Perceptions and Experiences of Physiotherapists Treating Trismus in Head and Neck Cancer Patients: Findings from a Spanish Web-Based Survey
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
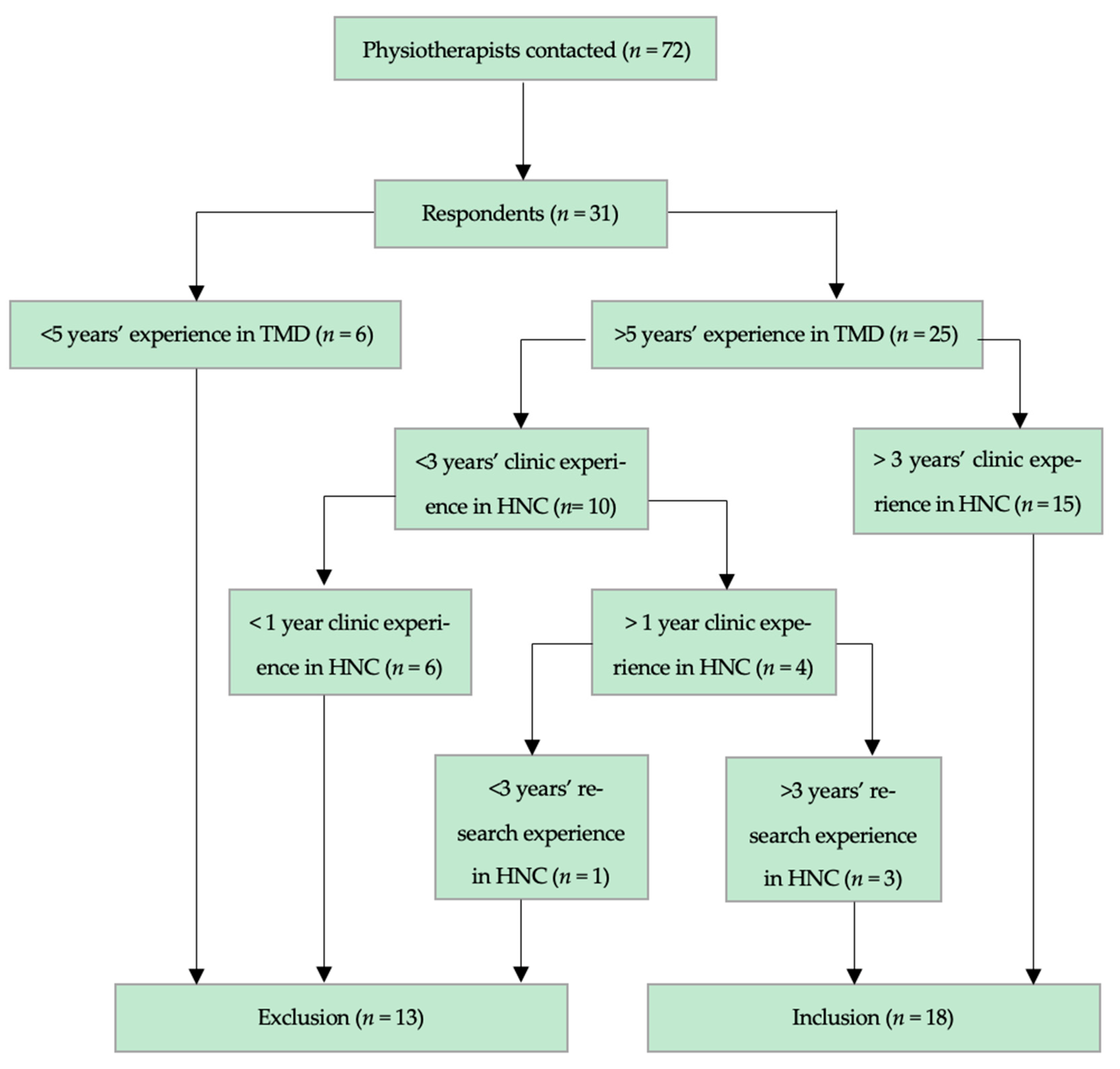
2.2. Participants and Recruitment
2.3. Questionnaire Development
2.4. Ethical Considerations and Informed Consent
2.5. Data Protection and Duplicate Entry Prevention
2.6. Data Analysis
3. Results
3.1. Sociodemographic Characteristics and Professional Information
3.2. Experience in HNC Management and General Associated Features of Patients
3.3. Treatment Practices
3.4. Barriers and Implementation of TE and MT
3.5. Medical Devices in the Rehabilitation of Trismus
4. Discussion
4.1. Limitations
4.2. Future Implications
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| MT | Manual Therapy |
| TE | Therapeutic Exercise |
| TMD | Temporomandibular Disorders |
| HNC | Head and Neck Cancer |
References
- Zhou, T.; Huang, W.; Wang, X.; Zhang, J.; Zhou, E.; Tu, Y.; Zou, J.; Su, K.; Yi, H.; Yin, S. Global burden of head and neck cancers from 1990 to 2019. iScience 2024, 27, 109282. [Google Scholar] [CrossRef]
- Verdonck-de Leeuw, I.; Dawson, C.; Licitra, L.; Eriksen, J.G.; Hosal, S.; Singer, S.; Laverty, D.P.; Golusinski, W.; Machczynski, P.; Varges Gomes, A.; et al. European Head and Neck Society recommendations for head and neck cancer survivorship care. Oral Oncol. 2022, 133, 106047. [Google Scholar] [CrossRef]
- Arends, C.R.; van der Molen, L.; Lindhout, J.E.; Bragante, K.; Navran, A.; van den Brekel, M.W.M.; Stuiver, M.M. Lymphedema and Trismus after Head and Neck Cancer, and the Impact on Body Image and Quality of Life. Cancers 2024, 16, 653. [Google Scholar] [CrossRef]
- Faravel, K.; Jarlier, M.; Senesse, P.; Huteau, M.E.; Janiszewski, C.; Stoebner, A.; Boisselier, P. Trismus Occurrence and Link with Radiotherapy Doses in Head and Neck Cancer Patients Treated with Chemoradiotherapy. Integr. Cancer Ther. 2023, 22, 15347354221147283. [Google Scholar] [CrossRef]
- Dijkstra, P.U.; Kalk, W.W.; Roodenburg, J.L. Trismus in head and neck oncology: A systematic review. Oral Oncol. 2004, 40, 879–889. [Google Scholar] [CrossRef] [PubMed]
- Watters, A.L.; Cope, S.; Keller, M.N.; Padilla, M.; Enciso, R. Prevalence of trismus in patients with head and neck cancer: A systematic review with meta-analysis. Head Neck 2019, 41, 3408–3421. [Google Scholar] [CrossRef]
- Aghajanzadeh, S.; Karlsson, T.; Tuomi, L.; Engström, M.; Finizia, C. Postradiation trismus in head and neck cancer survivors: A qualitative study of effects on life, rehabilitation, used coping strategies and support from the healthcare system. Eur. Arch. Otorhinolaryngol. 2024, 281, 3717–3726. [Google Scholar] [CrossRef] [PubMed]
