Wigley, F.M.; Klag, M.J. Joint Injury in Young Adults and Risk for Subsequent Knee and Hip Osteoarthritis. Ann. Intern. Med. 2000, 133, 321–328. [Google Scholar] [CrossRef]
- Gomoll, A.H.; Minas, T. The quality of healing: Articular cartilage. Wound Repair. Regen. 2014, 22, 30–38. [Google Scholar] [CrossRef]
- Falah, M.; Nierenberg, G.; Soudry, M.; Hayden, M.; Volpin, G. Treatment of articular cartilage lesions of the knee. Int. Orthop. 2010, 34, 621–630. [Google Scholar] [CrossRef]
- Birkenes, T.; Furnes, O.; Laastad Lygre, S.H.; Solheim, E.; Aaroen, A.; Knutsen, G.; Drogset, J.O.; Heir, S.; Engebretsen, L.; Loken, S.; et al. Long-Term Outcomes of Arthroscopically Verified Focal Cartilage Lesions in the Knee: A 19-Year Multicenter Follow-up with Patient-Reported Outcomes. J. Bone Jt. Surg. 2024, 106, 1991–2000. [Google Scholar] [CrossRef]
- Roos, E.M.; Engelhart, L.; Ranstam, J.; Anderson, A.F.; Irrgang, J.J.; Marx, R.G.; Tegner, Y.; Davis, A.M. ICRS Recommendation Document: Patient-Reported Outcome Instruments for Use in Patients with Articular Cartilage Defects. Cartilage 2011, 2, 122–136. [Google Scholar] [CrossRef]
- Niemeyer, P.; Hanus, M.; Belickas, J.; László, T.; Gudas, R.; Fiodorovas, M.; Cebatorius, A.; Pastucha, M.; Hoza, P.; Magos, K.; et al. Treatment of Large Cartilage Defects in the Knee by Hydrogel-Based Autologous Chondrocyte Implantation: Two-Year Results of a Prospective, Multicenter, Single-Arm Phase III Trial. Cartilage 2022, 13, 19476035221085146. [Google Scholar] [CrossRef]
- Roos, E.M.; Lohmander, L.S. The Knee injury and Osteoarthritis Outcome Score (KOOS): From joint injury to osteoarthritis. Health Qual. Life Outcomes 2003, 1, 64. [Google Scholar] [CrossRef]
