Image-Based Robotic Unicompartmental Knee Arthroplasty Results in Fewer Radiologic Outliers with No Impact on Revision Rates Compared to Imageless Systems: A Systematic Review
Abstract
1. Introduction
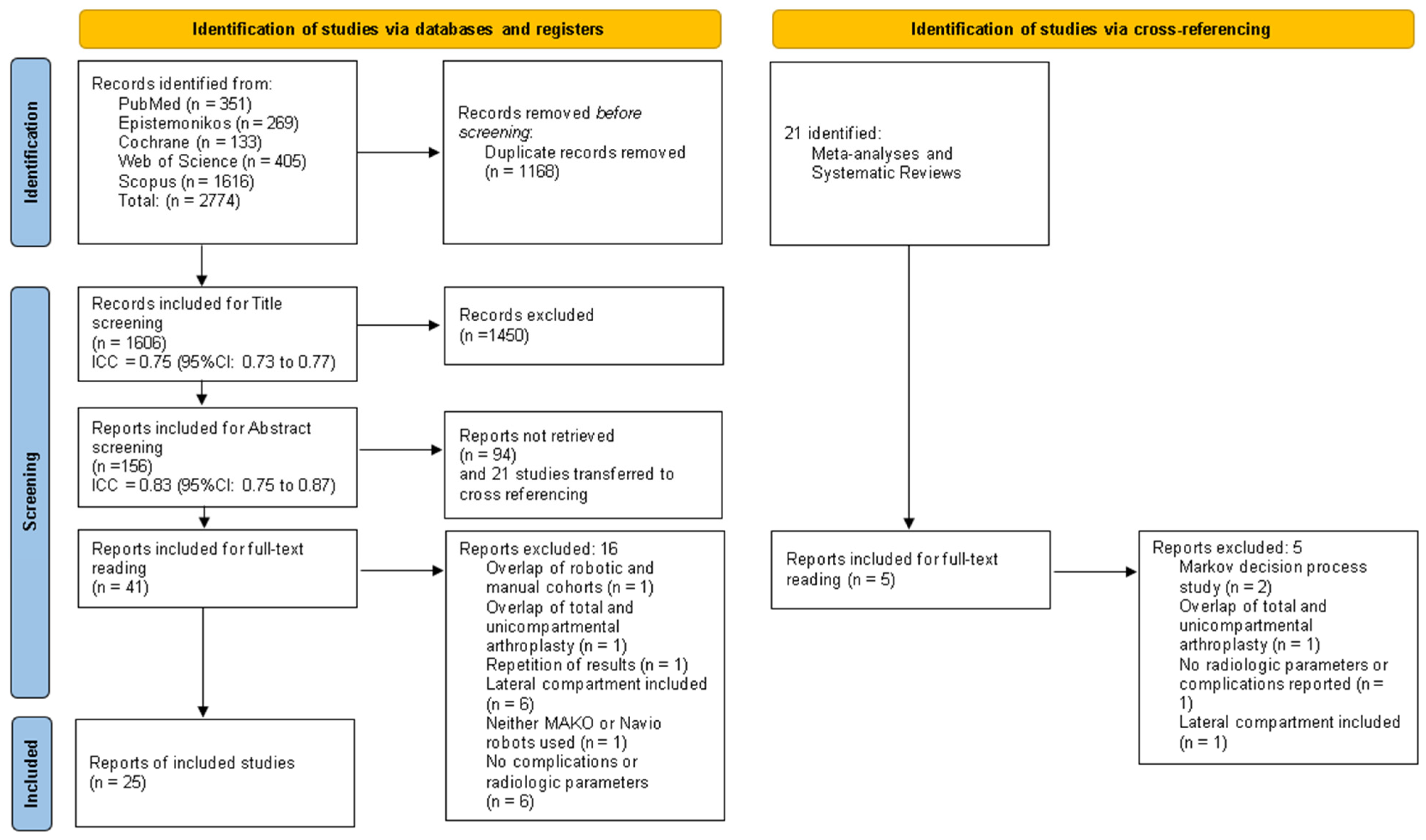
2. Materials and Methods
2.1. Information Sources and Eligibility Criteria
2.2. Data Extraction and Analysis
2.3. Study Quality, Bias, and Characteristics
2.4. Data Collection Process and Data Items
2.5. Statistical Analysis and Data Synthesis
3. Results
3.1. Patient Demographics
3.2. Planning Methodology and Measurements
3.3. Preoperative Radiologic Measurements
3.4. Postoperative Radiologic Measurements
3.5. Outliers
3.6. Revision Rate Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
References
- Wilson, H.A.; Middleton, R.; Abram, S.G.F.; Smith, S.; Alvand, A.; Jackson, W.F.; Bottomley, N.; Hopewell, S.; Price, A.J. Patient Relevant Outcomes of Unicompartmental versus Total Knee Replacement: Systematic Review and Meta-Analysis. BMJ 2019, 364, l352. [Google Scholar] [CrossRef]
- Di Martino, A.; Bordini, B.; Barile, F.; Ancarani, C.; Digennaro, V.; Faldini, C. Unicompartmental Knee Arthroplasty Has Higher Revisions than Total Knee Arthroplasty at Long Term Follow-up: A Registry Study on 6453 Prostheses. Knee Surg. Sports Traumatol. Arthrosc. 2021, 29, 3323–3329. [Google Scholar] [CrossRef] [PubMed]
- Kamenaga, T.; Hiranaka, T.; Hida, Y.; Nakano, N.; Kuroda, Y.; Tsubosaka, M.; Hayashi, S.; Kuroda, R.; Matsumoto, T. Lateral Osteoarthritis Progression Is Associated with a Postoperative Residual Tibiofemoral Subluxation in Oxford UKA. Knee Surg. Sports Traumatol. Arthrosc. 2022, 30, 3236–3243. [Google Scholar] [CrossRef]
- Barbadoro, P.; Ensini, A.; Leardini, A.; d’Amato, M.; Feliciangeli, A.; Timoncini, A.; Amadei, F.; Belvedere, C.; Giannini, S. Tibial Component Alignment and Risk of Loosening in Unicompartmental Knee Arthroplasty: A Radiographic and Radiostereometric Study. Knee Surg. Sports Traumatol. Arthrosc. 2014, 22, 3157–3162. [Google Scholar] [CrossRef]
- Jenny, J.; Boeri, C. Unicompartmental Knee Prosthesis Implantation with a Non-image-based Navigation System: Rationale, Technique, Case-control Comparative Study with a Conventional Instrumented Implantation. Knee Surg. Sports Traumatol. Arthrosc. 2003, 11, 40–45. [Google Scholar] [CrossRef] [PubMed]
- Klasan, A.; Carter, M.; Holland, S.; Young, S.W. Low Femoral Component Prominence Negatively Influences Early Revision Rate in Robotic Unicompartmental Knee Arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 2020, 28, 3906–3911. [Google Scholar] [CrossRef] [PubMed]
- Lonner, J.H.; Seidenstein, A.D.; Charters, M.A.; North, W.T.; Cafferky, N.L.; Durbhakula, S.M.; Kamath, A.F. Improved Accuracy and Reproducibility of a Novel CT-free Robotic Surgical Assistant for Medial Unicompartmental Knee Arthroplasty Compared to Conventional Instrumentation: A Cadaveric Study. Knee Surg. Sports Traumatol. Arthrosc. 2022, 30, 2759–2767. [Google Scholar] [CrossRef]
