The Role of Brachytherapy in the Management of Oral Squamous Cell Carcinoma: A Systematic Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Search Strategy and Database Screening
2.2. Eligibility Criteria
2.3. Focused PIO Question and Effect Measure
- (P) Participants: Patients with a histological diagnosis of oral squamous cell carcinoma (OSCC).
- (I) Intervention: Brachytherapy (LDR or HDR), either as definitive, adjuvant, or boost treatment.
- (O) Outcome: Oncologic outcomes (local control, overall survival), functional outcomes, and treatment-related toxicity.
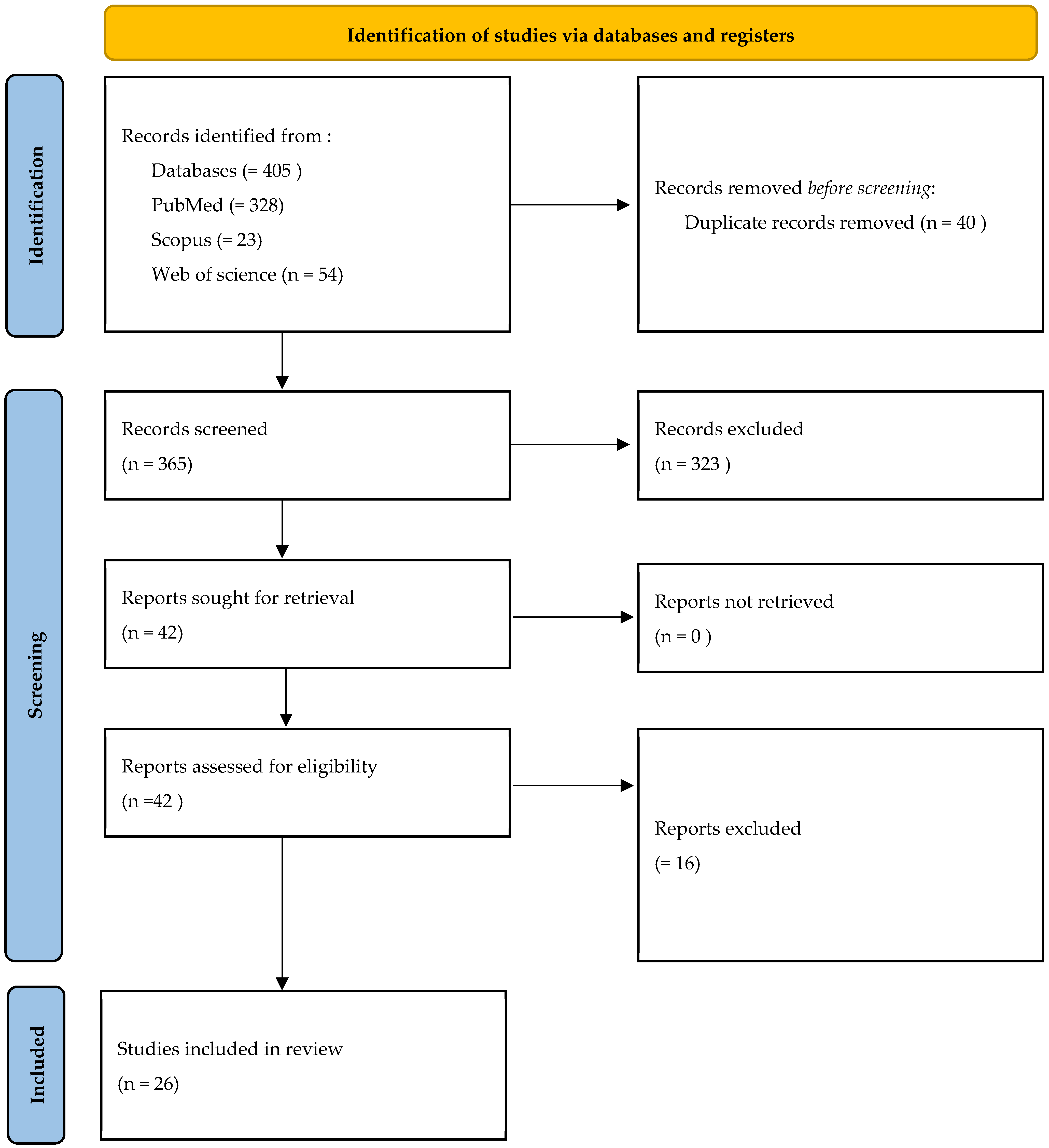
2.4. Studies Screening and Inclusion
