Multisegmented Foot and Lower Limb Kinematics During Gait in Males with Chronic Ankle Instability: Exploring Links with Hip Abductor Strength
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Ethical Approval
2.3. Study Protocol
2.4. Foot Posture Index
2.5. Kinematic Analysis
- Shank: fibular head, lateral malleolus, mid-shank marker
- Foot: posterior calcaneus, 1st and 5th metatarsal heads, virtual metatarsal head
- Calcaneus: posterior calcaneus, peroneal tubercle, sustentaculum tali
- Midfoot: navicular tuberosity, 2nd and 5th metatarsal bases
- Metatarsus: 2nd metatarsal base, 1st and 5th metatarsal heads
- Toe: 1st metatarsal head, proximal phalanx of the hallux
2.6. Hip Abductor Strength Measurement
2.7. Statistical Analysis
3. Results
3.1. Characteristics of Study Population
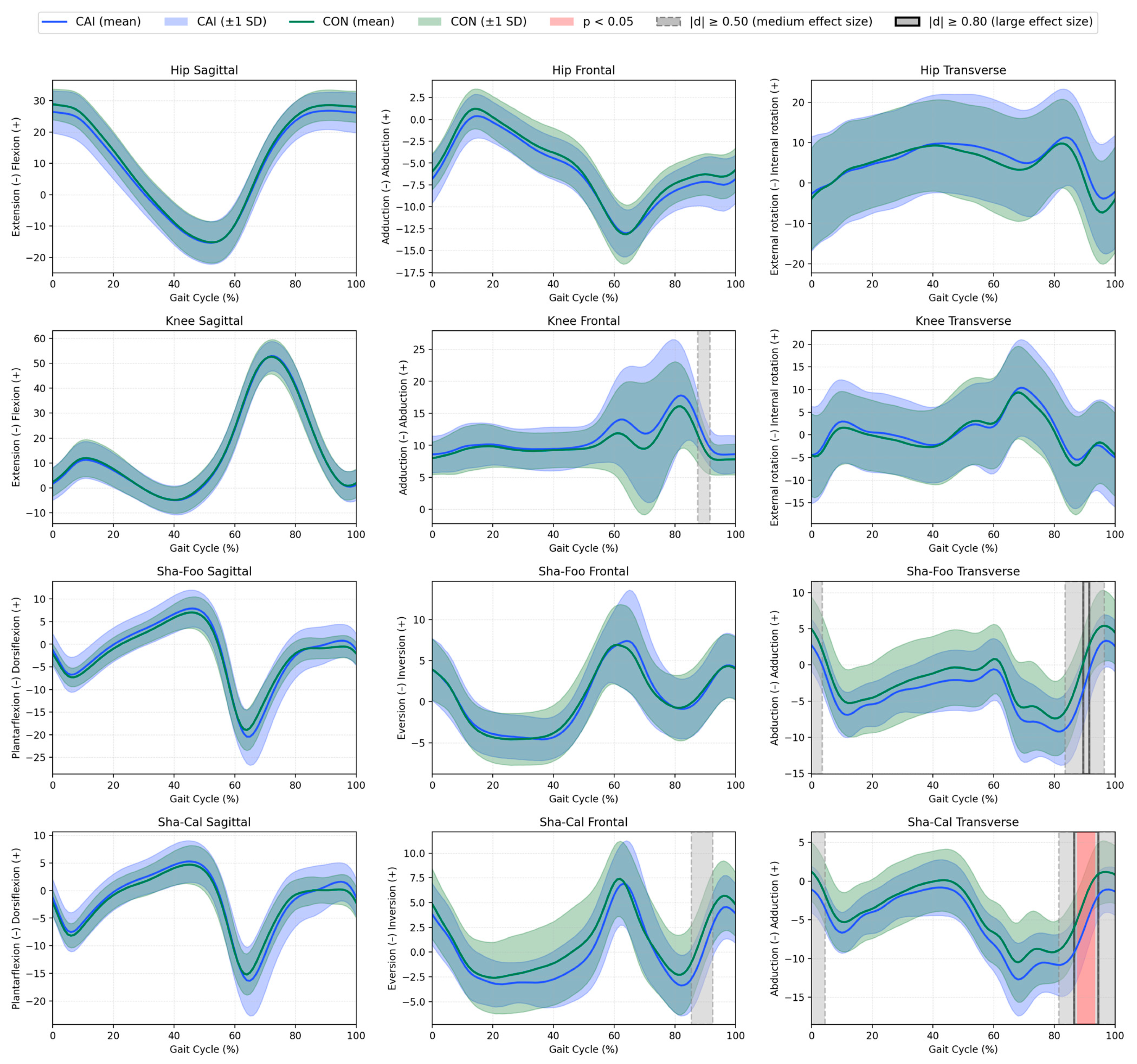
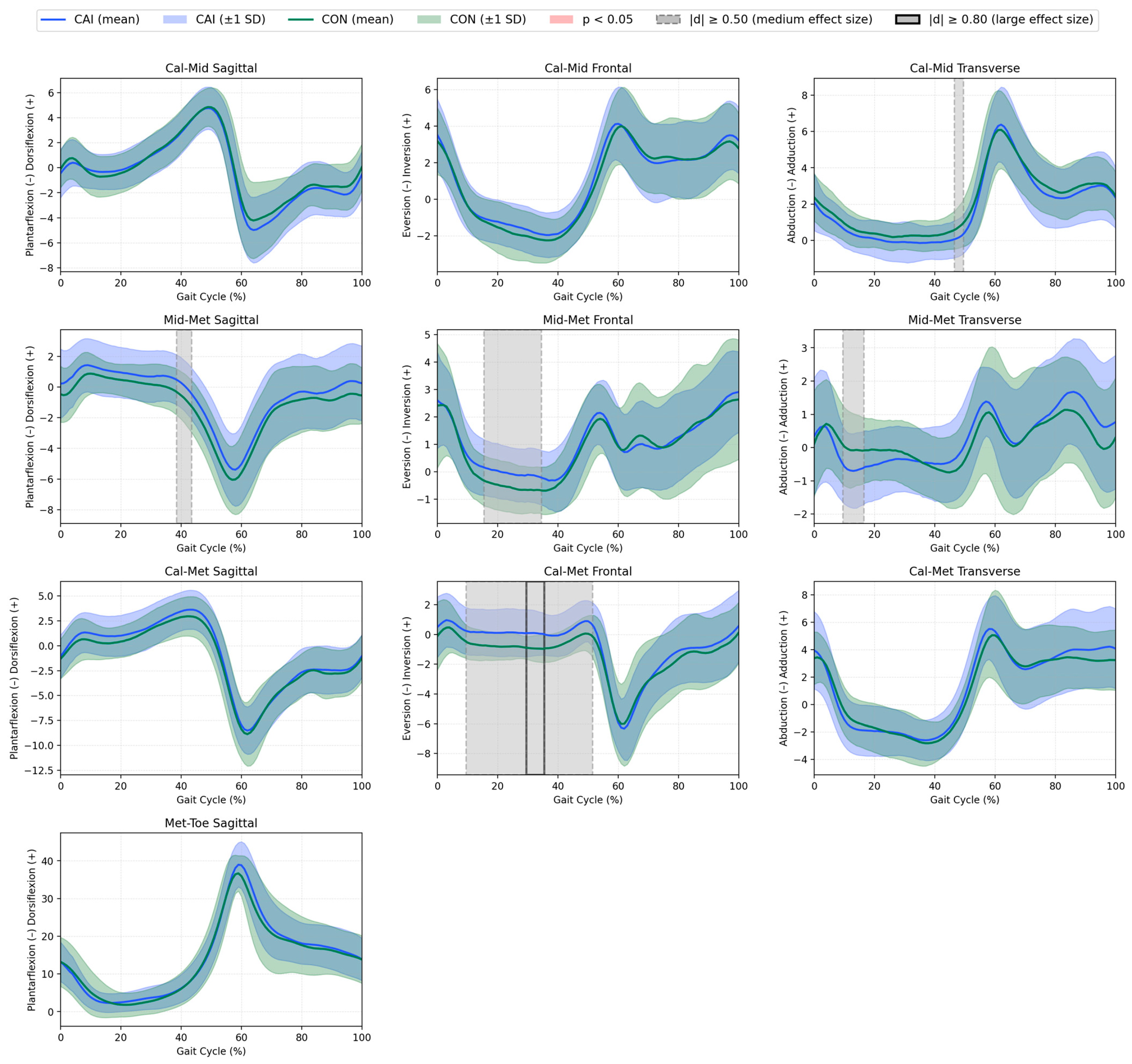
3.2. Curve Analyses
3.3. Correlation Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| BMI | Body Mass Index |
| CAI | Chronic Ankle Instability |
| CAIT-PL | The Polish version of the Cumberland Ankle Instability Tool |
| CON | Control group/Controls |
| CoM | Centre of Mass |
| Cal-Met | Metatarsus (forefoot) relative to the calcaneus (rearfoot) |
| d | Cohen’s d (effect size) |
| EMG | Electromyographic |
| FPI | Foot Posture Index |
| F-ROM | Frontal Plane Range of Motion |
| ICC | Intraclass Correlation Coefficient |
| LAS | Lateral Ankle Sprain |
| MD | Mean Difference |
| Met-Toe | Toe relative to the metatarsus |
| Mid-Met | Metatarsus (forefoot) relative to the midfoot |
| PL | Peroneus Longus |
| ROM | Range of Motion |
| Sha-Cal | Calcaneus (rearfoot) relative to the shank |
| Sha-Foo | Foot in relation to the shank |
| SD | Standard Deviation |
| SPM | Statistical Parametric Mapping |
References
- Waterman, B.R.; Owens, B.D.; Davey, S.; Zacchilli, M.A.; Belmont, P.J. The Epidemiology of Ankle Sprains in the United States. J. Bone Jt. Surg. 2010, 92, 2279–2284. [Google Scholar] [CrossRef] [PubMed]
- Feger, M.A.; Herb, C.C.; Fraser, J.J.; Glaviano, N.; Hertel, J. Supervised Rehabilitation Versus Home Exercise in the Treatment of Acute Ankle Sprains. Clin. Sports Med. 2015, 34, 329–346. [Google Scholar] [CrossRef] [PubMed]
- Lin, C.; Houtenbos, S.; Lu, Y.; Mayer, F.; Wippert, P. The Epidemiology of Chronic Ankle Instability with Perceived Ankle Instability- a Systematic Review. J. Foot Ankle Res. 2021, 14, 41. [Google Scholar] [CrossRef]
