Indication for Radial or Carpal Resurfacing for Wrist Arthritis in Elderly Patients (over 70): A Systematic Review of the Literature
Abstract
1. Introduction
2. Methods
2.1. Search Strategy
2.2. Inclusion Criteria and Exclusion Criteria
2.3. Data Extraction and Quality Assessment
3. Results
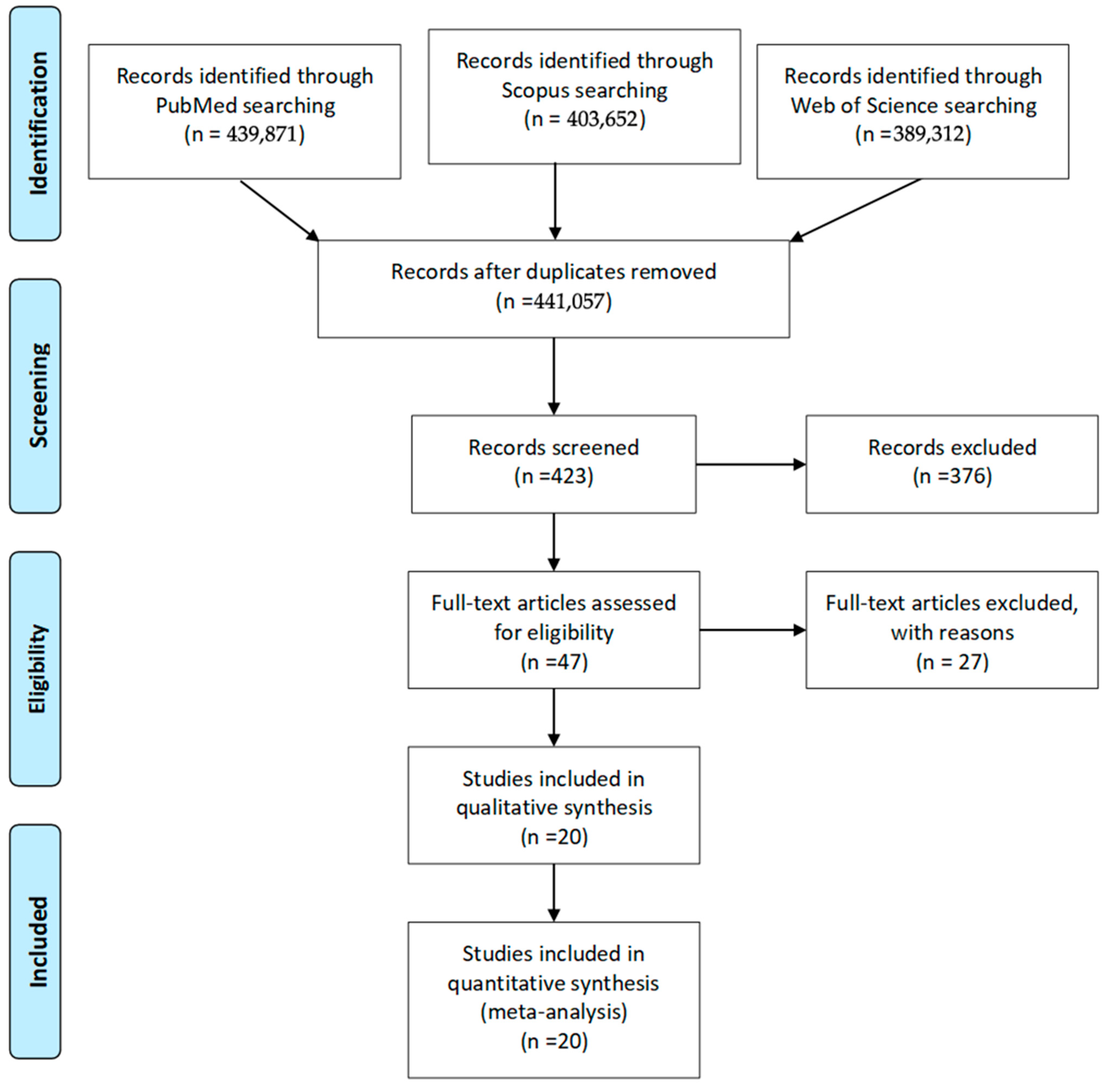
3.1. Study Selection
Rationale for Qualitative Synthesis
| Author | Selection (0–4★) | Comparability (0–2★) | Outcome (0–3★) | Total Score (0–9★) | Quality Rating |
|---|---|---|---|---|---|
| Benedikt, 2022 [21] | ★★★ | ★ | ★★ | 6★ | Moderate |
| Anger, 2019 [22] | ★★★ | ★ | ★★ | 6★ | Moderate |
| Apard, 2022 [23] | ★★ | ★ | ★★ | 5★ | Moderate |
| Herzberg, 2018 [24] | ★★★ | ★ | ★★ | 6★ | Moderate |
| Herzberg, 2023 [25] | ★★★ | ★ | ★★★ | 7★ | High |
| Herzberg, 2017 [26] | ★★★ | ★ | ★★ | 6★ | Moderate |
| Herzberg, 2015 [27] | ★★★ | ★ | ★★ | 6★ | Moderate |
| Martins, 2020 [19] | ★★★ | ★ | ★★ | 6★ | Moderate |
| Ichihara, 2015 [20] | ★★ | ★ | ★★ | 5★ | Moderate |
| Roux, 2009 [17] | ★★ | ★ | ★★ | 5★ | Moderate |
| Vergnenègre, 2015 [18] | ★★★ | ★ | ★★ | 6★ | Moderate |
| Anneberg, 2017 [31] | ★★★★ | ★★ | ★★★ | 9★ | High |
| Vance, 2012 [32] | ★★★ | ★★ | ★★ | 7★ | High |
| Rocchi, 2022 [3] | ★★★ | ★ | ★★ | 6★ | Moderate |
| Giacalone, 2017 [11] | ★★★★ | ★★ | ★★★ | 9★ | High |
| Ferrero, 2020 [14] | ★★★★ | ★★ | ★★★ | 9★ | High |
| Pelet, 2023 [15] | ★★★ | ★ | ★★★ | 7★ | High |
| Culp, 2012 [29] | ★★ | ★ | ★★ | 5★ | Moderate |
| Gaspar, 2016 [30] | ★★★ | ★ | ★★ | 6★ | Moderate |
| Author | Type of Prosthesis | Type of Study | Number of Patients | Sex | Mean Age | Prosthesis Indication | AO Classification | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| M | F | Fracture | Mal Union | Tumor | O.T.F. * | Arthrosis | C | C1 | C2 | C3 | A3 | |||||
| Benedikt 2022 [21] | COBRA | Retrospective cohort | 13 | 1 | 12 | 73.5 | 13 | 13 | ||||||||