- Ortiz-Comino, L.; Martín-Martín, L.; Galiano-Castillo, N.; Castro-Martín, E.; Fernández-Gualda, M.Á.; Lozano-Lozano, M.; Fernández-Lao, C. The effects of myofascial induction therapy in survivors of head and neck cancer: A randomized, controlled clinical trial. Support. Care Cancer 2022, 31, 49. [Google Scholar] [CrossRef]
- Bragante, K.C.; Groisman, S.; Carboni, C.; Baiocchi, J.M.T.; da Motta, N.W.; Silva, M.F.; Pinto, R.C.; Plentz, R.D.M.; Wienandts, P.; Jotz, G.P. Efficacy of exercise therapy during radiotherapy to prevent reduction in mouth opening in patients with head and neck cancer: A randomized controlled trial. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2020, 129, 27–38. [Google Scholar] [CrossRef] [PubMed]
- Lee, R.; Yeo, S.T.; Rogers, S.N.; Caress, A.L.; Molassiotis, A.; Ryder, D.; Sanghera, P.; Lunt, C.; Scott, B.; Keeley, P.; et al. Randomised feasibility study to compare the use of Therabite® with wooden spatulas to relieve and prevent trismus in patients with cancer of the head and neck. Br. J. Oral Maxillofac. Surg. 2018, 56, 283–291. [Google Scholar] [CrossRef] [PubMed]
- Shao, C.H.; Chiang, C.C.; Huang, T.W. Exercise therapy for cancer treatment-induced trismus in patients with head and neck cancer: A systematic review and meta-analysis of randomized controlled trials. Radiother. Oncol. 2020, 151, 249–255. [Google Scholar] [CrossRef]
- Kamstra, J.I.; Reintsema, H.; Roodenburg, J.L.; Dijkstra, P.U. Dynasplint Trismus System exercises for trismus secondary to head and neck cancer: A prospective explorative study. Support. Care Cancer 2016, 24, 3315–3323. [Google Scholar] [CrossRef]
- Li, Y.H.; Liu, C.C.; Chiang, T.E.; Chen, Y.W. EZBite open-mouth device: A new treatment option for oral submucous fibrosis-related trismus. J. Dent. Sci. 2018, 13, 80–81. [Google Scholar] [CrossRef] [PubMed]
- Charters, E.; Cheng, K.; Dunn, M.; Heng, C.; Loy, J.; Ricketts, V.; Luo, A.; Aung, Y.M.; Lewin, W.; Howes, D.; et al. Restorabite™: Phase II trial of jaw stretching exercises using a novel device for patients with trismus following head and neck cancer. Int. J. Cancer 2024, 155, 731–741. [Google Scholar] [CrossRef]
- Hutting, N.; Caneiro, J.P.; Ong’wen, O.M.; Miciak, M.; Roberts, L. Patient-centered care in musculoskeletal practice: Key elements to support clinicians to focus on the person. Musculoskelet. Sci. Pract. 2022, 57, 102434. [Google Scholar] [CrossRef] [PubMed]
- Charters, E.; Ricketts, V.; Sharman, A.R.; Clark, J. Systematic review of adherence to swallow and trismus exercises during radiation therapy for head and neck cancer. Head Neck 2024, 46, 2348–2362. [Google Scholar] [CrossRef]
