Impact of Exercise Therapy on Outcomes in Patients with Low Back Pain: An Umbrella Review of Systematic Reviews
Abstract
1. Introduction
2. Materials and Methods
2.1. Inclusion Criteria
2.2. Exclusion Criteria
2.3. Database Search
2.4. Data Extraction
2.5. Quality Assessment
2.6. Data Synthesis
- heterogeneity in populations;
- heterogeneity in interventions;
- heterogeneity in outcomes;
- heterogeneity in comparators;
- potential overlap of primary studies.
3. Results
3.1. Search Results and Included Studies
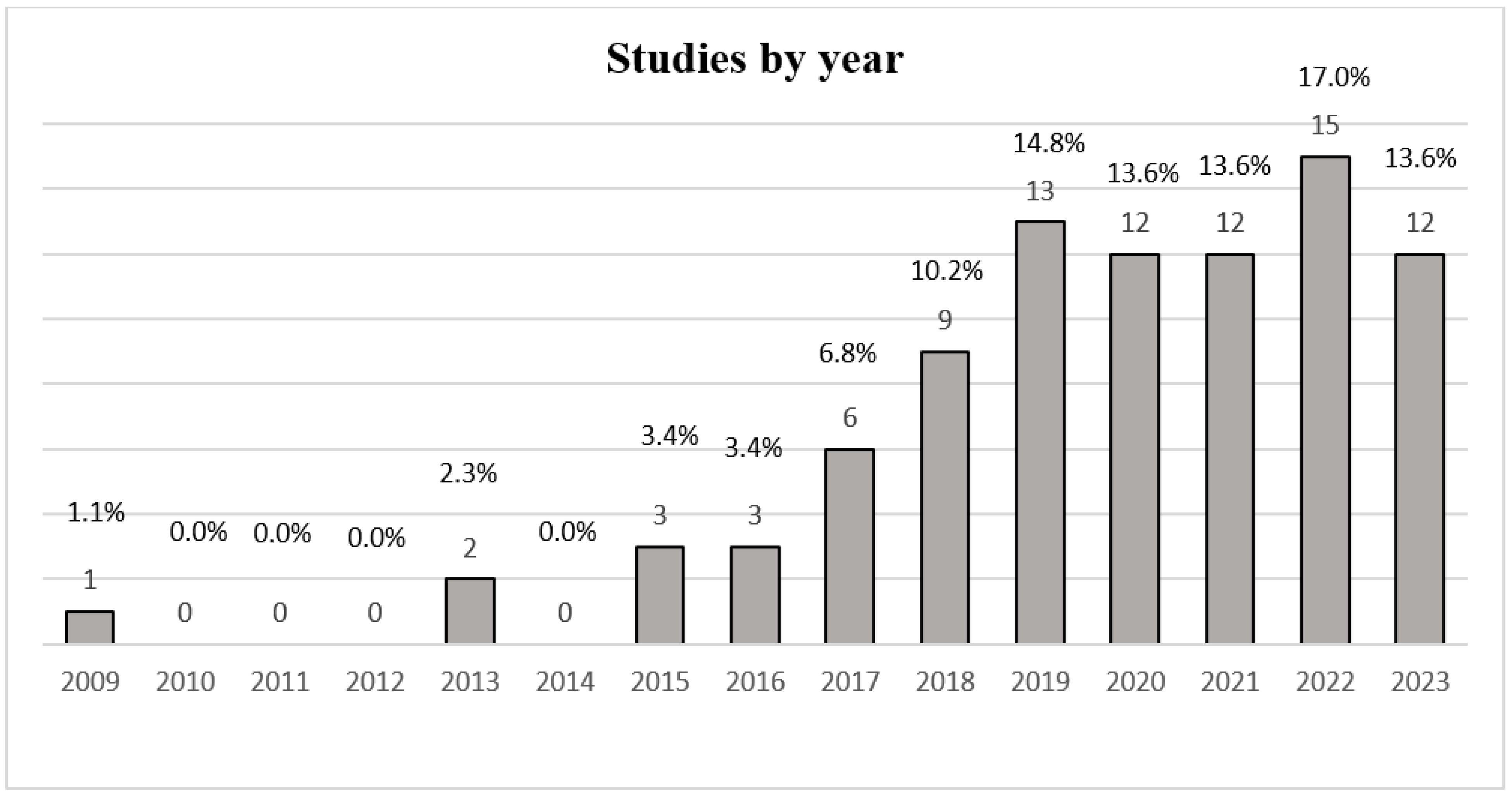
3.2. Characteristics of Publications
3.3. Classification of Exercise Therapy for LBP
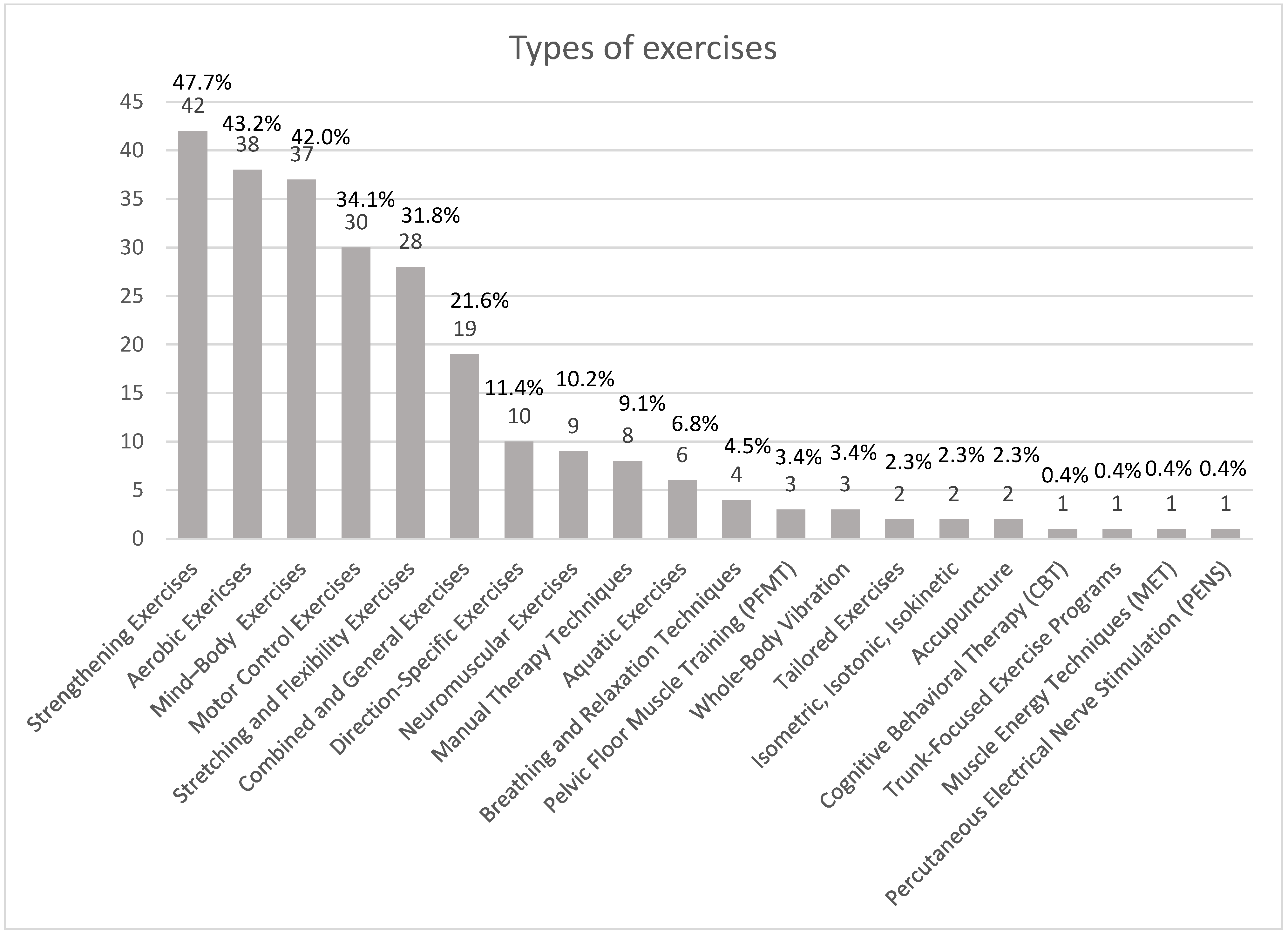
Characteristics of Exercises
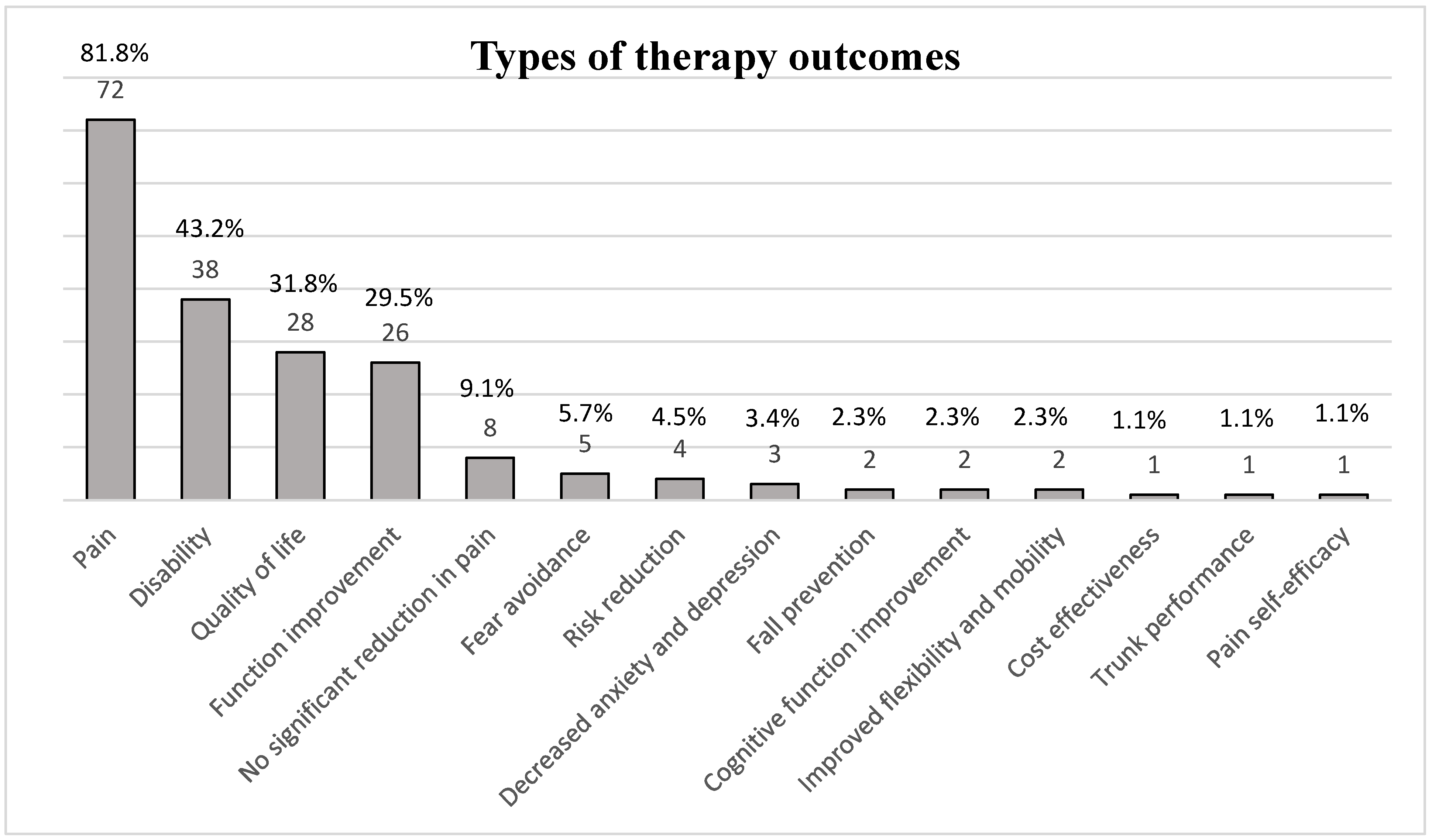
3.4. Characteristics of Outcomes
3.5. The Impact of Exercise on Pain Outcomes
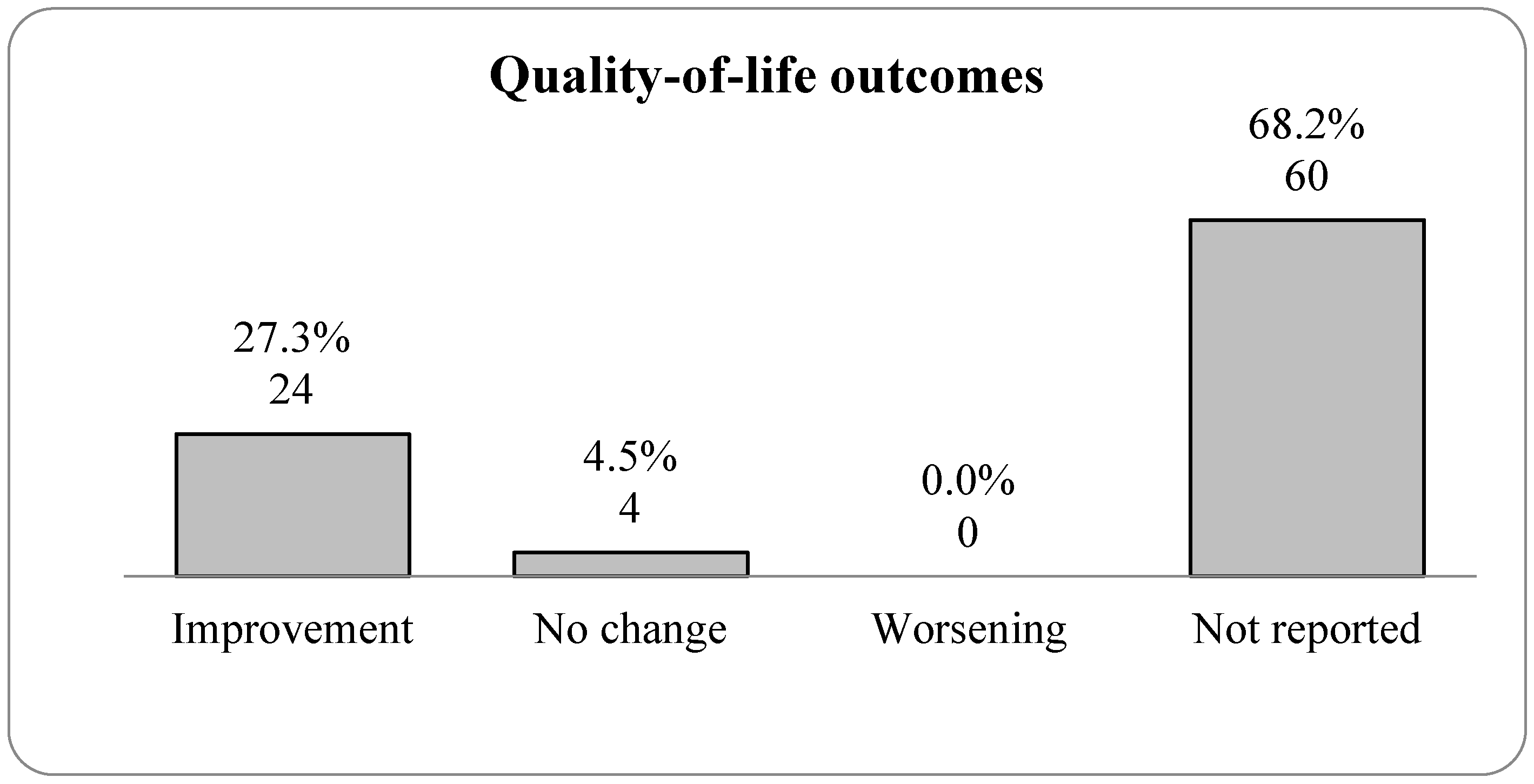
3.6. The Impact of Exercise on Quality of Life
3.7. Quality Assessment Results
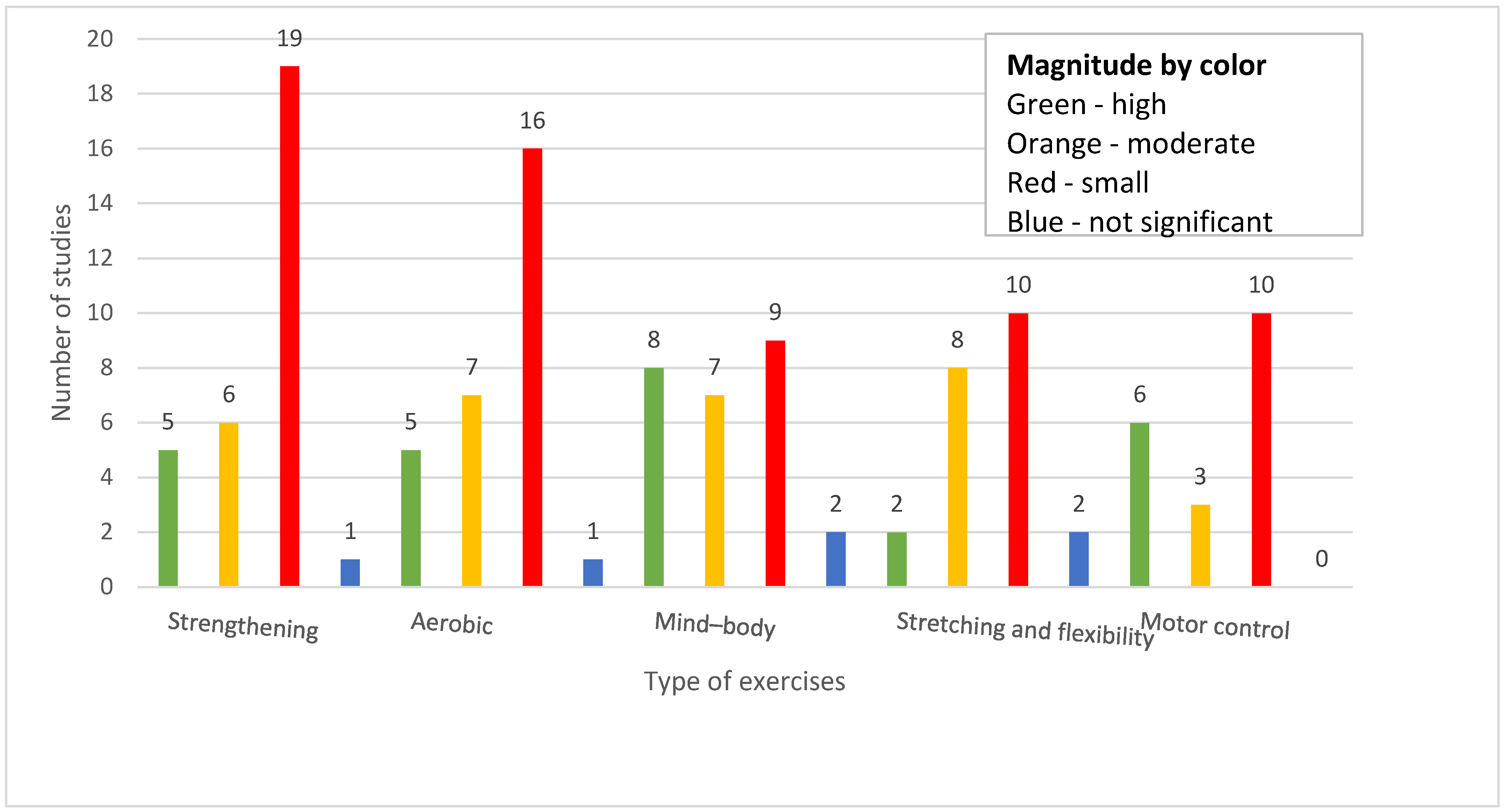
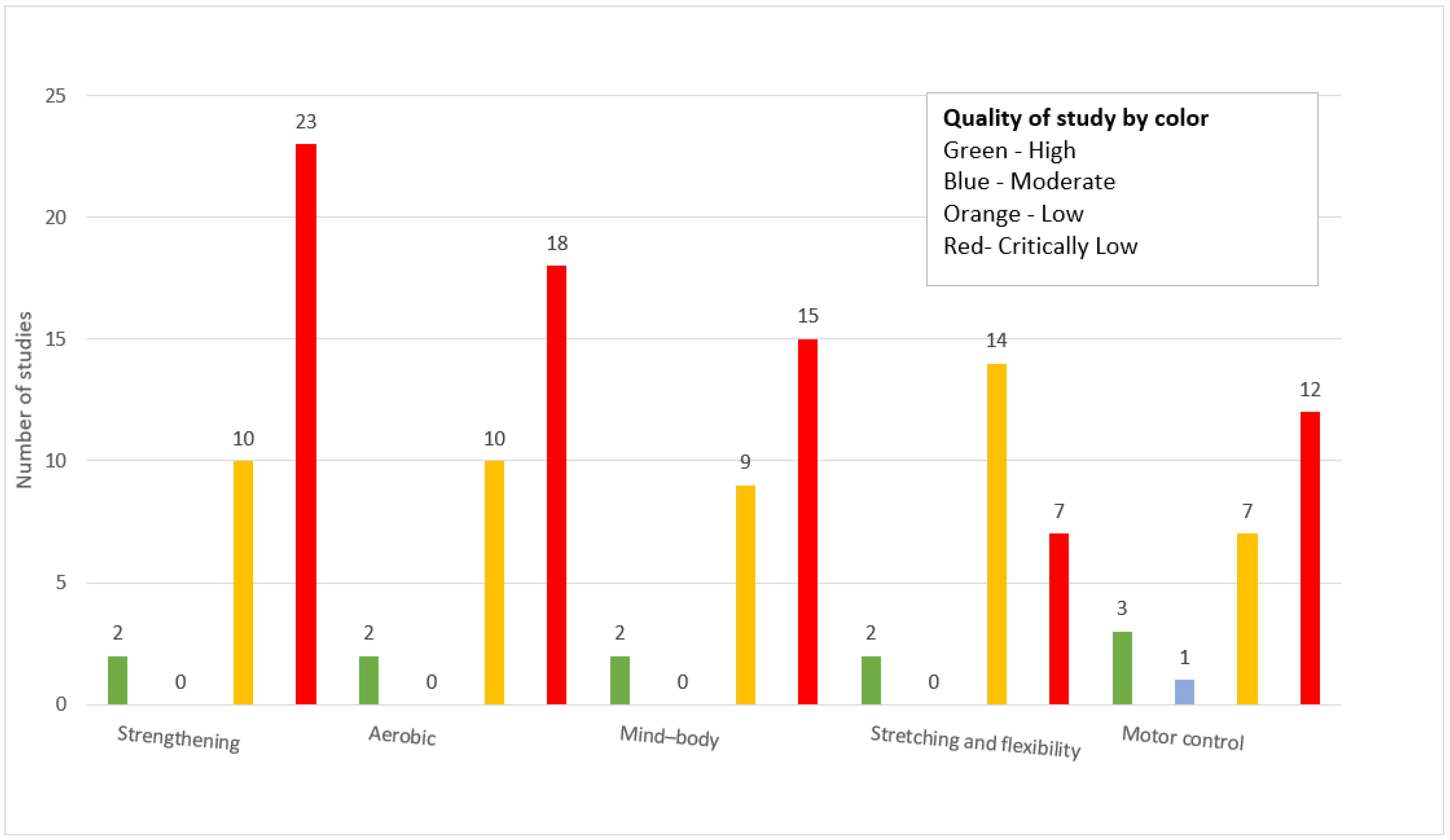
3.8. Magnitude of Effect and Study Quality by Exercise Type
- Pilates was more effective than general exercise and direction-specific exercise, with low certainty of evidence [10].
- An outcome matched to exercise treatment may be more effective than an unmatched primary outcome [52].
- Pilates, mind–body exercise, and core-based exercise were the most effective interventions [24].
- Motor control is only effective in combination with musculoskeletal therapies [27].
- Pilates and McKenzie therapies are better than flexibility, minimal treatment, and other effective exercises [35].
- Low back exercise in combination with health education might be the best approach [40].
- It is not clear whether a region-specific or general-specific approach is better for pain reduction [41].
- Walking is better than yoga in the short term, and yoga is better than walking in the intermediate term [46].
- Multidisciplinary-based rehabilitation may be better than active physical intervention [49].
- Primary outcome-matched exercises may be better than the unmatched category [52].
- Baduanjin exercise is more effective than general exercise or general exercise with routine drugs (ibuprofen) [61].
- Stabilization exercise is better than general exercise [86].
- Isometric and motor control exercises are both effective, and motor control exercises are more effective than isometric exercises [26].
- Individualized exercise is better than active exercises [22].
- Regarding insignificance and possible reasons for it:
- One study analyzed a specific population of older adults [65].
- One study was comparative and found equivalent effectiveness between walking and other physical exercises [76].
- One study investigated incidental physical activity as a planned program [63].
- Regarding cost-effectiveness:
- One review assessed cost-effectiveness and found that exercise therapy was more cost-effective than usual care for subacute and chronic low back pain, but was not superior to other active treatments. From a healthcare perspective, exercise therapy demonstrated favorable cost-utility ratios (CURs), ranging from GBP 3760 to GBP 17,447 per quality-adjusted life year (QALY) gained, indicating cost-effectiveness. However, from a societal perspective, the findings were mixed; one analysis reported a high CUR of GBP 82,657 per QALY gained, suggesting that exercise therapy may not be cost-effective compared to usual care in broader economic models [71].
4. Discussion
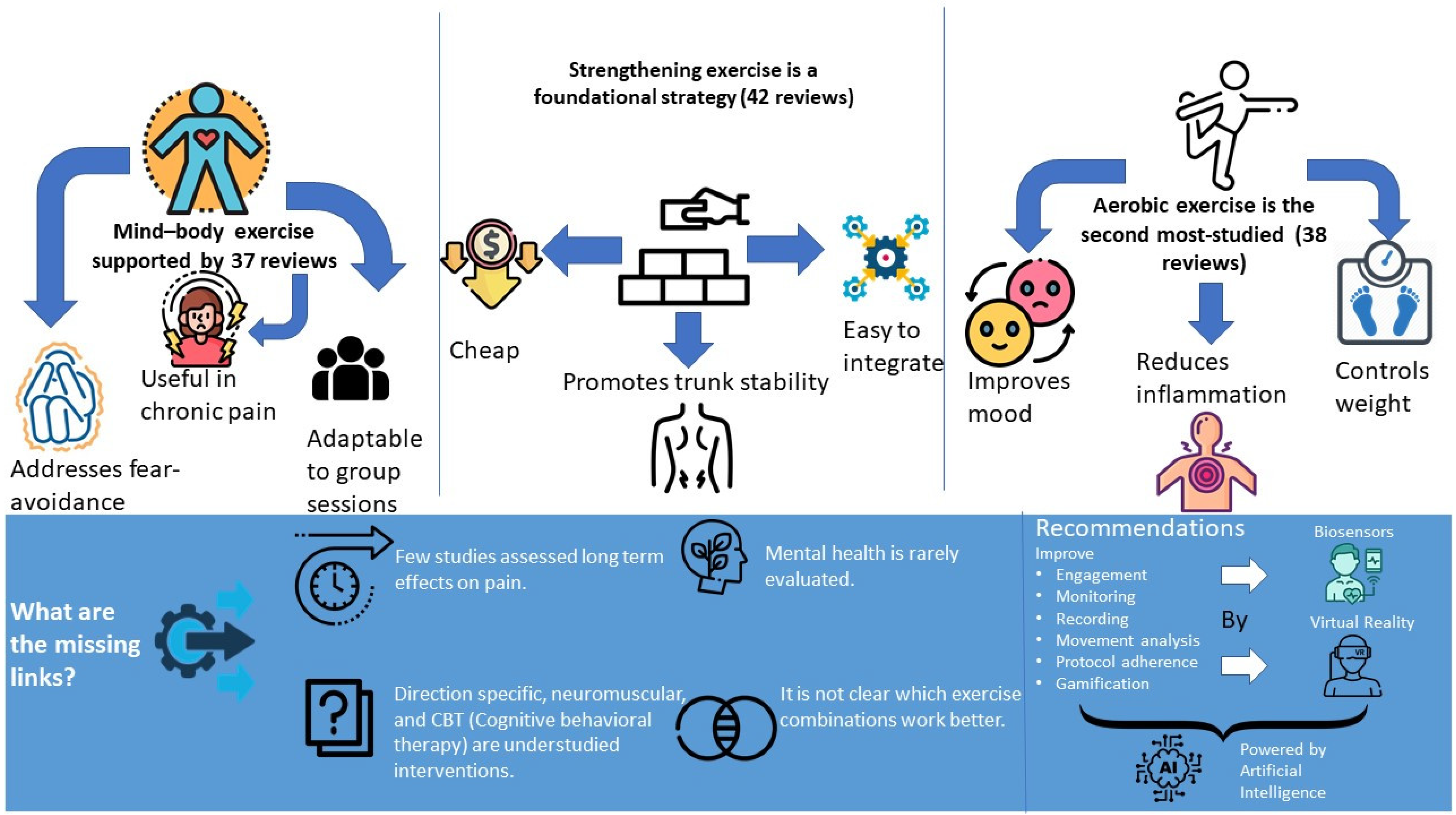
4.1. Summary of Key Findings
4.2. Comparison with the Existing Literature
4.3. Study Strengths and Limitations
4.4. Implications for Practice and Policy
4.5. Implications for Further Research
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hoy, D.; March, L.; Brooks, P.; Blyth, F.; Woolf, A.; Bain, C.; Williams, G.; Smith, E.; Vos, T.; Barendregt, J.; et al. The global burden of low back pain: Estimates from the Global Burden of Disease 2010 study. Ann. Rheum. Dis. 2014, 73, 968–974. [Google Scholar] [CrossRef] [PubMed]
- Ge, L.; Pereira, M.J.; Yap, C.W.; Heng, B.H. Chronic low back pain and its impact on physical function, mental health, and health-related quality of life: A cross-sectional study in Singapore. Sci. Rep. 2022, 12, 20040. [Google Scholar] [CrossRef]
- Steinmetz, A. Back pain treatment: A new perspective. Ther. Adv. Musculoskelet. Dis. 2022, 14. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Kolaski, K.; Logan, L.R.; Ioannidis, J.P.A. Guidance to best tools and practices for systematic reviews. Syst. Rev. 2023, 12, 96. [Google Scholar] [CrossRef]
- Shea, B.J.; Reeves, B.C.; Wells, G.; Thuku, M.; Hamel, C.; Moran, J.; Moher, D.; Tugwell, P.; Welch, V.; Kristjansson, E.; et al. AMSTAR 2: A critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ 2017, 358, j4008. [Google Scholar] [CrossRef]
- Zhang, S.K.; Gu, M.L.; Zhang, T.; Xu, H.; Mao, S.J.; Zhou, W.S. Effects of exercise therapy on disability, mobility, and quality of life in the elderly with chronic low back pain: A systematic review and meta-analysis of randomized controlled trials. J. Orthop. Surg. Res. 2023, 18, 513. [Google Scholar] [CrossRef]
- Ferraz, V.D.S.; Peixoto, C.; Ferreira Resstel, A.P.; Cerqueira De Paula, Y.T.; Gomes De Souza Pegorare, A.B. Effect of the pilates method on pain and quality of life in pregnancy: A systematic review and meta-analysis. J. Bodyw. Mov. Ther. 2023, 35, 220–227. [Google Scholar] [CrossRef]
- Gilanyi, Y.L.; Wewege, M.A.; Shah, B.; Cashin, A.G.; Williams, C.M.; Davidson, S.R.E.; McAuley, J.H.; Jones, M.D. Exercise Increases Pain Self-efficacy in Adults with Nonspecific Chronic Low Back Pain: A Systematic Review and Meta-analysis. J. Orthop. Sports Phys. Ther. 2023, 53, 335–342. [Google Scholar] [CrossRef] [PubMed]
- Wong, C.M.; Rugg, B.; Geere, J. The effects of Pilates exercise in comparison to other forms of exercise on pain and disability in individuals with chronic non-specific low back pain: A systematic review with meta-analysis. Musculoskelet. Care 2023, 21, 78–96. [Google Scholar] [CrossRef] [PubMed]
- Heidari, F.; Mohammad Rahimi, N.; Aminzadeh, R. Aquatic Exercise Impact on Pain Intensity, Disability and Quality of Life in Adults with Low Back Pain: A Systematic Review and Meta-analysis. Biol. Res. Nurs. 2023, 25, 527–541. [Google Scholar] [CrossRef]
- Yu, Z.; Yin, Y.; Wang, J.; Zhang, X.; Cai, H.; Peng, F. Efficacy of Pilates on Pain, Functional Disorders and Quality of Life in Patients with Chronic Low Back Pain: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2023, 20, 2850. [Google Scholar] [CrossRef]
- Syroyid Syroyid, I.; Cavero-Redondo, I.; Syroyid Syroyid, B. Effects of Resistance Training on Pain Control and Physical Function in Older Adults with Low Back Pain: A Systematic Review with Meta-analysis. J. Geriatr. Phys. Ther. 2023, 46, E113–E126. [Google Scholar] [CrossRef]
- Ram, A.K.; Summers, S.J.; Booth, J.; Gibbs, M.T.; Jones, M.D. Higher intensity exercise reduces disability more than lower intensity exercise in adults with chronic low back pain: A systematic review and meta-analysis. Musculoskelet. Care 2023, 21, 611–622. [Google Scholar] [CrossRef]
- Prat-Luri, A.; De Los Rios-Calonge, J.; Moreno-Navarro, P.; Manresa-Rocamora, A.; Vera-Garcia, F.J.; Barbado, D. Effect of Trunk-Focused Exercises on Pain, Disability, Quality of Life, and Trunk Physical Fitness in Low Back Pain and How Potential Effect Modifiers Modulate Their Effects: A Systematic Review with Meta-analyses. J. Orthop. Sports Phys. Ther. 2023, 53, 64–93. [Google Scholar] [CrossRef]
- Gilliam, J.R.; George, S.Z.; Norman, K.S.; Hendren, S.; Sahu, P.K.; Silfies, S.P. Mind-Body Exercise Performed by Physical Therapists for Reducing Pain and Disability in Low Back Pain: A Systematic Review with Meta-analysis. Arch. Phys. Med. Rehabil. 2023, 104, 776–789. [Google Scholar] [CrossRef] [PubMed]
- Hernandez-Lucas, P.; Leirós-Rodríguez, R.; Lopez-Barreiro, J.; García-Soidán, J.L. Is the combination of exercise therapy and health education more effective than usual medical care in the prevention of non-specific back pain? A systematic review with meta-analysis. Ann. Med. 2022, 54, 3106–3115. [Google Scholar] [CrossRef] [PubMed]
- Kazeminia, M.; Rajati, F.; Rajati, M. The effect of pelvic floor muscle-strengthening exercises on low back pain: A systematic review and meta-analysis on randomized clinical trials. Neurol. Sci. 2023, 44, 859–872. [Google Scholar] [CrossRef]
- Santos, G.K.; Gonçalves De Oliveira, R.; Campos De Oliveira, L.; Ferreira, C.; De Oliveira, C.; Andraus, R.A.; Ngomo, S.; Fusco, A.; Cortis, C.; Da Silva, R.A. Effectiveness of muscle energy technique in patients with nonspecific low back pain: A systematic review with meta-analysis. Eur. J. Phys. Rehabil. Med. 2023, 58, 827–837. Available online: https://www.minervamedica.it/index2.php?show=R33Y2022N06A0827 (accessed on 8 June 2025). [CrossRef] [PubMed]
- Belavy, D.L.; Tagliaferri, S.D.; Buntine, P.; Saueressig, T.; Ehrenbrusthoff, K.; Chen, X.; Diwan, A.; Miller, C.T.; Owen, P.J. Interventions for promoting evidence-based guideline-consistent surgery in low back pain: A systematic review and meta-analysis of randomised controlled trials. Eur. Spine J. 2022, 31, 2851–2865. [Google Scholar] [CrossRef]
- Wood, L.; Foster, N.E.; Lewis, M.; Bronfort, G.; Groessl, E.J.; Hewitt, C.; Miyamoto, G.C.; Reme, S.E.; Bishop, A. Matching the Outcomes to Treatment Targets of Exercise for Low Back Pain: Does it Make a Difference? Results of Secondary Analyses From Individual Patient Data of Randomised Controlled Trials and Pooling of Results Across Trials in Comparative Meta-analysis. Arch. Phys. Med. Rehabil. 2023, 104, 218–228. [Google Scholar] [CrossRef]
- Fleckenstein, J.; Floessel, P.; Engel, T.; Krempel, L.; Stoll, J.; Behrens, M.; Niederer, D. Individualized Exercise in Chronic Non-Specific Low Back Pain: A Systematic Review with Meta-Analysis on the Effects of Exercise Alone or in Combination with Psychological Interventions on Pain and Disability. J. Pain 2022, 23, 1856–1873. [Google Scholar] [CrossRef] [PubMed]
- Shanbehzadeh, S.; ShahAli, S.; Hides, J.; Ebrahimi-Takamjani, I.; Rasouli, O. Effect of Motor Control Training on Trunk Muscle Morphometry, Pain, and Disability in People with Chronic Low Back Pain: A Systematic Review and Meta-Analysis. J. Manip. Physiol. Ther. 2022, 45, 202–215. [Google Scholar] [CrossRef]
- Fernández-Rodríguez, R.; Álvarez-Bueno, C.; Cavero-Redondo, I.; Torres-Costoso, A.; Pozuelo-Carrascosa, D.P.; Reina-Gutiérrez, S.; Pascual-Morena, C.; Martínez-Vizcaíno, V. Best Exercise Options for Reducing Pain and Disability in Adults with Chronic Low Back Pain: Pilates, Strength, Core-Based, and Mind-Body. A Network Meta-analysis. J. Orthop. Sports Phys. Ther. 2022, 52, 505–521. [Google Scholar] [CrossRef]
- Dimitrijević, V.; Šćepanović, T.; Milankov, V.; Milankov, M.; Drid, P. Effects of Corrective Exercises on Lumbar Lordotic Angle Correction: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2022, 19, 4906. [Google Scholar] [CrossRef]
- Sutanto, D.; Ho, R.S.T.; Poon, E.T.C.; Yang, Y.; Wong, S.H.S. Effects of Different Trunk Training Methods for Chronic Low Back Pain: A Meta-Analysis. Int. J. Environ. Res. Public Health 2022, 19, 2863. [Google Scholar] [CrossRef] [PubMed]
- Mapinduzi, J.; Ndacayisaba, G.; Mahaudens, P.; Hidalgo, B. Effectiveness of motor control exercises versus other musculoskeletal therapies in patients with pelvic girdle pain of sacroiliac joint origin: A systematic review with meta-analysis of randomized controlled trials. J. Back Musculoskelet. Rehabil. 2022, 35, 713–728. [Google Scholar] [CrossRef] [PubMed]
