Comparison of Perioperative Outcomes for Prostate Artery Embolization Versus Transurethral Resection of the Prostate and Laser Enucleation for Benign Prostatic Hyperplasia: Results from the GRAND Study
Abstract
1. Introduction
2. Methods
2.1. GeRmAn Nationwide Inpatient Data (GRAND)
2.2. Data Source
2.3. Statistical Analysis
3. Results
3.1. Baseline Characteristics
3.2. Perioperative Outcomes
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Xiang, P.; Guan, D.; Du, Z.; Hao, Y.; Yan, W.; Wang, Y.; Liu, Y.; Liu, D.; Ping, H. Efficacy and safety of prostatic artery embolization for benign prostatic hyperplasia: A systematic review and meta-analysis of randomized controlled trials. Eur. Radiol. 2021, 31, 4929–4946. [Google Scholar] [CrossRef] [PubMed]
- Zumstein, V.; Betschart, P.; Vetterlein, M.W.; Kluth, L.A.; Hechelhammer, L.; Mordasini, L.; Engeler, D.S.; Kessler, T.M.; Schmid, H.-P.; Abt, D. Prostatic Artery Embolization versus Standard Surgical Treatment for Lower Urinary Tract Symptoms Secondary to Benign Prostatic Hyperplasia: A Systematic Review and Meta-analysis. Eur. Urol. Focus 2019, 5, 1091–1100. [Google Scholar] [CrossRef] [PubMed]
- Wang, M.Q.; Guo, L.P.; Zhang, G.D.; Yuan, K.; Li, K.; Duan, F.; Yan, J.Y.; Wang, Y.; Kang, H.Y.; Wang, Z.J. Prostatic arterial embolization for the treatment of lower urinary tract symptoms due to large (>80 mL) benign prostatic hyperplasia: Results of midterm follow-up from Chinese population. BMC Urol. 2015, 15, 33. [Google Scholar] [CrossRef] [PubMed]
- Bhatia, A.; Porto, J.G.; Maini, A.; Langade, D.; Herrmann, T.R.W.; Shah, H.N.; Bhatia, S. One-year outcomes after prostate artery embolization versus laser enucleation: A network meta-analysis. BJUI Compass 2024, 5, 189–206. [Google Scholar] [CrossRef]
- Sandhu, J.S.; Bixler, B.R.; Dahm, P.; Goueli, R.; Kirkby, E.; Stoffel, J.T.; Wilt, T.J. Management of Lower Urinary Tract Symptoms Attributed to Benign Prostatic Hyperplasia (BPH): AUA Guideline Amendment 2023. J. Urol. 2024, 211, 11–19. [Google Scholar] [CrossRef]
- Gravas, S.; Gacci, M.; Gratzke, C.; Herrmann, T.R.W.; Karavitakis, M.; Kyriazis, I.; Malde, S.; Mamoulakis, C.; Rieken, M.; Sakalis, V.I.; et al. Summary Paper on the 2023 European Association of Urology Guidelines on the Management of Non-neurogenic Male Lower Urinary Tract Symptoms. Eur. Urol. 2023, 84, 207–222. [Google Scholar] [CrossRef]