| Anger 2019 [22] | COBRA | Retrospective cohort | 11 | 11 | 80 | 11 | 2 | 9 | ||||||||
| Apard 2022 [23] | COBRA | Case report | 1 | 1 | 83 | 1 | 1 | |||||||||
| Holzbauer 2022 [28] | EMIREMOTION | Case report | 1 | 1 | 73 | 1 | 1 | |||||||||
| Roux 2009 [17] | SOPHIA | Retrospective cohort | 12 | 1 | 11 | 73 | 4 | 1 | 1 | |||||||
| Anneberg 2017 [31] | KinematX | Prospective cohort | 20 | 11 | 9 | 50 | ||||||||||
| Culp 2012 [29] | Maestro/REMOTION | Retrospective cohort | 10 | 6 | 4 | 64 | ||||||||||
| Gaspar 2016 [30] | Biomet/Remotion | Retrospective cohort | 52 | 20 | 32 | 62 | ||||||||||
| Vance 2012 [32] | KinematX | Prospective cohort | 9 | 3 | 6 | 43 | ||||||||||
| Vergnenègre 2015 [18] | SOPHIA | Retrospective cohort | 8 | 8 | 80 | 8 | 8 | |||||||||
| Herztberg 2023 [25] | REMOTION/COBRA | Retrospective cohort | 26 | 1 | 25 | 79 | 28 | 28 | ||||||||
| Herztberg 2017 [26] | REMOTION/COBRA | Retrospective cohort | 15 | 11 | 74 | 12 | 12 | |||||||||
| 4 | 78 | 1 | 3 | |||||||||||||
| Herztberg 2018 [24] | REMOTION/COBRA | Retrospective cohort | 25 | 1 | 24 | 77 | 19 | 5 | 3 | |||||||
| Herztberg 2015 [27] | REMOTION/COBRA | Retrospective cohort | 11 | 11 | 76 | 12 | 12 | |||||||||
| Ichihara 2015 [20] | PROSTHELAST | Retrospective cohort | 12 | 12 | 76 | 11 | 1 | 1 | 6 | 3 | 2 | |||||
| Martins 2020 [19] | PROSTHELAST | Retrospective cohort | 24 | 2 | 22 | 78 | 24 | 7 | 15 | |||||||
| Pelet 2023 [15] | RCPI | Retrospective cohort | 30 | 26 | 4 | 59 | 2 | 28 | ||||||||
| Giacalone 2017 [11] | RCPI | Retrospective case–control | 25 | 23 | 2 | 58 | 25 | |||||||||
| Ferrero 2020 [14] | RCPI | Retrospective case–control | 31 | 25 | 6 | 57 | 31 | |||||||||
| Rocchi 2022 [3] | RCPI | Retrospective cohort | 7 | 7 | 0 | 68 | 7 | |||||||||
