Mobile Versus Fixed-Bearing in Medial Unicompartmental Knee Arthroplasty: An Average 10-Year Follow-Up
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
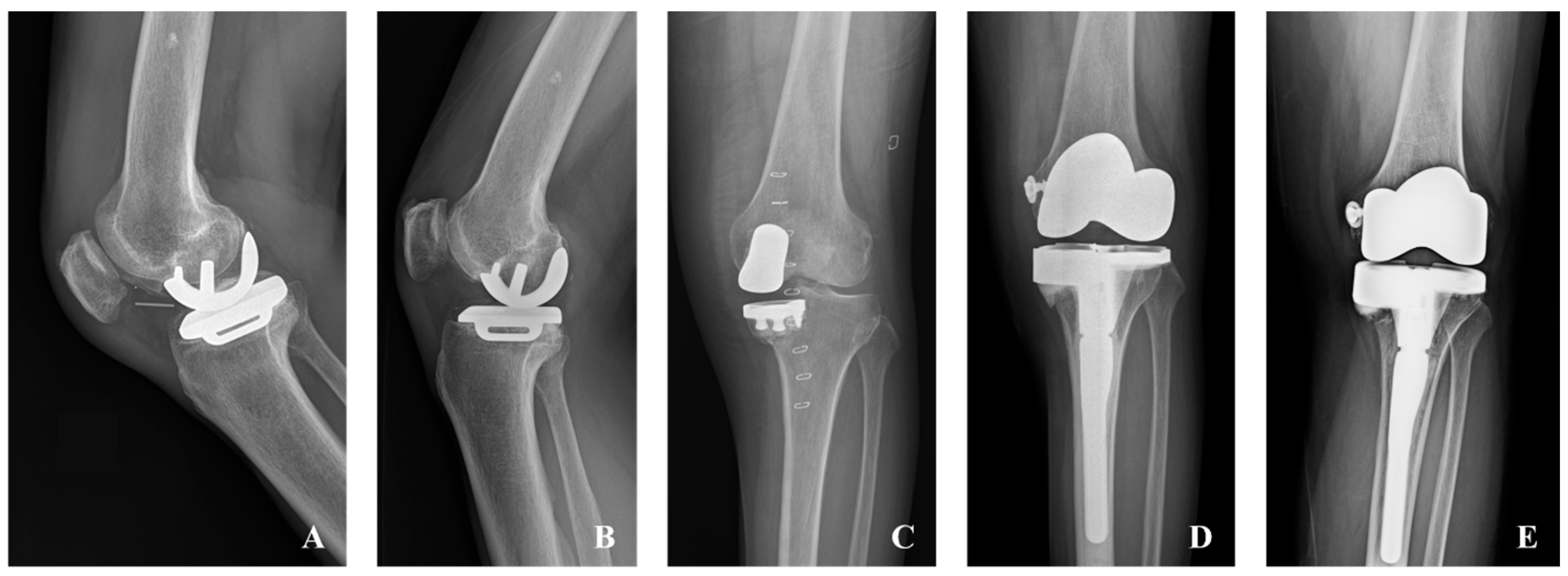
2.2. Surgical Treatment
2.3. Outcomes
2.4. Statistical Analyses
2.5. Intraobserver and Interobserver Reliability
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Dhanjani, S.A.; Schmerler, J.; Hussain, N.; Badin, D.; Srikumaran, U.; Hegde, V.; Oni, J.K. Racial, socioeconomic, and payer status disparities in utilization of unicompartmental knee arthroplasty in the USA. Knee Surg. Relat. Res. 2025, 37, 2. [Google Scholar] [CrossRef] [PubMed]
- Vasso, M.; Antoniadis, A.; Helmy, N. Update on unicompartmental knee arthroplasty: Current indications and failure modes. EFORT Open Rev. 2018, 3, 442–448. [Google Scholar] [CrossRef] [PubMed]
- Tay, M.L.; Bolam, S.M.; Maxwell, A.R.; Hooper, G.J.; Monk, A.P.; Young, S.W. Similar Survivorship but Different Revision Reasons for Uncemented Mobile-Bearing and Cemented Fixed-Bearing Medial UKA: A Long-Term Population-Based Cohort Study of 2015 Patients. J. Bone Jt. Surg. Am. 2023, 105, 755–761. [Google Scholar] [CrossRef] [PubMed]
- Moldovan, F.; Moldovan, L. A Modeling Study for Hip Fracture Rates in Romania. J. Clin. Med. 2025, 14, 3162. [Google Scholar] [CrossRef]
- Mori, Y.; Tarasawa, K.; Tanaka, H.; Kamimura, M.; Harada, K.; Mori, N.; Fushimi, K.; Aizawa, T.; Fujimori, K. Thromboembolic and infectious complication risks in TKA and UKA: Evidence from a Japanese nationwide cohort. Knee Surg. Relat. Res. 2025, 37, 19. [Google Scholar] [CrossRef]
- Zhang, W.; Wang, J.; Li, H.; Wang, W.; George, D.M.; Huang, T. Fixed- versus mobile-bearing unicompartmental knee arthroplasty: A meta-analysis. Sci. Rep. 2020, 10, 19075. [Google Scholar] [CrossRef]
- Emerson, R.H., Jr.; Hansborough, T.; Reitman, R.D.; Rosenfeldt, W.; Higgins, L.L. Comparison of a mobile with a fixed-bearing unicompartmental knee implant. Clin. Orthop. Relat. Res. 2002, 404, 62–70. [Google Scholar] [CrossRef]
