V-Notes Sentinel Lymph Node Staging for Endometrial Cancer: A Systematic Review
Abstract
1. Introduction
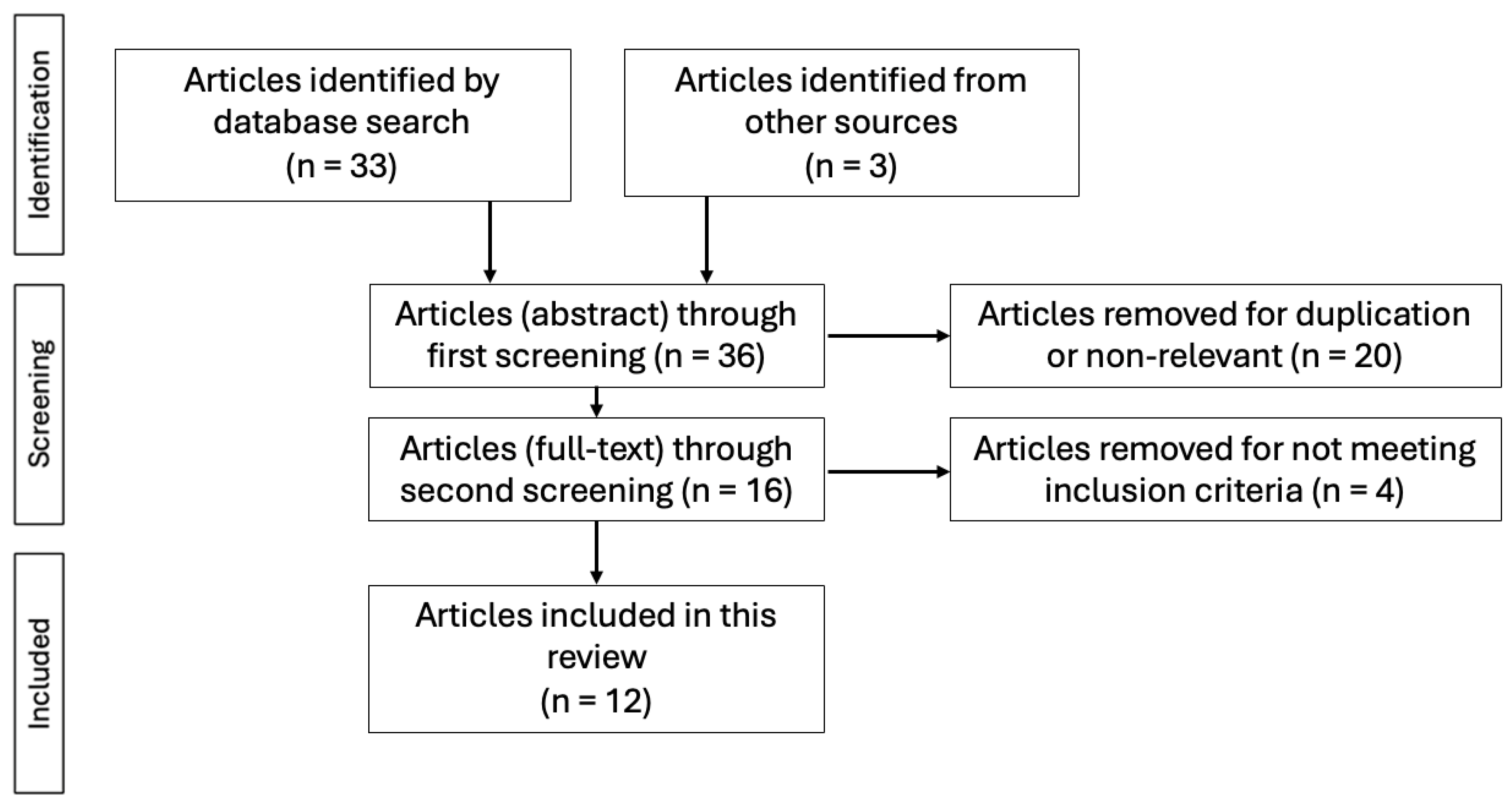
2. Materials and Methods
- Eligibility Criteria
- Study design: Original articles including case studies, observational studies and randomised trials.