| F.U. Months | VAS | DASH | Lyon Score | PRWE | Grip Strength | Flexion | Extension | Forearm Rotation Arc | Ulnar Deviation | Radial Deviation | Cemented | Non-Cemented | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| COBRA, Benedikt 2022 [21] | 31.2 | 1.1 | 39.1 | 63.3% | 36.2 | 78.3% | 22° | 46° | 136° | 29° | 17° | 7 | 5 |
| COBRA, Anger 2019 [22] | 18.3 | 3.8 | 59 | 50% | 72 | 44% | 36° | 27° | 164° | 26° | 15° | 8 | 3 |
| COBRA, Apard 2022 [23] | 6 | 1 | 80% | 70° | 0 | 1 | |||||||
| REMOTION, Holzbauer 2022 [28] | 78 | 0 | 38 | 28 kg | 35° | 35° | 180° | 20° | 15° | 0 | 1 | ||
| SOPHIA, Roux 2009 [17] | 27 | 1.5 | 27.2 | 80% | 30° | 65° | 110° | 20° | 20° | 6 | 0 | ||
| KinematX, Anneberg 2017 [31] | 48 | 24 | 21 kg | 96° | 32° | ||||||||
| Maestro/REMOTION, Culp 2012 [29] | 19 | 33 kg | 57° | 23° | |||||||||
| Biomet/Remotion, Gaspar 2016 [30] | 35 | ||||||||||||
| KinematX, Vance 2012 [32] | 7 | 29 | 19 kg/62% | 79° | 29° | ||||||||
| SOPHIA, Vergnenègre 2015 [18] | 25 | 2 | 18 | 92% | 46° | 44° | 160° | 25° | 25° | 8 | 0 | ||
| REMOTION/COBRA, Herztberg 2023 [25] | 32 | 1 | 75% | 68% | 25° | 35° | 148° | 2 COBRA | 10 REMOTION, 16 COBRA | ||||
| REMOTION/COBRA, Herztberg 2017 [26] | 32 | 1 | 25 | 75% | 22 | 69% | 27° | 35° | 149° | 0 | 12/12 | ||
| 24 | 2.3 | 31 | 67% | 39.3 | 59.3% | 25° | 41° | 146° | 0 | 4/4 | |||
| REMOTION/COBRA, Herztberg 2018 [24] | 32 | 1 | 26 | 74% | 25 | 68% | 24° | 36° | 150° | 2 | 25/27 | ||
| REMOTION/COBRA, Herztberg 2015 [27] | 30 | 1 | 32 | 73% | 24 | 64% | 26° | 34° | 151° | 9 REMOTION, 2 COBRA | 0 | ||
| PROSTHELAST, Ichihara 2015 [20] | 32 | 2.8 | 37.4 | 49.9% | 40° | 52° | 138° | 0 | 12 | ||||
| PROSTHELAST, Martins 2020 [19] | 55 | 2.1 | 39.8 | 42.7 | 65.5% | 39° | 49° | 142° | 0 | 24 | |||
| RCPI, Pelet 2023 [15] | 84 | 2 | 14 | 29 kg | 65° | 45° | 0 | 30 | |||||
| RCPI, Giacalone 2017 [11] | 33 | 2 | 20 | 28 | 54% | 27° | 33° | 27° | 12° | 0 | 33 | ||
| RCPI, Ferrero 2020 [14] | 46 | 2 | 20 | 23 | 55% | 27° | 33° | 25° | 12° | 0 | 31 | ||