- Watrinet, J.; Berger, D.; Blum, P.; Fabritius, M.P.; Arnholdt, J.; Schipp, R.; Reng, W.; Reidler, P. Fractures in Oxford unicompartmental knee arthroplasty are associated with a decreased medial keel-cortex distance of the tibial implant. Knee Surg. Relat. Res. 2024, 36, 36. [Google Scholar] [CrossRef]
- D’Ambrosi, R.; Valli, F.; Nuara, A.; Mariani, I.; Di Feo, F.; Ursino, N.; Formica, M.; Mangiavini, L.; Hantes, M.; Migliorini, F. No difference in mobile and fixed bearing partial knee arthroplasty in octogenarians: A clinical trial. Eur. J. Orthop. Surg. Traumatol. 2023, 33, 3081–3088. [Google Scholar] [CrossRef]
- Kannan, A.; Lewis, P.L.; Dyer, C.; Jiranek, W.A.; McMahon, S. Do Fixed or Mobile Bearing Implants Have Better Survivorship in Medial Unicompartmental Knee Arthroplasty? A Study From the Australian Orthopaedic Association National Joint Replacement Registry. Clin. Orthop. Relat. Res. 2021, 479, 1548–1558. [Google Scholar] [CrossRef]
- Hariri, M.; Hauer, G.; Smolle, M.; Sadoghi, P.; Leithner, A.; Panzram, B.; Merle, C.; Renkawitz, T.; Walker, T. Mobile bearing versus fixed bearing medial unicompartmental knee replacement: An independent two center matched-pairs analysis. Arch. Orthop. Trauma Surg. 2023, 143, 3383–3389. [Google Scholar] [CrossRef]
- Cao, Z.; Niu, C.; Gong, C.; Sun, Y.; Xie, J.; Song, Y. Comparison of Fixed-Bearing and Mobile-Bearing Unicompartmental Knee Arthroplasty: A Systematic Review and Meta-Analysis. J. Arthroplast. 2019, 34, 3114–3123.e3. [Google Scholar] [CrossRef]
- Neufeld, M.E.; Albers, A.; Greidanus, N.V.; Garbuz, D.S.; Masri, B.A. A Comparison of Mobile and Fixed-Bearing Unicompartmental Knee Arthroplasty at a Minimum 10-Year Follow-up. J. Arthroplast. 2018, 33, 1713–1718. [Google Scholar] [CrossRef]
- Pronk, Y.; Paters, A.A.M.; Brinkman, J.M. No difference in patient satisfaction after mobile bearing or fixed bearing medial unicompartmental knee arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 2021, 29, 947–954. [Google Scholar] [CrossRef] [PubMed]
- Parratte, S.; Pauly, V.; Aubaniac, J.M.; Argenson, J.N. No long-term difference between fixed and mobile medial unicompartmental arthroplasty. Clin. Orthop. Relat. Res. 2012, 470, 61–68. [Google Scholar] [CrossRef] [PubMed]