2.5. Data Extraction
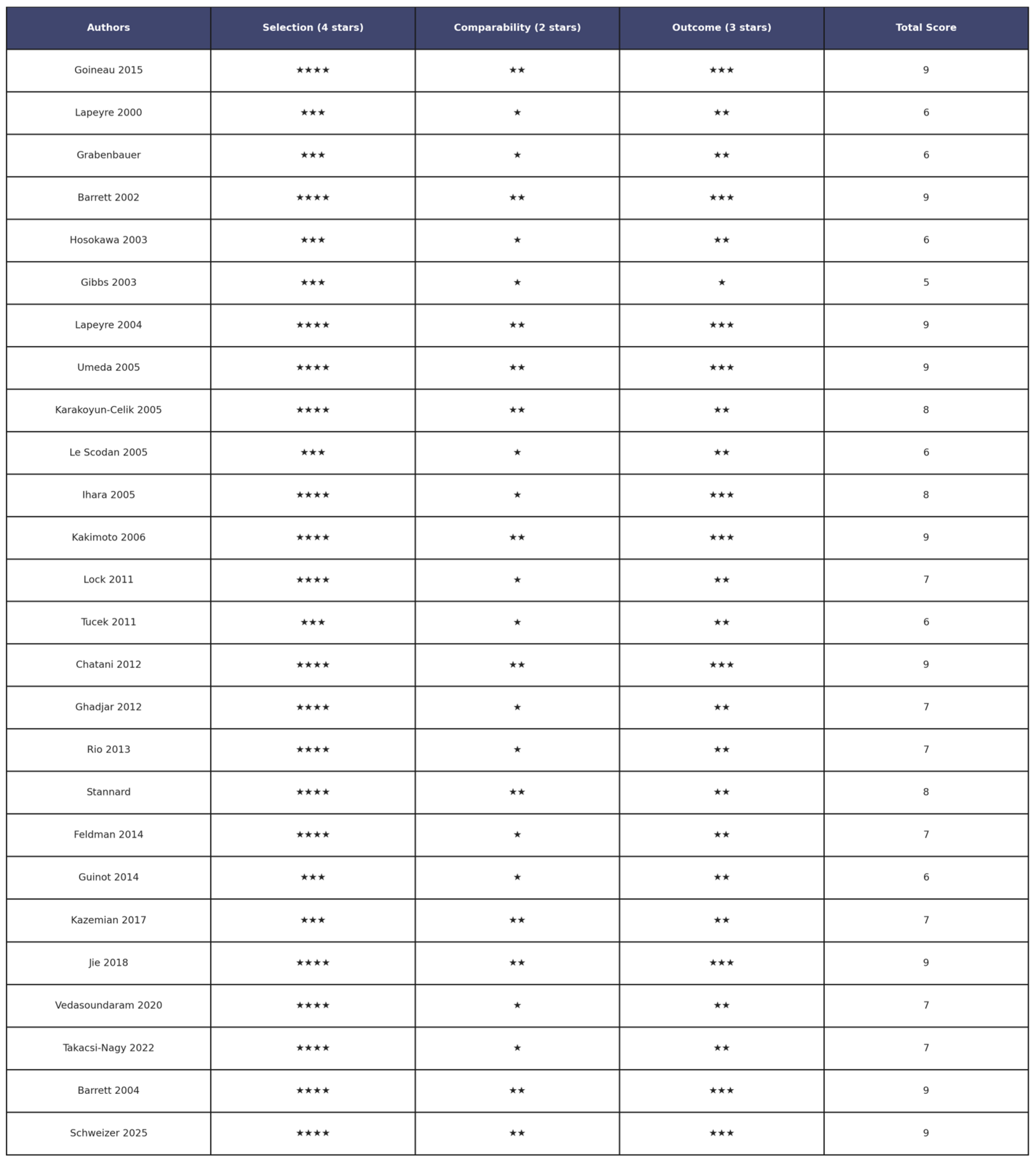
2.6. Assessment of Risk of Bias
2.7. Confidence in Cumulative Evidence
3. Results
3.1. Study Selection
3.2. Risk of Bias Assessment
3.3. Certanty of Evidence
3.4. Study Characteristics
3.4.1. Population and Tumor Characteristics
3.4.2. Brachytherapy Techniques
3.4.3. Treatment Setting (Local Control, Overall Survival, and Toxicity)
- Local control: 72–95% across studies;
- Overall survival: 3- to 5-year OS ranged from 60 to 85%;
- Toxicity: Acute mucositis was the most frequent complication (30–80%). Late complications included soft tissue necrosis (5–20%) and osteoradionecrosis (3–15%).