| RCPI, Rocchi 2022 [3] | 18 | 1 | 13 | 21 kg | 29° | 23° | |||||||
3.2. Patient Demographics
3.3. Indications for Prosthesis Implantation
3.4. Implant Characteristics and Surgical Techniques
3.5. Device-Specific Patient Populations
3.6. Follow-Up Duration
3.7. Pain Assessment
3.8. Functional Outcomes
3.9. Physical Performance Measures
3.9.1. Grip Strength
- SOPHIA: 80–92%;
- REMOTION/COBRA: 59.3–69%;
- PROSTHELAST: 49.9–65.5%;
- RCPI: 54–55%;
- COBRA: 44–78.3%.
3.9.2. Range of Motion
- KinematX: 79–96°;
- RCPI: 27–65°;
- PROSTHELAST: 39–40°;
- SOPHIA: 30–46°;
- COBRA: 22–36°;
- REMOTION/COBRA: 24–27°.
- SOPHIA: 44–65°;
- PROSTHELAST: 49–52°;
- REMOTION/COBRA: 34–41°;
- COBRA: 27–46°;
- RCPI: 23–42°.
- EMIREMOTION: 180°;
- COBRA: 136–164°;
- SOPHIA: 110–160°;
- RCPI: 128–150°.
3.10. Complications
3.10.1. Implant-Related Complications
- Implant loosening: 12 cases (3.5%), with a higher incidence in cemented designs (7.2%) compared to non-cemented designs (2.1%);
- Implant malposition: 9 cases (2.6%);
- Implant fracture/breakage: 5 cases (1.5%);
- Distal radioulnar joint instability: 7 cases (2.0%);
- Synovitis: 8 cases (2.3%);
- Metallosis: 2 cases (0.6%);
- Styloid impingement: 4 cases (1.2%).
3.10.2. Surgical Complications
- Surgical site infection: 6 cases (1.7%), with all cases resolving with antibiotic treatment;
- Delayed wound healing: 8 cases (2.3%);
- Complex regional pain syndrome: 7 cases (2.0%);
- Tendon rupture or irritation: 5 cases (1.5%);
- Nerve injury (transient): 5 cases (1.5%).
3.10.3. Age-Related Complications
- Cardiovascular events: 3 cases (0.9%);
- Pneumonia: 2 cases (0.6%);
- Delirium: 4 cases (1.2%);
- Fall-related injuries: 3 cases (0.9%).
3.10.4. Revision Surgery
- Conversion to total wrist arthrodesis: 11 cases (3.2%);
- Conversion to total wrist arthroplasty: 6 cases (1.7%);
- Implant repositioning: 5 cases (1.5%);
- Implant removal without replacement: 4 cases (1.2%).