- Petersson, K.; Finizia, C.; Pauli, N.; Tuomi, L. Preventing radiation-induced dysphagia and trismus in head and neck cancer-A randomized controlled trial. Head Neck 2025, 47, 159–174. [Google Scholar] [CrossRef] [PubMed]
- López-Rodríguez, J.A. Declaración de la iniciativa CHERRIES: Adaptación al castellano de directrices para la comunicación de resultados de cuestionarios y encuestas online [Improving the quality of Spanish web surveys: Spanish adaptation of the checklist for reporting results of internet e-surveys (CHERRIES) to the Spanish context]. Atención Primaria 2019, 51, 586–589. (In Spanish) [Google Scholar]
- Pérez Fernández, T.; Parra González, A. Fisioterapia en Procesos Oncológicos y Quirúrgicos de Cabeza y Cuello, 1st ed.; Elsevier España: Madrid, Spain, 2022. [Google Scholar]
- Braun, V.; Clarke, V. Using Thematic Analysis in Psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef]
- van Vugt, V.A.; de Kruif, A.J.; van der Wouden, J.C.; van der Horst, H.E.; Maarsingh, O.R. Experiences of patients and physiotherapists with blended internet-based vestibular rehabilitation: A qualitative interview study. BJGP Open 2020, 4, bjgpopen20X101092. [Google Scholar] [CrossRef]
- Gleadhill, C.; Bolsewicz, K.; Davidson, S.R.E.; Kamper, S.J.; Tutty, A.; Robson, E.; Da Silva, P.V.; Donald, B.; Dooley, K.; Manvell, J.; et al. Physiotherapists’ opinions, barriers, and enablers to providing evidence-based care: A mixed-methods study. BMC Health Serv. Res. 2022, 22, 1382. [Google Scholar] [CrossRef] [PubMed]
- Thomas, S.L.; Pitt, H.; McCarthy, S.; Arnot, G.; Hennessy, M. Methodological and practical guidance for designing and conducting online qualitative surveys in public health. Health Promot. Int. 2024, 39, daae061. [Google Scholar] [CrossRef]
- Anarte-Lazo, E.; Bernal-Utrera, C. A Scoping Review of Clinical Features and Mechanisms of Orofacial Pain and Headache in Patients with Head and Neck Cancer. J. Clin. Med. 2025, 14, 5722. [Google Scholar] [CrossRef] [PubMed]
- Khawaja, S.; Bavarian, R.; Abdul Rehman, S.; Hafeez, H. Head and Neck Cancer-Related Pain: A Descriptive Analysis of the Pain Phenotypes. J. Pain. Res. 2023, 16, 2919–2927. [Google Scholar] [CrossRef]
- Jiang, J.; Li, Y.; Shen, Q.; Rong, X.; Huang, X.; Li, H.; Zhou, L.; Mai, H.Q.; Zheng, D.; Chen, M.Y.; et al. Effect of Pregabalin on Radiotherapy-Related Neuropathic Pain in Patients With Head and Neck Cancer: A Randomized Controlled Trial. J. Clin. Oncol. 2019, 37, 135–143. [Google Scholar] [CrossRef]
- Rojo, R.D.; Ren, J.L.; Lipe, D.N.; Badr, H.; Shete, S.; Hanna, E.Y.; Reyes-Gibby, C.C. Neuropathic pain prevalence and risk factors in head and neck cancer survivors. Head Neck 2022, 44, 2820–2833. [Google Scholar] [CrossRef]