- Sokolakis, I.; Pyrgidis, N.; Russo, G.I.; Sountoulides, P.; Hatzichristodoulou, G. Preserving Ejaculation: A Guide Through the Landscape of Interventional and Surgical Options for Benign Prostatic Obstruction. Eur. Urol. Focus 2022, 8, 380–383. [Google Scholar] [CrossRef]
- Carnevale, F.C.; de Assis, A.M.; Moreira, A.M. Prostatic Artery Embolization: Equipment, Procedure Steps, and Overcoming Technical Challenges. Tech. Vasc. Interv. Radiol. 2020, 23, 100691. [Google Scholar] [CrossRef]
- Powell, T.; Rahman, S.; Staib, L.; Bhatia, S.; Ayyagari, R. Operator Learning Curve for Prostatic Artery Embolization and Its Impact on Outcomes in 296 Patients. Cardiovasc. Interv. Radiol. 2023, 46, 229–237. [Google Scholar] [CrossRef]
- Geevarghese, R.; Harding, J.; Parsons, N.; Hutchinson, C.; Parsons, C. The relationship of embolic particle size to patient outcomes in prostate artery embolisation for benign prostatic hyperplasia: A systematic review and meta-regression. Clin. Radiol. 2020, 75, 366–374. [Google Scholar] [CrossRef]
- Delgal, A.; Cercueil, J.-P.; Koutlidis, N.; Michel, F.; Kermarrec, I.; Mourey, E.; Cormier, L.; Krausé, D.; Loffroy, R. Outcome of transcatheter arterial embolization for bladder and prostate hemorrhage. J. Urol. 2010, 183, 1947–1953. [Google Scholar] [CrossRef]
- Jung, J.H.; McCutcheon, K.A.; Borofsky, M.; Young, S.; Golzarian, J.; Kim, M.H.; Narayan, V.; Dahm, P. Prostatic arterial embolisation for men with benign prostatic hyperplasia: A Cochrane review. BJU Int. 2023, 131, 32–45. [Google Scholar] [CrossRef]
- Pyrgidis, N.; Schulz, G.B.; Weinhold, P.; Atzler, M.; Stadelmeier, L.F.; Papadopoulos, I.; Stief, C.; Marcon, J.; Keller, P. Perioperative outcomes of HoLEP, ThuLEP, and TURP in patients with prostate cancer: Results from the GRAND study. Prostate Cancer Prostatic Dis. 2025, 1–6. [Google Scholar] [CrossRef]
- Müllhaupt, G.; Hechelhammer, L.; Engeler, D.S.; Güsewell, S.; Betschart, P.; Zumstein, V.; Kessler, T.M.; Schmid, H.; Mordasini, L.; Abt, D. In-hospital cost analysis of prostatic artery embolization compared with transurethral resection of the prostate: Post hoc analysis of a randomized controlled trial. BJU Int. 2019, 123, 1055–1060. [Google Scholar] [CrossRef]