- Method: Studies that involved performing the sentinel node mapping using the V-NOTES technique.
- Human involvement.
- Language: Studies published in English.
- Full text availability.
- Information Sources and Search Strategy
- Study Selection
- Data Extraction
3. Results
3.1. Characteristics of the Studies Included
3.2. Characteristics of the Population Included
3.3. Histological and Imaging Characteristics
3.4. Surgical Outcomes
3.5. SLN Mapping Outcomes
3.6. Complications and Follow-Up
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
Abbreviations
| V-NOTES | Vaginal Natural Orifice Transluminal Endoscopic Surgery |
| SLN | Sentinel Lymph Node |
| ICG | Indocyanine green |
References
- Oaknin, A.; Bosse, T.J.; Creutzberg, C.L.; Giornelli, G.; Harter, P.; Joly, F.; Lorusso, D.; Marth, C.; Makker, V.; Mirza, M.R.; et al. Endometrial Cancer: ESMO Clinical Practice Guideline for Diagnosis, Treatment and Follow-Up. Ann. Oncol. 2022, 33, 860–877. [Google Scholar] [CrossRef]
- Li, C.; Hua, K. Transvaginal Natural Orifice Transluminal Endoscopic Surgery (vNOTES) in Gynecologic Surgeries: A Systematic Review. Asian J. Surg. 2020, 43, 44–51. [Google Scholar] [CrossRef]
- Marchand, G.J.; Masoud, A.T.; Ulibarri, H.; Arroyo, A.; Moir, C.; Blanco, M.; Herrera, D.G.; Hamilton, B.; Ruffley, K.; Petersen, M.; et al. Systematic Review and Meta-Analysis of Vaginal Natural Orifice Transluminal Endoscopic Surgery vs Laparoscopic Hysterectomy. AJOG Glob. Rep. 2024, 4, 100320. [Google Scholar] [CrossRef]
- Benton-Bryant, C.; Pour, N.R.; Baekelandt, J.; Elhindi, J.; Ekanyake, K.; Kapurubandara, S. Transvaginal Natural Orifice Transluminal Endoscopic Surgery (vNOTES) in Benign Gynaecology: A Systematic Review of Adnexal, Myomectomy and Prolapse Procedures. J. Minim. Invasive Gynecol. 2025, 32, 318–351.e2. [Google Scholar] [CrossRef]
- Bouchez, M.-C.; Delporte, V.; Delplanque, S.; Leroy, M.; Vandendriessche, D.; Rubod, C.; Cosson, M.; Giraudet, G. vNOTES Hysterectomy: What about Obese Patients? J. Minim. Invasive Gynecol. 2023, 30, 569–575. [Google Scholar] [CrossRef]
- Leblanc, E.; Narducci, F.; Bresson, L.; Hudry, D. Fluorescence-Assisted Sentinel (SND) and Pelvic Node Dissections by Single-Port Transvaginal Laparoscopic Surgery, for the Management of an Endometrial Carcinoma (EC) in an Elderly Obese Patient. Gynecol. Oncol. 2016, 143, 686–687. [Google Scholar] [CrossRef]
- Ferro, R.; Hurni, Y.; Seidler, S.; Huber, D. Transvaginal Natural Orifice Transluminal Endoscopic Surgery (vNOTES) in Gynecological Emergencies. Eur. J. Obstet. Gynecol. Reprod. Biol. X 2023, 20, 100261. [Google Scholar] [CrossRef]
- Baekelandt, J.F. New Retroperitoneal Transvaginal Natural Orifice Transluminal Endoscopic Surgery Approach to Sentinel Node for Endometrial Cancer: A Demonstration Video. J. Minim. Invasive Gynecol. 2019, 26, 1231–1232. [Google Scholar] [CrossRef]
- Ottawa Hospital Research Institute. Available online: https://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (accessed on 10 July 2025).