- Kamstra, J.I.; Roodenburg, J.L.; Beurskens, C.H.; Reintsema, H.; Dijkstra, P.U. TheraBite exercises to treat trismus secondary to head and neck cancer. Support. Care Cancer 2013, 21, 951–957. [Google Scholar] [CrossRef] [PubMed]
- Charters, E.; Loy, J.; Wu, R.; Cheng, K.; Dunn, M.; Davies, S.; Clark, J. Pilot Study of Intensive Trismus Intervention Using Restorabite™ During Unilateral Adjuvant Radiation for Head and Neck Cancer. Dysphagia. 2024, 39, 864–871. [Google Scholar] [CrossRef]
- Anarte-Lazo, E.; Bravo-Vazquez, A.; Bernal-Utrera, C.; Torres-Lagares, D.; Falla, D.; Rodríguez-Blanco, C. The Rationale and Explanation for Rehabilitation Interventions in the Management of Treatment-Induced Trismus in People with Head and Neck Cancer: A Scoping Review of Randomized Controlled Trials. Medicina 2025, 61, 1392. [Google Scholar] [CrossRef]
- Nimonkar, S.; Godbole, S.; Belkhode, V.; Nimonkar, P.; Pisulkar, S. Effect of Rehabilitation of Completely Edentulous Patients with Complete Dentures on Temporomandibular Disorders: A Systematic Review. Cureus 2022, 14, e28012. [Google Scholar] [CrossRef]
- Sawczuk, B.; Nayar, S.; Szutko, P.; Sierpińska, T. Assessing the Impact of Removable Prosthetic Restorations on Nutritional Habits in Edentulous Patients Following Surgery for Head and Neck Cancer. Nutrients 2025, 17, 1483. [Google Scholar] [CrossRef] [PubMed]
- Castro-Martín, E.; Galiano-Castillo, N.; Fernández-Lao, C.; Ortiz-Comino, L.; Postigo-Martin, P.; Arroyo-Morales, M. Myofascial Induction Therapy Improves the Sequelae of Medical Treatment in Head and Neck Cancer Survivors: A Single-Blind, Placebo-Controlled, Randomized Cross-Over Study. J Clin Med. 2021, 10, 5003. [Google Scholar] [CrossRef]
- McMillan, H.; Barbon, C.E.A.; Cardoso, R.; Sedory, A.; Buoy, S.; Porsche, C.; Savage, K.; Mayo, L.; Hutcheson, K.A. Manual Therapy for Patients With Radiation-Associated Trismus After Head and Neck Cancer. JAMA Otolaryngol. Head Neck Surg. 2022, 148, 418–425. [Google Scholar] [CrossRef]
- Nedeljak, J.; Armijo-Olivo, S.; Hernandez, I.A.; Nayar, S.; McNeel, M.L. A Scoping Review of Physiotherapeutic Interventions for Trismus in Head and Neck Cancer: Where Is the Manual Therapy? Physiother. Can. 2021, 74, 173–183. [Google Scholar] [CrossRef]
- Dai, Y.M.; Virtanen, H.; Zhu, Y.; Wan, H. Effectiveness of mHealth intervention for trismus exercise in patients with head and neck cancer undergoing proton and heavy ion therapy: A randomized control trial. Support. Care Cancer 2024, 32, 470. [Google Scholar] [CrossRef] [PubMed]
- Saghafi, E.; Kadhim, K.; Andås, C.A.; Cahlin, B.J.; Finizia, C.; Axelsson, T.; Kjeller, G.; Tuomi, L. Jaw exercise in head and neck cancer patients for prevention of temporomandibular disorders: A randomized controlled trial. J. Cancer Surviv. 2024. [Google Scholar] [CrossRef]