- Campos-Juanatey, F.; Osman, N.I.; Greenwell, T.; Martins, F.E.; Riechardt, S.; Waterloos, M.; Barratt, R.; Chan, G.; Esperto, F.; Ploumidis, A.; et al. European Association of Urology Guidelines on Urethral Stricture Disease (Part 2): Diagnosis, Perioperative Management, and Follow-up in Males. Eur. Urol. 2021, 80, 201–212. [Google Scholar] [CrossRef] [PubMed]
- Franco, J.V.; Jung, J.H.; Imamura, M.; Borofsky, M.; Omar, M.I.; Escobar Liquitay, C.M.; Young, S.; Golzarian, J.; Veroniki, A.A.; Garegnani, L.; et al. Minimally invasive treatments for lower urinary tract symptoms in men with benign prostatic hyperplasia: A network meta-analysis. Cochrane Database Syst. Rev. 2021, 7, CD013656. [Google Scholar] [CrossRef] [PubMed]
- Pisco, J.M.; Rio Tinto, H.; Campos Pinheiro, L.; Bilhim, T.; Duarte, M.; Fernandes, L.; Pereira, J.; Oliveira, A.G. Embolisation of prostatic arteries as treatment of moderate to severe lower urinary symptoms (LUTS) secondary to benign hyperplasia: Results of short- and mid-term follow-up. Eur. Radiol. 2013, 23, 2561–2572. [Google Scholar] [CrossRef] [PubMed]
- McClure, T.D.; Ricke, J. What Is New in Prostate Artery Embolization for Lower Urinary Tract Symptoms? Eur. Urol. Focus 2018, 4, 46–48. [Google Scholar] [CrossRef]
- Cornu, J.N.; Herrmann, T.; Traxer, O.; Matlaga, B. Prevention and Management Following Complications from Endourology Procedures. Eur. Urol. Focus 2016, 2, 49–59. [Google Scholar] [CrossRef]
- Malling, B.; Røder, M.A.; Brasso, K.; Forman, J.; Taudorf, M.; Lönn, L. Prostate artery embolisation for benign prostatic hyperplasia: A systematic review and meta-analysis. Eur. Radiol. 2019, 29, 287–298. [Google Scholar] [CrossRef]
- Marcon, J.; Keller, P.; Pyrgidis, N.; Atzler, M.; Kidess, M.; Götz, M.; Jokisch, J.-F.; Chaloupka, M.; Stief, C.G.; Schulz, G.B.; et al. Trends and Perioperative Outcomes of Surgical Treatments for Benign Prostatic Hyperplasia in Germany: Results from the GRAND Study. Eur. Urol. Focus 2025, S2405-4569(25)00002-1. [Google Scholar] [CrossRef]
- Huang, S.-W.; Tsai, C.-Y.; Tseng, C.-S.; Shih, M.-C.; Yeh, Y.-C.; Chien, K.-L.; Pu, Y.-S.; Tu, Y.-K. Comparative efficacy and safety of new surgical treatments for benign prostatic hyperplasia: Systematic review and network meta-analysis. BMJ 2019, 367, l5919. [Google Scholar] [CrossRef]