- JBI Critical Appraisal Tools | JBI. Available online: https://jbi.global/critical-appraisal-tools (accessed on 10 July 2025).
- Baekelandt, J.; Jespers, A.; Huber, D.; Badiglian-Filho, L.; Stuart, A.; Chuang, L.; Ali, O.; Burnett, A. vNOTES Retroperitoneal Sentinel Lymph Node Dissection for Endometrial Cancer Staging: First Multicenter, Prospective Case Series. Acta Obs. Gynecol. Scand. 2024, 103, 1311–1317. [Google Scholar] [CrossRef]
- Comba, C.; Karakas, S.; Erdogan, S.V.; Demir, O.; Şimşek, E.; Karasabanoglu, F.; Demirayak, G.; Ozdemir, I.A. Transvaginal Natural Orifice Transluminal Endoscopic Surgery (VNOTES) Retroperitoneal Sentinel Lymph Node BIOPSY Compared with Conventional Laparoscopy in Patients with Endometrial Cancer. Surg. Oncol. 2024, 55, 102099. [Google Scholar] [CrossRef]
- Comba, C.; Demirayak, G.; Simsek, C.; Atas, B.S.; Özdemir, İ.A. Transvaginal Natural Orifice Transluminal Endoscopic Surgery (VNOTES) Total Retroperitoneal Sentinel Lymph Node Biopsy for an Endometrial Cancer Patient with Prior Colon Cancer Surgery. Int. J. Gynecol. Cancer 2021, 31, 1386–1387. [Google Scholar] [CrossRef]
- Deng, L.; Liu, Y.; Yao, Y.; Deng, Y.; Tang, S.; Sun, L.; Wang, Y. Efficacy of Vaginal Natural Orifice Transluminal Endoscopic Sentinel Lymph Node Biopsy for Endometrial Cancer: A Prospective Multicenter Cohort Study. Int. J. Surg. 2023, 109, 2996–3002. [Google Scholar] [CrossRef]
- Huber, D.; Hurni, Y. Sentinel Node Biopsy for Endometrial Cancer by Retroperitoneal Transvaginal Natural Orifice Transluminal Endoscopic Surgery: A Preliminary Study. Front. Surg. 2022, 9, 907548. [Google Scholar] [CrossRef]
- Huber, D.; Hurni, Y. Anatomical Distribution of Sentinel Lymph Nodes Harvested by Retroperitoneal vNOTES in 34 Consecutive Patients With Early-Stage Endometrial Cancer: Analysis of 124 Lymph Nodes. J. Minim. Invasive Gynecol. 2024, 31, 438–444. [Google Scholar] [CrossRef]
- Lee, C.-L.; Liu, H.-M.; Khan, S.; Lee, P.-S.; Huang, K.-G.; Yen, C.-F. Vaginal Natural Orifice Transvaginal Endoscopic Surgery (vNOTES) Surgical Staging for Endometrial Carcinoma: The Feasibility of an Innovative Approach. Taiwan. J. Obstet. Gynecol. 2022, 61, 345–352. [Google Scholar] [CrossRef]
- Matak, L.; Šimičević, M.; Dukić, B.; Matak, M.; Baekelandt, J. vNOTES Surgical Staging for Endometrial Carcinoma in Overweight Patients: A Case Series. Arch. Gynecol. Obstet. 2024, 309, 2829–2832. [Google Scholar] [CrossRef]
- Mathey, M.-P.; Romito, F.; Huber, D.E. Retroperitoneal Sentinel Lymph Node Biopsy by Vaginally Assisted Natural Orifices Endoscopic Transluminal Endoscopic Surgery in Early Stage Endometrial Cancer: Description of Technique and Surgeon’s Perspectives after the First Experience. Case Rep. Oncol. 2022, 15, 291–299. [Google Scholar] [CrossRef]