- Gribble, P.A.; Bleakley, C.M.; Caulfield, B.M.; Docherty, C.L.; Fourchet, F.; Fong, D.T.-P.; Hertel, J.; Hiller, C.E.; Kaminski, T.W.; McKeon, P.O.; et al. 2016 Consensus Statement of the International Ankle Consortium: Prevalence, Impact and Long-Term Consequences of Lateral Ankle Sprains. Br. J. Sports Med. 2016, 50, 1493–1495. [Google Scholar] [CrossRef] [PubMed]
- Fraser, J.J.; Feger, M.A.; Hertel, J. Clinical Commentary on Midfoot and Forefoot Involvement in Lateral Ankle Sprains and Chronic Ankle Instability. part 2: Clinical Considerations. Int. J. Sports Phys. Ther. 2016, 11, 1191–1203. [Google Scholar] [PubMed]
- Søndergaard, L.; Konradsen, L.; Hølmer, P.; Jørgensen, L.N.; Nielsen, P.T. Acute Midtarsal Sprains: Frequency and Course of Recovery. Foot Ankle Int. 1996, 17, 195–199. [Google Scholar] [CrossRef]
- Deschamps, K.; Staes, F.; Roosen, P.; Nobels, F.; Desloovere, K.; Bruyninckx, H.; Matricali, G.A. Body of Evidence Supporting the Clinical Use of 3D Multisegment Foot Models: A Systematic Review. Gait Posture 2011, 33, 338–349. [Google Scholar] [CrossRef]
- Luan, L.; Orth, D.; Newman, P.; Adams, R.; El-Ansary, D.; Han, J. Do Individuals with Ankle Instability Show Altered Lower Extremity Kinematics and Kinetics during Walking? A Systematic Review and Meta-Analysis. Physiotherapy 2024, 125, 101420. [Google Scholar] [CrossRef]
- Moisan, G.; Descarreaux, M.; Cantin, V. Effects of Chronic Ankle Instability on Kinetics, Kinematics and Muscle Activity during Walking and Running: A Systematic Review. Gait Posture 2017, 52, 381–399. [Google Scholar] [CrossRef]
- Delahunt, E.; Monaghan, K.; Caulfield, B. Altered Neuromuscular Control and Ankle Joint Kinematics during Walking in Subjects with Functional Instability of the Ankle Joint. Am. J. Sports Med. 2006, 34, 1970–1976. [Google Scholar] [CrossRef]
- Monaghan, K.; Delahunt, E.; Caulfield, B. Ankle Function during Gait in Patients with Chronic Ankle Instability Compared to Controls. Clin. Biomech. 2006, 21, 168–174. [Google Scholar] [CrossRef]
- Drewes, L.K.; McKeon, P.O.; Paolini, G.; Riley, P.; Kerrigan, D.C.; Ingersoll, C.D.; Hertel, J. Altered Ankle Kinematics and Shank-Rear-Foot Coupling in Those with Chronic Ankle Instability. J. Sport Rehabil. 2009, 18, 375–388. [Google Scholar] [CrossRef]