- Uhlig, A.; Baunacke, M.; Groeben, C.; Borkowetz, A.; Volkmer, B.; Ahyai, S.A.; Trojan, L.; Eisenmenger, N.; Schneider, A.; Thomas, C.; et al. Contemporary surgical management of benign prostatic obstruction in Germany: A population-wide study based on German hospital quality report data from 2006 to 2019. Die Urol. 2022, 61, 508–517. [Google Scholar] [CrossRef]
- Ditonno, F.; Manfredi, C.; Licari, L.C.; Bologna, E.; Franco, A.; Pandolfo, S.D.; De Sio, M.; De Nunzio, C.; Fiori, C.; Cherullo, E.E.; et al. Benign Prostatic Hyperplasia Surgery: A Snapshot of Trends, Costs, and Surgical Retreatment Rates in the USA. Eur. Urol. Focus 2024, 10, 826–832. [Google Scholar] [CrossRef] [PubMed]
- Daniels, J.P.; Patel, D.N.; Galvan, G.C.; Friedrich, N.A.; Das, S.; Akhavein, A.; Daskivich, T.; Josephson, D.; Desai, P.; De Nunzio, C.; et al. Investigating trends in interest for benign prostatic hyperplasia surgery options using Google Trends. Prostate Cancer Prostatic Dis. 2024, 27, 150–152. [Google Scholar] [CrossRef]
- Seizilles de Mazancourt, E.; Pagnoux, G.; Codas Duarte, R.; Moldovan, P.C.; Ruffion, A.; Colombel, M.; Badet, L.; Fassi-Fehri, H. Prostatic arterial embolization versus holmium laser enucleation of the prostate: 1-year outcomes. World J. Urol. 2023, 41, 151–157. [Google Scholar] [CrossRef]
- Abt, D.; Müllhaupt, G.; Hechelhammer, L.; Markart, S.; Güsewell, S.; Schmid, H.-P.; Mordasini, L.; Engeler, D.S. Prostatic Artery Embolisation Versus Transurethral Resection of the Prostate for Benign Prostatic Hyperplasia: 2-yr Outcomes of a Randomised, Open-label, Single-centre Trial. Eur. Urol. 2021, 80, 34–42. [Google Scholar] [CrossRef]
- Abt, D.; Hechelhammer, L.; Müllhaupt, G.; Markart, S.; Güsewell, S.; Kessler, T.M.; Schmid, H.-P.; Engeler, D.S.; Mordasini, L. Comparison of prostatic artery embolisation (PAE) versus transurethral resection of the prostate (TURP) for benign prostatic hyperplasia: Randomised, open label, non-inferiority trial. BMJ 2018, 361, k2338. [Google Scholar] [CrossRef]
- Insausti, I.; Sáez de Ocáriz, A.; Galbete, A.; Capdevila, F.; Solchaga, S.; Giral, P.; Bilhim, T.; Isaacson, A.; Urtasun, F.; Napal, S. Randomized Comparison of Prostatic Artery Embolization versus Transurethral Resection of the Prostate for Treatment of Benign Prostatic Hyperplasia. J. Vasc. Interv. Radiol. 2020, 31, 882–890. [Google Scholar] [CrossRef]