4. Discussion
5. Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| OSCC | Oral squamous cell carcinoma |
| CT | Chemotherapy |
| EBRT | external beam radiation therapy |
| LDR-BT | Low-dose-rate interstitial brachytherapy |
| LDR | low dose rate |
| HDR | high dose rate |
| Ir 192 | Iridium-192 |
| C 137 | Caesium-137 |
| I 125 | Iodine-125 |
References
- Bray, F.; Laversanne, M.; Sung, H.; Ferlay, J.; Siegel, R.L.; Soerjomataram, I.; Jemal, A. Global cancer statistics 2022: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2024, 74, 229–263. [Google Scholar] [CrossRef]
- Esperouz, F.; Ciavarella, D.; Lorusso, M.; Santarelli, A.; Muzio, L.L.; Campisi, G.; Russo, L.L. Critical review of OCT in clinical practice for the assessment of oral lesions. Front. Oncol. 2025, 15, 1569197. [Google Scholar] [CrossRef]
- Huang, S.-H.; O’Sullivan, B. Oral cancer: Current role of radiotherapy and chemotherapy. Med. Oral Patol. Oral Y Cir. Bucal. 2013, 18, e233–e240. [Google Scholar] [CrossRef]
- Esperouz, F.; Caponio, V.C.A.; Santarelli, A.; Ballini, A.; Muzio, L.L.; Ciavarella, D.; Russo, L.L. Are we ready to use ultrasounds in the clinical assessment of depth of invasion and tumor thickness in oral squamous cell carcinoma? Results from a systematic review, meta-analysis and trial sequential analysis. Oral Oncol. 2024, 159, 107104. [Google Scholar] [CrossRef]
- Bhalavat, R.; Pareek, V.; Chandra, M.; Nellore, L.; George, K.; Borade, D.; Kalariya, K.; Moosa, Z.; Srivastava, A.; Reddy, N.; et al. High-dose-rate interstitial brachytherapy in recurrent head and neck cancer: An effective salvage option. J. Contemp. Brachyther. 2018, 10, 425–430. [Google Scholar] [CrossRef]
- Sankar, V.; Xu, Y. Oral Complications from Oropharyngeal Cancer Therapy. Cancers 2023, 15, 4548. [Google Scholar] [CrossRef]
- Hunte, S.O.; Clark, C.H.; Zyuzikov, N.; Nisbet, A. Volumetric modulated arc therapy (VMAT): A review of clinical outcomes-what is the clinical evidence for the most effective implementation? Br. J. Radiol. 2022, 95, 20201289. [Google Scholar] [CrossRef]
- Koka, K.; Verma, A.; Dwarakanath, B.S.; Papineni, R.V.L. Technological Advancements in External Beam Radiation Therapy (EBRT): An Indispensable Tool for Cancer Treatment. Cancer Manag. Res. 2022, 14, 1421–1429. [Google Scholar] [CrossRef]
- Mayer, C.; Gasalberti, D.P.; Kumar, A. Brachytherapy. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2025. [Google Scholar]
- Vavassori, A.; Gherardi, F.; Colangione, S.P.; Fodor, C.; Cattani, F.; Lazzari, R.; Calabrese, L.; Bruschini, R.; Alterio, D.; Jereczek-Fossa, B.A.; et al. High-dose-rate interstitial brachytherapy in early stage buccal mucosa and lip cancer: Report on 12 consecutive patients and review of the literature. Tumori 2012, 98, 471–477. [Google Scholar] [CrossRef]
- Lee, C.D. Recent developments and best practice in brachytherapy treatment planning. Br. J. Radiol. 2014, 87, 20140146. [Google Scholar] [CrossRef]
- Mazeron, J.J.; Ardiet, J.M.; Haie-Méder, C.; Kovács, G.; Levendag, P.; Peiffert, D.; Polo, A.; Rovirosa, A.; Strnad, V. GEC-ESTRO recommendations for brachytherapy for head and neck squamous cell carcinomas. Radiother. Oncol. 2009, 91, 150–156. [Google Scholar] [CrossRef]