- Batailler, C.; Bordes, M.; Lording, T.; Nigues, A.; Servien, E.; Calliess, T.; Lustig, S. Improved Sizing with Image-Based Robotic-Assisted System Compared to Image-Free and Conventional Techniques in Medial Unicompartmental Knee Arthroplasty: A Case Control Study. Bone Jt. J. 2021, 103-B, 610–618. [Google Scholar] [CrossRef]
- Robinson, P.G.; Clement, N.D.; Hamilton, D.; Blyth, M.J.G.; Haddad, F.S.; Patton, J.T. A Systematic Review of Robotic-Assisted Unicompartmental Knee Arthroplasty: Prosthesis Design and Type Should Be Reported. Bone Jt. J. 2019, 101-B, 838–847. [Google Scholar] [CrossRef]
- Haffar, A.; Krueger, C.A.; Goh, G.S.; Lonner, J.H. UKA with a Handheld Robotic Device Results in Greater Surgeon Physiological Stress than Conventional Instrumentation. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 777–785. [Google Scholar] [CrossRef]
- Zambianchi, F.; Seracchioli, S.; Franceschi, G.; Cuoghi Costantini, R.; Malatesta, A.; Barbo, G.; Catani, F. Image-based Robotic-arm Assisted Unicompartmental Knee Arthroplasty Provides High Survival and Good-to-excellent Clinical Outcomes at Minimum 10 Years Follow-up. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 5477–5484. [Google Scholar] [CrossRef]
- Negrín, R.; Duboy, J.; Reyes, N.O.; Barahona, M.; Iñiguez, M.; Infante, C.; Cordero, J.A.; Sepulveda, V.; Ferrer, G. Robotic-assisted Unicompartmental Knee Arthroplasty Optimizes Joint Line Restitution Better than Conventional Surgery. J. Exp. Orthop. 2020, 7, 94. [Google Scholar] [CrossRef]
- Avram, G.M.; Tomescu, H.; Dennis, C.; Rusu, V.; Mengis, N.; Ammann, E.; Pacchiarotti, G.; Hirschmann, M.T.; Predescu, V.; Russu, O. Robotic-Assisted Medial Unicompartmental Knee Arthroplasty Provides Better FJS-12 Score and Lower Mid-Term Complication Rates Compared to Conventional Implantation: A Systematic Review and Meta-Analysis. J. Pers. Med. 2024, 14, 1137. [Google Scholar] [CrossRef]
- Gaggiotti, S.; Foissey, C.; Pineda, T.; Batailler, C.; Gaggiotti, G.; Gaggiotti, S.; Servien, E.; Lustig, S. Enhancing Robotic Precision in Medial UKA: Image-based Robot-assisted System Had Higher Accuracy in Implant Positioning than Imageless Robot-assisted System across 292 Knees. Knee Surg. Sports Traumatol. Arthrosc. 2024, 32, 2097–2106. [Google Scholar] [CrossRef]
- Jones, G.G.; Clarke, S.; Harris, S.; Jaere, M.; Aldalmani, T.; De Klee, P.; Cobb, J.P. A Novel Patient-Specific Instrument Design Can Deliver Robotic Level Accuracy in Unicompartmental Knee Arthroplasty. Knee 2019, 26, 1421–1428. [Google Scholar] [CrossRef] [PubMed]
- Yeung, M.H.Y.; Fu, H.; Cheung, A.; Kwan, V.C.W.; Cheung, M.H.; Chan, P.K.; Chiu, K.Y.; Yan, C.H. Robotic Arm-Assisted Unicondylar Knee Arthroplasty Resulted in Superior Radiological Accuracy: A Propensity Score-Matched Analysis. Arthroplasty 2023, 5, 55. [Google Scholar] [CrossRef]