4. Discussion
4.1. Summary of Key Findings
4.2. Age-Related Physiological Factors and Clinical Implications
4.2.1. Bone Mineral Density and Fixation Considerations
4.2.2. Clinical Implications and Pathophysiological Considerations
4.3. Prosthesis-Specific Considerations
4.3.1. Radial Resurfacing Implants
4.3.2. Carpal Resurfacing Considerations
4.4. Patient-Centered Outcomes and Quality of Life
4.4.1. Independence in Activities of Daily Living
4.4.2. Functional Outcome Measures: Clinical Relevance
4.4.3. Cost-Effectiveness Considerations
4.5. Long-Term Outcomes and Durability
4.6. Limitations
4.7. Future Research Directions
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| TWA | Total wrist arthroplasty |
| PRC | Proximal row carpectomy |
| RCPI | Resurfacing capitate pyrocarbon implant |
| DRF | Distal radius fracture |
| VAS | Visual Analog Scale |
| DASH | Disability of the Arm, Shoulder, and Hand |
| PRWE | Patient-Rated Wrist Evaluation |
| FCA | Four-corner arthrodesis |
| DCI | Dorsal capsular interposition |
References
- Lameijer, C.M.; Ten Duis, H.J.; Dusseldorp, I.V.; Dijkstra, P.U.; van der Sluis, C.K. Prevalence of posttraumatic arthritis and the association with outcome measures following distal radius fractures in non-osteoporotic patients: A systematic review. Arch. Orthop. Trauma. Surg. 2017, 137, 1499–1513, Erratum in: Arch. Orthop. Trauma. Surg. 2021, 141, 2019. [Google Scholar] [CrossRef] [PubMed]
- Lameijer, C.M.; Ten Duis, H.J.; Vroling, D.; Hartlief, M.T.; El Moumni, M.; van der Sluis, C.K. Prevalence of posttraumatic arthritis following distal radius fractures in non-osteoporotic patients and the association with radiological measurements, clinician and patient-reported outcomes. Arch. Orthop. Trauma. Surg. 2018, 138, 1699–1712. [Google Scholar] [CrossRef]
- Rocchi, L.; De Vitis, R.; Pietramala, S.; Fulchignoni, C.; D’Orio, M.; Mazzone, V.; Marcuzzi, A. Resurfacing Capitate Pyrocarbon Implant for the treatment of advanced wrist arthritis in the elderly: A retrospective study. Eur. Rev. Med. Pharmacol. Sci. 2022, 26 (Suppl. 1), 92–99. [Google Scholar]
- Cornette, B.; Hollevoet, N. Patterns of osteoarthritis of the wrist: A single-centre observational cohort study. J. Hand Surg. Eur. Vol. 2025, 50, 27–33. [Google Scholar] [CrossRef]
- Boeckstyns, M.E.H. Functional outcomes after salvage procedures for the destroyed wrist: An overview. J. Hand Surg. Eur. Vol. 2020, 45, 19–27. [Google Scholar] [CrossRef]
- Cavaliere, C.M.; Chung, K.C. A systematic review of total wrist arthroplasty compared with total wrist arthrodesis for rheumatoid arthritis. Plast. Reconstr. Surg. 2008, 122, 813–825. [Google Scholar] [CrossRef]
- Eschweiler, J.; Li, J.; Quack, V.; Rath, B.; Baroncini, A.; Hildebrand, F.; Migliorini, F. Total Wrist Arthroplasty-A Systematic Review of the Outcome, and an Introduction of FreeMove-An Approach to Improve TWA. Life 2022, 12, 411. [Google Scholar] [CrossRef] [PubMed]
- Chong, H.H.; Zabaglo, M.; Asif, A.; Boksh, K.; Kulkarni, K. A systematic review and network meta-analysis of outcomes after total wrist arthroplasty in inflammatory and non-inflammatory arthritis. J. Hand Surg. Eur. Vol. 2024, 49, 17–24. [Google Scholar] [CrossRef]