- Peersman, G.; Stuyts, B.; Vandenlangenbergh, T.; Cartier, P.; Fennema, P. Fixed- versus mobile-bearing UKA: A systematic review and meta-analysis. Knee Surg. Sports Traumatol. Arthrosc. 2015, 23, 3296–3305. [Google Scholar] [CrossRef] [PubMed]
- Migliorini, F.; Maffulli, N.; Cuozzo, F.; Elsner, K.; Hildebrand, F.; Eschweiler, J.; Driessen, A. Mobile Bearing versus Fixed Bearing for Unicompartmental Arthroplasty in Monocompartmental Osteoarthritis of the Knee: A Meta-Analysis. J. Clin. Med. 2022, 11, 2837. [Google Scholar] [CrossRef]
- Huang, F.; Wu, D.; Chang, J.; Zhang, C.; Qin, K.; Liao, F.; Yin, Z. A Comparison of Mobile- and Fixed-Bearing Unicompartmental Knee Arthroplasties in the Treatment of Medial Knee Osteoarthritis: A Systematic Review and Meta-analysis of 1861 Patients. J. Knee Surg. 2021, 34, 434–443. [Google Scholar] [CrossRef]
- Liddle, A.D.; Pandit, H.; Judge, A.; Murray, D.W. Optimal usage of unicompartmental knee arthroplasty: A study of 41,986 cases from the National Joint Registry for England and Wales. Bone Jt. J. 2015, 97-B, 1506–1511. [Google Scholar] [CrossRef]
- Park, D.Y.; Park, K.H.; Jin, Y.J.; Yun, H.W.; Lee, J.M.; Chung, J.Y.; Park, J.Y.; Min, B.H.; Lim, S. Fixed-Bearing Unicompartmental Knee Arthroplasty in Tibia Vara Knees Results in Joint Surface Malalignment and Varus Joint Line Obliquity, but Does Not Affect Functional Outcomes at Greater Than 5 Years Follow-Up. J. Arthroplast. 2024, 39, 645–650. [Google Scholar] [CrossRef]
- Mclnnes, J.; Larson, M.G.; Daltroy, L.H.; Brown, T.; Fossel, A.H.; Eaton, H.M.; Shulman-Kirwan, B.; Steindorf, S.; Poss, R.; Liang, M.H. A controlled evaluation of continuous passive motion in patients undergoing total knee arthroplasty. JAMA 1992, 268, 1423–1428. [Google Scholar] [CrossRef]
- Ranawat, C.S.; Ranawat, A.S.; Mehta, A. Total knee arthroplasty rehabilitation protocol: Whatmakes the difference? J. Arthroplast. 2003, 18, 27–30. [Google Scholar] [CrossRef]
- Kellgren, J.H.; Lawrence, J.S. Radiological assessment of osteo-arthrosis. Ann. Rheum. Dis. 1957, 16, 494–502. [Google Scholar] [CrossRef] [PubMed]