- Muto, P.; Pastore, F. Radiotherapy in the Adjuvant and Advanced Setting of CSCC. Dermatol. Pract. Concept. 2021, 11, e2021168S. [Google Scholar] [CrossRef]
- Lapeyre, M.; Hoffstetter, S.; Peiffert, D.; Guérif, S.; Maire, F.; Dolivet, G.; Toussaint, B.; Mundt, A.; Chassagne, J.-F.; Simon, C.; et al. Postoperative brachytherapy alone for T1-2 N0 squamous cell carcinomas of the oral tongue and floor of mouth with close or positive margins. Int. J. Radiat. Oncol. Biol. Phys. 2000, 48, 37–42. [Google Scholar] [CrossRef]
- Grabenbauer, G.G.; Rödel, C.; Brunner, T.; Schulze-Mosgau, S.; Strnad, V.; Müller, R.G.; Iro, H.; Sauer, R. Interstitial brachytherapy with Ir-192 low-dose-rate in the treatment of primary and recurrent cancer of the oral cavity and oropharynx. Review of 318 patients treated between 1985 and 1997. Strahlenther. Onkol. 2001, 177, 338–344. [Google Scholar] [CrossRef]
- Barrett, W.L.; Gleich, L.; Wilson, K.; Gluckman, J. Organ preservation with interstitial radiation for base of tongue cancer. Am. J. Clin. Oncol. 2002, 25, 485–488. [Google Scholar] [CrossRef]
- Hosokawa, Y.; Shirato, H.; Nishioka, T.; Tsuchiya, K.; Chang, T.-C.; Kagei, K.; Ohomori, K.; Obinata, K.-I.; Kaneko, M.; Miyasaka, K.; et al. Effect of treatment time on outcome of radiotherapy for oral tongue carcinoma. Int. J. Radiat. Oncol. Biol. Phys. 2003, 57, 71–78. [Google Scholar] [CrossRef]
- Gibbs, I.C.; Le, Q.T.; Shah, R.D.; Terris, D.J.; Fee, W.E.; Goffinet, D.R. Long-term outcomes after external beam irradiation and brachytherapy boost for base-of-tongue cancers. Int. J. Radiat. Oncol. Biol. Phys. 2003, 57, 489–494. [Google Scholar] [CrossRef]
- Barrett, W.L.; Gluckman, J.L.; Wilson, K.M.; Gleich, L.L. A comparison of treatments of squamous cell carcinoma of the base of tongue: Surgical resection combined with external radiation therapy, external radiation therapy alone, and external radiation therapy combined with interstitial radiation. Brachytherapy 2004, 3, 240–245. [Google Scholar] [CrossRef] [PubMed]
- Lapeyre, M.; Bollet, M.A.; Racadot, S.; Geoffrois, L.; Kaminsky, M.; Hoffstetter, S.; Dolivet, G.; Toussaint, B.; Luporsi, E.; Peiffert, D. Postoperative brachytherapy alone and combined postoperative radiotherapy and brachytherapy boost for squamous cell carcinoma of the oral cavity, with positive or close margins. Head Neck 2004, 26, 216–223. [Google Scholar] [CrossRef]
- Umeda, M.; Komatsubara, H.; Nishimatsu, N.; Yokoo, S.; Shibuya, Y.; Komori, T. High-dose rate interstitial brachytherapy for stage I-II tongue cancer. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2000, 90, 667–670. [Google Scholar] [CrossRef]
- Karakoyun-Celik, O.; Norris, C.M.J.; Tishler, R.; Mahadevan, A.; Clark, J.R.; Goldberg, S.; Devlin, P.; Busse, P.M. Definitive radiotherapy with interstitial implant boost for squamous cell carcinoma of the tongue base. Head Neck 2005, 27, 353–361. [Google Scholar] [CrossRef]
- Le Scodan, R.; Pommier, P.; Ardiet, J.M.; Montbarbon, X.; Malet, C.; Favrel, V.; Zrounba, P.; Poupart, M.; Céruse, P.; Ferlay, C.; et al. Exclusive brachytherapy for T1 and T2 squamous cell carcinomas of the velotonsillar area: Results in 44 patients. Int. J. Radiat. Oncol. Biol. Phys. 2005, 63, 441–448. [Google Scholar] [CrossRef]