- Batailler, C.; White, N.; Ranaldi, F.M.; Neyret, P.; Servien, E.; Lustig, S. Improved Implant Position and Lower Revision Rate with Robotic-Assisted Unicompartmental Knee Arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 2019, 27, 1232–1240. [Google Scholar] [CrossRef] [PubMed]
- Mergenthaler, G.; Batailler, C.; Lording, T.; Servien, E.; Lustig, S. Is Robotic-assisted Unicompartmental Knee Arthroplasty a Safe Procedure? A Case Control Study. Knee Surg. Sports Traumatol. Arthrosc. 2021, 29, 931–938. [Google Scholar] [CrossRef]
- Omari, A.; Ingelsrud, L.H.; Bandholm, T.Q.; Lentz, S.I.; Troelsen, A.; Gromov, K. What Is the Effect of Supervised Rehabilitation Regime vs. Self-Management Instruction Following Unicompartmental Knee Arthroplasty?—A Pilot Study in Two Cohorts. J. Exp. Orthop. 2021, 8, 38. [Google Scholar] [CrossRef] [PubMed]
- Tay, M.L.; Bolam, S.M.; Monk, A.P.; McGlashan, S.R.; Young, S.W.; Matthews, B.G. Better Post-operative Outcomes at 1-year Follow-up Are Associated with Lower Levels of Pre-operative Synovitis and Higher Levels of IL-6 and VEGFA in Unicompartmental Knee Arthroplasty Patients. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 4109–4116. [Google Scholar] [CrossRef]
- Bernard, C.D.; Pareek, A.; Sabbag, C.M.; Parkes, C.W.; Krych, A.J.; Cummings, N.M.; Dahm, D.L. Pre-operative Patella Alta Does Not Affect Midterm Clinical Outcomes and Survivorship of Patellofemoral Arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 2021, 29, 1670–1677. [Google Scholar] [CrossRef]
- Gaggiotti, S.; Foissey, C.; Rossi, V.; Batailler, C.; Gaggiotti, G.; Gaggiotti, S.; Servien, E.; Lustig, S. Valgus Stress Knee Radiographs Accurately Anticipate the Bone Resection in Medial Unicompartmental Knee Arthroplasty: Protocol Validation Using an Image-based Robotic System. Knee Surg. Sports Traumatol. Arthrosc. 2025, 33, 286–295. [Google Scholar] [CrossRef]
- Wong, J.; Murtaugh, T.; Lakra, A.; Cooper, H.J.; Shah, R.P.; Geller, J.A. Robotic-Assisted Unicompartmental Knee Replacement Offers No Early Advantage over Conventional Unicompartmental Knee Replacement. Knee Surg. Sports Traumatol. Arthrosc. 2019, 27, 2303–2308. [Google Scholar] [CrossRef]
- Jiao, X.; Du, M.; Li, Q.; Huang, C.; Ding, R.; Wang, W. Does Patient-Specific Instrument or Robot Improve Imaging and Functional Outcomes in Unicompartmental Knee Arthroplasty? A Bayesian Analysis. Arch. Orthop. Trauma Surg. 2024, 144, 4827–4838. [Google Scholar] [CrossRef] [PubMed]
- Wan, X.; Wang, W.; Liu, J.; Tong, T. Estimating the Sample Mean and Standard Deviation from the Sample Size, Median, Range and/or Interquartile Range. BMC Med. Res. Methodol. 2014, 14, 135. [Google Scholar] [CrossRef] [PubMed]