- Hung, K.T.; Chen, C.C.; Lin, Y.C.; Lee, S.H.; Hu, C.C.; Chang, Y.H.; Hsieh, P.H.; Shih, H.N.; Chang, C.H. Survivorship of the fixed-bearing medial unicompartmental knee arthroplasty: Mean 14-year follow-up in a single medical center. BMC Musculoskelet. Disord. 2024, 25, 283. [Google Scholar] [CrossRef] [PubMed]
- Bruni, D.; Iacono, F.; Raspugli, G.; Zaffagnini, S.; Marcacci, M. Is unicompartmental arthroplasty an acceptable option for spontaneous osteonecrosis of the knee? Clin. Orthop. Relat. Res. 2012, 470, 1442–1451. [Google Scholar] [CrossRef] [PubMed]
- Berger, R.A.; Meneghini, R.M.; Jacobs, J.J.; Sheinkop, M.B.; Della Valle, C.J.; Rosenberg, A.G.; Galante, J.O. Results of unicompartmental knee arthroplasty at a minimum of ten years of follow-up. J. Bone Jt. Surg. Am. 2005, 87, 999–1006. [Google Scholar] [CrossRef]
- Koh, J.H.; Lim, S.; Park, J.Y.; Chung, J.Y.; Jin, Y.J.; Yun, H.W.; Noh, S.; Park, D.Y. Controlled posterior condylar milling technique for unicompartmental knee arthroplasty minimises tibia resection during gap balancing: Short-term clinical results. Knee Surg. Sports Traumatol. Arthrosc. 2024, 32, 499–508. [Google Scholar] [CrossRef]
- Slaven, S.E.; Cody, J.P.; Sershon, R.A.; Ho, H.; Hopper, R.H., Jr.; Fricka, K.B. The Impact of Coronal Alignment on Revision in Medial Fixed-Bearing Unicompartmental Knee Arthroplasty. J. Arthroplast. 2020, 35, 353–357. [Google Scholar] [CrossRef]
- Wang, Z.; Deng, W.; Shao, H.; Zhou, Y.; Yang, D.; Li, H. Predictors of a forgotten joint after medial fixed-bearing unicompartmental knee arthroplasty. Knee 2022, 37, 103–111. [Google Scholar] [CrossRef]
- Zuiderbaan, H.A.; van der List, J.P.; Chawla, H.; Khamaisy, S.; Thein, R.; Pearle, A.D. Predictors of Subjective Outcome After Medial Unicompartmental Knee Arthroplasty. J. Arthroplast. 2016, 31, 1453–1458. [Google Scholar] [CrossRef]
- Kim, S.J.; Postigo, R.; Koo, S.; Kim, J.H. Causes of revision following Oxford phase 3 unicompartmental knee arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 2014, 22, 1895–1901. [Google Scholar] [CrossRef]
- Sun, X.; Liu, P.; Lu, F.; Wang, W.; Guo, W.; Zhang, Q. Bearing dislocation of mobile bearing unicompartmental knee arthroplasty in East Asian countries: A systematic review with meta-analysis. J. Orthop. Surg. Res. 2021, 16, 28. [Google Scholar] [CrossRef]