- De Vitis, R.; Passiatore, M.; Cilli, V.; Pamelin, E.; Velluto, C.; Ceravolo, I.; D’Orio, M.; Ferrari, F.; Taccardo, G. Secondary Wrist Arthritis in Active Workers: Does Capitate Pyrocarbon Resurfacing (RCPI) Improve Proximal Row Carpectomy? A Retrospective Cohort Study. J. Hand Surg. Asian Pac. Vol. 2021, 26, 625–634. [Google Scholar] [CrossRef]
- Hones, K.M.; Rakauskas, T.R.; Hao, K.A.; Densley, S.; Kim, J.; Wright, T.W.; Chim, H. Proximal Row Carpectomy with and without Capitate Resurfacing: A Preliminary Systematic Review and Meta-Analysis. JBJS Rev. 2024, 22, 12. [Google Scholar] [CrossRef] [PubMed]
- Giacalone, F.; di Summa, P.G.; Fenoglio, A.; Sard, A.; Dutto, E.; Ferrero, M.; Bertolini, M.; Garcia-Elias, M. Resurfacing Capitate Pyrocarbon Implant versus Proximal Row Carpectomy Alone: A Comparative Study to Evaluate the Role of Capitate Prosthetic Resurfacing in Advanced Carpal Collapse. Plast. Reconstr. Surg. 2017, 140, 962–970. [Google Scholar] [CrossRef]
- Rieussec, C.; Caillard, G.; Helfter, L.; Girard, P.; Forli, A.; Corcella, D. Comparison of proximal row carpectomy with RCPI® versus proximal row carpectomy with Eaton’s capsular interposition in the management of advanced wrist osteoarthritis. Orthop. Traumatol. Surg. Res. 2024, 110, 103783. [Google Scholar] [CrossRef] [PubMed]
- Marcuzzi, A.; Pederiva, D.; Pilla, F.; Canovi, A.; Corradini, A.; Adani, R.; Ruffilli, A.; Faldini, C.; Vita, F. The use of resurfacing capitate pyrocarbon implants (RCPI) in chronic diseases of the wrist: Outcomes of more than 100 cases. Musculoskelet. Surg. 2024, 108, 367–371. [Google Scholar] [CrossRef]
- Ferrero, M.; di Summa, P.G.; Giacalone, F.; Senesi, L.; Sapino, G.; Battiston, B. Salvage of advanced carpal collapse: Proximal row carpectomy with pyrocarbon resurfacing of the capitate versus four-corner arthrodesis. J. Hand Surg. Eur. Vol. 2020, 45, 687–692. [Google Scholar] [CrossRef]
- Pelet, H.; Delgove, A.; Morchikh, A.; Dunet, B.; Harper, L.; Laumonerie, P.; Abi-Chahla, M.L. Long-term results of first row carpectomy with proximal capitate resurfacing using a pyrocarbon implant. J. Hand Surg. Eur. Vol. 2023, 48, 561–565. [Google Scholar] [CrossRef] [PubMed]
- Cannella, A.; Caruso, L.; Sassara, G.M.; Taccardo, G.; Passiatore, M.; Marescalchi, M.; De Vitis, R. Hemiarthroplasty for irreparable distal radius fractures in the elderly: A comprehensive review. World J. Orthop. 2024, 15, 578–584. [Google Scholar] [CrossRef] [PubMed]
- Roux, J.L. La prothèse de remplacement et resurfaçage du radius distal: Un nouveau concept thérapeutique [Replacement and resurfacing prosthesis of the distal radius: A new therapeutic concept]. Chirurgie de la Main 2009, 28, 10–17. [Google Scholar] [CrossRef]
- Vergnenègre, G.; Hardy, J.; Mabit, C.; Charissoux, J.L.; Marcheix, P.S. Hemiarthroplasty for Complex Distal Radius Fractures in Elderly Patients. J. Wrist Surg. 2015, 4, 169–173. [Google Scholar] [CrossRef]
- Martins, A.; Lazarus, P.; Facca, S.; Gouzou, S.; Meyer, N.; Liverneaux, P. Isoelastic resurfacing prosthesis for distal radius fractures: Outcomes in 24 cases with at least 2 years’ follow-up. Orthop. Traumatol. Surg. Res. 2020, 106, 1613–1618. [Google Scholar] [CrossRef]