- Şimşek, E.; Yıldız, Ö.A.; Gündüz, S.; Karakaş, S.; Yaşar, L. vNOTES Scarless and Painless Endometrial Cancer Staging Surgery. J. Obs. Gynaecol. Res. 2024, 50, 1965–1970. [Google Scholar] [CrossRef]
- Tantitamit, T.; Lee, C.-L. Application of Sentinel Lymph Node Technique to Transvaginal Natural Orifices Transluminal Endoscopic Surgery in Endometrial Cancer. J. Minim. Invasive Gynecol. 2019, 26, 949–953. [Google Scholar] [CrossRef]
- Wang, Y.; Deng, L.; Tang, S.; Dou, Y.; Yao, Y.; Li, Y.; Deng, Y.; Chen, Y.; Liang, Z. vNOTES Hysterectomy with Sentinel Lymph Node Mapping for Endometrial Cancer: Description of Technique and Perioperative Outcomes. J. Minim. Invasive Gynecol. 2021, 28, 1254–1261. [Google Scholar] [CrossRef]
- Onstad, M.A.; Schmandt, R.E.; Lu, K.H. Addressing the Role of Obesity in Endometrial Cancer Risk, Prevention, and Treatment. J. Clin. Oncol. 2016, 34, 4225–4230. [Google Scholar] [CrossRef]
- Wang, F.; Liu, Y.; Xing, Y.; Wang, D.; Bai, X.; Li, L.; Ma, C.; Sun, Y.; Bai, Y.; Wang, L. Clinical Efficacy and Safety Study of vNOTES for Benign Ovarian Tumors in Obese Patients. Sci. Rep. 2025, 15, 4609. [Google Scholar] [CrossRef]
- Kapurubandara, S.; Lowenstein, L.; Salvay, H.; Herijgers, A.; King, J.; Baekelandt, J. Consensus on Safe Implementation of Vaginal Natural Orifice Transluminal Endoscopic Surgery (vNOTES). Eur. J. Obstet. Gynecol. Reprod. Biol. 2021, 263, 216–222. [Google Scholar] [CrossRef]
- Concin, N.; Matias-Guiu, X.; Vergote, I.; Cibula, D.; Mirza, M.R.; Marnitz, S.; Ledermann, J.; Bosse, T.; Chargari, C.; Fagotti, A.; et al. ESGO/ESTRO/ESP Guidelines for the Management of Patients with Endometrial Carcinoma. Int. J. Gynecol. Cancer 2021, 31, 12–39. [Google Scholar] [CrossRef]
- Hurni, Y.; Romito, F.; Huber, D. Transvaginal Natural Orifice Transluminal Endoscopic Surgery for Surgical Staging of Early-Stage Ovarian Cancers: A Report of Two Cases. Front. Surg. 2022, 9, 833126. [Google Scholar] [CrossRef]
- Kellerhals, G.; Nef, J.; Hurni, Y.; Huber, D. Transvaginal Natural Orifice Transluminal Endoscopic Surgery for Early-Stage Ovarian Cancer and Borderline Ovarian Tumors: A Case Series. Front. Surg. 2025, 12, 1542486. [Google Scholar] [CrossRef]
- Hurni, Y.; Huber, D.E. Sentinel Node Biopsy by Transvaginal Natural Orifice Transluminal Endoscopic Surgery in a Patient with Early-Stage Cervical Cancer: A Case Report. Case Rep. Oncol. 2022, 15, 547–552. [Google Scholar] [CrossRef]
- Holloway, R.W.; Abu-Rustum, N.R.; Backes, F.J.; Boggess, J.F.; Gotlieb, W.H.; Jeffrey Lowery, W.; Rossi, E.C.; Tanner, E.J.; Wolsky, R.J. Sentinel Lymph Node Mapping and Staging in Endometrial Cancer: A Society of Gynecologic Oncology Literature Review with Consensus Recommendations. Gynecol. Oncol. 2017, 146, 405–415. [Google Scholar] [CrossRef]