- Nasa, P.; Jain, R.; Juneja, D. Delphi methodology in healthcare research: How to decide its appropriateness. World J. Methodol. 2021, 11, 116–129. [Google Scholar] [CrossRef] [PubMed]
| Sociodemographic and Professional Information | Experience with Patients with HNC and Their Features | Assessment and Treatment Practices | Barriers in the Implementation of TE and MT | Medical Devices in the Rehabilitation of Trismus |
|---|---|---|---|---|
| Age | Years in the management of people with H&NC | Treatment modalities for trismus | Limitations to (a) MT and (b) TE because of dental prostheses | Use of medical devices |
| Gender | Patients treated per year with H&NC | MT modalities | Recommended strategies to develop functional chewing rehabilitation | Models used |
| Years of experience in patients with TMD | Main clinical features associated to trismus | TE modalities | Limitations for implementing and boosting adherence in TE | Limitations coming from these medical devices |
| - | ADL most affected by trismus | - | - | - |
| “How many years have you been practicing as a physiotherapist?” | “Do you use manual therapy in trismus rehabilitation? Please specify how.” | “Which exercise modalities do you prescribe (e.g., mobility, resistance, functional chewing)?” | “What are the main advantages or limitations you encounter with trismus devices?” | “In your experience, what factors hinder or facilitate patient adherence to rehabilitation?” |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Anarte-Lazo, E.; Bernal-Utrera, C. Perceptions and Experiences of Physiotherapists Treating Trismus in Head and Neck Cancer Patients: Findings from a Spanish Web-Based Survey. J. Clin. Med. 2025, 14, 7092. https://doi.org/10.3390/jcm14197092
Anarte-Lazo E, Bernal-Utrera C. Perceptions and Experiences of Physiotherapists Treating Trismus in Head and Neck Cancer Patients: Findings from a Spanish Web-Based Survey. Journal of Clinical Medicine. 2025; 14(19):7092. https://doi.org/10.3390/jcm14197092
Chicago/Turabian StyleAnarte-Lazo, Ernesto, and Carlos Bernal-Utrera. 2025. "Perceptions and Experiences of Physiotherapists Treating Trismus in Head and Neck Cancer Patients: Findings from a Spanish Web-Based Survey" Journal of Clinical Medicine 14, no. 19: 7092. https://doi.org/10.3390/jcm14197092
APA StyleAnarte-Lazo, E., & Bernal-Utrera, C. (2025). Perceptions and Experiences of Physiotherapists Treating Trismus in Head and Neck Cancer Patients: Findings from a Spanish Web-Based Survey. Journal of Clinical Medicine, 14(19), 7092. https://doi.org/10.3390/jcm14197092