- Chamorro-Moriana, G.; Perez-Cabezas, V.; Espuny-Ruiz, F.; Torres-Enamorado, D.; Ridao-Fernández, C. Assessing knee functionality: Systematic review of validated outcome measures. Ann. Phys. Rehabil. Med. 2022, 65, 101608. [Google Scholar] [CrossRef] [PubMed]
- Hirschmuller, A.; Andres, T.; Schoch, W.; Baur, H.; Konstantinidis, L.; Sudkamp, N.P.; Niemeyer, P. Quadriceps Strength in Patients With Isolated Cartilage Defects of the Knee: Results of Isokinetic Strength Measurements and Their Correlation with Clinical and Functional Results. Orthop. J. Sports Med. 2017, 5, 2325967117703726. [Google Scholar] [CrossRef] [PubMed]
- Niemeyer, P.; Schweigler, K.; Grotejohann, B.; Maurer, J.; Angele, P.; Aurich, M.; Becher, C.; Fay, J.; Feil, R.; Fickert, S.; et al. The German Cartilage Registry (KnorpelRegister DGOU) for evaluation of surgical treatment for cartilage defects: Experience after six months including first demographic data. Z. Orthop. Unf. 2015, 153, 67–74. [Google Scholar] [CrossRef]
- Hefti, E.; Müller, W.; Jakob, R.P.; Stäubli, H.U. Evaluation of knee ligament injuries with the IKDC form. Knee Surg. Sports Traumatol. Arthrosc. 1993, 1, 226–234. [Google Scholar] [CrossRef]
- Irrgang, J.J.; Anderson, A.F.; Boland, A.L.; Harner, C.D.; Kurosaka, M.; Neyret, P.; Richmond, J.C.; Shelborne, K.D. Development and Validation of the International Knee Documentation Committee Subjective Knee Form. Am. J. Sports Med. 2001, 29, 600–613. [Google Scholar] [CrossRef]
- Gauthier, M.; Lê, T.N.; Wehn, A.; Joseph, S.; Tscholl, P.M. Subjective knee apprehension is not associated to physical parameters 6-12 months after anterior cruciate ligament reconstruction. J. Exp. Orthop. 2022, 9, 110. [Google Scholar] [CrossRef]