- Zhang, Q.; Dong, W.; Huang, B.; Xie, A.; Gong, Z.; Feng, D.; He, L.; Lin, Y. Analysis of the Learning Curve for Transvaginal Natural Orifice Transluminal Endoscopic Surgery in Ovarian Cystectomy. Front. Med. 2025, 12, 1629418. [Google Scholar] [CrossRef]
- Charles, F.; Luyckx, M.; Dubois, N. The Learning Curve of V-NOTES Hysterectomy: A Single-Surgeon Experience. Front. Med. 2025, 12, 1574457. [Google Scholar] [CrossRef]
- Restaino, S.; Buda, A.; Puppo, A.; Capozzi, V.A.; Sozzi, G.; Casarin, J.; Gallitelli, V.; Murgia, F.; Vizzielli, G.; Baroni, A.; et al. Anatomical Distribution of Sentinel Lymph Nodes in Patients with Endometrial Cancer: A Multicenter Study. Int. J. Gynecol. Cancer 2022, 32, 517–524. [Google Scholar] [CrossRef] [PubMed]
- Sozzi, G.; Fanfani, F.; Berretta, R.; Capozzi, V.A.; Uccella, S.; Buono, N.; Giallombardo, V.; Di Donna, M.C.; Monterossi, G.; Restaino, S.; et al. Laparoscopic Sentinel Node Mapping with Intracervical Indocyanine Green Injection for Endometrial Cancer: The SENTIFAIL Study—A Multicentric Analysis of Predictors of Failed Mapping. Int. J. Gynecol. Cancer 2020, 30, 1713–1718. [Google Scholar] [CrossRef] [PubMed]
- Laufer, J.; Scasso, S.; Papadia, A. Different Tracers for Sentinel Node Detection in Gynecologic Oncology. Curr. Opin. Oncol. 2024, 36, 371–375. [Google Scholar] [CrossRef]
- Hou, Q.; Li, X.; Li, Y.; Zhang, Q.; Liu, T.; Huang, L.; Gong, Z.; Feng, D.; Gu, D.; Lin, Y.; et al. Analysis and Suggestions on the Complications in 2000 Cases of Transvaginal Natural Orifice Transluminal Endoscopic Surgery: Can It Be a Conventional Surgery? Int. J. Gynecol. Obstet. 2024, 164, 541–549. [Google Scholar] [CrossRef]
- DeNardis, S.A.; Holloway, R.W.; Bigsby, G.E.; Pikaart, D.P.; Ahmad, S.; Finkler, N.J. Robotically Assisted Laparoscopic Hysterectomy versus Total Abdominal Hysterectomy and Lymphadenectomy for Endometrial Cancer. Gynecol. Oncol. 2008, 111, 412–417. [Google Scholar] [CrossRef]
- Kaya, A.C.; Radosa, M.P.; Zimmermann, J.S.M.; Stotz, L.; Findeklee, S.; Hamza, A.; Sklavounos, P.; Takacs, F.Z.; Wagenpfeil, G.; Radosa, C.G.; et al. Intraoperative and Postoperative Complications of Gynecological Laparoscopic Interventions: Incidence and Risk Factors. Arch. Gynecol. Obstet. 2021, 304, 1259–1269. [Google Scholar] [CrossRef]
- Pickett, C.M.; Seeratan, D.D.; Mol, B.W.J.; Nieboer, T.E.; Johnson, N.; Bonestroo, T.; Aarts, J.W. Surgical Approach to Hysterectomy for Benign Gynaecological Disease. Cochrane Database Syst. Rev. 2023, 2023, CD003677. [Google Scholar] [CrossRef]
| Author | Year | Design | Patients | Mean Age | Mean BMI (kg/m2) | >25 kg/m2 (%) | Mean Parity | Prior Surgery (%) |
|---|---|---|---|---|---|---|---|---|
| Baekeland [11] | 2024 | Case series | 64 | 69.5 | 26 | 34 | - | 38 |