- Fraser, J.J.; Hart, J.M.; Saliba, S.F.; Park, J.S.; Tumperi, M.; Hertel, J. Multisegmented Ankle-Foot Kinematics during Gait Initiation in Ankle Sprains and Chronic Ankle Instability. Clin. Biomech. 2019, 68, 80–88. [Google Scholar] [CrossRef] [PubMed]
- Dingenen, B.; Deschamps, K.; Delchambre, F.; Van Peer, E.; Staes, F.F.; Matricali, G.A. Effect of Taping on Multi-Segmental Foot Kinematic Patterns during Walking in Persons with Chronic Ankle Instability. J. Sci. Med. Sport 2017, 20, 835–840. [Google Scholar] [CrossRef]
- De Ridder, R.; Willems, T.; Vanrenterghem, J.; Robinson, M.; Pataky, T.; Roosen, P. Gait Kinematics of Subjects with Ankle Instability Using a Multisegmented Foot Model. Med. Sci. Sports Exerc. 2013, 45, 2129–2136. [Google Scholar] [CrossRef]
- Koldenhoven, R.M.; Hart, J.; Saliba, S.; Abel, M.F.; Hertel, J. Gait Kinematics & Kinetics at Three Walking Speeds in Individuals with Chronic Ankle Instability and Ankle Sprain Copers. Gait Posture 2019, 74, 169–175. [Google Scholar] [CrossRef] [PubMed]
- Huang, D.; Zhang, C.; Song, W.; Gao, J.; Tian, H.; Li, H.; Ke, X.; Jiang, C.; Lin, Z. Gait Variability and Biomechanical Distinctions in Individuals with Functional Ankle Instability: A Case–Control Study Based on Three-Dimensional Motion Analysis. Eur. J. Med. Res. 2025, 30, 493. [Google Scholar] [CrossRef] [PubMed]
- Zheng, J.; Xu, B.; Xiong, X.; Chen, J. Hip Muscle Strength in Patients with Chronic Ankle Instability: A Systematic Review and Meta-Analysis. Phys. Ther. Sport 2025, 75, 48–57. [Google Scholar] [CrossRef]
- DeJong, A.F.; Mangum, L.C.; Hertel, J. Gluteus Medius Activity during Gait Is Altered in Individuals with Chronic Ankle Instability: An Ultrasound Imaging Study. Gait Posture 2019, 71, 7–13. [Google Scholar] [CrossRef]
- DeJong, A.F.; Koldenhoven, R.M.; Hart, J.M.; Hertel, J. Gluteus Medius Dysfunction in Females with Chronic Ankle Instability Is Consistent at Different Walking Speeds. Clin. Biomech. 2020, 73, 140–148. [Google Scholar] [CrossRef]
- Luan, L.; Witchalls, J.; Ganderton, C.; Adams, R.; El-Ansary, D.; Han, J. Is Chronic Ankle Instability Associated with Contractile Thickness of Gluteus Medius and Gluteus Maximus during Functional Movement and Exercise? A Systematic Review and Meta-Analysis. J. Sports Med. Phys. Fit. 2025, 65, 255–266. [Google Scholar] [CrossRef]