- Kechichian, A.; Lafrance, S.; Matifat, E.; Dubé, F.; Lussier, D.; Benhaim, P.; Perreault, K.; Filiatrault, J.; Rainville, P.; Higgins, J.; et al. Multimodal Interventions Including Rehabilitation Exercise for Older Adults with Chronic Musculoskeletal Pain: A Systematic Review and Meta-analyses of Randomized Controlled Trials. J. Geriatr. Phys. Ther. 2022, 45, 34–49. [Google Scholar] [CrossRef]
- Zhang, S.-K.; Yang, Y.; Gu, M.-L.; Mao, S.-J.; Zhou, W.-S. Effects of Low Back Pain Exercises on Pain Symptoms and Activities of Daily Living: A Systematic Review and Meta-Analysis. Percept. Mot. Skills 2022, 129, 63–89. [Google Scholar] [CrossRef]
- Arcanjo, F.L.; Martins, J.V.P.; Moté, P.; Leporace, G.; Oliveira, D.A.D.; Sousa, C.S.D.; Saquetto, M.B.; Gomes-Neto, M. Proprioceptive neuromuscular facilitation training reduces pain and disability in individuals with chronic low back pain: A systematic review and meta-analysis. Complement. Ther. Clin. Pract. 2022, 46, 101505. [Google Scholar] [CrossRef]
- Pocovi, N.C.; De Campos, T.F.; Christine Lin, C.W.; Merom, D.; Tiedemann, A.; Hancock, M.J. Walking, Cycling, and Swimming for Nonspecific Low Back Pain: A Systematic Review with Meta-analysis. J. Orthop. Sports Phys. Ther. 2022, 52, 85–99. [Google Scholar] [CrossRef]
- Rathnayake, A.P.S.; Sparkes, V.; Sheeran, L. What is the effect of low back pain self-management interventions with exercise components added? A systematic review with meta-analysis. Musculoskelet. Sci. Pract. 2021, 56, 102469. [Google Scholar] [CrossRef] [PubMed]
- Dal Farra, F.; Arippa, F.; Arru, M.; Cocco, M.; Porcu, E.; Tramontano, M.; Monticone, M. Effects of exercise on balance in patients with non-specific low back pain: A systematic review and meta-analysis. Eur. J. Phys. Rehabil. Med. 2022, 58, 423–434. Available online: https://www.minervamedica.it/index2.php?show=R33Y2022N03A0423 (accessed on 8 June 2025). [CrossRef]
- Hayden, J.A.; Ellis, J.; Ogilvie, R.; Malmivaara, A.; Van Tulder, M.W. Exercise therapy for chronic low back pain. Cochrane Database Syst. Rev. 2021, 2021, CD009790. [Google Scholar] [CrossRef]
- Hayden, J.A.; Ellis, J.; Ogilvie, R.; Stewart, S.A.; Bagg, M.K.; Stanojevic, S.; Yamato, T.P.; Saragiotto, B.T. Some types of exercise are more effective than others in people with chronic low back pain: A network meta-analysis. J. Physiother. 2021, 67, 252–262. [Google Scholar] [CrossRef]
- Quentin, C.; Bagheri, R.; Ugbolue, U.C.; Coudeyre, E.; Pélissier, C.; Descatha, A.; Menini, T.; Bouillon-Minois, J.-B.; Dutheil, F. Effect of Home Exercise Training in Patients with Nonspecific Low-Back Pain: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2021, 18, 8430. [Google Scholar] [CrossRef]
- Gao, P.; Tang, F.; Liu, W.; Mo, Y. The effects of proprioceptive neuromuscular facilitation in treating chronic low back pain: A systematic review and meta-analysis. J. Back Musculoskelet. Rehabil. 2022, 35, 21–33. [Google Scholar] [CrossRef]
- Chen, Z.; Wu, J.; Wang, X.; Wu, J.; Ren, Z. The effects of myofascial release technique for patients with low back pain: A systematic review and meta-analysis. Complement. Ther. Med. 2021, 59, 102737. [Google Scholar] [CrossRef] [PubMed]
- Zhang, C.; Li, Y.; Zhong, Y.; Feng, C.; Zhang, Z.; Wang, C. Effectiveness of motor control exercise on non-specific chronic low back pain, disability and core muscle morphological characteristics: A meta-analysis of randomized controlled trials. Eur. J. Phys. Rehabil. Med. 2021, 57, 793–806. Available online: https://www.minervamedica.it/index2.php?show=R33Y2021N05A0793 (accessed on 8 June 2025). [CrossRef]
- Sun, W.; Zhang, H.; Lv, C.; Tang, L.; Tian, S. Comparative efficacy of 12 non-drug interventions on non-specific chronic low back pain in nurses: A systematic review and network meta-analysis. J. Back Musculoskelet. Rehabil. 2021, 34, 499–510. [Google Scholar] [CrossRef] [PubMed]
- Ouellet, P.; Lafrance, S.; Pizzi, A.; Roy, J.S.; Lewis, J.; Christiansen, D.H.; Dubois, B.; Langevin, P.; Desmeules, F. Region-specific Exercises vs General Exercises in the Management of Spinal and Peripheral Musculoskeletal Disorders: A Systematic Review with Meta-analyses of Randomized Controlled Trials. Arch. Phys. Med. Rehabil. 2021, 102, 2201–2218. [Google Scholar] [CrossRef]
- Thornton, J.S.; Caneiro, J.P.; Hartvigsen, J.; Ardern, C.L.; Vinther, A.; Wilkie, K.; Trease, L.; Ackerman, K.E.; Dane, K.; McDonnell, S.-J.; et al. Treating low back pain in athletes: A systematic review with meta-analysis. Br. J. Sports Med. 2021, 55, 656–662. [Google Scholar] [CrossRef] [PubMed]
- Barros Dos Santos, A.O.; Pinto De Castro, J.B.; Lima, V.P.; Da Silva, E.B.; De Souza Vale, R.G. Effects of Physical Exercise on Low Back Pain and Cortisol Levels: A Systematic Review with Meta-Analysis of Randomized Controlled Trials. Pain Manag. 2021, 11, 49–57. [Google Scholar] [CrossRef] [PubMed]
- Mueller, J.; Niederer, D. Dose-response-relationship of stabilisation exercises in patients with chronic non-specific low back pain: A systematic review with meta-regression. Sci. Rep. 2020, 10, 16921. [Google Scholar] [CrossRef]
- Hanel, J.; Owen, P.J.; Held, S.; Tagliaferri, S.D.; Miller, C.T.; Donath, L.; Belavy, D.L. Effects of Exercise Training on Fear-Avoidance in Pain and Pain-Free Populations: Systematic Review and Meta-analysis. Sports Med. 2020, 50, 2193–2207. [Google Scholar] [CrossRef]
- Nduwimana, I.; Nindorera, F.; Thonnard, J.L.; Kossi, O. Effectiveness of walking versus mind-body therapies in chronic low back pain: A systematic review and meta-analysis of recent randomized controlled trials. Medicine 2020, 99, e21969. [Google Scholar] [CrossRef] [PubMed]
- Zhu, F.; Zhang, M.; Wang, D.; Hong, Q.; Zeng, C.; Chen, W. Yoga compared to non-exercise or physical therapy exercise on pain, disability, and quality of life for patients with chronic low back pain: A systematic review and meta-analysis of randomized controlled trials. PLoS ONE 2020, 15, e0238544. [Google Scholar] [CrossRef]
- Domingues De Freitas, C.; Costa, D.A.; Junior, N.C.; Civile, V.T. Effects of the pilates method on kinesiophobia associated with chronic non-specific low back pain: Systematic review and meta-analysis. J. Bodyw. Mov. Ther. 2020, 24, 300–306. [Google Scholar] [CrossRef]
- Casey, M.B.; Smart, K.M.; Segurado, R.; Doody, C. Multidisciplinary-based Rehabilitation (MBR) Compared with Active Physical Interventions for Pain and Disability in Adults with Chronic Pain: A Systematic Review and Meta-analysis. Clin. J. Pain 2020, 36, 874–886. [Google Scholar] [CrossRef]
- De Jesus, F.L.A.; Fukuda, T.Y.; Souza, C.; Guimarães, J.; Aquino, L.; Carvalho, G.; Powers, C.; Gomes-Neto, M. Addition of specific hip strengthening exercises to conventional rehabilitation therapy for low back pain: A systematic review and meta-analysis. Clin. Rehabil. 2020, 34, 1368–1377. [Google Scholar] [CrossRef]
- Amaral, L.K.B.; Souza, M.B.; Campos, M.G.M.; Mendonça, V.A.; Bastone, A.; Pereira, L.S.M.; Mascarenhas, R.O.; Oliveira, V.C. Efficacy of conservative therapy in older people with nonspecific low back pain: A systematic review with meta-analysis and GRADE recommendations. Arch. Gerontol. Geriatr. 2020, 90, 104177. [Google Scholar] [CrossRef]
- Wood, L.; Foster, N.E.; Lewis, M.; Bishop, A. Exercise Interventions for Persistent Non-Specific Low Back Pain—Does Matching Outcomes to Treatment Targets Make a Difference? A Systematic Review and Meta-Analysis. J. Pain 2021, 22, 107–126. [Google Scholar] [CrossRef]
- Bernard, S.; Gentilcore-Saulnier, E.; Massé-Alarie, H.; Moffet, H. Is adding pelvic floor muscle training to an exercise intervention more effective at improving pain in patients with non-specific low back pain? A systematic review of randomized controlled trials. Physiotherapy 2021, 110, 15–25. [Google Scholar] [CrossRef]
- Niederer, D.; Mueller, J. Sustainability effects of motor control stabilisation exercises on pain and function in chronic nonspecific low back pain patients: A systematic review with meta-analysis and meta-regression. PLoS ONE 2020, 15, e0227423. [Google Scholar] [CrossRef]
- Hayden, J.A.; Wilson, M.N.; Stewart, S.; Cartwright, J.L.; Smith, A.O.; Riley, R.D.; Van Tulder, M.; Bendix, T.; Cecchi, F.; Costa, L.O.P.; et al. Exercise treatment effect modifiers in persistent low back pain: An individual participant data meta-analysis of 3514 participants from 27 randomised controlled trials. Br. J. Sports Med. 2020, 54, 1277–1278. [Google Scholar] [CrossRef]
- Huang, R.; Ning, J.; Chuter, V.H.; Taylor, J.B.; Christophe, D.; Meng, Z.; Xu, Y.; Jiang, L. Exercise alone and exercise combined with education both prevent episodes of low back pain and related absenteeism: Systematic review and network meta-analysis of randomised controlled trials (RCTs) aimed at preventing back pain. Br. J. Sports Med. 2020, 54, 766–770. [Google Scholar] [CrossRef] [PubMed]
- Owen, P.J.; Miller, C.T.; Mundell, N.L.; Verswijveren, S.J.J.M.; Tagliaferri, S.D.; Brisby, H.; Bowe, S.J.; Belavy, D.L. Which specific modes of exercise training are most effective for treating low back pain? Network meta-analysis. Br. J. Sports Med. 2020, 54, 1279–1287. [Google Scholar] [CrossRef] [PubMed]
- Alzahrani, H.; Mackey, M.; Stamatakis, E.; Zadro, J.R.; Shirley, D. The association between physical activity and low back pain: A systematic review and meta-analysis of observational studies. Sci. Rep. 2019, 9, 8244. [Google Scholar] [CrossRef]
- Zhang, Q.; Jiang, S.; Young, L.; Li, F. The Effectiveness of Group-Based Physiotherapy-Led Behavioral Psychological Interventions on Adults with Chronic Low Back Pain: A Systematic Review and Meta-Analysis. Am. J. Phys. Med. Rehabil. 2019, 98, 215–225. [Google Scholar] [CrossRef] [PubMed]
- Dong, Y.; Wang, W.; Zheng, J.; Chen, S.; Qiao, J.; Wang, X. Whole Body Vibration Exercise for Chronic Musculoskeletal Pain: A Systematic Review and Meta-analysis of Randomized Controlled Trials. Arch. Phys. Med. Rehabil. 2019, 100, 2167–2178. [Google Scholar] [CrossRef]
- Li, H.; Ge, D.; Liu, S.; Zhang, W.; Wang, J.; Si, J.; Zhai, J. Baduanjin exercise for low back pain: A systematic review and meta-analysis. Complement. Ther. Med. 2019, 43, 109–116. [Google Scholar] [CrossRef]
- Alayat, M.S.M.; Alshehri, M.A.; Shousha, T.M.; Abdelgalil, A.A.; Alhasan, H.; Khayyat, O.K.; Al-Attar, W.S. The effectiveness of high intensity laser therapy in the management of spinal disorders: A systematic review and meta-analysis. J. Back Musculoskelet. Rehabil. 2019, 32, 869–884. [Google Scholar] [CrossRef] [PubMed]
- Alzahrani, H.; Mackey, M.; Stamatakis, E.; Pinheiro, M.B.; Wicks, M.; Shirley, D. The effectiveness of incidental physical activity interventions compared to other interventions in the management of people with low back pain: A systematic review and meta-analysis of randomised controlled trials. Phys. Ther. Sport 2019, 36, 34–42. [Google Scholar] [CrossRef]
- Pourahmadi, M.; Hesarikia, H.; Keshtkar, A.; Zamani, H.; Bagheri, R.; Ghanjal, A.; Shamsoddini, A. Effectiveness of Slump Stretching on Low Back Pain: A Systematic Review and Meta-analysis. Pain Med. 2019, 20, 378–396. [Google Scholar] [CrossRef]
- Nascimento, P.R.C.D.; Costa, L.O.P.; Araujo, A.C.; Poitras, S.; Bilodeau, M. Effectiveness of interventions for non-specific low back pain in older adults. A systematic review and meta-analysis. Physiotherapy 2019, 105, 147–162. [Google Scholar] [CrossRef] [PubMed]
- Bernet, B.A.; Peskura, E.T.; Meyer, S.T.; Bauch, P.C.; Donaldson, M.B. The effects of hip-targeted physical therapy interventions on low back pain: A systematic review and meta-analysis. Musculoskelet. Sci. Pract. 2019, 39, 91–100. [Google Scholar] [CrossRef]
- Davenport, M.H.; Marchand, A.A.; Mottola, M.F.; Poitras, V.J.; Gray, C.E.; Jaramillo Garcia, A.; Barrowman, N.; Sobierajski, F.; James, M.; Meah, V.L.; et al. Exercise for the prevention and treatment of low back, pelvic girdle and lumbopelvic pain during pregnancy: A systematic review and meta-analysis. Br. J. Sports Med. 2019, 53, 90–98. [Google Scholar] [CrossRef]