- DeMeritt, J.S.; Elmasri, F.F.; Esposito, M.P.; Rosenberg, G.S. Relief of benign prostatic hyperplasia-related bladder outlet obstruction after transarterial polyvinyl alcohol prostate embolization. J. Vasc. Interv. Radiol. 2000, 11, 767–770. [Google Scholar] [CrossRef]

| Characteristic | Overall, n = 272,916 | Prostate Artery Embolization, n = 3665 | TURP, n = 218,388 | Laser Enucleation, n = 50,863 | p-Value |
|---|---|---|---|---|---|
| Age (years) | 71 (65–78) | 69 (63–76) | 72 (65–78) | 71 (65–77) | <0.001 |
| Diabetes | 52,277 (19%) | 345 (9.4%) | 44,107 (20%) | 7825 (15%) | <0.001 |
| Chronic heart failure | 10,280 (3.8%) | 68 (1.9%) | 8963 (4.1%) | 1249 (2.5%) | <0.001 |
| COPD | 17,108 (6.3%) | 105 (2.9%) | 14,792 (6.8%) | 2211 (4.3%) | <0.001 |
| Chronic kidney disease | 21,514 (7.9%) | 130 (3.5%) | 18,861 (8.6%) | 2523 (5%) | <0.001 |
| Cerebrovascular disease | 4521 (1.7%) | 30 (0.8%) | 3968 (1.8%) | 523 (1%) | <0.001 |
| Dementia | 3648 (1.3%) | 16 (0.4%) | 3226 (1.5%) | 406 (0.8%) | <0.001 |
| Hypertension | 153,076 (56%) | 1445 (39%) | 126,224 (58%) | 25,407 (50%) | <0.001 |
| Obesity | 14,417 (5.3%) | 147 (4%) | 12,424 (5.7%) | 1846 (3.6%) | <0.001 |
| Year of surgery | <0.001 | ||||
| 2017 | 43,480 (16%) | 543 (15%) | 38,320 (18%) | 4617 (9.1%) | |
| 2018 | 45,430 (17%) | 794 (22%) | 37,944 (17%) | 6692 (13%) | |
| 2019 | 48,231 (18%) | 690 (19%) | 39,064 (18%) | 8477 (17%) | |
| 2020 | 41,860 (15%) | 513 (14%) | 32,926 (15%) | 8421 (17%) | |
| 2021 | 43,847 (16%) | 474 (13%) | 33,273 (15%) | 10,100 (20%) | |
| 2022 | 50,068 (18%) | 651 (18%) | 36,861 (17%) | 12,556 (25%) | |
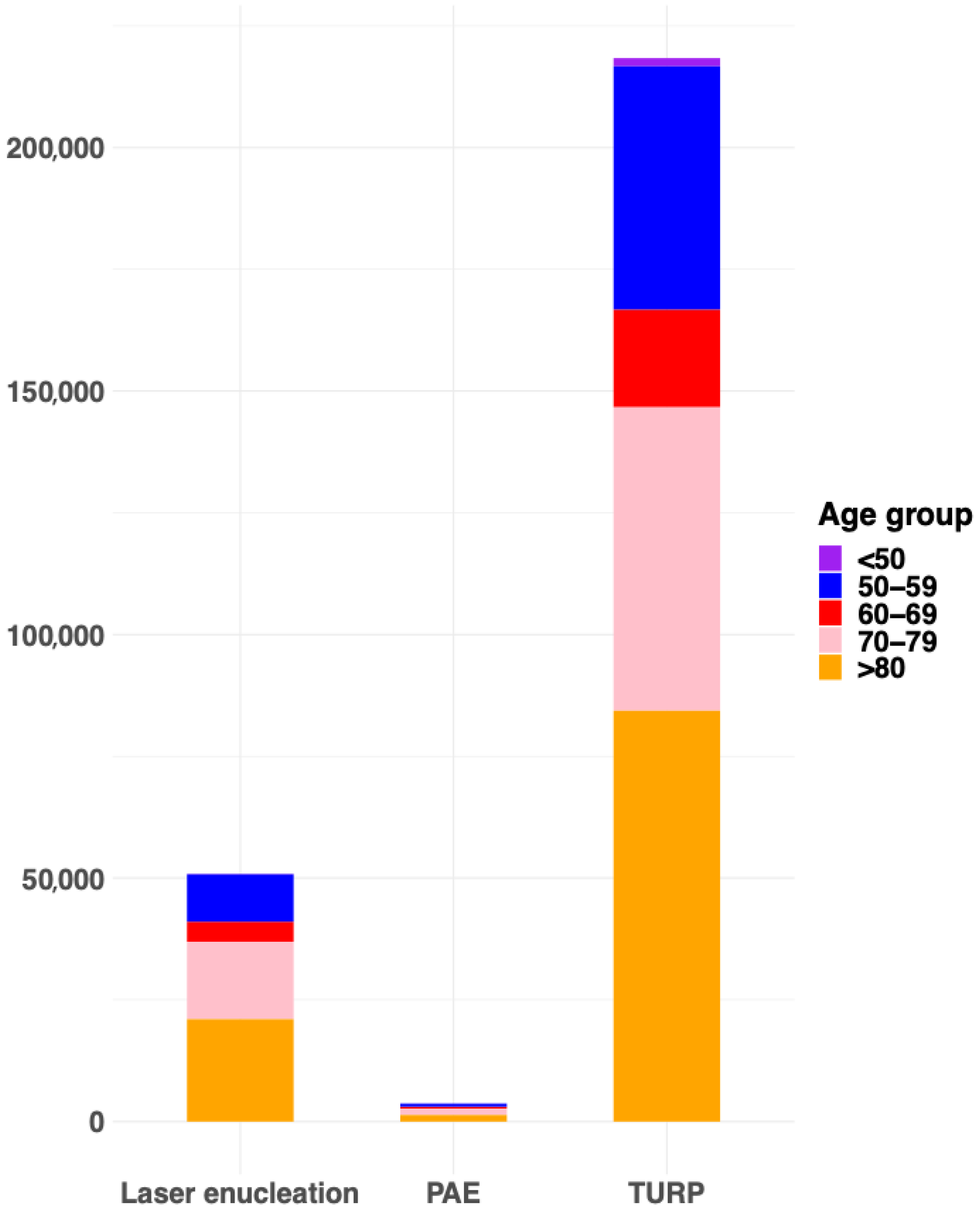
| Age group | <0.001 | ||||
| <50 | 1819 (0.7%) | 21 (0.6%) | 1682 (0.8%) | 116 (0.2%) | |
| 50–59 | 24,606 (9.0%) | 407 (11%) | 20,090 (9.2%) | 4109 (8.1%) | |
| 60–69 | 79,485 (29%) | 1258 (34%) | 62,310 (29%) | 15,917 (31%) | |
| 70–79 | 106,699 (39%) | 1351 (37%) | 84,359 (39%) | 20,989 (41%) | |
| >80 | 60,307 (22%) | 628 (17%) | 49,947 (23%) | 9732 (19%) |
| Outcome | Prostate Artery Embolization | TURP | Laser Enucleation | |||
|---|---|---|---|---|---|---|
| Cases | Estimate (95% CI), p-Value | Cases | Estimate (95% CI), p-Value | Cases | Estimate (95% CI), p-Value | |
| ICU admission | 24 (0.7%) | — | 1668 (0.8%) | 0.97 (0.66, 1.5), 0.9 | 392 (0.8%) | 1.1 (0.73, 1.7), 0.7 |
| Transfusion | 51 (1.4%) | — | 3932 (1.8%) | 1.1 (0.8, 1.4), 0.7 | 678 (1.3%) | 0.9 (0.67, 1.2), 0.4 |