- Powers, C.M.; Ghoddosi, N.; Straub, R.K.; Khayambashi, K. Hip Strength as a Predictor of Ankle Sprains in Male Soccer Players: A Prospective Study. J. Athl. Train. 2017, 52, 1048–1055. [Google Scholar] [CrossRef]
- Olszewski, M.; Golec, J.; Zając, B.; Krężałek, P. Isometric and Isokinetic Hip Strength in Males with Chronic Ankle Instability and Its Relationship with Dynamic Balance and Self-Reported Instability. Phys. Ther. Sport 2025, 72, 9–17. [Google Scholar] [CrossRef]
- Olszewski, M.; Zając, B.; Mika, A.; Golec, J. Ankle Dorsiflexion Range of Motion and Hip Abductor Strength Can Predict Lower Quarter Y-Balance Test Performance in Healthy Males. J. Bodyw. Mov. Ther. 2024, 38, 567–573. [Google Scholar] [CrossRef] [PubMed]
- Khalaj, N.; Vicenzino, B.; Smith, M.D. Hip and Knee Muscle Torque and Its Relationship with Dynamic Balance in Chronic Ankle Instability, Copers and Controls. J. Sci. Med. Sport 2021, 24, 647–652. [Google Scholar] [CrossRef] [PubMed]
- McCann, R.S.; Crossett, I.D.; Terada, M.; Kosik, K.B.; Bolding, B.A.; Gribble, P.A. Hip Strength and Star Excursion Balance Test Deficits of Patients with Chronic Ankle Instability. J. Sci. Med. Sport 2017, 20, 992–996. [Google Scholar] [CrossRef] [PubMed]
- Song, K.; Jang, J.; Nolte, T.; Wikstrom, E.A. Dynamic Reach Deficits in Those with Chronic Ankle Instability: A Systematic Review and Meta-Analysis. Phys. Ther. Sport 2022, 53, 40–50. [Google Scholar] [CrossRef]
- Lee, S.-P.; Powers, C.M. Individuals with Diminished Hip Abductor Muscle Strength Exhibit Altered Ankle Biomechanics and Neuromuscular Activation during Unipedal Balance Tasks. Gait Posture 2014, 39, 933–938. [Google Scholar] [CrossRef]
- Bruijn, S.M.; van Dieën, J.H. Control of Human Gait Stability through Foot Placement. J. R. Soc. Interface 2018, 15, 20170816. [Google Scholar] [CrossRef]
- Hof, A.L.; Duysens, J. Responses of Human Hip Abductor Muscles to Lateral Balance Perturbations during Walking. Exp. Brain Res. 2013, 230, 301–310. [Google Scholar] [CrossRef]
- Holmes, S.C.; Montgomery, M.M.; Lynn, S.K.; Pamukoff, D.N. Sex-Specific Associations between Hip Muscle Strength and Foot Progression Angle. J. Electromyogr. Kinesiol. 2023, 68, 102723. [Google Scholar] [CrossRef]
- Gribble, P.A.; Delahunt, E.; Bleakley, C.M.; Caulfield, B.; Docherty, C.L.; Fong, D.T.P.; Fourchet, F.; Hertel, J.; Hiller, C.E.; Kaminski, T.W.; et al. Selection Criteria for Patients with Chronic Ankle Instability in Controlled Research: A Position Statement of the International Ankle Consortium. J. Athl. Train. 2014, 49, 121–127. [Google Scholar] [CrossRef] [PubMed]