- Logerstedt, D.; Di Stasi, S.; Grindem, H.; Lynch, A.; Eitzen, I.; Engebretsen, L.; Risberg, M.A.; Axe, M.J.; Snyder-Mackler, L. Self-reported knee function can identify athletes who fail return-to-activity criteria up to 1 year after anterior cruciate ligament reconstruction: A delaware-oslo ACL cohort study. J. Orthop. Sports Phys. Ther. 2014, 44, 914–923. [Google Scholar] [CrossRef]
- Al-Gburi, M.; Kristiansen, J.B.; Christensen, K.B.; Krogsgaard, M. Functional performance tests, clinical measurements, and patient-reported outcome measures do not correlate as outcomes 1 year after anterior cruciate ligament reconstruction. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 5905–5912. [Google Scholar] [CrossRef]
- Hill, B.; Shah, S.; Moschetti, W.; Schilling, P. Do Patient Reported Outcomes Reflect Objective Measures of Function? Implications for Total Knee Arthroplasty. J. Arthroplast. 2023, 38, S162–S168.e3. [Google Scholar] [CrossRef]
- Ekanayake, C.D.; DeMik, D.E.; Glass, N.A.; Kotseos, C.; Callaghan, J.J.; Ratigan, B.L. Comparison of Patient-Reported Outcomes and Functional Assessment Using a Marker-Less Image Capture System in End-Stage Knee Arthritis. J. Arthroplast. 2022, 37, 2158–2163. [Google Scholar] [CrossRef]
- Oettl, F.C.; Leuthard, L.; Brunner, M.; Stadelmann, V.A.; Preiss, S.; Leunig, M.; Salzmann, G.M.; Hax, J. Correlation and Comparative Evaluation of MOCART and MOCART 2.0 for Assessing Cartilage Repair. Medicina 2025, 61, 745. [Google Scholar] [CrossRef]
- Sonesson, S.; Osterberg, A.; Gauffin, H.; Ardern, C.L.; Kvist, J.; Hagglund, M. Low correlation between functional performance and patient reported outcome measures in individuals with non-surgically treated ACL injury. Phys. Ther. Sport. 2021, 47, 185–192. [Google Scholar] [CrossRef]