- Zhang, Y.; Loprinzi, P.D.; Yang, L.; Liu, J.; Liu, S.; Zou, L. The Beneficial Effects of Traditional Chinese Exercises for Adults with Low Back Pain: A Meta-Analysis of Randomized Controlled Trials. Medicina 2019, 55, 118. [Google Scholar] [CrossRef]
- Zheng, Y.-L.; Zhang, Z.-J.; Peng, M.-S.; Hu, H.-Y.; Zhang, J.; Wang, X.-Q. Whole-body vibration exercise for low back pain: A meta-analysis protocol of randomized controlled trial. Medicine 2018, 97, e12534. [Google Scholar] [CrossRef]
- Wewege, M.A.; Booth, J.; Parmenter, B.J. Aerobic vs. resistance exercise for chronic non-specific low back pain: A systematic review and meta-analysis. J. Back Musculoskelet. Rehabil. 2018, 31, 889–899. [Google Scholar] [CrossRef] [PubMed]
- Miyamoto, G.C.; Lin, C.-W.C.; Cabral, C.M.N.; Van Dongen, J.M.; Van Tulder, M.W. Cost-effectiveness of exercise therapy in the treatment of non-specific neck pain and low back pain: A systematic review with meta-analysis. Br. J. Sports Med. 2019, 53, 172–181. [Google Scholar] [CrossRef] [PubMed]
- Luomajoki, H.A.; Bonet Beltran, M.B.; Careddu, S.; Bauer, C.M. Effectiveness of movement control exercise on patients with non-specific low back pain and movement control impairment: A systematic review and meta-analysis. Musculoskelet. Sci. Pract. 2018, 36, 1–11. [Google Scholar] [CrossRef]
- Lam, O.T.; Strenger, D.M.; Chan-Fee, M.; Pham, P.T.; Preuss, R.A.; Robbins, S.M. Effectiveness of the McKenzie Method of Mechanical Diagnosis and Therapy for Treating Low Back Pain: Literature Review with Meta-analysis. J. Orthop. Sports Phys. Ther. 2018, 48, 476–490. [Google Scholar] [CrossRef]
- Coulter, I.D.; Crawford, C.; Hurwitz, E.L.; Vernon, H.; Khorsan, R.; Suttorp Booth, M.; Herman, P.M. Manipulation and mobilization for treating chronic low back pain: A systematic review and meta-analysis. Spine J. 2018, 18, 866–879. [Google Scholar] [CrossRef]
- Sitthipornvorakul, E.; Klinsophon, T.; Sihawong, R.; Janwantanakul, P. The effects of walking intervention in patients with chronic low back pain: A meta-analysis of randomized controlled trials. Musculoskelet. Sci. Pract. 2018, 34, 38–46. [Google Scholar] [CrossRef]
- Vanti, C.; Andreatta, S.; Borghi, S.; Guccione, A.A.; Pillastrini, P.; Bertozzi, L. The effectiveness of walking versus exercise on pain and function in chronic low back pain: A systematic review and meta-analysis of randomized trials. Disabil. Rehabil. 2019, 41, 622–632. [Google Scholar] [CrossRef]
- Shiri, R.; Coggon, D.; Falah-Hassani, K. Exercise for the Prevention of Low Back Pain: Systematic Review and Meta-Analysis of Controlled Trials. Am. J. Epidemiol. 2018, 187, 1093–1101. [Google Scholar] [CrossRef]
- Shiri, R.; Coggon, D.; Falah-Hassani, K. Exercise for the prevention of low back and pelvic girdle pain in pregnancy: A meta-analysis of randomized controlled trials. Eur. J. Pain 2018, 22, 19–27. [Google Scholar] [CrossRef] [PubMed]
- Shi, Z.; Zhou, H.; Lu, L.; Pan, B.; Wei, Z.; Yao, X.; Kang, Y.; Liu, L.; Feng, S. Aquatic Exercises in the Treatment of Low Back Pain: A Systematic Review of the Literature and Meta-Analysis of Eight Studies. Am. J. Phys. Med. Rehabil. 2018, 97, 116–122. [Google Scholar] [CrossRef]
- Basson, A.; Olivier, B.; Ellis, R.; Coppieters, M.; Stewart, A.; Mudzi, W. The Effectiveness of Neural Mobilization for Neuromusculoskeletal Conditions: A Systematic Review and Meta-analysis. J. Orthop. Sports Phys. Ther. 2017, 47, 593–615. [Google Scholar] [CrossRef] [PubMed]
- Shiri, R.; Falah-Hassani, K. Does leisure time physical activity protect against low back pain? Systematic review and meta-analysis of 36 prospective cohort studies. Br. J. Sports Med. 2017, 51, 1410–1418. [Google Scholar] [CrossRef]
- Geneen, L.J.; Moore, R.A.; Clarke, C.; Martin, D.; Colvin, L.A.; Smith, B.H. Physical activity and exercise for chronic pain in adults: An overview of Cochrane Reviews. Cochrane Database Syst. Rev. 2017, 2017, CD011279. [Google Scholar] [CrossRef] [PubMed]
- Nicolson, P.J.A.; Bennell, K.L.; Dobson, F.L.; Van Ginckel, A.; Holden, M.A.; Hinman, R.S. Interventions to increase adherence to therapeutic exercise in older adults with low back pain and/or hip/knee osteoarthritis: A systematic review and meta-analysis. Br. J. Sports Med. 2017, 51, 791–799. [Google Scholar] [CrossRef]
- Wieland, L.S.; Skoetz, N.; Pilkington, K.; Vempati, R.; D’Adamo, C.R.; Berman, B.M. Yoga treatment for chronic non-specific low back pain. Cochrane Database Syst. Rev. 2017, 2017, CD010671. [Google Scholar] [CrossRef] [PubMed]
- Coulombe, B.J.; Games, K.E.; Neil, E.R.; Eberman, L.E. Core Stability Exercise Versus General Exercise for Chronic Low Back Pain. J. Athl. Train. 2017, 52, 71–72. [Google Scholar] [CrossRef]
- Gomes-Neto, M.; Lopes, J.M.; Conceição, C.S.; Araujo, A.; Brasileiro, A.; Sousa, C.; Carvalho, V.O.; Arcanjo, F.L. Stabilization exercise compared to general exercises or manual therapy for the management of low back pain: A systematic review and meta-analysis. Phys. Ther. Sport 2017, 23, 136–142. [Google Scholar] [CrossRef]
- Moreira-Silva, I.; Teixeira, P.M.; Santos, R.; Abreu, S.; Moreira, C.; Mota, J. The Effects of Workplace Physical Activity Programs on Musculoskeletal Pain: A Systematic Review and Meta-Analysis. Workplace Health Saf. 2016, 64, 210–222. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, C.B.; Franco, M.R.; Maher, C.G.; Christine Lin, C.; Morelhão, P.K.; Araújo, A.C.; Negrão Filho, R.F.; Pinto, R.Z. Physical Activity Interventions for Increasing Objectively Measured Physical Activity Levels in Patients with Chronic Musculoskeletal Pain: A Systematic Review. Arthritis Care Res. 2016, 68, 1832–1842. [Google Scholar] [CrossRef]
- Peek, A.L.; Stevens, M.L. Different forms of exercise for chronic low back pain (PEDro synthesis). Br. J. Sports Med. 2016, 50, 188. [Google Scholar] [CrossRef]
- Yamato, T.P.; Maher, C.G.; Saragiotto, B.T.; Hancock, M.J.; Ostelo, R.W.; Cabral, C.M.; Menezes Costa, L.C.; Costa, L.O. Pilates for low back pain. Cochrane Database Syst. Rev. 2015, 2015, CD010265. [Google Scholar] [CrossRef]
- Searle, A.; Spink, M.; Ho, A.; Chuter, V. Exercise interventions for the treatment of chronic low back pain: A systematic review and meta-analysis of randomised controlled trials. Clin. Rehabil. 2015, 29, 1155–1167. [Google Scholar] [CrossRef] [PubMed]
- Meng, X.-G.; Yue, S.-W. Efficacy of Aerobic Exercise for Treatment of Chronic Low Back Pain: A Meta-Analysis. Am. J. Phys. Med. Rehabil. 2015, 94, 358–365. [Google Scholar] [CrossRef] [PubMed]
- Byström, M.G.; Rasmussen-Barr, E.; Grooten, W.J.A. Motor Control Exercises Reduces Pain and Disability in Chronic and Recurrent Low Back Pain: A Meta-Analysis. Spine 2013, 38, E350–E358. [Google Scholar] [CrossRef]
- Bell, J.A.; Burnett, A. Exercise for the Primary, Secondary and Tertiary Prevention of Low Back Pain in the Workplace: A Systematic Review. J. Occup. Rehabil. 2009, 19, 8–24. [Google Scholar] [CrossRef]
- Saragiotto, B.T.; Maher, C.G.; Yamato, T.P.; Costa, L.O.; Menezes Costa, L.C.; Ostelo, R.W.; Macedo, L.G. Motor control exercise for chronic non-specific low-back pain. Cochrane Database Syst. Rev. 2016, 2016, CD012004. [Google Scholar] [CrossRef]
- Gianola, S.; Bargeri, S.; Del Castillo, G.; Corbetta, D.; Turolla, A.; Andreano, A.; Moja, L.; Castellini, G. Effectiveness of treatments for acute and subacute mechanical non-specific low back pain: A systematic review with network meta-analysis. Br. J. Sports Med. 2022, 56, 41–50. [Google Scholar] [CrossRef]
- IJzelenberg, W.; Oosterhuis, T.; Hayden, J.A.; Koes, B.W.; Van Tulder, M.W.; Rubinstein, S.M.; De Zoete, A. Exercise therapy for treatment of acute non-specific low back pain. Cochrane Database Syst. Rev. 2023, 2023, CD009365. [Google Scholar] [CrossRef]
- Sowden, G.; Hill, J.C.; Morso, L.; Louw, Q.; Foster, N.E. Advancing practice for back pain through stratified care (STarT Back). Braz. J. Phys. Ther. 2018, 22, 255–264. [Google Scholar] [CrossRef]
- Enthoven, P.; Eddeborn, F.; Abbott, A.; Schröder, K.; Fors, M.; Öberg, B. Patients’ experiences of the BetterBack model of care for low back pain in primary care—A qualitative interview study. Int. J. Qual. Stud. Health Well-Being 2021, 16, 1861719. [Google Scholar] [CrossRef]
- Cieza, A.; Stucki, G.; Weigl, M.; Disler, P.; Jackel, W.; Van Der Linden, S.; Kostanjsek, N.; De Bie, R. ICF Core Sets for low back pain. J. Rehabil. Med. 2004, 36, 69–74. [Google Scholar] [CrossRef] [PubMed]
- Brea-Gómez, B.; Torres-Sánchez, I.; Ortiz-Rubio, A.; Calvache-Mateo, A.; Cabrera-Martos, I.; López-López, L.; Valenza, M.C. Virtual Reality in the Treatment of Adults with Chronic Low Back Pain: A Systematic Review and Meta-Analysis of Randomized Clinical Trials. Int. J. Environ. Res. Public Health 2021, 18, 11806. [Google Scholar] [CrossRef] [PubMed]
- Yalfani, A.; Abedi, M.; Raeisi, Z. Effects of an 8-Week Virtual Reality Training Program on Pain, Fall Risk, and Quality of Life in Elderly Women with Chronic Low Back Pain: Double-Blind Randomized Clinical Trial. Games Health J. 2022, 11, 85–92. [Google Scholar] [CrossRef] [PubMed]


| Author, Year | Study Design | Disease/Pathology, Comorbidities | N of Patients | Total Number of Studies | Type of Physical Exercise (Resistance/Aerobic, Tai Chi) | Pain Reduction Due to Exercise (+/−) | Possible Mechanisms of Pain Reduction/Exercise-Induced Hypoalgesia | Study Conclusions/Comments |
|---|---|---|---|---|---|---|---|---|
| Zhang et al., 2023 [7] | SR and MA of RCTs | CLBP | 989 | 18 | Comprehensive, strength, mind-body, traditional physical, aerobic, stretching exercises | + | Strengthening muscles, endorphin release, physical and psychological benefits, improved mobility and function, improved muscle function. | Exercise therapy effectively improves pain, dysfunction, and quality of life. Not approved for mobility. |
| Ferraz et al., 2023 [8] | SR and MA of RCTs | LBP during pregnancy | 65 | 2 | Comprehensive exercise, aerobic exercise, mind–body exercise, strength exercise, stretching exercise | + | Pilates may reduce pain through improved muscular strength and stabilization of the lumbar and pelvic regions, which are typically stressed during pregnancy. Enhanced physical stability could lead to decreased strain and discomfort. | Pilates exercise may reduce pregnancy-related low back pain more effectively than usual prenatal care or no exercise. It was recommended that Pilates should be considered a safe and beneficial option for pain management during pregnancy. |
| Gilanyi et al., 2023 [9] | SR and MA of RCTs | CNSLBP | 1121 | 17 | yoga, aerobic exercise, resistance training, combined aerobic and flexibility exercises | + | Higher PSE (pain self-efficacy) is associated with better treatment adherence and improvements in pain, disability, and emotional distress following treatment. | Interventions could be more effective if specifically designed to target key aspects of self-efficacy, potentially leading to better outcomes in pain management and functional abilities. |
| Wong et al., 2023 [10] | SR and MA of RCTs | CNSLBP | 369 for pain + 418 for disability = 787 | 11 | Pilates | + | Pilates may enhance core stability and postural alignment, which can reduce stress on the lower back and alleviate pain. | The review found no strong evidence for using one type of exercise intervention over another when managing patients with CNSLBP. |
| Heidari et al., 2023 [11] | SR and MA of RCTs | LBP | 484 | 14 | Aquatic exercise | + | Mechanisms include the supportive properties of water, which reduce load and stress on the body, potentially allowing for greater movement freedom and reducing pain sensations. | Aquatic workout interventions improve pain intensity, functional disability, and quality of life in adults with chronic LBP. |