- Ichihara, S.; Díaz, J.J.; Peterson, B.; Facca, S.; Bodin, F.; Liverneaux, P. Distal Radius Isoelastic Resurfacing Prosthesis: A Preliminary Report. J. Wrist Surg. 2015, 4, 150–155. [Google Scholar] [CrossRef]
- Benedikt, S.; Kaiser, P.; Schmidle, G.; Kastenberger, T.; Stock, K.; Arora, R. Lessons learned with the Cobra prosthesis in elderly patients with complex distal radius fractures-a retrospective follow-up study. Arch. Orthop. Trauma. Surg. 2022, 142, 343–353. [Google Scholar] [CrossRef] [PubMed]
- Anger, F.; Legré, R.; Nguyen, M.K. Results of wrist hemiarthroplasty for comminuted distal radius fractures in independent elderly people: A retrospective study on eleven patients. Hand Surg. Rehabil. 2019, 38, 150–156. [Google Scholar] [CrossRef]
- Apard, T.; Odoemene, M.; Descamps, J. Wrist Hemiarthroplasty of Irreparable Distal Radius Fracture under Wide-Awake Local Anesthetic and No Tourniquet. Life 2022, 12, 1624. [Google Scholar] [CrossRef]
- Herzberg, G.; Walch, A.; Burnier, M. Wrist hemiarthroplasty for irreparable DRF in the elderly. Eur. J. Orthop. Surg. Traumatol. 2018, 28, 1499–1503. [Google Scholar] [CrossRef]
- Herzberg, G.; Burnier, M.; Ly, L. Role for Wrist Hemiarthroplasty in Acute Irreparable Distal Radius Fracture in the Elderly. Hand Clin. 2023, 39, 545–550. [Google Scholar] [CrossRef]
- Herzberg, G.; Merlini, L.; Burnier, M. Hemi-arthroplasty for distal radius fracture in the independent elderly. Orthop. Traumatol. Surg. Res. 2017, 103, 915–918. [Google Scholar] [CrossRef] [PubMed]
- Herzberg, G.; Burnier, M.; Marc, A.; Izem, Y. Primary Wrist Hemiarthroplasty for Irreparable Distal Radius Fracture in the Independent Elderly. J. Wrist Surg. 2015, 4, 156–163. [Google Scholar] [CrossRef]
- Holzbauer, M.; Bodell, L.S.; Froschauer, S.M. Wrist Hemiarthroplasty for Complex Intraarticular Distal Radius Fracture in a Patient with Manifest Osteoporosis. Life 2022, 12, 471. [Google Scholar] [CrossRef]
- Culp, R.W.; Bachoura, A.; Gelman, S.E.; Jacoby, S.M. Proximal row carpectomy combined with wrist hemiarthroplasty. J. Wrist Surg. 2012, 1, 39–46. [Google Scholar] [CrossRef] [PubMed]
- Gaspar, M.P.; Lou, J.; Kane, P.M.; Jacoby, S.M.; Osterman, A.L.; Culp, R.W. Complications following partial and total wrist arthroplasty: A single-center retrospective review. J. Hand Surg. Am. 2016, 41, 47–53. [Google Scholar] [CrossRef] [PubMed]
- Anneberg, M.; Packer, G.; Crisco, J.J.; Wolfe, S. Four-Year Outcomes of Midcarpal Hemiarthroplasty for Wrist Arthritis. J. Hand Surg. Am. 2017, 42, 894–903. [Google Scholar] [CrossRef]
- Vance, M.C.; Packer, G.; Tan, D.; Crisco, J.J.; Wolfe, S.W. Midcarpal hemiarthroplasty for wrist arthritis: Rationale and early results. J. Wrist Surg. 2012, 1, 61–68. [Google Scholar] [CrossRef]
- Salomon, G.D.; Eaton, R.G. Proximal row carpectomy with partial capitate resection. J. Hand Surg. Am. 1996, 21, 2–8. [Google Scholar] [CrossRef]
- Adenikinju, A.; Wu, K.Y.; Karim, K.; Carlsen, B.; Kakar, S. Outcomes of Proximal Row Carpectomy With Interposition Arthroplasty for Advanced Wrist Arthritis. Hand 2024, 23, 15589447241298721. [Google Scholar] [CrossRef] [PubMed]