- Olszewski, M.; Zając, B.; Golec, J. Cross Cultural Adaptation, Reliability and Validity of the Polish Version of the Cumberland Ankle Instability Tool. Disabil. Rehabil. 2023, 46, 2926–2932. [Google Scholar] [CrossRef] [PubMed]
- Amireault, S.; Godin, G. The Godin-Shephard Leisure-Time Physical Activity Questionnaire: Validity Evidence Supporting Its Use for Classifying Healthy Adults into Active and Insufficiently Active Categories. Percept. Mot. Ski. 2015, 120, 604–622. [Google Scholar] [CrossRef]
- Redmond, A.C.; Crosbie, J.; Ouvrier, R.A. Development and Validation of a Novel Rating System for Scoring Standing Foot Posture: The Foot Posture Index. Clin. Biomech. 2006, 21, 89–98. [Google Scholar] [CrossRef]
- BTS Bioengineering. BTS SMART Capture User’s Guide; BTS Bioengineering: Milan, Italy, 2006. [Google Scholar]
- Leardini, A.; Benedetti, M.G.; Berti, L.; Bettinelli, D.; Nativo, R.; Giannini, S. Rear-Foot, Mid-Foot and Fore-Foot Motion during the Stance Phase of Gait. Gait Posture 2007, 25, 453–462. [Google Scholar] [CrossRef]
- Hubbard, T.J.; Kramer, L.C.; Denegar, C.R.; Hertel, J. Contributing Factors to Chronic Ankle Instability. Foot Ankle Int. 2007, 28, 343–354. [Google Scholar] [CrossRef] [PubMed]
- Kirmizi, M.; Cakiroglu, M.A.; Elvan, A.; Simsek, I.E.; Angin, S. Reliability of Different Clinical Techniques for Assessing Foot Posture. J. Manip. Physiol. Ther. 2020, 43, 901–908. [Google Scholar] [CrossRef]
- Schallig, W.; van den Noort, J.C.; Maas, M.; Harlaar, J.; van der Krogt, M.M. Marker Placement Sensitivity of the Oxford and Rizzoli Foot Models in Adults and Children. J. Biomech. 2021, 126, 110629. [Google Scholar] [CrossRef]
- Thorborg, K.; Petersen, J.; Magnusson, S.P.; Hölmich, P. Clinical Assessment of Hip Strength Using a Hand-Held Dynamometer Is Reliable. Scand. J. Med. Sci. Sports 2010, 20, 493–501. [Google Scholar] [CrossRef]
- Pataky, T.C. Generalized N-Dimensional Biomechanical Field Analysis Using Statistical Parametric Mapping. J. Biomech. 2010, 43, 1976–1982. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences; Routledge: Oxford, UK, 2013; ISBN 9781134742707. [Google Scholar]