| Yu et al., 2023 [12] | SR and MA of RCTs | CLBP | 1108 | 19 | Pilates | + | Pilates may improve pain by enhancing core muscle strength and endurance, promoting better spinal alignment and control, and improving overall somatic stability, which may in turn reduce the biomechanical stresses that contribute to pain. | Pilates is associated with positive pain relief and improvement of functional disorders in patients with chronic low back pain. |
| Syroyid et al., 2023 [13] | SR and MA of RCTs and non-RCTs | LBP | 1661 | 21 | PRT | + | Strengthening the supporting muscles and enhancing spinal stability. | PRT interventions can be beneficial for enhancing physical function in elderly individuals who have general lower back pain (LBP) that is not attributed to lumbar spinal stenosis and who have a body mass index below 27. Furthermore, in older adults with LBP unrelated to lumbar spinal stenosis, PRT interventions have been observed to reduce LBP. |
| Ram et al., 2023 [14] | SR and MA | CLBP | 214 | 4 | High-intensity and low-intensity exercise | No change | Exercise intensity might not significantly influence clinical outcomes in chronic low back pain based on the available data. | There is very low-certainty evidence from a limited number of studies that high-intensity exercise does not provide significant clinical benefits over lower-intensity exercise for reducing disability, improving pain, or enhancing quality of life in people with chronic low back pain. |
| Prat-Luri et al., 2023 [15] | SR and MA of RCTs | CNSLBP | 2391 | 40 | TEPs | + | Increased mobility in these areas may alleviate mechanical stressors contributing to back pain. | Trunk-focused exercise programs had positive effects on pain, disability, quality of life, and trunk performance compared to control groups, and on pain and disability compared to general exercises. |
| Gilliam et al., 2023 [16] | SR and MA | LBP | 558 | 8 | Pilates, yoga, and tai chi | + | Enhancing core strength, flexibility of the lower back muscles, and proper breathing for better posture control. | MB exercise interventions performed by physical therapists are more effective in the short term than non-exercise treatments for low back-related pain and disability, and Pilates interventions are more effective in the long term for pain. |
| Hernandez-Lucas et al., 2022 [17] | SR and MA of RCTs | NSLBP | 1235 | 4 | Strength training, flexibility exercises, and yoga, while the health education component included ergonomics, self-management techniques, pain neuroscience education, and stress reduction techniques | + | Pain reduction is achieved through physical improvements from exercise (such as increased strength and flexibility), combined with cognitive and behavioral changes brought about by educational interventions, which might alter pain perceptions and improve pain coping strategies. | The combination of exercise therapy and health education is more effective than usual medical care in preventing non-specific back pain. This approach not only reduces pain, but also addresses disability and kinesiophobia (fear of movement due to pain), suggesting a comprehensive benefit that extends beyond physical symptoms to include psychological aspects of chronic pain management. |
| Kazeminia et al., 2023 [18] | SR and MA of RCTs | LBP | 926 in total (456 intervention group + 470 control group) | 19 | Pelvic floor muscle-strengthening exercises | + | Strengthening pelvic floor muscles can provide better support for the pelvic organs and spine, potentially alleviating back pain by stabilizing the lower spine and reducing stress on the back. | Pelvic floor muscle-strengthening exercises significantly reduce low back pain intensity. Therefore, these exercises can be regarded as a part of a low back pain management plan. |
| Santos et al., 2023 [19] | SR and MA | NSLBP | 609 | 19 | MET | + | MET involves using voluntary muscle contractions of the patient against a controlled resistance provided by the therapist, which may help in strengthening muscles, increasing range of motion, and providing pain relief through various physiological mechanisms like improved blood flow and reduced muscle tension. | MET may not be efficient for improving incapacity related to lumbar spine issues, but it can be beneficial in reducing the intensity of LBP. |
| Belavy et al., 2022 [20] | SR and MA of RCTs | LBP | 258,329 | 6 | No physical exercises mentioned, only guideline-adherent surgical referrals for low back pain | No change | N/A | The meta-analysis is out of the scope of the topic, which is about the effect of exercise on low back pain. |
| Wood et al., 2023 [21] | Secondary analysis of previous RCTs and Comparative MA. | LBP | 1897 | 7 | Yoga, Pilates, supervised exercise Programs, McKenzie exercises, home exercises | + | Outcomes matched to exercise treatment targets tend to show greater SMDs. | Matching outcomes to treatment targets in exercise RCTs for CNSLBP might improve the detection of exercise benefits. |
| Fleckenstein et al., 2022 [22] | SR and MA | CNSLBP | 10,084 | 58 | Mixed individualized exercises, sensorimotor training, aerobic exercise, Pilates, McKenzie, back schools, and yoga | + | The effectiveness of individualized exercise may be enhanced when combined with psychological interventions, particularly cognitive-behavioral therapies, indicating that a multimodal approach could be beneficial. | Different exercises may have different effects, and it is important to find a personal set of exercises for each patient. |
| Shanbehzadeh et al., 2022 [23] | SR and MA | CLBP | 763 | 15 | Motor control exercise training | + | Increased muscle activation, particularly of the transversus abdominis. | Increased muscle activation and improved pain and disability levels compared to other interventions, but did not increase resting muscle thickness. |
| Fernandez-Rodriguez et al., 2022 [24] | SR and NMA of RCTs | CLBP | 9710 | 118 | Pilates, mind–body, core-based, strength, stretching, aerobic, McKenzie | + | Increased muscle activation and control, enhanced mindfulness and relaxation, improved core stability and muscle strength. | The study concluded that most types of exercise were beneficial for managing chronic LBP, with Pilates, strength, and core-based exercises being the most effective in reducing pain and disability. Pilates had the highest likelihood for reducing pain and disability based on SUCRA analysis. |
| Dimitrijevic et al., 2022 [25] | SR and MA | LBP | 482 | 10 | Lumbar stabilization exercise, forward head posture-corrective exercises, William training, combining core stability with stretching exercises, sling exercise, corrective exercises of the American National Academy of Sports Medicine, and Pilates exercise | N/A | N/A | This meta-analysis concludes that physical exercises may have a positive impact on the correction of lordosis and hyperlordosis. The results became heterogeneous after the exclusion of one study from the meta-analysis. |
| Sutanto et al., 2022 [26] | SR and MA | CLBP | 2299 | 47 | Isometric and isotonic exercises, motor control exercises | + | Motor control and isotonic trunk training may be effective in reducing low back pain; however, the details are not discussed. However, it was mentioned that isometric trunk training may be effective in reducing the risk of future re-injury based on increased trunk extensor endurance. | The study concludes that isotonic trunk training and motor control are effective in reducing low back pain; however, isometric exercises demonstrated low effectiveness. Further research on how these exercises influence low back pain is needed. |
| Mapinduzi et al., 2022 [27] | SR and MA of RCTs | NSLBP | 1407 | 12 | Motor control exercises | No change | The mechanism remains unclear, but it is suggested that staying physically active may reduce the level of biomechanical change, which may reduce the load on the back, increase the stabilization of joints, and segmental motion. | MSKTs were found to be more effective than MCE in terms of pain reduction, so the combination of both should be used for the most effective outcome. |
| Kechichian et al., 2022 [28] | SR and MA of RCTs | CLBP | 2322 | 16 | Stretching, aerobic, strengthening, and functional tasks, repetitions of step-up, and walking | + | N/A | The meta-analysis suggests that there might be bias in the studies included and concludes that exercises might be effective in reducing pain and improving the functional performance of the participants. |
| Zhang et al., 2022 [29] | SR and MA of RCTs | LBP | 910 | 18 | Tai chi and wu qin xi, aerobic exercise, core stability exercises, resistance training, and integrated training | + | Improved blood circulation, improving joint mobility, improving the protective effect of the spine, reducing stress, and enhancing euphoria. | The meta-analysis concludes that exercises can reduce low back pain in middle-aged and elderly adults. It is recommended to take tai chi and wu qin xi for at least 12 weeks, three times a week. |
| Arcanjo et al., 2022 [30] | SR and MA of RCTs | CLBP | 722 | 16 | PNF | + | Exercises may improve neuromuscular control and motor function by improving movement efficiency, which may reduce pain and improve physical function. | A study suggests that PNF can be used in rehabilitation, since it can improve pain and disability in the lower back. However, the authors suggest that studies and evidence of higher quality are needed to prove this conclusion. |
| Pocovi et al., 2022 [31] | SR and MA | NSLBP | 2362 | 19 | Walking, cycling, and swimming | + | N/A | The authors identified that walking, swimming, and cycling were less effective in reducing low back pain in comparison with other alternatives. So, it is better for patients to try more effective exercises. |
| Rathnayake et al., 2021 [32] | SR and MA of RCTs | CLBP | 1866 | 9 | Self-management interventions with exercise components added | + | N/A | The review identified that SMIs may have a positive effect on patients with CLBP; this effect may vary by duration. |
| Dal Farra et al., 2022 [33] | SR and MA | NSLBP | 521 | 12 | Spinal stabilization exercise, muscle energy technique, Pilates exercise program, whole-body vibration training, Pilates exercises | N/A | Muscle endurance, functional stabilization, proprioception, coordination, and flexibility. | The systematic review and meta-analysis found very low-quality evidence that exercise is effective in improving balance-related outcomes. |
| Hayden et al., 2021 (a) [34] | SR and MA | CNSLBP | 24,486 | 249 | Core strengthening, Pilates, stretching, aerobic exercise | + | Increase in muscle and joint strength, and improvement in muscle function and range of motion. | The study found moderate-certainty evidence that exercise is probably effective for the treatment of chronic low back pain compared to no treatment, usual care, or placebo for pain. |
| Hayden et al., 2021 (b) [35] | SR and NMA | CNSLBP | 20,969 | 217 | Pilates, McKenzie therapy, and functional restoration for chronic low back pain | + | Strengthening of muscles and improvement in posture, increased production of neurotrophic factors, and psychological factors | The study provides strong evidence supporting the effectiveness of Pilates, McKenzie therapy, and functional restoration as exercise treatments for reducing pain and functional limitations in individuals with chronic low back pain. |
| Quentin et al., 2021 [36] | SR and MA | NSLBP | 9588 | 33 | Home-based exercises, trunk, pelvic, leg stretching exercises, and yoga | + | Improvement in pain intensity and functional limitation. | Home-based exercise training was found to be effective in reducing pain intensity and improving functional limitation in patients with non-specific low back pain. |
| Gao et al., 2022 [37] | SR and MA | CLBP | 410 | 12 | Trunk muscle training, PNF, and electromagnetic stimulation | + | Improving trunk proprioception, muscle strength, exercise control, balance, and endurance. | Proprioceptive neuromuscular facilitation showed beneficial effects in relieving pain and improving waist function in patients with chronic low back pain; however, PNF did not significantly improve dynamic balance compared to the control group. |