- Wu, C.; Fukui, N.; Lin, Y.-K.; Lee, C.-Y.; Chou, S.-H.; Huang, T.-J.; Chen, J.-Y.; Wu, M.-H. Comparison of Robotic and Conventional Unicompartmental Knee Arthroplasty Outcomes in Patients with Osteoarthritis: A Retrospective Cohort Study. J. Clin. Med. 2021, 11, 220. [Google Scholar] [CrossRef]
- Çabuk, H.; Turan, K.; Görkem Muratoğlu, O.; Ergün, T.; Öztürk, Ç.; Erden Ertürer, R. Comparison of the Radiological Parameters between Dynamic-Referencing Tactile Guidance Robotic System and Microplasty® Instrumentation in Unicompartmental Knee Arthroplasty. Jt. Dis. Relat. Surg. 2022, 33, 580–587. [Google Scholar] [CrossRef] [PubMed]
- Park, K.K.; Han, C.D.; Yang, I.-H.; Lee, W.-S.; Han, J.H.; Kwon, H.M. Robot-Assisted Unicompartmental Knee Arthroplasty Can Reduce Radiologic Outliers Compared to Conventional Techniques. PLoS ONE 2019, 14, e0225941. [Google Scholar] [CrossRef]
- Hansen, D.C.; Kusuma, S.K.; Palmer, R.M.; Harris, K.B. Robotic Guidance Does Not Improve Component Position or Short-Term Outcome in Medial Unicompartmental Knee Arthroplasty. J. Arthroplast. 2014, 29, 1784–1789. [Google Scholar] [CrossRef]
- MacCallum, K.P.; Danoff, J.R.; Geller, J.A. Tibial Baseplate Positioning in Robotic-Assisted and Conventional Unicompartmental Knee Arthroplasty. Eur. J. Orthop. Surg. Traumatol. 2016, 26, 93–98. [Google Scholar] [CrossRef]
- Kazarian, G.S.; Barrack, R.L.; Barrack, T.N.; Lawrie, C.M.; Nunley, R.M. Radiological Outcomes Following Manual and Robotic-Assisted Unicompartmental Knee Arthroplasty. Bone Jt. Open 2021, 2, 191–197. [Google Scholar] [CrossRef] [PubMed]
- Thilak, J.; Thadi, M.; Mane, P.P.; Sharma, A.; Mohan, V.; Babu, B.C. Accuracy of Tibial Component Positioning in the Robotic Arm Assisted versus Conventional Unicompartmental Knee Arthroplasty. J. Orthop. 2020, 22, 367–371. [Google Scholar] [CrossRef]
- Kwon, S.C.; Jung, H.J.; Lee, J.H.; Hyun, J.T.; Hwang, J.H.; Kim, J.I. Robotic-assisted Medial Unicompartmental Knee Arthroplasty Restored Prearthritic Alignment and Led to Superior Functional Outcomes Compared with Conventional Techniques. Knee Surg. Sports Traumatol. Arthrosc. 2024, 33, 265–273. [Google Scholar] [CrossRef]
- Bell, S.W.; Anthony, I.; Jones, B.; MacLean, A.; Rowe, P.; Blyth, M. Improved Accuracy of Component Positioning with Robotic-Assisted Unicompartmental Knee Arthroplasty: Data from a Prospective, Randomized Controlled Study. J. Bone Jt. Surg. 2016, 98, 627–635. [Google Scholar] [CrossRef] [PubMed]
- Kayani, B.; Konan, S.; Tahmassebi, J.; Rowan, F.E.; Haddad, F.S. An Assessment of Early Functional Rehabilitation and Hospital Discharge in Conventional versus Robotic-Arm Assisted Unicompartmental Knee Arthroplasty: A Prospective Cohort Study. Bone Jt. J. 2019, 101-B, 24–33. [Google Scholar] [CrossRef]
- Lonner, J.H.; John, T.K.; Conditt, M.A. Robotic Arm-Assisted UKA Improves Tibial Component Alignment: A Pilot Study. Clin. Orthop. Relat. Res. 2010, 468, 141–146. [Google Scholar] [CrossRef]