| Sepsis | 11 (0.3%) | — | 1238 (0.6%) | 1.6 (0.95, 3.2), 0.1 | 171 (0.3%) | 1.1 (0.6, 2.1), 0.9 |
| Postoperative incontinence | 98 (2.7%) | — | 6698 (3.1%) | 1.1 (0.88, 1.3), 0.5 | 2139 (4.2%) | 1.6 (1.3, 1.9), <0.001 |
| Urinary retention | 119 (3.2%) | — | 15,600 (7.1%) | 2.2 (1.8, 2.6), <0.001 | 2532 (5%) | 1.5 (1.3, 1.8), <0.001 |
| Length of hospital stay | 2 (1–2) | — | 5 (3–6) | 2.6 (2.5, 2.7), <0.001 | 4 (3–5) | 1.5 (1.4, 1.6), <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pyrgidis, N.; Puhr-Westerheide, D.; Schulz, G.B.; Fabritius, M.P.; Kazmierczak, P.M.; Seidensticker, M.; Ricke, J.; Stief, C.; Weinhold, P.; Marcon, J.; et al. Comparison of Perioperative Outcomes for Prostate Artery Embolization Versus Transurethral Resection of the Prostate and Laser Enucleation for Benign Prostatic Hyperplasia: Results from the GRAND Study. J. Clin. Med. 2025, 14, 6135. https://doi.org/10.3390/jcm14176135
Pyrgidis N, Puhr-Westerheide D, Schulz GB, Fabritius MP, Kazmierczak PM, Seidensticker M, Ricke J, Stief C, Weinhold P, Marcon J, et al. Comparison of Perioperative Outcomes for Prostate Artery Embolization Versus Transurethral Resection of the Prostate and Laser Enucleation for Benign Prostatic Hyperplasia: Results from the GRAND Study. Journal of Clinical Medicine. 2025; 14(17):6135. https://doi.org/10.3390/jcm14176135
Chicago/Turabian StylePyrgidis, Nikolaos, Daniel Puhr-Westerheide, Gerald Bastian Schulz, Matthias Philipp Fabritius, Philipp M. Kazmierczak, Max Seidensticker, Jens Ricke, Christian Stief, Philipp Weinhold, Julian Marcon, and et al. 2025. "Comparison of Perioperative Outcomes for Prostate Artery Embolization Versus Transurethral Resection of the Prostate and Laser Enucleation for Benign Prostatic Hyperplasia: Results from the GRAND Study" Journal of Clinical Medicine 14, no. 17: 6135. https://doi.org/10.3390/jcm14176135
APA StylePyrgidis, N., Puhr-Westerheide, D., Schulz, G. B., Fabritius, M. P., Kazmierczak, P. M., Seidensticker, M., Ricke, J., Stief, C., Weinhold, P., Marcon, J., & Keller, P. (2025). Comparison of Perioperative Outcomes for Prostate Artery Embolization Versus Transurethral Resection of the Prostate and Laser Enucleation for Benign Prostatic Hyperplasia: Results from the GRAND Study. Journal of Clinical Medicine, 14(17), 6135. https://doi.org/10.3390/jcm14176135