| Chen et al., 2021 [38] | SR and MA | LBP | 386 | 8 | MFR alone or MFR combined with physical therapy, manual therapy, or exercise therapy for low back pain | No change | Soft tissue release and extension, improvement of local blood circulation, and improvement of muscle pain, stiffness, or excessive fatigue to a certain extent. | The findings suggest that MFR can improve the effect of physical therapy alone and exercise therapy alone, and that MFR can be an effective adjuvant therapy. |
| Zhang et al., 2021 [39] | MA of RCTs | CNSLBP | 1333 | 18 | Motor control exercise and sham treatment, hands-on therapies, and hands-off therapies | + | Improvement in muscle strength and stability, reduction in inflammation, and psychological factors. | Motor control exercise was associated with a significant reduction in pain compared to sham treatment and hands-off therapies for non-specific chronic low back pain. |
| Sun et al., 2021 [40] | SR and NMA | CNSLBP | 7116 | 31 | Low back exercise, targeted muscle strength exercises, and stretching exercises | + | Improvements in muscle strength and flexibility, release of neurotrophic factors, and improved blood circulation. | Low back exercise plus health education is the most effective approach for reducing CNSCLBP in nurses. |
| Ouellet et al., 2021 [41] | SR and MA of RCTs | NSLBP | 1719 | 18 | Tai chi chuan, core stability training, aerobic exercise, resistance exercise, and yoga exercise | No change | Improvement in muscle strength and stability, reduction in inflammation, and oxidative stress. | A study suggests that exercise can lead to pain reduction in musculoskeletal conditions. |
| Thornton et al., 2021 [42] | SR and MA | LBP | 541 | 14 | Exercise, massage, biomechanical modifications, and manual therapy | + | Improvements in muscle strength. | While several treatments for low back pain in athletes improved pain and function, it remains unclear what the most effective treatments are. |
| Barros-Dos-Santos et al., 2021 [43] | SR and MA of RCTs | CLBP | 169 (85 exercise group + 84 control) | 4 | Physical exercise, interventions with qigong, core stabilization, and aerobic exercises | + | Improved muscle strength and stability, improved blood flow, and tissue healing. | Physical exercise, when performed for at least 6 weeks, is effective in reducing low back pain levels in individuals with chronic LBP. |
| Mueller and Niederer, 2020 [44] | SR and MR | CNSLBP | 2786 | 50 | Stabilization exercises | + | Improvements in muscle strength. | Stabilization exercises had a significant effect on reducing pain and disability in patients with chronic non-specific low back pain. However, there are limitations in exercise trials. |
| Hanel et al., 2020 [45] | SR and MA | CLBP | 2014 | 17 | Exercise training, general practitioner care, and psychological interventions | N/A | Activation of pain inhibitory pathways, improvements in mood, and stress reduction. | Low to very low-quality evidence that exercise training alone may be effective in reducing fear-avoidance beliefs. |
| Nduwimana et al., 2020 [46] | SR and MA of RCTs | CLBP | 3193 | 31 | Walking, yoga, and control interventions | + | The reduction of blood glucose levels in patients with type 2 diabetes maintains functional capabilities, increasing spine motor control and fitness levels, stimulating the brain’s release of serotonin and endorphins, which reduce pain and improve mood. | In the short term, walking has the same effectiveness as control interventions in pain reduction and activity limitation, while yoga is more effective than control interventions. But the results do not provide sufficient proof to support the clinical effectiveness of meditation interventions in CLBP treatment, given the limited number of available trials. |
| Zhu et al., 2020 [47] | SR and MA of RCTs | CLBP | 1466 (exercise only) | 18 (9 exercise only) | Yoga, physical therapy, and conventional therapeutic exercises | + | Improving flexibility, mobility, and stability in muscles and joints, spinal alignment and posture, increasing mental and physical relaxation, controlling breath, and improving body awareness. | Yoga was as effective for pain and disability as any other training or physical exercise. Based on the merging outcome, yoga may not increase mental and physical quality level of life. There were no studies studying pain in the long-term. |
| Domingues-De-Freitas et al., 2020 [48] | SR and MA | CNSLBP | 507 | 5 | Pilates exercises | N/A | Improving the effects of kinesiophobia, promoting the movement pattern that the patient is afraid of and that produces pain. | Pilates exercises are more effective at relieving kinesiophobia related to persistent non-specific LBP than limited intervention or no therapy. |
| Casey et al., 2020 [49] | SR and MA | CLBP | NA | 27 | Individualized treatment with a cognitive-behavioral therapy component | + | Reducing disability and improving quality of life. | Low-quality proof to propose that multidisciplinary-based rehabilitation is superior to active physical interventions in lowering the pain levels and functional limitations in people suffering from chronic pain over the long and short term. |
| DeJesus et al., 2020 [50] | SR and MA | LBP | 309 | 5 | Specific hip strengthening exercises, mobilization techniques | + | Gluteal muscles provide pelvis stability, which in turn provides a stable base for spine function (especially during single-limb tasks). | For those with LBP, adding targeted hip strengthening exercises to traditional treatment for rehabilitation may help reduce pain and disability. |
| Amaral et al., 2020 [51] | SR and MA and GRADE recommendations | NSLBP | 758 | 11 | Acupuncture, auriculotherapy, exercise (on coping strategies and strength), meditation, self-management, trigger-point acupuncture, and CBT | + | Still unknown. | For elderly patients with low back pain, exercise and trigger point acupuncture have positive short-term effects on pain and impairment. However, information about the long- and medium-term efficacy of conservative therapy is still lacking, namely, regarding other significant outcomes in this particular population. |
| Wood et al., 2021 [52] | SR and MA | NSLBP | 5870 | 27 | Strengthening exercise, spinal stabilization and motor control exercise, stretching focused exercise (yoga, Pilates, tai chi), McKenzie, Godelieve Denys–Struyf or Cesar exercise therapy | + | Spinal stabilization, strengthening muscles, stretching, and flexibility, improving motor control, movement patterns, and activation of muscles. | Training interventions might be more efficient than recent publications, if the results of the therapies match the intervention targets better. |
| Bernard et al., 2021 [53] | SR of RCTs and MA | NSLBP | 200 | 6 | Pelvic floor muscle training (strength, coordination, and endurance exercises) | + | PFM contraction causes the transversus abdominis muscle, which controls the lumbar spine, to co-activate and raise intra-abdominal pressure. Stiffening the sacroiliac joint in women via PFM contraction. | Very low-quality data indicates that there may be little advantage to combining PFMT with another exercise treatment for non-specific low back pain in terms of pain intensity. An integrated lumbopelvic exercise program that includes PFMT with a longer duration is likely to affect pain outcomes in a positive manner, although the change in magnitude did not achieve minimal clinically important change. |
| Niederer and Mueller, 2020 [54] | SR and MA and MR | CNSLBP | 1081 | 2 CTs + 8 RCTs = 10 studies | Motor control exercise | + | Release of beta-endorphins, both spinal and supraspinal, by activation of μ-opioid receptors. | When comparing exercises focused on stabilization of motor control to other types of control, low- to intermediate-quality proof was found for a lasting favorable impact of the first one on pain and inability in people with LBP. The impacts of the subgroups are less evident, and neither the type, nor the dosage of the comparator, nor the direction of short-term, mid-term, or long-term is made obvious. |
| Hayden et al., 2020 [55] | MA of RCTs | LBP | 3514 | 27 | Exercise therapy (yoga, stretching, etc.), manual therapy, education, or psychological therapy | + | Decreasing pain and improving function. | For persisting non-specific low back pain (LBP) results, exercise therapy had minimal positive effects. It seems that people who are taking pharmaceuticals for their LBP, as well as those who have work that does not demand heavy physical activities, may obtain more advantages from exercising compared to other therapies. |
| Huang et al., 2020 [56] | SR and NMA of RCTs | LBP | N/A | 40 | Standard care, normal activity, routinely performed military exercises, ergonomic advice, and video training control | + | N/A | Both training alone and exercise in conjunction with education can stop LBP episodes and absenteeism associated with LBP. |
| Owen et al., 2020 [57] | NMA | CNSLBP | 5578 | 89 studies | Aerobic, resistance, stabilization/motor control exercise, yoga, Pilates, water-based training, McKenzie exercise | + | Improving mental health, trunk muscle strength, improving physical function. | For adults with CNSCLBP, there is low-quality data to suggest that the most beneficial therapies are Pilates, stabilization control, resistance training, and aerobic exercise training, in expectation of the desired outcome. Additionally, exercise instruction could be more beneficial than direct therapy from a therapist. |
| Alzahrani et al., 2019 [58] | SR and MA | LBP | 95,796 | 24 | LTPA, transportation and domestic activities, walking, cycling, gardening, swimming, aerobics, jogging | + | Increasing muscle strength and flexibility. | Low back pain and physical activity have an inverse relationship. A medium activity level led to a lower prevalence of LBP. |
| Zhang et al., 2019 (a) [59] | MA of RCTs | LBP | 886 | 11 | Traditional Chinese exercises (tai chi, qigong, wuqinxi, yijinjing, baduanjin) | + | Posture control, improvement of core strength, lumbar muscular flexibility, and breathing. | Evidence of a positive effect on lower back pain intensity reduction. Recommend conducting further studies on the topic |
| Dong et al., 2019 [60] | SR and MA of RCTs | CLBP | 680 | 16 | Whole-body vibration exercises | + | Tonic vibration reflexes, spinal and supraspinal neurophysiological mechanisms. | Evidence of a positive effect on chronic musculoskeletal pain. Shows worse results than “traditional treatment.” |
| Li et al., 2019 [61] | SR and MA | LBP | 519 | 9 | Baduanjin | + | Improving back and abdominal muscle strength and spine curvature. | Shows minor improvement in pain relief. Evidence is limited, so a larger-scale and well-designed study is warranted. |
| Alayat et al., 2019 [62] | SR and MA | LBP | 15 (LBP) | 1 (LBP) | Stretching, strength, breathing, stabilizing, mobilizing, lumbar isometric and postural exercises, and physical therapy in combination with high-intensity laser therapy | + | Decreasing inflammation, slowing down the transmission of pain signals, and inducing the production of morphine-mimetic substances. | Low-quality evidence of effective pain relief improvement in combination with high-intensity laser therapy. |
| Alzahrani et al., 2019 [63] | SR and MA of RCTs | LBP | 422 | 3 | Walking (Nordic or pedometer-based) | + | Improving overall health, reducing the risk of obesity and musculoskeletal diseases. | Indefinite evidence for no change in lower back pain. Requires further research. |