- Gilmour, A.; MacLean, A.D.; Rowe, P.J.; Banger, M.S.; Donnelly, I.; Jones, B.G.; Blyth, M.J.G. Robotic-Arm–Assisted vs Conventional Unicompartmental Knee Arthroplasty. The 2-Year Clinical Outcomes of a Randomized Controlled Trial. J. Arthroplast. 2018, 33, S109–S115. [Google Scholar] [CrossRef]
- Clement, N.D.; Fraser, E.; Gilmour, A.; Doonan, J.; MacLean, A.; Jones, B.G.; Blyth, M.J.G. Cost-Utility Analysis of Robotic Arm-Assisted Medial Compartment Knee Arthroplasty: Five-Year Data from a Randomized Controlled Trial. Bone Jt. Open 2023, 4, 889–899. [Google Scholar] [CrossRef]
- Banger, M.; Doonan, J.; Rowe, P.; Jones, B.; MacLean, A.; Blyth, M.J.B. Robotic Arm-Assisted versus Conventional Medial Unicompartmental Knee Arthroplasty: Five-Year Clinical Outcomes of a Randomized Controlled Trial. Bone Jt. J. 2021, 103-B, 1088–1095. [Google Scholar] [CrossRef] [PubMed]
- Herry, Y.; Batailler, C.; Lording, T.; Servien, E.; Neyret, P.; Lustig, S. Improved Joint-Line Restitution in Unicompartmental Knee Arthroplasty Using a Robotic-Assisted Surgical Technique. Int. Orthop. 2017, 41, 2265–2271. [Google Scholar] [CrossRef]
- Negrín, R.; Duboy, J.; Iñiguez, M.; Reyes, N.O.; Barahona, M.; Ferrer, G.; Infante, C.; Jabes, N. Robotic-Assisted vs Conventional Surgery in Medial Unicompartmental Knee Arthroplasty: A Clinical and Radiological Study. Knee Surg. Relat. Res. 2021, 33, 5. [Google Scholar] [CrossRef] [PubMed]
- Foissey, C.; Batailler, C.; Vahabi, A.; Fontalis, A.; Servien, E.; Lustig, S. Better Accuracy and Implant Survival in Medial Imageless Robotic-Assisted Unicompartmental Knee Arthroplasty Compared to Conventional Unicompartmental Knee Arthroplasty: Two- to Eleven-Year Follow-up of Three Hundred Fifty-Six Consecutive Knees. Int. Orthop. 2023, 47, 533–541. [Google Scholar] [CrossRef]
- Ashok Kumar, P.S.; Pawar, S.; Kanniyan, K.; Pichai, S.; Bose, V.C.; Patil, S. Does Robotic-Assisted Unicompartmental Knee Arthroplasty Restore Native Joint Line More Accurately than with Conventional Instruments? J. Robot. Surg. 2024, 18, 49. [Google Scholar] [CrossRef]
- Batailler, C.; Lording, T.; Naaim, A.; Servien, E.; Cheze, L.; Lustig, S. No Difference of Gait Parameters in Patients with Image-Free Robotic-Assisted Medial Unicompartmental Knee Arthroplasty Compared to a Conventional Technique: Early Results of a Randomized Controlled Trial. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 803–813. [Google Scholar] [CrossRef]
- Goh, G.S.; Haffar, A.; Tarabichi, S.; Courtney, P.M.; Krueger, C.A.; Lonner, J.H. Robotic-Assisted Versus Manual Unicompartmental Knee Arthroplasty: A Time-Driven Activity-Based Cost Analysis. J. Arthroplast. 2022, 37, 1023–1028. [Google Scholar] [CrossRef]
- Crizer, M.P.; Haffar, A.; Battenberg, A.; McGrath, M.; Sutton, R.; Lonner, J.H. Robotic Assistance in Unicompartmental Knee Arthroplasty Results in Superior Early Functional Recovery and Is More Likely to Meet Patient Expectations. Adv. Orthop. 2021, 2021, 1–8. [Google Scholar] [CrossRef]