- Bolink, S.A.; Grimm, B.; Heyligers, I.C. Patient-reported outcome measures versus inertial performance-based outcome measures: A prospective study in patients undergoing primary total knee arthroplasty. Knee 2015, 22, 618–623. [Google Scholar] [CrossRef]

| Variable | Mean ± SD or N (%) |
|---|---|
| Age, years | 39.2 ± 11.9 |
| BMI, kg/m2 | 28.5 ± 5.8 |
| Gender, male/female, n | 38/14 |
| Smoking status | Active: 9 (17.3%) |
| Former: 1 (1.9%) | |
| Never: 42 (80.8%) | |
| Follow-up time, months | 66.8 ± 31.2 |
| Clinical limb alignment, cm | Mean: −1.2 ± 2.3 (range −7.0 to +4.1) |
| Alignment categories | Varus: 23 (44.2%) |
| Neutral: 24 (46.2%) | |
| Valgus: 5 (9.6%) | |
| Etiology of defect | Traumatic: 28 (53.8%) |
| Degenerative: 24 (46.2%) | |
| Number of cartilage defects | 1 defect: 42 (80.8%) |
| 2 defects: 9 (17.3%) | |
| 3 defects: 1 (1.9%) | |
| Worst ICRS grade (n = 51) | Grade 1: 1 (1.9%) |
| Grade 2: 8 (15.4%) | |
| Grade 3: 33 (63.5%) | |
| Grade 4: 9 (17.3%) | |
| Previous surgeries on index knee | None: 34 (65.4%) |
| 1: 15 (28.8%) | |
| 2: 2 (3.8%) | |
| 3: 1 (1.9%) |
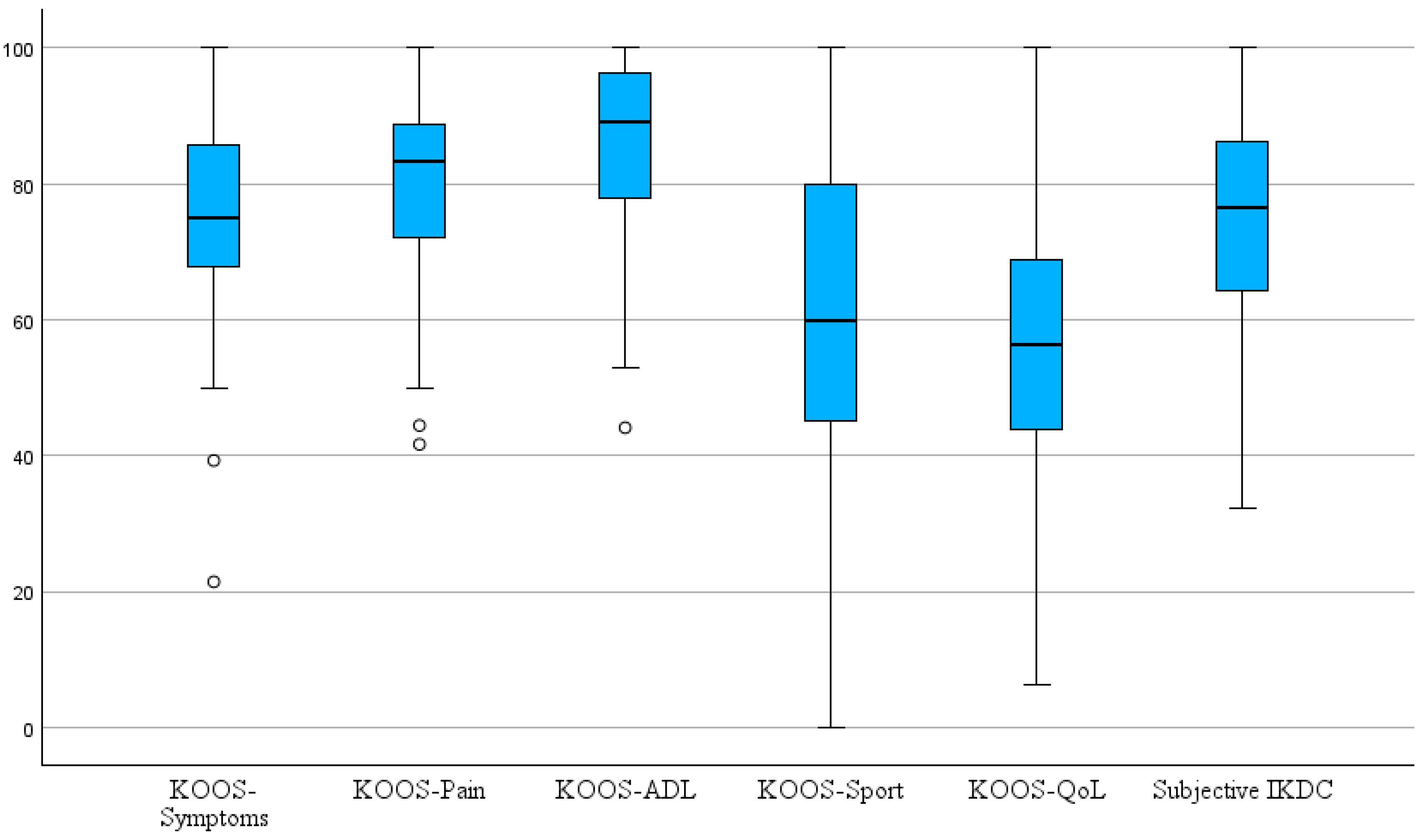
| Outcome Measure | Mean ± SD | Range | N |
|---|---|---|---|
| Subjective IKDC | 74.6 ± 15.6 | 32.2–100.0 | 52 |
| KOOS–Symptoms | 75.5 ± 15.7 | 21.4–100.0 | 43 |
| KOOS–Pain | 79.1 ± 14.6 | 41.7–100.0 | 43 |
| KOOS–ADL | 85.7 ± 13.1 | 44.1–100.0 | 43 |
| KOOS–Sport | 59.2 ± 26.1 | 0.0–100.0 | 42 |
| KOOS–QoL | 55.5 ± 19.1 | 6.3–100.0 | 43 |
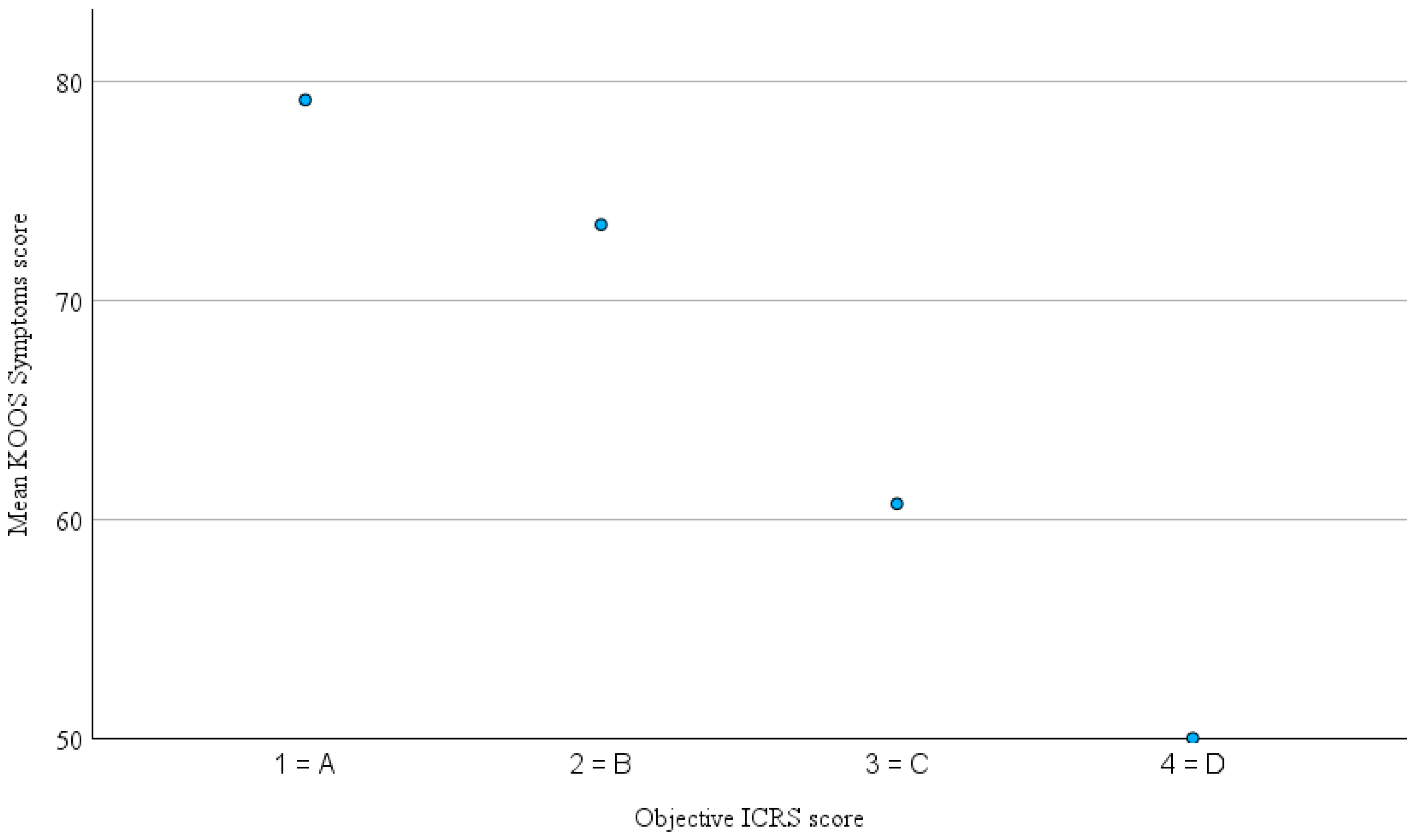
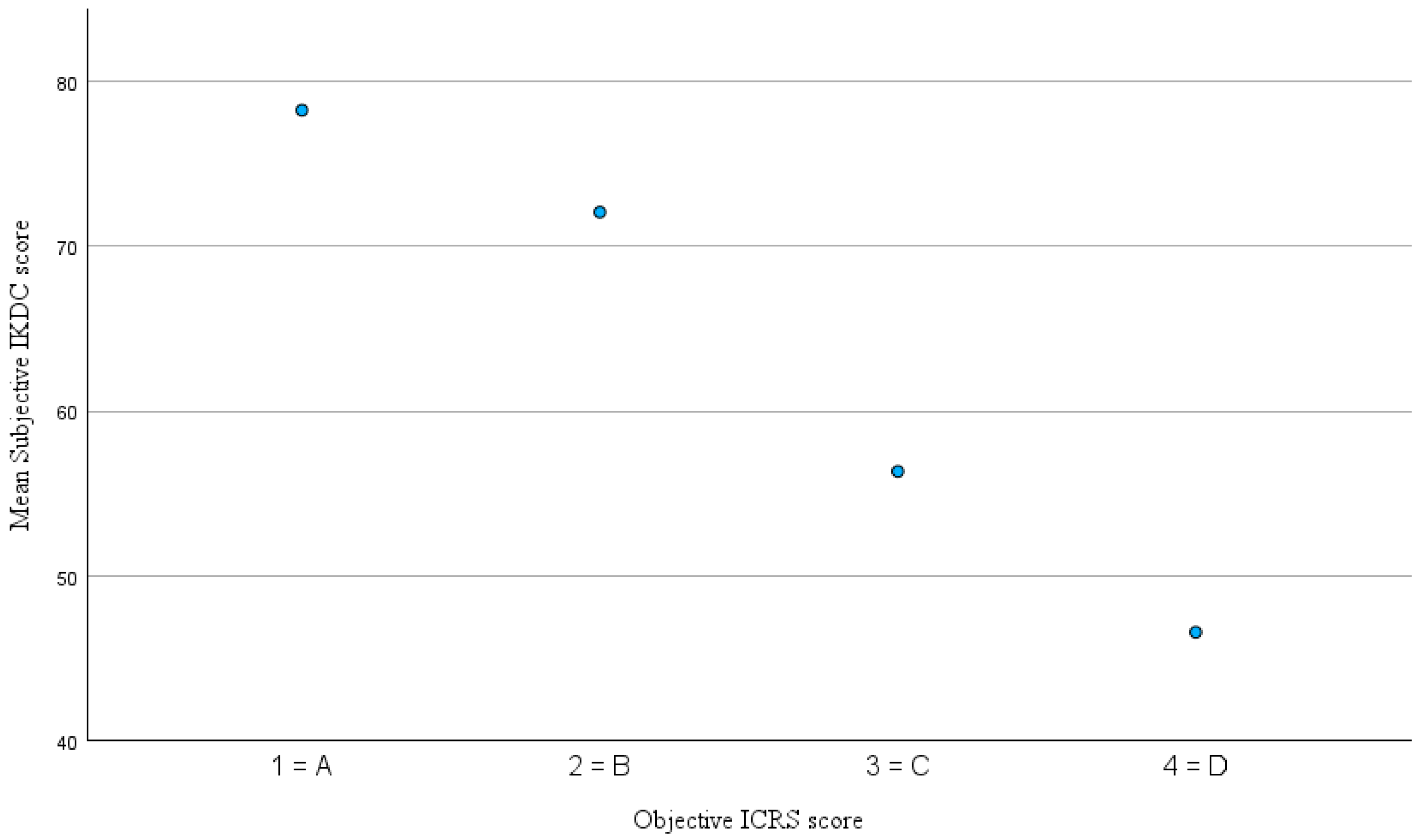
| Variable Pair | Spearman’s ρ | p-Value | Interpretation |
|---|---|---|---|
| KOOS–Pain vs. objective ICRS | –0.268 | 0.082 | weak, not significant |