- Fowler, J.R.; Tang, P.C.; Imbriglia, J.E. Osteochondral resurfacing with proximal row carpectomy: 8-year follow-up. Orthopedics 2014, 37, e856–e859. [Google Scholar] [CrossRef] [PubMed]
- Andersson, J.K.; Hagert, E.; Brittberg, M. Cartilage Injuries and Posttraumatic Osteoarthritis in the Wrist: A Review. Cartilage 2021, 13 (Suppl. 1), 156S–168S. [Google Scholar] [CrossRef]
- Rabinovich, R.V.; Lee, S.J. Proximal Row Carpectomy Using Decellularized Dermal Allograft. J. Hand Surg. Am. 2018, 43, 392.e1–392.e9. [Google Scholar] [CrossRef] [PubMed]
- Artuso, M.; Protais, M.; Soubeyrand, M. Arthroscopic proximal carpal row replacement by semitendinosus and gracilis graft (CArpus Row Plasty Using the Semitendinosus: CARPUS procedure). An anatomical study of 16 cases. Orthop. Traumatol. Surg. Res. 2022, 108, 103124. [Google Scholar] [CrossRef]
- Bellemère, P. Pyrocarbon implants for the hand and wrist. Hand Surg. Rehabil. 2018, 37, 129–154. [Google Scholar] [CrossRef]
- Bellemère, P. Medium- and long-term outcomes for hand and wrist pyrocarbon implants. J. Hand Surg. Eur. Vol. 2019, 44, 887–897. [Google Scholar] [CrossRef]
- Marcuzzi, A.; Fulchignoni, C.; Teodori, J.; Rocchi, L. Resurfacing capitate pyrocarbon implant as salvage procedure in several serious outcomes of carpal injuries. Clinical experience and follow-up. Acta Biomed. 2022, 92, e2021536. [Google Scholar] [PubMed]
- Adams, B.D.; Lawler, E.A.; Kuhl, T.L. Distal Radius Hemiarthroplasty. J. Wrist Surg. 2016, 5, 217–221. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Stegelmann, S.D.; Porter, S.; Yim, J.; Druessel, L.; Koepplinger, M.; Lee, A. Outcomes of radial-sided wrist hemiarthroplasty: A systematic review. J. Orthop. 2025, 69, 191–199. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cannella, A.; Sassara, G.M.; Caruso, L.; Rapisarda, A.M.; Passiatore, M.; Cilli, V.; Guzzini, M.; De Vitis, R. Indication for Radial or Carpal Resurfacing for Wrist Arthritis in Elderly Patients (over 70): A Systematic Review of the Literature. J. Clin. Med. 2025, 14, 6063. https://doi.org/10.3390/jcm14176063
Cannella A, Sassara GM, Caruso L, Rapisarda AM, Passiatore M, Cilli V, Guzzini M, De Vitis R. Indication for Radial or Carpal Resurfacing for Wrist Arthritis in Elderly Patients (over 70): A Systematic Review of the Literature. Journal of Clinical Medicine. 2025; 14(17):6063. https://doi.org/10.3390/jcm14176063
Chicago/Turabian StyleCannella, Adriano, Giulia Maria Sassara, Ludovico Caruso, Antonio Maria Rapisarda, Marco Passiatore, Vitale Cilli, Matteo Guzzini, and Rocco De Vitis. 2025. "Indication for Radial or Carpal Resurfacing for Wrist Arthritis in Elderly Patients (over 70): A Systematic Review of the Literature" Journal of Clinical Medicine 14, no. 17: 6063. https://doi.org/10.3390/jcm14176063
APA StyleCannella, A., Sassara, G. M., Caruso, L., Rapisarda, A. M., Passiatore, M., Cilli, V., Guzzini, M., & De Vitis, R. (2025). Indication for Radial or Carpal Resurfacing for Wrist Arthritis in Elderly Patients (over 70): A Systematic Review of the Literature. Journal of Clinical Medicine, 14(17), 6063. https://doi.org/10.3390/jcm14176063