- Ihara, N.; Shibuya, H.; Yoshimura, R.; Oota, S.; Miura, M.; Watanabe, H. Interstitial brachytherapy and neck dissection for Stage III squamous cell carcinoma of the mobile tongue. Acta Oncol. 2005, 44, 709–716. [Google Scholar] [CrossRef]
- Kakimoto, N.; Inoue, T.; Inoue, T.; Murakami, S.; Furukawa, S.; Yoshida, K.; Yoshioka, Y.; Yamazaki, H.; Tanaka, E.; Kimishige Shimizutani, K. High-dose-rate interstitial brachytherapy for mobile tongue cancer: Influence of the non-irradiated period. Anticancer Res. 2006, 26, 3933–3937. [Google Scholar]
- Lock, M.; Cao, J.Q.; D’Souza, D.P.; Hammond, J.A.; Karnas, S.; Lewis, C.; Venkatesan, V.M.; Whiston, E.; Yau, G.; Yu, E.; et al. Brachytherapy with permanent gold grain seeds for squamous cell carcinoma of the lip. Radiother. Oncol. 2011, 98, 352–356. [Google Scholar] [CrossRef]
- Tuček, L.; Petera, J.; Sirák, I.; Vošmik, M.; Doležalová, H.; Brokešová, S.; Hodek, M.; Kašaová, L.; Paluska, P. Hyperfractionated high-dose rate brachytherapy in the treatment of oral tongue cancer. Rep. Pract. Oncol. Radiother. 2011, 16, 243–247. [Google Scholar] [CrossRef]
- Chatani, M.; Tsuboi, K.; Yagi, M.; Fujiwara, K.; Tachimoto, R.; Yoshioka, H. High dose rate brachytherapy using molds after chemoradiotherapy for oral cavity cancer. Jpn. J. Radiol. 2012, 30, 40–44. [Google Scholar] [CrossRef]
- Ghadjar, P.; Bojaxhiu, B.; Simcock, M.; Vošmik, M.; Doležalová, H.; Brokešová, S.; Hodek, M.; Kašaová, L.; Paluska, P. High dose-rate versus low dose-rate brachytherapy for lip cancer. Int. J. Radiat. Oncol. Biol. Phys. 2012, 83, 1205–1212. [Google Scholar] [CrossRef]
- Rio, E.; Bardet, E.; Mervoyer, A.; Piot, B.; Dreno, B.; Malard, O. Interstitial brachytherapy for lower lip carcinoma: Global assessment in a retrospective study of 89 cases. Head Neck 2013, 35, 350–353. [Google Scholar] [CrossRef]
- Stannard, C.; Maree, G.; Tovey, S.; Hunter, A.; Wetter, J. Iodine-125 brachytherapy in the management of squamous cell carcinoma of the oral cavity and oropharynx. Brachytherapy 2014, 13, 405–412. [Google Scholar] [CrossRef]
- Feldman, J.; Appelbaum, L.; Sela, M.; Voskoboinik, N.; Kadouri, S.; Weinberger, J.; Orion, I.; Meirovitz, A. Novel high dose rate lip brachytherapy technique to improve dose homogeneity and reduce toxicity by customized mold. Radiat. Oncol. 2014, 9, 271. [Google Scholar] [CrossRef]
- Guinot, J.L.; Arribas, L.; Vendrell, J.B.; Santos, M.; Tortajada, M.I.; Mut, A.; Cruz, J.; Mengual, J.L.; Chust, M.L. Prognostic factors in squamous cell lip carcinoma treated with high-dose-rate brachytherapy. Head Neck 2014, 36, 1737–1742. [Google Scholar] [CrossRef]
- Goineau, A.; Piot, B.; Malard, O.; Ferron, C.; Lisbona, A.; Cassagnau, E.; Delamazure, A.-S.; Campion, L.; Bardet, E. Postoperative interstitial brachytherapy for resectable squamous cell carcinoma of the tongue. Brachytherapy 2015, 14, 71–76. [Google Scholar] [CrossRef]
- Kazemian, A.; Babaei, M.; Lashkari, M.; Ghalehtaki, R.; Garajei, A.; Motiee-Langroudi, M.; Sebzari, A.; Jaberi, R.; Gholami, S.; Babaloui, S.; et al. Adjuvant high-dose-rate brachytherapy in the management of oral cavity cancers: 5 years of experience in Iran. J. Contemp. Brachyther. 2017, 9, 323–329. [Google Scholar] [CrossRef]