- Rivière, C.; Sivaloganathan, S.; Villet, L.; Cartier, P.; Lustig, S.; Vendittoli, P.; Cobb, J. Kinematic Alignment of Medial UKA Is Safe: A Systematic Review. Knee Surg. Sports Traumatol. Arthrosc. 2022, 30, 1082–1094. [Google Scholar] [CrossRef]
- Ruderman, L.V.; Bayoumi, T.; Ten Noever De Brauw, G.V.; Lan, R.; Nguyen, J.T.; Pearle, A.D. Robotic-arm-assisted Lateral Unicompartmental Knee Arthroplasty Leads to High Implant Survival and Patient Satisfaction at Mean 10-year Follow-up. Knee Surg. Sports Traumatol. Arthrosc. 2024, 32, 2297–2308. [Google Scholar] [CrossRef]
- Leelasestaporn, C.; Tarnpichprasert, T.; Arirachakaran, A.; Kongtharvonskul, J. Comparison of 1-Year Outcomes between MAKO versus NAVIO Robot-Assisted Medial UKA: Nonrandomized, Prospective, Comparative Study. Knee Surg. Relat. Res. 2020, 32, 13. [Google Scholar] [CrossRef] [PubMed]
- Porcelli, P.; Marmotti, A.; Bellato, E.; Colombero, D.; Ferrero, G.; Agati, G.; Calò, M.; Ferraris, C.; Pautasso, A.; Castoldi, F. Comparing Different Approaches in Robotic-Assisted Surgery for Unicompartmental Knee Arthroplasty: Outcomes at a Short-Term Follow-up of MAKO versus NAVIO System. J. Biol. Regul. Homeost. Agents. 2020, 34, 393–404. [Google Scholar] [PubMed]
- Luyckx, T.; Bori, E.; Saldari, R.; Fiore, S.; Altamore, V.; Innocenti, B. Effect of Design and Surgical Parameters Variations in Mobile-bearing versus Fixed-bearing Unicompartmental Knee Arthroplasty: A Finite Element Analysis. J. Exp. Orthop. 2024, 11, e70053. [Google Scholar] [CrossRef]
- Diquattro, E.; Lettner, J.; Adriani, M.; Prill, R.; Salzmann, M.; Becker, R. High Accuracy of Component Positioning and Restoration of Lower Limb Alignment Using Robotic Medial Unicompartmental Knee Arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 2025, 33, 1982–1991. [Google Scholar] [CrossRef]
- Gifstad, T.; Nordskar, J.J.; Egeberg, T.; Wik, T.S.; Winther, S.B. Cementless Unicompartmental Knee Arthroplasty Results in Higher Pain Levels Compared to the Cemented Technique: A Prospective Register Study. Knee Surg. Sports Traumatol. Arthrosc. 2022, 30, 2738–2743. [Google Scholar] [CrossRef]
- Hirschmann, M.T.; Avram, G.; Graichen, H.; Tandogan, R.N.; Mengis, N.; Zaffagnini, S. Same Same but Different—Image-based versus Imageless Robotic-assisted Total Knee Arthroplasty! J. Exp. Orthop. 2024, 11, e70062. [Google Scholar] [CrossRef] [PubMed]
- Fitzpatrick, C.; FitzPatrick, D.; Lee, J.; Auger, D. Statistical Design of Unicompartmental Tibial Implants and Comparison with Current Devices. Knee 2007, 14, 138–144. [Google Scholar] [CrossRef]
- Kim, M.-K.; Yoon, J.-R.; Yang, S.-H.; Shin, Y.-S. Unicompartmental Knee Arthroplasty Fails to Completely Restore Normal Gait Patterns during Level Walking. Knee Surg. Sports Traumatol. Arthrosc. 2018, 26, 3280–3289. [Google Scholar] [CrossRef] [PubMed]