- Milner, C.E.; Brindle, R.A. Reliability and Minimal Detectable Difference in Multisegment Foot Kinematics during Shod Walking and Running. Gait Posture 2016, 43, 192–197. [Google Scholar] [CrossRef]
- Buldt, A.K.; Levinger, P.; Murley, G.S.; Menz, H.B.; Nester, C.J.; Landorf, K.B. Foot Posture Is Associated with Kinematics of the Foot during Gait: A Comparison of Normal, Planus and Cavus Feet. Gait Posture 2015, 42, 42–48. [Google Scholar] [CrossRef]
- Wright, I.C.; Neptune, R.R.; van den Bogert, A.J.; Nigg, B.M. The Influence of Foot Positioning on Ankle Sprains. J. Biomech. 2000, 33, 513–519. [Google Scholar] [CrossRef]
- Rankin, B.L.; Buffo, S.K.; Dean, J.C. A Neuromechanical Strategy for Mediolateral Foot Placement in Walking Humans. J. Neurophysiol. 2014, 112, 374–383. [Google Scholar] [CrossRef]
- Murley, G.S.; Buldt, A.K.; Trump, P.J.; Wickham, J.B. Tibialis Posterior EMG Activity during Barefoot Walking in People with Neutral Foot Posture. J. Electromyogr. Kinesiol. 2009, 19, e69–e77. [Google Scholar] [CrossRef]
- Neumann, D.A. Kinesiology of the Musculoskeletal System, 3rd ed.; Mosby: St. Louis, USA, 2016. [Google Scholar]
- Wilkerson, G.B.; Pinerola, J.J.; Caturano, R.W. Invertor Vs. Evertor Peak Torque and Power Deficiencies Associated with Lateral Ankle Ligament Injury. J. Orthop. Sports Phys. Ther. 1997, 26, 78–86. [Google Scholar] [CrossRef] [PubMed]
- Abdel-aziem, A.A.; Draz, A.H. Chronic Ankle Instability Alters Eccentric Eversion/Inversion and Dorsiflexion/Plantarflexion Ratio. J. Back Musculoskelet. Rehabil. 2014, 27, 47–53. [Google Scholar] [CrossRef] [PubMed]
- Santilli, V.; Frascarelli, M.A.; Paoloni, M.; Frascarelli, F.; Camerota, F.; De Natale, L.; De Santis, F. Peroneus Longus Muscle Activation Pattern during Gait Cycle in Athletes Affected by Functional Ankle Instability. Am. J. Sports Med. 2005, 33, 1183–1187. [Google Scholar] [CrossRef]
- Labanca, L.; Mosca, M.; Ghislieri, M.; Agostini, V.; Knaflitz, M.; Benedetti, M.G. Muscle Activations during Functional Tasks in Individuals with Chronic Ankle Instability: A Systematic Review of Electromyographical Studies. Gait Posture 2021, 90, 340–373. [Google Scholar] [CrossRef] [PubMed]
- Mendez-Rebolledo, G.; Guzmán-Venegas, R.; Cruz-Montecinos, C.; Watanabe, K.; Calatayud, J.; Martinez-Valdes, E. Individuals with Chronic Ankle Instability Show Altered Regional Activation of the Peroneus Longus Muscle during Ankle Eversion. Scand. J. Med. Sci. Sports 2024, 34, e14535. [Google Scholar] [CrossRef]