- Kang, S.W.; Kim, K.T.; Hwang, Y.S.; Park, W.R.; Shin, J.K.; Song, M.H. Is Mobile-Bearing Medial Unicompartmental Knee Arthroplasty Appropriate for Asian Patients With the Risk of Bearing Dislocation? J. Arthroplast. 2020, 35, 1222–1227. [Google Scholar] [CrossRef] [PubMed]

| Total (n = 81) | Fixed (n = 45) | Mobile (n = 36) | p-Value | |
|---|---|---|---|---|
| Age (years) | 57.2 ± 6.4 | 57.5 ± 6.6 | 56.8 ± 6.2 | 0.596 |
| Follow-up period (months) | 127.0 ± 28.6 | 121.6 ± 27.0 | 133.9 ± 29.5 | 0.056 |
| Height (cm) | 158.2 ± 8.3 | 158.0 ± 8.3 | 158.5 ± 8.5 | 0.770 |
| Weight (kg) | 66.1 ± 10.4 | 65.8 ± 9.7 | 66.5 ± 11.3 | 0.753 |
| BMI (kg/m2) | 26.3 ± 3.1 | 26.3 ± 3.1 | 26.4 ± 3.1 | 0.945 |
| Sex (M/F) | 17/64 | 7/38 | 10/26 | 0.286 |
| Side (L/R) | 46/35 | 28/17 | 18/18 | 0.380 |
| Total (n = 77) | Fixed (n = 44) | Mobile (n = 33) | p-Value | Mean Difference [95% CI] | |
|---|---|---|---|---|---|
| ROM (°) (preoperative) | 145.5 ± 18.3 | 144.4 ± 22.2 | 146.8 ± 11.2 | 0.540 | 2.4 [−6.0, 10.8] |
| ROM (°) (postoperative) | 144.6 ± 13.6 | 143.4 ± 14.7 | 146.1 ± 12.0 | 0.386 | 2.7 [−3.4, 8.7] |
| ROM (°) (delta) | −0.9 ± 23.4 | −1.0 ± 27.6 | −0.8 ± 16.6 | 0.958 | 0.2 [−9.8, 10.4] |
| WOMAC score (postoperative) | 28.2 ± 20.8 | 27.6 ± 21.8 | 28.9 ± 19.7 | 0.791 | 1.3 [−8.3, 10.8] |
| Total (n = 77) | Fixed (n = 44) | Mobile (n = 33) | p-Value | |
|---|---|---|---|---|
| Contralateral K-L grade (Pre.) grade (0/1/2) | 8/52/17 | 5/31/8 | 3/21/9 | 0.628 |
| Contralateral K-L grade (Post.) grade (1/2/3/4) | 25/47/4/1 | 14/27/3/0 | 11/20/1/1 | 0.600 |
| Contralateral K-L grade (delta) grade (0/1/2) | 32/41/4 | 16/26/2 | 16/15/2 | 0.495 |
| PFJ K-L grade (Pre.) grade (0/1/2) | 7/46/24 | 5/29/10 | 2/17/14 | 0.167 |
| PFJ K-L grade (Post.) grade (1/2/3/4) | 1/34/38/4 | 0/23/18/3 | 1/11/20/1 | 0.182 |
| PFJ K-L grade (delta) grade (0/1/2) | 50/26/1 | 26/17/1 | 24/9/0 | 0.366 |
| HKA (°) (Pre.) | 173.1 ± 4.3 | 173.0 ± 4.6 | 173.2 ± 4.0 | 0.795 |
| HKA (°) (Post.) | 174.6 ± 4.9 | 174.1 ± 5.1 | 175.1 ± 4.6 | 0.378 |