- Jie, W.P.; Bai, J.Y.; Li, B.B. Clinicopathologic Analysis of Oral Squamous Cell Carcinoma After (125)I Interstitial Brachytherapy. Technol. Cancer Res. Treat. 2018, 17. [Google Scholar] [CrossRef]
- Vedasoundaram, P.; Raghava Ks, A.; Periasamy, K.; Selvarajan, G.; K, S.; Kandasamy, S.; R, S.; Kumar, A. The Effect of High Dose Rate Interstitial Implant on Early and Locally Advanced Oral Cavity Cancers: Update and Long-Term Follow-Up Study. Cureus 2020, 12, e7910. [Google Scholar] [CrossRef]
- Takácsi-Nagy, Z.; Ferenczi, Ö.; Major, T.; Akiyama, H.; Fröhlich, G.; Oberna, F.; Révész, M.; Poósz, M.; Polgár, C. Results of sole postoperative interstitial, high-dose-rate brachytherapy of T1-2 tongue tumours. Strahlenther. Onkol. 2022, 198, 812–819. [Google Scholar] [CrossRef] [PubMed]
- Schweizer, C.; Strnad, V.; Lotter, M.; Kreppner, S.; Merten, R.; Fietkau, R.; Karius, A. Postoperative brachytherapy alone for 217 patients with early-stage oral cavity squamous cell carcinoma. Clin. Transl. Radiat. Oncol. 2025, 51, 100922. [Google Scholar] [CrossRef]
- Granholm, A.; Alhazzani, W.; Møller, M.H. Use of the GRADE approach in systematic reviews and guidelines. Br. J. Anaesth. 2019, 123, 554–559. [Google Scholar] [CrossRef]
- Umeda, M.; Komatsubara, H.; Ojima, Y.; Minamikawa, T.; Shibuya, Y.; Yokoo, S.; Ishii, J.; Komori, T. A comparison of brachytherapy and surgery for the treatment of stage I-II squamous cell carcinoma of the tongue. Int. J. Oral Maxillofac. Surg. 2005, 34, 739–744. [Google Scholar] [CrossRef]
- Draghini, L.; Lancellotta, V.; Fionda, B.; De Angeli, M.; Cornacchione, P.; Massaccesi, M.; Trippa, F.; Kovács, G.; Morganti, A.G.; Bussu, F.; et al. Can interventional radiotherapy (brachytherapy) be an alternative to surgery in early-stage oral cavity cancer? A systematic review. Strahlenther. Onkol. 2024, 200, 367–376. [Google Scholar] [CrossRef]
- Abdulkadir, M.K.; Appalanaido, G.K.; Musa, M.Y.; Bin Jalil, J.; Bin Mohamad, A.F.; Yogabalan, K.; Aziz, M.Z.A. Sole high dose-rate interstitial brachytherapy for early-stage tongue cancer: A systematic review. Cancer Radiother. 2025, 29, 104626. [Google Scholar] [CrossRef]
- Shi, J.; Chen, J.; He, G.; Peng, Q. Artificial intelligence in high-dose-rate brachytherapy treatment planning for cervical cancer: A review. Front. Oncol. 2025, 15, 1507592. [Google Scholar] [CrossRef]
- Banerjee, S.; Goyal, S.; Mishra, S.; Gupta, D.; Bisht, S.S.; K, V.; Narang, K.; Kataria, T. Artificial intelligence in brachytherapy: A summary of recent developments. Br. J. Radiol. 2021, 94, 20200842. [Google Scholar] [CrossRef]
- Wong, K.C.W.; Johnson, D.; Hui, E.P.; Lam, R.C.T.; Ma, B.B.Y.; Chan, A.T.C. Opportunities and challenges in combining immunotherapy and radiotherapy in head and neck cancers. Cancer Treat. Rev. 2022, 105, 102361. [Google Scholar] [CrossRef]
| Author | Country | Study Design | N° Patients | Lesion Type | Site | Stage | Therapy | Source | Dose | Local Control | Overall Survival (5 Years) | Toxicity |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Lapayre 2000 [14] | France | Retrospective study | 36 | OSCC | Tongue (19) Floor of the mouth (17) | T1(24) T2 (12) | LDR-BT | Ir 192 | 60 Gy | 88.5% | 85% | Necrosis |