| Pourahmadi et al., 2019 [64] | SR and MA | LBP | 515 | 12 | Slump stretching, occasionally in combination with stabilization exercises, or exercises | + | Dispersing intraneural edema, restoring pressure gradients, relieving hypoxia, improving associated symptoms in neurogenic pain syndromes, relieving local tension, and reducing inflammation. | Both very low-quality and high-quality evidence for alleviating lower back pain. Recommend researching long-term effects for slump stretching. |
| Nascimento et al., 2019 [65] | SR and MA | NSLBP | 1857 | 18 | Stretching, flexibility, strength, and/or aerobic exercise, yoga, qigong, Pilates, and/or walking | No change | Increasing muscle strength and flexibility. | Limited evidence for a positive change in pain among older adults. |
| Bernet et al., 2019 [66] | SR and MA | LBP | 387 | 6 | Hip strengthening and active resistance exercises, or aquatic-resisted exercises with stretching, strengthening, and aerobic exercises | + | Increasing hip strength and flexibility due to its anatomical interrelationship with the lower back. | No evidence of a statistically significant reduction in pain. |
| Davenport et al., 2019 [67] | SR and MA | LBP during pregnancy | 52,297 | 32 | Aerobic exercises, yoga, specific strengthening exercises, and/or general strengthening exercises | + | Decreasing load on the spine, improving joint stabilization, providing better spinal alignment and segmental motion, and reversing trunk muscle imbalance. | Sufficient evidence for reducing the severity of low back pain. Not possible to distinguish between low back pain subjects and the rest from the paper alone. |
| Zhang et al., 2019 (b) [68] | SR and MA of RCTs | CLBP | 2189 + 2210 (control) = 4399 | 13 | Stretching, postural, respiratory, aerobic, strengthening, cardiovascular, movement, and/or core exercises | + | Promoting a healthy lifestyle and enhancing self-management skills. | Insufficient evidence to support it being universally prescribed. Has a long-term beneficial effect. |
| Zheng et al., 2018 [69] | MA protocol of RCTs | LBP | N/A | N/A | Whole-body vibration | N/A | Activating muscle fibers, strengthening core stability muscles, relaxing paravertebral muscles, and improving proprioceptive function. | The work provides no useful information, since it is a protocol for a potential study. |
| Wewege et al., 2018 [70] | SR and MA | CNSLBP | 333 | 6 | Progressive aerobic training, or progressive resistance training | + | Improving cardiovascular fitness, strengthening. | Sufficient evidence to show that both methods are effective, while neither is superior. Requires studies that combine the two methods. |
| Miyamoto et al., 2019 [71] | SR and MA | NSLBP | varies from 80 to 1287 | 22 | General exercise, yoga exercise, stretching, aerobic, strengthening, walking, and manual therapy | + | N/A | For neck pain and subacute and chronic low back pain, exercise therapy is cost-effective, although its results and cost-effectiveness are comparable to those of other therapies. |
| Luomajoki et al., 2018 [72] | SR and MA | NSLBP | 781 | 11 | Movement control exercise, physical exercise, high-load training, specific trunk movements, posture free of pain, physiotherapy, spinal manipulation therapies, muscle energy techniques, therapeutic massage, therapeutic ultrasound, traction | + | Pain duration decreased, pain intensity decreased, posture control improved, strengthening of flexor, extensor, and oblique trunk muscles, and patient education, functional-activity modifications in subject’s trunk movements, individual sensorimotor and cognitive learning. | The MVCE intervention appears to produce better disability improvement than other therapies in individuals with non-specific low back pain and motor control impairments, both in the short and long term. However, the majority of pain relief occurs in the near term, and early patient identification for MVCI is essential. |
| Lam et al., 2018 [73] | SR and MA | LBP | N/A | 17 studies | Physical therapy, manual therapy, joint mobilizations, motion exercise, stretching exercise | + | Pain reduction, improved physical condition. | Moderate to strong evidence suggests that, when it comes to reducing pain and impairment in patients with acute low back pain, MDT CLBP is not superior to alternative rehabilitation options. However, compared to other rehabilitation interventions, there is moderate to strong evidence that MDT is more effective in reducing pain and disability for patients with chronic low back pain; however, the degree of superiority may differ depending on the particular type of intervention being compared to MDT. |
| Coulter et al., 2018 [74] | SR and MA | CLBP | 1176 | 9 | Spinal manipulation therapy, behavioral therapy, exercise therapy, transcutaneous electrical nerve stimulation, interferential currents, low-level laser therapy, yoga, massage, acupuncture, superficial heat therapy, physiotherapy, massage, chiropractic, occupational, and osteopathic therapies | + | Reduction in pain, reduction in disability, improved health-related quality of life. | Both manipulation and mobilization are likely to improve function and reduce pain in people with chronic low back pain, according to moderate-quality data; however, manipulation appears to have a greater overall impact than mobilization. Furthermore, it is thought that both of these medicines are safe, and the application of multimodal programs may also be promising. |
| Sitthipornvorakul et al., 2018 [75] | MA of RCTs | CLBP | N/A | 13 | Muscle strengthening, flexibility, and aerobic fitness training, walking | + | Aerobic capacity, body mass index, systolic/diastolic blood pressure, triglyceride levels, and high-density lipoprotein cholesterol levels. | Walking is a simple and easily accessible activity that can be used to minimize disability and relieve pain in the treatment of persistent low back pain, provided that other high-quality research shows different results. |
| Vanti et al., 2019 [76] | SR and MA of RTs | CLBP | 329 | 5 | Walking exercise, walking techniques, circuit training exercise, aerobic exercise, trunk, upper limb, and lower limb strengthening | No change | Pain, disability, quality of life, and fear avoidance improved. | Exercise and walking both have advantages for people with chronic low back pain. It is necessary to conduct more research using bigger sample sizes and various walking techniques. |
| Shiri et al., 2018 (a) [77] | SR and MA of CTs | LBP | 3015 | 8 RCTs + 6 trials = 14 studies | Stretching exercise, strengthening exercise, aerobic fitness, endurance and coordination exercise, yoga, neuromuscular exercise, combination posture and balance exercise, | + | Improved strength, knowledge about health and work conditions, and health promotion. | According to the meta-analysis, a reasonable guideline for preventing lower back discomfort in the general population is to combine strength training with either stretching or aerobic exercises, performed two to three times per week. Future studies should look into how encouraging spinal exercises affects the amount of time people spend in the hospital and miss work because of lower back discomfort. |
| Shiri et al., 2018 (b) [78] | MA of RCTs | LBP during pregnancy | 2347 | 11 | energy expenditure exercise, water gymnastics, sitting pelvic tilt exercise, strengthening exercises for abdominal, hamstrings, and spinal muscles, low-impact gymnastics and strengthening exercises, aerobic, strengthening, stretching and relaxation, flexibility and endurance, resistance exercises, pelvic floor muscle training, or balance exercises | + | Plausible protective effect from pain, exercise improves muscle strength and endurance, and seems to be more effective in the prevention of new episodes of low back pain. | There is inconclusive information about the effect of exercise on pelvic girdle pain; however, it appears to minimize the incidence of low back pain in pregnant women and the amount of sick leave attributed to lumbopelvic discomfort. |
| Shi et al., 2018 [79] | SR and MA | LBP | 331 | 8 | Aquatic exercise, hydrotherapy, MMPTP + DWR, DWR, and GP | + | Increased physical function. | More research is required to validate the benefits of aquatic exercise for people with lower back pain and improve physical function. |
| Basson et al., 2017 [80] | SR and MA | NSLBP | 1759 | 40 | Neural mobilization exercise, lumbar mobilization exercise, stabilization exercise, slump stretching, manual therapy, nerve gliding exercise, tendon gliding exercises, and splinting | + | Improved functional status scale, median nerve distal motor latency, education in intraneural edema, decreased intraneural edema, decreased temporal summation. | In difficult cases such as persistent lower back pain, neck pain, and plantar heel pain, mobilization techniques help with pain and function and provide direction for carpal tunnel syndrome and pain management. |
| Shiri and Falah-Hassani, 2017 [81] | SR and MA | LBP | 15,475 | 36 | Physical activity | + | Protection from frequent or chronic low back pain. | Physical activity during leisure time may offer a small protective advantage against the development of recurrent or persistent lower back pain. Given the shortcomings of the initial research, it is crucial to interpret these results cautiously. |
| Geneen et al., 2017 [82] | Cochrane review | CLBP | 37,143 | 381 | Resistance and aerobic exercises | + | Improve support around joints, reducing stiffness, and may enhance metabolic exchange in lumbar discs, among other mechanisms. | The study acknowledges the benefits of managed chronic pain through physical exercise, suggesting potential reductions in healthcare use due to improved self-management and reduced pain severity. |
| Nicolson et al., 2017 [83] | SR and MA | LBP | 1045 | 9 | General aerobic exercise, strengthening, flexibility, balance, or body region-specific exercises | N/A | Booster sessions with a physiotherapist to better adhere to therapeutic exercise, motivational strategies, and behavioral graded exercise to improve adherence to exercise. | The meta-analysis offers reasonably reliable evidence supporting the effectiveness of booster sessions with a physiotherapist in enhancing patient adherence to therapeutic exercise among individuals with osteoarthritis. High-quality individual trials indicate that there is emerging evidence to endorse the utilization of patient motivational strategies and graded exercise with a behavioral approach to enhance exercise adherence in individuals with chronic low back pain and osteoarthritis. |
| Wieland et al., 2013 [84] | SR and MA | CNSLBP | N/A | N/A | Various yoga practices such as physical poses (asanas) and controlled breathing (pranayama), and the incorporation of meditation (dhyana) | + | Improved flexibility and muscular strength, increased mental and physical relaxation, improved body awareness. | The review provides no useful information, since it is a protocol for a potential study. |
| Coulombe et al., 2017 [85] | SR and MA | CSLBP | 414 | 5 | Core stability exercises, general exercises | + | Corset-like stability that leads to a stable Spine and a stable base of support, acts as a transfer point for powerful extremity muscles to generate forceful dynamic contractions reduce the possibility of the injury. | Short-term results showed that core stability exercises were superior to general exercise in reducing pain and enhancing back-specific functional status in individuals with lower back pain. |
| Gomes-Neto et al., 2017 [86] | SR and MA | LBP | 413 stabilization exercises + 297general exercises + 185—manual therapy = 895 | 11 | Stabilization exercises, general exercises, manual therapy | + | Increased muscles strength, enhanced muscle coordination, increased control and coordination of spine and pelvis. | Stabilization exercises were equally effective as manual therapy in reducing pain and disability, and they should be promoted as an integral component of musculoskeletal rehabilitation for individuals with lower back pain. |