- Woiczinski, M.; Schröder, C.; Paulus, A.; Kistler, M.; Jansson, V.; Müller, P.E.; Weber, P. Varus or Valgus Positioning of the Tibial Component of a Unicompartmental Fixed-Bearing Knee Arthroplasty Does Not Increase Wear. Knee Surg. Sports Traumatol. Arthrosc. 2020, 28, 3016–3021. [Google Scholar] [CrossRef] [PubMed]
- Mofidi, A.; Plate, J.F.; Lu, B.; Conditt, M.A.; Lang, J.E.; Poehling, G.G.; Jinnah, R.H. Assessment of Accuracy of Robotically Assisted Unicompartmental Arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 2014, 22, 1918–1925. [Google Scholar] [CrossRef]
- Perazzini, P.; Sembenini, P.; Alberton, F.; Cochetti, A.; Innocenti, B.; Bori, E. Robotic-assisted Partial Knee Surgery Performances: A 10-year Follow-up Retrospective Study. Knee Surg. Sports Traumatol. Arthrosc. 2025, 33, 2197–2203. [Google Scholar] [CrossRef]
| Image-Based | Imageless | p-Value | |
|---|---|---|---|
| Total Included | 970 [8,16,23,26,27,28,29,30,31,32,33,34,35,36,37,38,39] | 652 [8,17,40,41,42,43,44,45,46] | - |
| Age * (years) | 64.2 (8.7) [8,23,26,27,28,29,31,32,33,34,35,36,37,38] | 64.2 (9) [8,17,41,42,43,44,45,46] | 1 |
| Gender (M/F) (%) | 42.8/57.2 [8,23,26,27,28,29,32,33,35,36,37,38] | 47.6/52.4 [8,41,42,43,44,45,46] | - |
| Operative Time * (minutes) | 90.7 (18) [16,26,29,30] | 80.7 (15.2) [41,42,45] | <0.001 |
| BMI * | 28.4 (4.4) [8,23,28,29,31,33,35,36] | 27.8 (4) [8,17,42,44,45,46] | 0.023 |
| Image-Based | Imageless | Mean Difference (95% CI) | p-Value | |
|---|---|---|---|---|
| Preoperative HKA * | 174.6 (3.3) [28,32,33] | 173.9 (2.4) [42,44] | −0.7 (−1.38; −0.02) | 0.044 |
| Preoperative Tibial Slope * | 78.7 (3.2) [26] | 81.8 (2.3) [42] | 3.1 (2.18; 4.03) | <0.001 |
| Postoperative HKA * | 178.7 (2.4) [28,32,33] | 176.6 (2.2) [42,44] | −2.1 (−2.62; −1.58) | <0.001 |
| Postoperative Tibial Slope * | 83.9 (2.3) [16,26,28,29,30,32] | 85.6 (1.9) [17,41,42,44] | 1.7 (1.37; 2.03) | <0.001 |
| Image-Based | Imageless | Mean Difference (95% CI) | p-Value | |
|---|---|---|---|---|
| Femoral Sagittal Angle * | 37.6 (5.4) [26] | 47.8 (4.2) [41] | 10.2 (7.66; 12.74) | <0.001 |
| Tibial Coronal Angle * | 1.4 (2.7) [16,27,28,29,30] | 3.9 (2.5) [42] | 2.5 (2.02; 2.97) | <0.001 |
| Fit Posterior Tibia (mm) * | 3.4 (1.4) [8,27] | 5.1 (1.1) [8] | 1.7 (1.37; 2.03) | <0.001 |
| Fit Posterior Femur (mm) * | 3.4 (1.1) [8,27] | 5.1 (1.2) [8] | 1.7 (1.29; 1.91) | <0.001 |
| Image-Based | Imageless | Log Odds Ratio (95% CI) | p-Value | |
|---|---|---|---|---|
| Outliers HKA (%) | 17.5 [28,32,33] | 28.7 [17,42] | 0.6 (0.09; 1.19) | 0.024 |
| Outliers Joint Line Height (%) | 0 [33] | 31.6 [42,43] | 3.5 (0.69; 6.30) | 0.015 |
| Outliers Femoral Sagittal Angle (%) | 27.8 [31,34] | 25 [41] | −0.1 (−1.33; 1.05) | 0.814 |
| Outliers Fit Medial Tibia (%) | 3.4 [8,31] | 0 [8] | −1.9 (−4.83; 0.94) | 0.186 |