| Grabenbauer 2001 [15] | Germany | Retrospective study | 318 | OSCC | Floor of the mouth (99) Tongue (169) Lower lip (19) Tonsil (19) Others (12) | UICC I (61) II (71) III (58) IV (128) | LDR-BT | Ir 192 | 45 Gy | 74% | 54% | Necrosis and osteonecrosis |
| Barrett 2002 [16] | USA | Retrospective study | 20 | OSCC | Tongue | T1N2 (1) T1N3 (1) T2 N0 (2) T2N1 (1) T2N2 (7) T2N3 (1) T3N2 (3) T3N3 (1) T4N3 (3) | BT + EBRT | Ir 192 | 40 Gy | 86% | 30% | NR |
| Hosokawa 2003 [17] | Japan | Retrospective study | 94 | OSCC | Tongue | T1 (29) T2 (65) | LDR-BT + EBRT | Cs 137 | 40Gy | 92.8% | 78.4% | Ulcer |
| Gibbs 2003 [18] | Australia | Prospective study | 41 | OSCC | Tongue | T1N0 (1) T1N2 (5) T1N3 (1) T2N0 (6) T2N1 (3) T2N2 (4) T2N3 (1) T3N0 (2) T3N1 (2) T3N2 (6) T4N0 (4) T4N2 (4) T4N3 (2) | LDR-BT + EBRT | Ir 192 | 26 Gy | 82% | 66% | Mucositis Ulcer |
| Barrett 2004 [19] | USA | Retrospective study | 20 | OSCC | Tongue | T1N2 (1) T1N3 (1) T2N0 (2) T2N1 (1) T2N2 (7) T2N3 (1) T3N2 (3) T2N3 (1) T4N3 (3) | LDR-BT + EBRT | Ir 192 | 25 Gy | 89% | 87% | NR |
| Lapeyre 2004 [20] | France | Retrospective study | 82 | OSCC | Tongue (37) Floor of the mouth (45) | T1N0 (28) T1N1 (1) T2N0 (23) T2N1 (5) T2N2 (1) T3N0 (5) T3N1 (3) T3N2 (2) T4N0 (7) T4N1 (4) T4N2 (2) T4N3 (1) | LDR-BT + EBRT | Ir 192 | 60 Gy | 67% | 44% | Necrosis |
| Umeda 2000 [21] | Japan | Retrospective study | 175 | OSCC | Tongue | I (92) II (83) | LDR-BT, HDR-BT | Rd 226 Cs 137 Ir 192 | 61 Gy 59 Gy | 91% (LDR) 85% (HDR) | 84.0% (LDR) 72.9% (HDR) | Ulcer osteonecrosis |
| Karakoyun-Celik 2005 [22] | Turkey | Cohort study | 122 | OSCC | Tongue (104) Floor of the mouth (10) Tonsil (5) Other (3) | T1 (8) T2 (11) T3 (16) T4 (5) | LDR-BT | Ir 192 Au 198 | 80 Gy | 78% | 62% | Trismus Swallowing dysfunction Chronic throat pain Osteonecrosis |
| Le Scodan 2005 [23] | France | Retrospective study | 44 | OSCC | Tonsil (10) Soft palate (8) Tonsil soft palate (26) | T1N0 (29) T1N1 (1) T1N2 (1) T2N0 (12) T2N1 (1) | LDR-BT | Ir 192 | 66 Gy | 98% | 76% | Necrosis |
| Ihara 2005 [24] | Japan | Retrospective study | 117 | OSCC | Tongue | T1N1 (1) T2N1 (28) T3N0 (68) T3N1 (20) | LDR-BT | Au 198/Rn-222 (21) Cs-137/Ra-226 (63) Ir 192 (33) | 70 Gy | NR | 50% | Mucositis |
| Kakimoto 2006 [25] | Japan | Randomized controlled trial | 71 | OSCC | Tongue | T1N0 (28) T2N0 (43) | HDR-BT | NR | 57 Gy | 94% | 81% | Necrosis |
| Lock 2011 [26] | UK | Retrospective study | 51 | OSCC | Lip | T1 (46) T2 (5) | LDR-BT | Au 198 | 55 Gy | 97.9% | 87.9% | Swelling and dry skin |
| Tuček 2011 [27] | Czech Republic | Retrospective study | 20 | OSCC | Tongue | T1 (16) T2 (4) | HDR-BT | Ir 192 | 3 Gy twice a day | 85% | 75% | Necrosis and osteonecrosis |
| Chatani 2012 [28] | Japan | Retrospective study | 9 | OSCC | Oral floor (6) Gingiva (2) Soft palate (1) | T1N0 (7) T2N0 (2) | HDR-BT | GBq 370 Ir 192 | 9-24 Gy | 100% | 100% | Ulcer |
| Ghadjar 2012 [29] | Switzerland | Retrospective study | 103 | OSCC | Lip | T1 (20; 43) T2 (9; 25) T3 (3; 9) | LDR-BT + HDR-BT | Ir 192 | 60 Gy LDR 3.5 Gy HDR | 93% | 77% | Dermatitis (49%), pain (42%), mucositis (41%). |