| Comba [12] | 2024 | Cohort | 19 | 59.4 | 29 | 100 | 2 | - |
| Comba [13] | 2021 | Case report | 1 | 46 | 27.4 | 100 | 2 | 100 |
| Deng [14] | 2023 | Cohort | 57 | 51.46 | 26.25 | 78.95 | 2 | 31.58 |
| Huber [15] | 2022 | Case series | 7 | 68 | 26.4 | 57 | 2.2 | 57 |
| Huber [16] | 2024 | Case series | 34 | 68 | 27.3 | - | - | 58.8 |
| Lee [17] | 2022 | Case series | 15 | 52.8 | 27.8 | 26 | 1.8 | 26 |
| Matak [18] | 2024 | Case series | 4 | 67 | 28.45 | 100 | 2 | 25 |
| Mathey [19] | 2022 | Case report | 1 | 64 | - | - | - | - |
| Simsek [20] | 2024 | Case series | 24 | 56.5 | 31 | - | - | 67 |
| Tantitamit [21] | 2018 | Case series | 4 | 60.3 | 25.6 | 75 | 3.2 | 50 |
| Wang [22] | 2021 | Cohort | 23 | 53 | 24.2 | - | 2 | 34 |
| Author | Year | Tumour Histology | Tumour Grading | Imaging (US/MRI) | Staging |
|---|---|---|---|---|---|
| Baekeland [11] | 2024 | All types and Complex Atypical Hyperplasia | 1–3 | No | I-II |
| Comba [12] | 2024 | - | - | Yes | - |
| Comba [13] | 2021 | Endometrioid | 2 | Yes | I |
| Deng [14] | 2023 | Endometrioid | - | Yes | I |
| Huber [15] | 2022 | Endometrioid and Complex Atypical Hyperplasia | 1–2 | Yes | I |
| Huber [16] | 2024 | Endometrioid and Complex Atypical Hyperplasia | - | Yes | I |
| Lee [17] | 2022 | Endometrioid | 1–2 | Yes | I |
| Matak [18] | 2024 | Endometrioid | 1 | No | I |
| Mathey [19] | 2022 | Endometrioid | 1 | Yes | I |
| Simsek [20] | 2024 | - | - | Yes | - |
| Tantitamit [21] | 2018 | - | - | No | I |
| Wang [22] | 2021 | Endometrioid | 1–2 | Yes | I |
| Author | Year | SLN Approach | Tracer | Mean op. Time | Estimated Blood Loss (mL) | Pre-op-Post-op HB (g/dL) |
|---|---|---|---|---|---|---|
| Baekeland [11] | 2024 | Retroperitoneal | ICG | 126 | 80 | −1 |
| Comba [12] | 2024 | Retroperitoneal | ICG | 208.4 | 76.3 | −1.5 |
| Comba [13] | 2021 | Retroperitoneal | ICG | 180 | 20 | - |
| Deng [14] | 2023 | Transperitoneal | ICG, CNP | 132.35 | 75 | - |
| Huber [15] | 2022 | Retroperitoneal | ICG | 113 | 20 | - |
| Huber [16] | 2024 | Retroperitoneal | ICG | - | - | - |
| Lee [17] | 2022 | Transperitoneal | ICG | 231.4 | 122 | −1.44 |
| Matak [18] | 2024 | Retroperitoneal | ICG | 169 | - | −1.9 |
| Mathey [19] | 2022 | Retroperitoneal | ICG | 113 | 100 | - |
| Simsek [20] | 2024 | Retroperitoneal | ICG | 125 | 70 | - |
| Tantitamit [21] | 2018 | Transperitoneal | ICG | 182.7 | 67 | −0.57 |
| Wang [22] | 2021 | Transperitoneal | CNP | 132.3 | 90 | −1 |
| Author | Year | Succes Rate (%) | Total LN | Mean Right LN | Mean Left LN | Overall DR (%) | Bilateral DR (%) | Unilateral DR (%) |
|---|---|---|---|---|---|---|---|---|
| Baekeland [11] | 2024 | 98.5 | 3 | - | - | 100 | 97 | 3 |
| Comba [12] | 2024 | 94.8 | - | - | - | 94.8 | - | - |