- Lilley, T.; Herb, C.C.; Hart, J.; Hertel, J. Lower Extremity Joint Coupling Variability during Gait in Young Adults with and without Chronic Ankle Instability. Sports Biomech. 2018, 17, 261–272. [Google Scholar] [CrossRef]
- Dury, J.; Ravier, G.; Michel, F. Hip Abductor Muscle Fatigue Induces Different Strategies During Disrupted Postural Control. Front. Sports Act. Living 2022, 4, 918402. [Google Scholar] [CrossRef]
- Ortega, C.E.; Torp, D.M.; Donovan, L.; Simpson, J.D.; Forsyth, L.; Koldenhoven, R.M. Gait-Training Interventions for Individuals with Chronic Ankle Instability: A Systematic Review and Meta-Analysis. J. Athl. Train. 2025, 60, 332–351. [Google Scholar] [CrossRef]
- da Silva Neto, W.C.; Lopes, A.D.; Ribeiro, A.P. Gait Retraining with Visual Biofeedback Reduces Rearfoot Pressure and Foot Pronation in Recreational Runners. J. Sport Rehabil. 2022, 31, 165–173. [Google Scholar] [CrossRef] [PubMed]
- Mousavi, S.H.; Khorramroo, F.; Jafarnezhadgero, A. Gait Retraining Targeting Foot Pronation: A Systematic Review and Meta-Analysis. PLoS ONE 2024, 19, e0298646. [Google Scholar] [CrossRef] [PubMed]
- Ko, D.; Choi, Y.; Lee, K. Effects of Peroneus Brevis versus Peroneus Longus Muscle Training on Muscle Function in Chronic Ankle Instability: A Randomized Controlled Trial. Healthcare 2024, 12, 547. [Google Scholar] [CrossRef]
- Panichawit, C.; Bovonsunthonchai, S.; Vachalathiti, R.; Limpasutirachata, K. Effects of Foot Muscles Training on Plantar Pressure Distribution during Gait, Foot Muscle Strength, and Foot Function in Persons with Flexible Flatfoot. J. Med. Assoc. Thail. 2015, 98 (Suppl. S5), S12–S17. [Google Scholar]
- Rowe, E.; Beauchamp, M.K.; Astephen Wilson, J. Age and Sex Differences in Normative Gait Patterns. Gait Posture 2021, 88, 109–115. [Google Scholar] [CrossRef]
- Houck, J.R.; Tome, J.M.; Nawoczenski, D.A. Subtalar Neutral Position as an Offset for a Kinematic Model of the Foot during Walking. Gait Posture 2008, 28, 29–37. [Google Scholar] [CrossRef] [PubMed]
- Schallig, W.; van den Noort, J.C.; Piening, M.; Streekstra, G.J.; Maas, M.; van der Krogt, M.M.; Harlaar, J. The Amsterdam Foot Model: A Clinically Informed Multi-segment Foot Model Developed to Minimize Measurement Errors in Foot Kinematics. J. Foot Ankle Res. 2022, 15, 46. [Google Scholar] [CrossRef] [PubMed]