| Outliers Fit Anterior Tibia (%) | 2.8 [8,31] | 1.1 [8] | −1 (−3.13; 1.19) | 0.378 |
| Outliers Fit Posterior Tibia (%) | 4.5 [8,31] | 31.2 [8] | 2.3 (1.44; 3.10) | <0.001 |
| Outliers Fit Posterior Femur (%) | 12.9 [8] | 7.5 [8] | −0.6 (−1.58; 0.38) | 0.231 |
| Image-Based | Imageless | Log Odds Ratio (95% CI) | p-Value | |
|---|---|---|---|---|
| All Follow-up Periods | ||||
| Total Included | 583 [16,23,26,29,30,35,36,37,38,39] | 486 [17,41,42,44,45,46] | - | - |
| Mean Follow-up (months) | 23.7 | 30.5 | - | - |
| Total Revisions (%) | 2.23 | 2.88 | 0.26 (−0.50; 1.03) | 0.501 |
| Revisions to TKA (%) | 0 | 2.06 | 2.78 (−0.06; 5.62) | 0.055 |
| Revisions for Pain (%) | 0.68 | 0.41 | −0.51 (−2.22; 1.19) | 0.554 |
| Revisions for Aseptic Loosening (%) | 1.03 | 1.65 | 0.476 (−0.59; 1.54) | 0.381 |
| Minimum 12 Months Follow-up | ||||
| Total Included | 479 [16,23,26,29,30,37,38,39] | 304 [17,42,46] | - | - |
| Mean Follow-up (months) | 28.2 | 46.5 | - | - |
| Total Revisions (%) | 2.71 | 3.29 | 0.20 (−0.64; 1.04) | 0.643 |
| Revisions to TKA (%) | 0 | 2.96 | 2.82 (−0.03; 5.67) | 0.052 |
| Revisions for Pain (%) | 0.63 | 0.33 | −0.65 (−2.92; 1.62) | 0.576 |
| Revisions for Aseptic Loosening (%) | 1.25 | 2.63 | 0.76 (−0.31; 1.83) | 0.165 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tomescu, H.; Avram, G.M.; Pacchiarotti, G.; Elsheikh, R.; Russu, O.; Nowakowski, A.M.; Hirschmann, M.T.; Predescu, V. Image-Based Robotic Unicompartmental Knee Arthroplasty Results in Fewer Radiologic Outliers with No Impact on Revision Rates Compared to Imageless Systems: A Systematic Review. J. Clin. Med. 2025, 14, 5996. https://doi.org/10.3390/jcm14175996
Tomescu H, Avram GM, Pacchiarotti G, Elsheikh R, Russu O, Nowakowski AM, Hirschmann MT, Predescu V. Image-Based Robotic Unicompartmental Knee Arthroplasty Results in Fewer Radiologic Outliers with No Impact on Revision Rates Compared to Imageless Systems: A Systematic Review. Journal of Clinical Medicine. 2025; 14(17):5996. https://doi.org/10.3390/jcm14175996
Chicago/Turabian StyleTomescu, Horia, George M. Avram, Giacomo Pacchiarotti, Randa Elsheikh, Octav Russu, Andrej M. Nowakowski, Michael T. Hirschmann, and Vlad Predescu. 2025. "Image-Based Robotic Unicompartmental Knee Arthroplasty Results in Fewer Radiologic Outliers with No Impact on Revision Rates Compared to Imageless Systems: A Systematic Review" Journal of Clinical Medicine 14, no. 17: 5996. https://doi.org/10.3390/jcm14175996
APA StyleTomescu, H., Avram, G. M., Pacchiarotti, G., Elsheikh, R., Russu, O., Nowakowski, A. M., Hirschmann, M. T., & Predescu, V. (2025). Image-Based Robotic Unicompartmental Knee Arthroplasty Results in Fewer Radiologic Outliers with No Impact on Revision Rates Compared to Imageless Systems: A Systematic Review. Journal of Clinical Medicine, 14(17), 5996. https://doi.org/10.3390/jcm14175996