| HKA (°) (delta) | 1.5 ± 3.8 | 1.2 ± 3.9 | 1.9 ± 3.9 | 0.417 |
| Total (n = 81) | Fixed (n = 45) | Mobile (n = 36) | p-Value | |
|---|---|---|---|---|
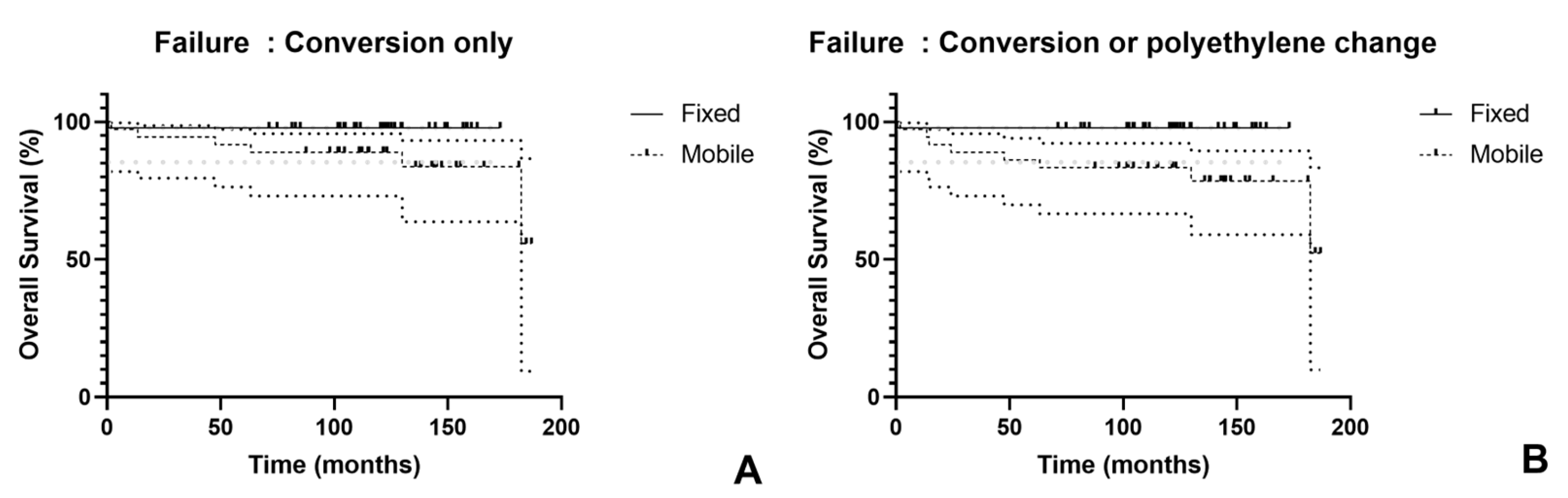
| Failure (TKA conversion) | 7 (8.6%) | 1 (2.2%) | 6 (16.7%) | 0.041 |
| Early/Late | 3/4 | 1/0 | 2/4 | |
| Failure (TKA conversion or PE exchange) | 9 (11.1%) | 1 (2.2%) | 8 (22.2%) | 0.009 |
| Early/Late | 4/5 | 1/0 | 3/5 |
| Authors | Year | Bearing | No. of Knees | Mean Follow-Up (Years) | Survivorship |
|---|---|---|---|---|---|
| Emerson et al. [7] | 2002 | FB | 51 | 7.7 | 11 years: 92% |
| MB | 50 | 6.8 | 11 years: 92% | ||
| Parratte et al. [15] | 2012 | FB | 79 | 17.2 | 20 years: 83% |
| MB | 77 | 17.2 | 20 years: 80% | ||
| Neufeld et al. [13] | 2018 | FB | 68 | 11.5 | 10 years: 90.9% |
| MB | 38 | 14.2 | 10 years: 82.9% | ||
| Tay et al. [3] | 2023 | FB | 450 | 7.0 | 15 years: 92% |
| MB | 496 | 11.3 | 15 years: 80% | ||
| Lim et al. (current study) | 2025 | FB | 45 | 10.1 | 10 years: 97.8% |
| MB | 36 | 11.2 | 10 years: 88.9% (conversion to TKA) 10 years: 83.3% (conversion to TKA + PE exchange) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lim, S.; Kim, T.H.; Park, D.Y.; Sunwoo, J.; Chung, J.Y. Mobile Versus Fixed-Bearing in Medial Unicompartmental Knee Arthroplasty: An Average 10-Year Follow-Up. J. Clin. Med. 2025, 14, 7144. https://doi.org/10.3390/jcm14207144
Lim S, Kim TH, Park DY, Sunwoo J, Chung JY. Mobile Versus Fixed-Bearing in Medial Unicompartmental Knee Arthroplasty: An Average 10-Year Follow-Up. Journal of Clinical Medicine. 2025; 14(20):7144. https://doi.org/10.3390/jcm14207144
Chicago/Turabian StyleLim, Sumin, Tae Hun Kim, Do Young Park, Jung Sunwoo, and Jun Young Chung. 2025. "Mobile Versus Fixed-Bearing in Medial Unicompartmental Knee Arthroplasty: An Average 10-Year Follow-Up" Journal of Clinical Medicine 14, no. 20: 7144. https://doi.org/10.3390/jcm14207144
APA StyleLim, S., Kim, T. H., Park, D. Y., Sunwoo, J., & Chung, J. Y. (2025). Mobile Versus Fixed-Bearing in Medial Unicompartmental Knee Arthroplasty: An Average 10-Year Follow-Up. Journal of Clinical Medicine, 14(20), 7144. https://doi.org/10.3390/jcm14207144