| CAI Group (n = 25) | CON Group (n = 25) | p-Value | |
|---|---|---|---|
| Age [years] | 23.1 (3.6) | 21.8 (2.9) | 0.139 |
| Body mass [kg] | 78.2 (12.8) | 77.2 (10.3) | 0.786 |
| Body height [m] | 1.81 (0.07) | 1.78 (0.07) | 0.153 |
| BMI [kg/m2] | 23.9 (3.4) | 24.4 (2.7) | 0.473 |
| GODIN | 60.5 (24.3) | 58.6 (30.3) | 0.809 |
| Foot Posture Index | 1.8 (3.8) | 4.6 (3.4) | 0.01 * |
| CAIT-PL | 20 (18–22) | 30 (30–30) | <0.001 * |
| # of ankle sprains | 3 (2–4) | 0 (0–0) | <0.001 * |
| # of ankle giving-way | 2 (1–4) | 0 (0–0) | <0.001 * |
| Spatiotemporal parameters | |||
| Stance Phase [%] | 60.0 (1.7) | 59.9 (1.0) | 0.934 |
| Swing Phase [%] | 40.0 (1.7) | 40.1 (1.0) | 0.959 |
| Stride time [s] | 1.1 (0.1) | 1.1 (0.1) | 0.316 |
| Velocity [m/s] | 1.2 (0.2) | 1.2 (0.1) | 0.900 |
| Independent Variable | Dependent Variables | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Sha-Foo Peak Inversion | Sha-Foo F-ROM | Sha-Cal Peak Inversion | Sha-Cal F-ROM | ||||||
| CAI | CON | CAI | CON | CAI | CON | CAI | CON | ||
| Hip Abductor Isometric strength [Nm/kg] | r | −0.09 | −0.23 | −0.26 | −0.11 | 0.13 | −0.19 | −0.03 | −0.20 |
| p | 0.68 | 0.28 | 0.22 | 0.60 | 0.52 | 0.37 | 0.88 | 0.33 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Olszewski, M.; Krężałek, P.; Golec, J. Multisegmented Foot and Lower Limb Kinematics During Gait in Males with Chronic Ankle Instability: Exploring Links with Hip Abductor Strength. J. Clin. Med. 2025, 14, 5977. https://doi.org/10.3390/jcm14175977
Olszewski M, Krężałek P, Golec J. Multisegmented Foot and Lower Limb Kinematics During Gait in Males with Chronic Ankle Instability: Exploring Links with Hip Abductor Strength. Journal of Clinical Medicine. 2025; 14(17):5977. https://doi.org/10.3390/jcm14175977
Chicago/Turabian StyleOlszewski, Maciej, Piotr Krężałek, and Joanna Golec. 2025. "Multisegmented Foot and Lower Limb Kinematics During Gait in Males with Chronic Ankle Instability: Exploring Links with Hip Abductor Strength" Journal of Clinical Medicine 14, no. 17: 5977. https://doi.org/10.3390/jcm14175977
APA StyleOlszewski, M., Krężałek, P., & Golec, J. (2025). Multisegmented Foot and Lower Limb Kinematics During Gait in Males with Chronic Ankle Instability: Exploring Links with Hip Abductor Strength. Journal of Clinical Medicine, 14(17), 5977. https://doi.org/10.3390/jcm14175977