| KOOS–Symptoms vs. objective ICRS | –0.420 * | 0.005 | moderate, significant |
| KOOS–QoL vs. objective ICRS | –0.377 * | 0.013 | moderate, significant |
| KOOS–ADL vs. objective ICRS | –0.249 | 0.107 | weak, not significant |
| KOOS–Sport vs. objective ICRS | –0.198 | 0.209 | weak, not significant |
| Subjective IKDC vs. objective ICRS | –0.305 * | 0.028 | moderate, significant |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Heinz, T.; Wegerich, N.; Frischholz, S.; Stratos, I.; Horas, K.; Reppenhagen, S.; Rudert, M.; Weißenberger, M. Bridging the Gap: Do Patient-Reported Outcome Measures Reflect Objective Knee Function After Cartilage Repair? J. Clin. Med. 2025, 14, 7895. https://doi.org/10.3390/jcm14227895
Heinz T, Wegerich N, Frischholz S, Stratos I, Horas K, Reppenhagen S, Rudert M, Weißenberger M. Bridging the Gap: Do Patient-Reported Outcome Measures Reflect Objective Knee Function After Cartilage Repair? Journal of Clinical Medicine. 2025; 14(22):7895. https://doi.org/10.3390/jcm14227895
Chicago/Turabian StyleHeinz, Tizian, Niklas Wegerich, Sebastian Frischholz, Ioannis Stratos, Konstantin Horas, Stephan Reppenhagen, Maximilian Rudert, and Manuel Weißenberger. 2025. "Bridging the Gap: Do Patient-Reported Outcome Measures Reflect Objective Knee Function After Cartilage Repair?" Journal of Clinical Medicine 14, no. 22: 7895. https://doi.org/10.3390/jcm14227895
APA StyleHeinz, T., Wegerich, N., Frischholz, S., Stratos, I., Horas, K., Reppenhagen, S., Rudert, M., & Weißenberger, M. (2025). Bridging the Gap: Do Patient-Reported Outcome Measures Reflect Objective Knee Function After Cartilage Repair? Journal of Clinical Medicine, 14(22), 7895. https://doi.org/10.3390/jcm14227895