| Moreira-Silva et al., 2016 [87] | SR and MA | NSLBP | N/A | 12 | Physical activity interventions at the workplace | + | Improve functionality, physical endurance, muscle strength, and joint mobility, reduce localized pain, depression, and social isolation, correct poor posture, increase bone density, relieve stress. | Limited research on the relationship between low back pain and discomfort in the arm, elbow, wrist, hand, or fingers did not yield statistically significant findings. However, there is strong and consistent evidence indicating that interventions involving physical activity in the workplace significantly reduce overall musculoskeletal pain and pain in the neck and shoulders. |
| Oliveira et al., 2016 [88] | SR and MA | CLBP | N/A | 8 published trials + 6 registered trials = 14 | Physical activity interventions | N/A | Increasing physical activity levels. | The results indicate that interventions centered around physical activity do not seem to result in a significant change in the objectively measured physical activity levels of individuals with chronic musculoskeletal pain compared to minimal or no intervention. It is important to note that the combined effect observed in the review may alter as more trial results become accessible, considering the numerous registered trials. |
| Peek and Stevens, 2016 [89] | MA | CLBP | 4109 | 39 | All forms of exercises, general exercises | + | Activation of skeletal muscles in a planned and structured manner. | The findings from the meta-analysis indicate that exercise programs for patients which include coordination and stabilization exercises, as well as strength and resistance exercises, have a notable impact on decreasing lower back pain (LBP). However, it is important to note that the study does not offer any supporting evidence for the effectiveness of cardiovascular exercise in reducing LBP. |
| Yamato et al., 2015 [90] | SR and MA of RCTs | CNSLBP | 510 | 10 | Pilates method, several stretching and strengthening exercises | No change | Improvements in strength, range of motion, coordination, balance, muscle symmetry, flexibility, proprioception (awareness of posture), body definition, and general health. | The studies included in the analysis suggest that Pilates is likely more effective than minimal intervention in the short and medium term when it comes to reducing pain and disability and improving function and the overall impression of recovery. However, when it comes to pain and disability, Pilates does not appear to be significantly more effective than other exercise methods in the short and medium term. In terms of function, other exercises were more effective than Pilates in the medium term, but not in the short term. |
| Searle et al., 2015 [91] | SR and MA of RCTs | CLBP | 4462 | 39 | Coordination/stabilization exercises, regular, purposeful, continuous exercise involving major muscle groups, comprised exercise programs with multiple components such as strengthening, stretching, endurance and aerobic training | + | Improve back strength, flexibility, range of motion, and fitness, acute improvement in mood and protection from depression. | The findings indicate that resistance and coordination/stabilization exercise programs are more effective than other interventions in managing chronic low back pain, while cardiorespiratory and combined exercise programs do not appear to provide significant benefits in the treatment of this condition. |
| Meng and Yue, 2015 [92] | MA of RCTs | CLBP | 310 | 8 clinical studies | Aerobic exercises such as walking, running, treadmill, cycling, and calisthenics | + | Diminish pain intensity and improve physical and psychological functioning. | The meta-analysis offers credible evidence that aerobic exercise can effectively reduce pain intensity and enhance the physical and psychological well-being of individuals with chronic low back pain (CLBP). Therefore, incorporating aerobic exercise into the treatment regimen may be a favorable option for managing CLBP. |
| Byström et al., 2013 [93] | MA of RCTs | CLBP | N/A | 16 | Motor control exercises | + | Improved muscle activation and coordination, enhanced core strength, improved posture and body awareness. | Among individuals with chronic and recurring low back pain, MCE appears to outperform various alternative treatments. Nevertheless, further research is required to explore which specific patient subgroups with low back pain are most responsive to MCE. |
| Bell and Burnett, 2009 [94] | SR | LBP | N/A | 10 RCTs + 5 non-RCTs = 15 | General exercise such as muscle strengthening, flexibility training or cardiovascular endurance, stabilization exercises | + | Improved core stability, decreased LBP incidence, LBP intensity, and impact of LBP and disability. | While there was robust evidence demonstrating the effectiveness of exercise in alleviating the severity of lower back pain (LBP) and its impact on daily activities, the limited quality of study methods and conflicting findings resulted in only limited support for the use of exercise to prevent LBP episodes in a workplace setting. |
| Author, Year | Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | Q9 | Q10 | Q11 | Q12 | Q13 | Q14 | Q15 | Q16 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Zhang et al., 2023 [7] | + | + | + | Partially yes | + | + | - | + | + | - | + | + | + | + | + | + |
| Ferraz et al., 2023 [8] | + | Partially yes | + | Partially yes | - | - | - | + | + | - | + | + | + | + | + | + |
| Gilanyi et al., 2023 [9] | + | + | + | Partially yes | + | + | - | + | + | - | + | + | + | + | + | - |
| Wong et al., 2023 [10] | + | + | + | Partially yes | - | - | + | + | + | - | + | + | + | + | + | - |
| Heidari et al., 2023 [11] | + | + | + | Partially yes | - | - | - | + | + | - | + | + | + | + | + | - |
| Yu et al., 2023 [12] | + | Partially yes | + | Partially yes | + | + | - | + | + | - | + | + | + | + | + | - |
| Syroyid et al., 2023 [13] | + | Partially yes | + | Partially yes | - | + | - | + | + | - | + | + | + | + | + | + |
| Ram et al., 2023 [14] | + | Partially yes | - | Partially yes | + | + | - | + | - | - | - | - | - | + | - | - |
| Prat-Luri et al., 2023 [15] | + | + | + | Partially yes | + | + | + | + | + | - | + | + | + | + | + | + |
| Gilliam et al., 2023 [16] | + | Partially yes | + | Partially yes | + | + | - | + | + | - | + | + | + | + | - | - |
| Hernandez-Lucas et al., 2022 [17] | + | + | - | Partially yes | + | + | - | + | + | - | - | - | - | + | - | - |
| Kazeminia et al., 2023 [18] | + | Partially yes | + | Partially yes | - | - | - | + | + | + | + | + | + | + | - | + |
| Santos et al., 2022 [19] | + | + | + | Partially yes | + | + | + | + | + | - | + | + | + | + | + | - |
| Belavy et al., 2022 [20] | + | Partially yes | + | - | + | + | + | + | + | + | + | - | + | + | - | - |
| Wood et al., 2022 [21] | - | - | + | - | + | + | + | + | - | - | - | - | - | + | - | - |
| Fleckenstein et al., 2022 [22] | + | + | + | Partially yes | + | + | + | + | + | - | + | + | + | - | + | + |
| Shanbehzaden et al., 2022 [23] | + | Partially yes | - | Partially yes | + | + | - | - | - | - | + | + | + | + | + | + |
| Fernandez-Rodriguez et al., 2022 [24] | + | + | + | - | + | + | + | + | + | - | + | + | + | + | + | - |
| Dimitrijevic et al., 2022 [25] | + | Partially yes | - | Partially yes | + | + | Partially yes | Partially yes | Partially yes | - | + | + | + | + | - | - |
| Sutanto et al., 2022 [26] | - | - | - | - | + | + | - | + | - | - | + | + | + | + | N/A | + |
| Mapinduzi et al., 2021 [27] | + | Partially yes | + | - | + | + | + | + | + | - | + | + | + | + | - | + |
| Kechichian et al., 2022 [28] | - | - | - | - | + | - | - | + | - | - | + | + | + | + | + | + |
| Zhang et al., 2022 [29] | + | - | + | - | - | - | + | + | - | + | + | + | + | + | - | - |
| Arcanjo et al., 2020 [30] | - | - | - | - | + | + | - | - | - | - | - | - | - | - | + | - |
| Pocovi et al., 2022 [31] | + | Partially yes | - | - | + | + | + | + | - | - | - | - | - | + | + | + |
| Rathnayake et al., 2021 [32] | - | - | + | Partially yes | + | + | + | Partially yes | - | - | - | - | + | - | - | - |
| Dal Farra et al., 2021 [33] | + | + | + | + | + | - | - | + | Partially yes | - | + | + | + | + | - | + |
| Hayden et al., 2021 (a) [34] | + | Partially yes | + | Partially yes | + | + | + | + | Partially yes | - | + | + | + | + | + | + |
| Hayden et al., 2021 (a) [35] | + | Partially yes | + | Partially yes | - | - | - | + | Partially yes | + | + | - | + | + | + | + |
| Quentin et al., 2021 [36] | + | Partially yes | + | Partially yes | + | + | - | Partially yes | Partially yes | - | + | + | + | + | + | + |
| Gao et al., 2021 [37] | + | + | + | Partially yes | + | + | + | + | Partially yes | + | + | + | + | + | + | + |
| Chen et al., 2021 [38] | + | - | + | Partially yes | + | + | Partially yes | + | + | + | + | - | - | + | - | + |
| Zhang et al., 2021 [39] | + | Partially yes | + | Partially yes | + | + | Partially yes | Partially yes | + | - | + | + | - | + | + | + |
| Sun et al., 2021 [40] | + | Partially yes | + | Partially yes | + | + | Partially yes | Partially yes | + | - | + | + | + | + | + | + |
| Ouellet et al., 2021 [41] | + | Partially yes | + | Partially yes | + | + | - | + | - | - | + | + | + | + | - | + |
| Thornton et al., 2021 [42] | + | Partially yes | + | Partially yes | + | + | Partially yes | Partially yes | Partially yes | - | + | + | + | + | - | + |
| Barros-Dos-Santos et al., 2021 [43] | + | Partially yes | + | Partially yes | + | + | Partially yes | Partially yes | Partially yes | - | - | + | + | - | + | + |
| Mueller et al., 2020 [44] | + | Partially yes | + | + | + | + | - | Partially yes | Partially yes | - | - | + | + | - | + | + |
| Hanel et al., 2020 [45] | + | Partially yes | + | + | + | + | - | Partially yes | Partially yes | - | - | + | + | - | + | + |
| Nduwimana et al., 2020 [46] | + | + | + | Partially yes | + | + | - | Partially yes | Partially yes | - | - | - | - | - | - | + |
| Zhu et al., 2020 [47] | + | Partially yes | + | Partially yes | N/A | + | - | Partially yes | + | - | + | + | + | + | + | + |
| Domingues-de-Freitas 2019 [48] | + | Partially yes | - | Partially yes | + | + | - | + | + | - | + | + | - | + | - | + |
| Casey et al., 2020 [49] | + | Partially yes | + | Partially yes | + | + | - | Partially yes | + | - | + | + | + | + | + | + |
| De-Jesus et al., 2020 [50] | + | Partially yes | - | Partially yes | + | + | - | Partially yes | Partially yes | - | - | - | + | - | + | + |
| Amaral et al., 2020 [51] | + | Partially yes | + | Partially yes | + | + | - | + | Partially yes | - | + | + | + | + | - | + |
| Wood et al., 2021 [52] | + | Partially yes | + | Partially yes | + | + | - | + | + | - | + | + | + | + | + | + |
| Bernard et al., 2020 [53] | + | Partially yes | + | Partially yes | + | + | - | + | + | + | - | + | + | - | - | + |
| Niederer and Muller, 2020 [54] | + | Partially yes | + | Partially yes | + | + | - | Partially yes | Partially yes | - | + | + | + | + | + | + |
| Hayden et al., 2019 [55] | + | Partially yes | + | - | - | - | - | + | - | - | + | - | + | + | - | + |
| Huang et al., 2018 [56] | + | Partially yes | + | Partially yes | + | + | - | Partially yes | Partially yes | - | + | + | - | - | - | + |
| Owen et al., 2019 [57] | + | Partially yes | + | Partially yes | + | + | - | + | + | - | - | + | + | + | - | + |
| Alzahrani et al., 2020 [58] | + | Partially yes | - | Partially yes | + | + | - | Partially yes | - | - | + | - | + | - | - | + |
| Zhang et al., 2019 (a) [59] | + | - | - | Partially yes | - | + | - | Partially yes | + | - | + | - | - | + | + | + |
| Dong et al., 2019 [60] | + | Partially yes | - | Partially yes | + | + | - | + | + | - | + | - | + | + | + | - |
| Li et al., 2019 [61] | + | + | - | + | + | + | - | Partially yes | + | - | - | + | + | - | + | + |