| Rio 2013 [30] | France | Retrospective study | 89 | OSCC | Lip | T1 (44) T2 (33) T3 (2) | LDR-BT | Ir 192 | 58 Gy | 95% | 82% | Desquamation |
| Stannard 2014 [31] | Africa | Retrospective study | 112 | OSCC | Tongue (54) Soft palate (25) Floor of the mouth (21) Tonsil (10) | T1 (46) T2 (56) T3 (10) | LDR-BT | I 125 | 0.5 Gy | 80.7% | 74.3% | Ulcer |
| Feldman 2014 [32] | Israel | Retrospective study | 7 | OSCC | Lip | T2 (7) | HDR-BT | Ir 192 | 25-42 Gy | 90% | NR | Mucositis and lip edema |
| Guinot 2014 [33] | Spain | Retrospective study | 102 | OSCC | Lip | T1 (54) T2 (33) T4 (15) | HDR-BT | Ir 192 | 4.5 Gy | 95% | 85% | Telan- giectasia |
| Goineau 2015 [34] | France | Retrospective study | 112 | OSCC | Tongue | T1N0(55) T2N0 (40) T1N1 (1) T2N1 (10) T2N2 (5) | LDR-BT | Ir 192 | 50-55 Gy | 79% | 72% | Necrosis and chronic pain |
| Kazemian 2017 [35] | Iran | Retrospective study | 78 | OSCC | Tongue (70) Floor of the mouth (4) Lips (2) Buccal mucosa (2) | T1N0 (42) T1N1 (7) T2N0 (14) T2N1 (8) T3N0 (5) T3N1 (2) | HDR-BT + EBRT | Ir 192 | 39 Gy (HDR) 15 Gy (HDR+EBRT) | 90% | 83% | Trismus catheter insertion site fibrosis. |
| Jie 2018 [36] | China | Retrospective study | 76 | OSCC | Tongue (27) Gingiva (19) Buccal mucosa (8) Floor of the mouth (8) Others (14) | T1 (27) T2 (24) T3 (25) | LDR-BT | I 125 | 60-160 Gy | 95.3% | 81.5% | Necrosis |
| Vedasoundaram 2020 [37] | India | Retrospective study | 125 | OSCC | Tongue (75) Buccal mucosa (43) Floor of the mouth (7) | T1 (15) T2 (53) T3 (57) | HDR-BT + EBRT | Ir 192 | 21 Gy | 80% | 83% | Mucositis and ulcer |
| Takácsi-Nagy 2022 [38] | Hungary | Retrospective study | 45 | OSCC | Tongue | T1 (21) T2 (22) T3 (2) | HDR-BT | Ir 192 GBq 370 | 29 Gy | 85% | 73% | Mucositis and ulcer |
| Schweizer 2025 [39] | Germany | s | 217 | OSCC | Tongue (115) Floor of the mouth (102) | T1 (72) T2 (107) T3 (34) T4 (4) | HDR-BT | Ir 192 | 34.2 Gy | 89.7% | 94% | Necrosis and osteonecrosis |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Esperouz, F.; Lorusso, M.; De Lillo, A.; Zhurakivska, K.; Lo Muzio, L.; Ciavarella, D.; Lo Russo, L. The Role of Brachytherapy in the Management of Oral Squamous Cell Carcinoma: A Systematic Review. J. Clin. Med. 2025, 14, 6033. https://doi.org/10.3390/jcm14176033
Esperouz F, Lorusso M, De Lillo A, Zhurakivska K, Lo Muzio L, Ciavarella D, Lo Russo L. The Role of Brachytherapy in the Management of Oral Squamous Cell Carcinoma: A Systematic Review. Journal of Clinical Medicine. 2025; 14(17):6033. https://doi.org/10.3390/jcm14176033
Chicago/Turabian StyleEsperouz, Fariba, Mauro Lorusso, Alfredo De Lillo, Khrystyna Zhurakivska, Lorenzo Lo Muzio, Domenico Ciavarella, and Lucio Lo Russo. 2025. "The Role of Brachytherapy in the Management of Oral Squamous Cell Carcinoma: A Systematic Review" Journal of Clinical Medicine 14, no. 17: 6033. https://doi.org/10.3390/jcm14176033
APA StyleEsperouz, F., Lorusso, M., De Lillo, A., Zhurakivska, K., Lo Muzio, L., Ciavarella, D., & Lo Russo, L. (2025). The Role of Brachytherapy in the Management of Oral Squamous Cell Carcinoma: A Systematic Review. Journal of Clinical Medicine, 14(17), 6033. https://doi.org/10.3390/jcm14176033