| Comba [13] | 2021 | 100 | - | - | - | 100 | - | - |
| Deng [14] | 2023 | 81.5 | - | - | - | 94.7 | 82.4 | 12.3 |
| Huber [15] | 2022 | 100 | 3.1 | 1.2 | 1.8 | 100 | 100 | - |
| Huber [16] | 2024 | 91.2 | 3 | 1 | 1 | 97.1 | 91.2 | 5.9 |
| Lee [17] | 2022 | 100 | 5.3 | 2.3 | 1.9 | 100 | - | - |
| Matak [18] | 2024 | 100 | 12.5 | 5.7 | 6.2 | 100 | - | - |
| Mathey [19] | 2022 | 100 | 3 | 1 | 2 | 100 | 100 | - |
| Simsek [20] | 2024 | 96 | 2 | 1 | 1 | 96 | 91 | 4 |
| Tantitamit [21] | 2018 | 100 | 8.5 | 5 | 2.5 | 100 | 100 | - |
| Wang [22] | 2021 | 95.7 | 5 | - | - | 95.7 | 87 | 8.7 |
| Characteristic | Retroperitoneal V-NOTES | Transperitoneal V-NOTES |
|---|---|---|
| Access Route | Via retroperitoneal space, avoiding the peritoneal cavity | Through the peritoneal cavity from the vaginal canal |
| Peritoneum Penetration | Not penetrated | Penetrated to access abdominal cavity |
| Visualization | Limited, more challenging anatomy orientation | Excellent visualization of intra-abdominal structures |
| Risk of Intraperitoneal Injury | Lower | Higher (bowel, bladder, vessels) |
| Adhesion Risk | Reduced | Possible if adhesions present |
| Suitable For | Select procedures (e.g., lymphadenectomy, small masses) | Broader range of gynecologic surgeries (e.g., hysterectomy) |
| Learning Curve | Steeper due to complex anatomy | Less steep, similar to standard laparoscopy |
| CO2 Insufflation | Confined to retroperitoneum | Fills the peritoneal cavity |
| Postoperative Recovery | Potentially faster and less pain | Slightly more discomfort due to peritoneal irritation |
| Preferred When | Avoiding peritoneal contamination or minimizing invasiveness | When broader access is needed or for complex procedures |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nădăban, M.; Balint, O.; Secoșan, C.; Furău, A.M.; Olaru, F.; Pirtea, L. V-Notes Sentinel Lymph Node Staging for Endometrial Cancer: A Systematic Review. J. Clin. Med. 2025, 14, 6451. https://doi.org/10.3390/jcm14186451
Nădăban M, Balint O, Secoșan C, Furău AM, Olaru F, Pirtea L. V-Notes Sentinel Lymph Node Staging for Endometrial Cancer: A Systematic Review. Journal of Clinical Medicine. 2025; 14(18):6451. https://doi.org/10.3390/jcm14186451
Chicago/Turabian StyleNădăban, Mihai, Oana Balint, Cristina Secoșan, Alexandru Marius Furău, Flavius Olaru, and Laurențiu Pirtea. 2025. "V-Notes Sentinel Lymph Node Staging for Endometrial Cancer: A Systematic Review" Journal of Clinical Medicine 14, no. 18: 6451. https://doi.org/10.3390/jcm14186451
APA StyleNădăban, M., Balint, O., Secoșan, C., Furău, A. M., Olaru, F., & Pirtea, L. (2025). V-Notes Sentinel Lymph Node Staging for Endometrial Cancer: A Systematic Review. Journal of Clinical Medicine, 14(18), 6451. https://doi.org/10.3390/jcm14186451