| Alayat et al., 2019 [62] | + | + | - | + | + | - | - | + | + | - | + | + | + | + | + | + |
| Alzahrani et al., 2019 [63] | + | + | - | Partially yes | + | + | - | + | + | - | + | + | + | + | + | + |
| Pourahmadi et al., 2019 [64] | + | + | - | Partially yes | + | + | - | + | + | - | + | - | + | + | + | + |
| Nascimento et al., 2019 [65] | + | + | + | Partially yes | + | - | - | + | + | - | + | + | + | + | - | + |
| Bernet et al., 2019 [66] | + | + | - | Partially yes | + | + | - | + | Partially yes | - | - | + | + | + | - | + |
| Davenport et al., 2019 [67] | + | + | - | Partially yes | + | - | Partially yes | Partially yes | - | - | + | + | - | + | + | + |
| Zhang et al., 2019 (b) [68] | + | Partially yes | - | Partially yes | + | + | - | + | Partially yes | - | + | + | + | + | - | + |
| Zheng et al., 2018 [69] | + | + | - | Partially yes | + | + | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | + |
| Wewege et al., 2019 [70] | + | Partially yes | - | Partially yes | + | + | - | Partially yes | Partially yes | - | + | - | - | + | + | + |
| Miyamoto et al., 2019 [71] | + | + | + | Partially yes | + | + | + | + | + | + | + | + | + | + | + | - |
| Luomajoki et al., 2018 [72] | + | + | + | Partially yes | + | + | + | + | + | + | + | + | + | + | + | - |
| Lam et al., 2018 [73] | + | + | + | Partially yes | + | + | - | + | + | - | + | + | + | + | + | + |
| Coulter et al., 2018 [74] | + | + | + | Partially yes | + | + | - | Partially yes | + | - | + | + | + | + | - | - |
| Sitthipornvorakul et al., 2018 [75] | + | + | + | + | + | + | + | + | Partially yes | - | + | + | + | + | - | - |
| Vanti et al., 2019 [76] | + | + | + | + | + | + | + | + | Partially yes | - | + | + | + | + | - | - |
| Shiri et al., 2018 (a) [77] | + | + | + | + | + | + | + | + | + | - | + | + | + | + | - | + |
| Shiri et al., 2018 (b) [78] | + | + | + | + | + | + | + | + | Partially yes | - | + | + | + | + | - | - |
| Shi et al., 2018 [79] | + | + | + | + | + | + | + | + | Partially yes | - | + | + | + | + | - | + |
| Basson et al., 2017 [80] | + | + | + | + | + | + | + | + | + | - | + | + | + | + | - | - |
| Shiri and Falah-Hassani, 2017 [81] | + | + | + | + | + | + | + | + | + | - | + | + | + | + | - | + |
| Geneen et al., 2017 [82] | + | + | + | + | + | + | + | + | Partially yes | - | + | + | + | + | - | - |
| Nicolson et al., 2017 [83] | + | Partially yes | + | + | + | + | - | - | + | + | + | + | + | - | - | - |
| Wieland et al., 2013 [84] | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + |
| Coulombe et al., 2017 [85] | + | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - |
| Gomes-Neto et al., 2017 [86] | + | Partially yes | + | Partially yes | + | + | - | Partially yes | - | - | + | - | - | + | - | + |
| Moreira-Silva et al., 2016 [87] | + | Partially yes | + | Partially yes | + | - | - | Partially yes | + | + | + | + | - | - | - | + |
| Oliveira et al., 2016 [88] | + | + | + | Partially yes | + | + | + | + | Partially yes | - | + | + | - | + | - | + |
| Peek and Stevens, 2016 [89] | + | - | - | Partially yes | - | - | - | - | - | - | + | - | - | - | - | + |
| Yamato et al., 2015 [90] | + | Partially yes | - | Partially yes | + | + | + | + | + | + | + | - | - | + | - | + |
| Searle et al., 2015 [91] | + | Partially yes | - | Partially yes | + | - | - | - | - | - | + | - | - | + | - | + |
| Meng and Yue, 2015 [92] | + | - | - | Partially yes | - | + | - | - | - | - | + | - | - | + | + | + |
| Byström et al., 2013 [93] | + | - | + | Partially yes | + | - | - | + | - | - | + | - | - | - | - | + |
| Bell et al., 2009 [94] | + | - | - | Partially yes | - | - | - | Partially yes | - | - | + | - | - | - | - | + |
| No | Article | Exercise Type | Effect Size Magnitude | Study Quality |
|---|---|---|---|---|
| 1 | Zhang et al., 2023 [7] | Strengthening, Aerobic, Mind–body, Stretching and flexibility | High | Low |
| 2 | Ferraz et al., 2023 [8] | Mind–body, Stretching and flexibility | Moderate | Low |
| 3 | Gilanyi et al., 2023 [9] | Strengthening, Aerobic, Mind–body, Stretching and flexibility | Small | Low |
| 4 | Heidari et al., 2023 [11] | Aquatic | Small | Low |
| 5 | Yu et al., 2023 [12] | Mind–body, Motor control, Multimodal, Direction-specific | High | Low |
| 6 | Syroyid et al., 2023 [13] | Strengthening | Small | Low |
| 7 | Ram et al., 2023 [14] | Multimodal | Not significant | Critically low |
| 8 | Prat-Luri et al., 2023 [15] | Trunk-focused exercise | Small | High |
| 9 | Gilliam et al., 2023 [16] | Mind–body | High | Critically low |
| 10 | Hernandez-Lucas et al., 2022 [17] | Strengthening, Mind–body, Stretching and flexibility | Moderate | Critically low |
| 11 | Kazeminia et al., 2023 [18] | Strengthening | High | Critically low |
| 12 | Santos et al., 2023 [19] | Muscle energy technique | Small | Moderate |
| 13 | Belavy et al., 2022 [20] | Strengthening, Aerobic, Motor control, Stretching and flexibility | Small | Critically low |
| 14 | Shanbehzadeh et al., 2022 [23] | Motor control | High | Moderate |
| 15 | Dimitrijevic et al., 2022 [25] | Strengthening, Stretching and flexibility | Moderate | Low |
| 16 | Kechichian et al., 2022 [28] | Strengthening, Aerobic, Motor control, Stretching and flexibility | Moderate | Critically low |
| 17 | Zhang et al., 2022 [29] | Strengthening, Aerobic, Mind–body, Motor control | Small | Critically low |
| 18 | Arcanjo et al., 2022 [30] | Neuromuscular exercise | High | Critically low |
| 19 | Pocovi et al., 2022 [31] | Aerobic | High | Critically low |
| 20 | Rathnayake et al., 2021 [32] | Strengthening, Aerobic, Stretching and flexibility | Small | Critically low |
| 21 | Dal Farra et al., 2022 [33] | Mind–body, Motor control | Small | Critically low |
| 22 | Hayden et al., 2021 (a) [34] | Strengthening, Aerobic, Mind–body, Stretching and flexibility, Multimodal, Direction-specific | Moderate | High |
| 23 | Quentin et al., 2021 [36] | Strengthening, Aerobic, Mind–body, Motor control | High | Low |
| 24 | Gao et al., 2022 [37] | Motor control, Neuromuscular exercise | High | High |
| 25 | Chen et al., 2021 [38] | Myofascial release | Small | Critically low |
| 26 | Zhang et al., 2021 [39] | Motor control | High | Low |
| 27 | Barros-Dos-Santos et al., 2021 [43] | Aerobic, Mind–body, Motor control | High | Low |
| 28 | Mueller and Niederer, 2020 [44] | Mind–body, Motor control | High | Critically low |
| 29 | Hanel et al., 2020 [45] | Strengthening, Aerobic, Mind–body, Motor control, Stretching and flexibility, Multimodal | Small | Critically low |
| 30 | Zhu et al., 2020 [47] | Mind–body | High | Low |
| 31 | Domingues-De-Freitas et al., 2020 [48] | Mind–body | Small | Critically low |
| 32 | De-Jesus et al., 2020 [50] | Strengthening | Small | Critically low |
| 33 | Amaral et al., 2020 [51] | Strengthening, Aerobic | Moderate | Critically low |
| 34 | Bernard et al., 2021 [53] | Multimodal | Small | Critically low |
| 35 | Niederer and Mueller, 2020 [54] | Motor control | Small | Low |
| 36 | Hayden et al., 2020 [55] | Strengthening, Aerobic, Mind–body, Stretching and flexibility, Direction-specific | Moderate | Critically low |
| 37 | Huang et al., 2020 [56] | Aerobic, Mind–body, Motor control, Stretching and flexibility | Moderate | Critically low |
| 38 | Alzahrani et al., 2019 (a) [58] | Aerobic, Multimodal | Small | Critically low |
| 39 | Zhang et al., 2019 (a) [59] | Strengthening, Aerobic, Multimodal | Small | Critically low |
| 40 | Dong et al., 2019 [60] | Whole-body vibration | Moderate | Low |
| 41 | Alayat et al., 2019 [62] | High-intensity laser therapy | High | Low |
| 42 | Alzahrani et al., 2019 (b) [63] | Incidental physical activity | Not significant | Low |
| 43 | Pourahmadi et al., 2019 [64] | Stretching and flexibility | High | Low |
| 44 | Nascimento et al., 2019 [65] | Mind–body | Not significant | Critically low |
| 45 | Davenport et al., 2019 [67] | Strengthening, Aerobic, Mind–body | High | Critically low |
| 46 | Zhang et al., 2019 (b) [68] | Mind–body | Moderate | Critically low |
| 47 | Wewege et al., 2018 [70] | Strengthening, Aerobic | Small | Critically low |
| 48 | Miyamoto et al., 2019 [71] | Strengthening, Aerobic, Motor control, Stretching and flexibility, Multimodal | (Cost effectiveness is considered) | High |
| 49 | Luomajoki et al., 2018 [72] | Motor control | Small | High |
| 50 | Lam et al., 2018 [73] | Direction-specific | Moderate | Low |
| 51 | Coulter et al., 2018 [74] | Stretching and flexibility | Small | Critically low |
| 52 | Shiri et al., 2018 (a) [77] | Strengthening, Aerobic, Mind–body, Motor control, Stretching and flexibility | Moderate | Low |
| 53 | Shiri et al., 2018 (b) [78] | Strengthening, Aerobic, Motor control, Multimodal | Small | Low |
| 54 | Shi et al., 2018 [79] | Aquatic | Moderate | Low |
| 55 | Basson et al., 2017 [80] | Neural mobilization | Small | Low |
| 56 | Shiri and Falah-Hassani, 2017 [81] | Multimodal | Small | Low |
| 57 | Geneen et al., 2017 [82] | Strengthening, Aerobic, Mind–body, Stretching and flexibility | No meta-analysis | Low |
| 58 | Nicolson et al., 2017 [83] | Strengthening, Aerobic, Motor control | Small | Critically low |
| 59 | Wieland et al., 2013 [84] | Mind–body | Small | High |
| 60 | Coulombe et al., 2017 [85] | Strengthening, Multimodal | Small | Critically low |
| 61 | Moreira-Silva et al., 2016 [87] | Strengthening, Aerobic, Stretching and flexibility | Small | Critically low |
| 62 | Oliveira et al., 2016 [88] | Strengthening, Aerobic, Stretching and flexibility | Small | Critically low |
| 63 | Yamato et al., 2015 [90] | Mind–body, Motor control | Small | Critically low |
| 64 | Searle et al., 2015 [91] | Strengthening, Aerobic, Stretching and flexibility | Small | Critically low |
| 65 | Meng and Yue, 2015 [92] | Strengthening, Aerobic | Small | Critically low |
| 66 | Byström et al., 2013 [93] | Strengthening, Motor control, Stretching and flexibility, Multimodal | Small | Critically low |
| 67 | Bell and Burnett, 2009 [94] | Strengthening, Motor control, Stretching and flexibility | No meta-analysis | Critically low |
| 68 | Thornton et al., 2021 [42] | Strengthening, Aerobic, Mind–body | Small | Low |
| 69 | Bernet et al., 2019 [66] | Strengthening, Mind–body | Not significant | Critically low |
| 70 | Zheng et al., 2018 [69] | Whole-body vibration | Not reported | High |
| 71 | Sitthipornvorakul et al., 2018 [75] | Aerobic | Moderate | Low |
| 72 | Vanti et al., 2019 [76] | Strengthening, Aerobic, Stretching and flexibility, Multimodal | Not significant | Low |
| 73 | Peek and Stevens, 2016 [89] | Strengthening, Mind–body, Motor control | Not reported | Critically low |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Viderman, D.; Kalikanov, S.; Myrkhiyeva, Z.; Alisherov, S.; Dossov, M.; Seitenov, S.; Abdildin, Y. Impact of Exercise Therapy on Outcomes in Patients with Low Back Pain: An Umbrella Review of Systematic Reviews. J. Clin. Med. 2025, 14, 5942. https://doi.org/10.3390/jcm14175942
Viderman D, Kalikanov S, Myrkhiyeva Z, Alisherov S, Dossov M, Seitenov S, Abdildin Y. Impact of Exercise Therapy on Outcomes in Patients with Low Back Pain: An Umbrella Review of Systematic Reviews. Journal of Clinical Medicine. 2025; 14(17):5942. https://doi.org/10.3390/jcm14175942
Chicago/Turabian StyleViderman, Dmitriy, Sultan Kalikanov, Zhuldyz Myrkhiyeva, Shakhrizat Alisherov, Mukhit Dossov, Serik Seitenov, and Yerkin Abdildin. 2025. "Impact of Exercise Therapy on Outcomes in Patients with Low Back Pain: An Umbrella Review of Systematic Reviews" Journal of Clinical Medicine 14, no. 17: 5942. https://doi.org/10.3390/jcm14175942
APA StyleViderman, D., Kalikanov, S., Myrkhiyeva, Z., Alisherov, S., Dossov, M., Seitenov, S., & Abdildin, Y. (2025). Impact of Exercise Therapy on Outcomes in Patients with Low Back Pain: An Umbrella Review of Systematic Reviews. Journal of Clinical Medicine, 14(17), 5942. https://doi.org/10.3390/jcm14175942







