Impact of Molar Teeth Distalization by Clear Aligners on the Temporomandibular Joint: Systematic Review and Meta-Analysis
Abstract
1. Introduction
1.1. Rationale
1.2. Objectives
2. Materials and Methods
2.1. Eligibility Criteria
2.2. Search Strategy
2.3. Information Sources
2.4. Selection Process
2.5. Data Collection Process
2.6. Data Items
2.7. Study Risk of Bias Assessment
2.8. Effect Measures
2.9. Synthesis Methods
2.10. Registration
3. Results
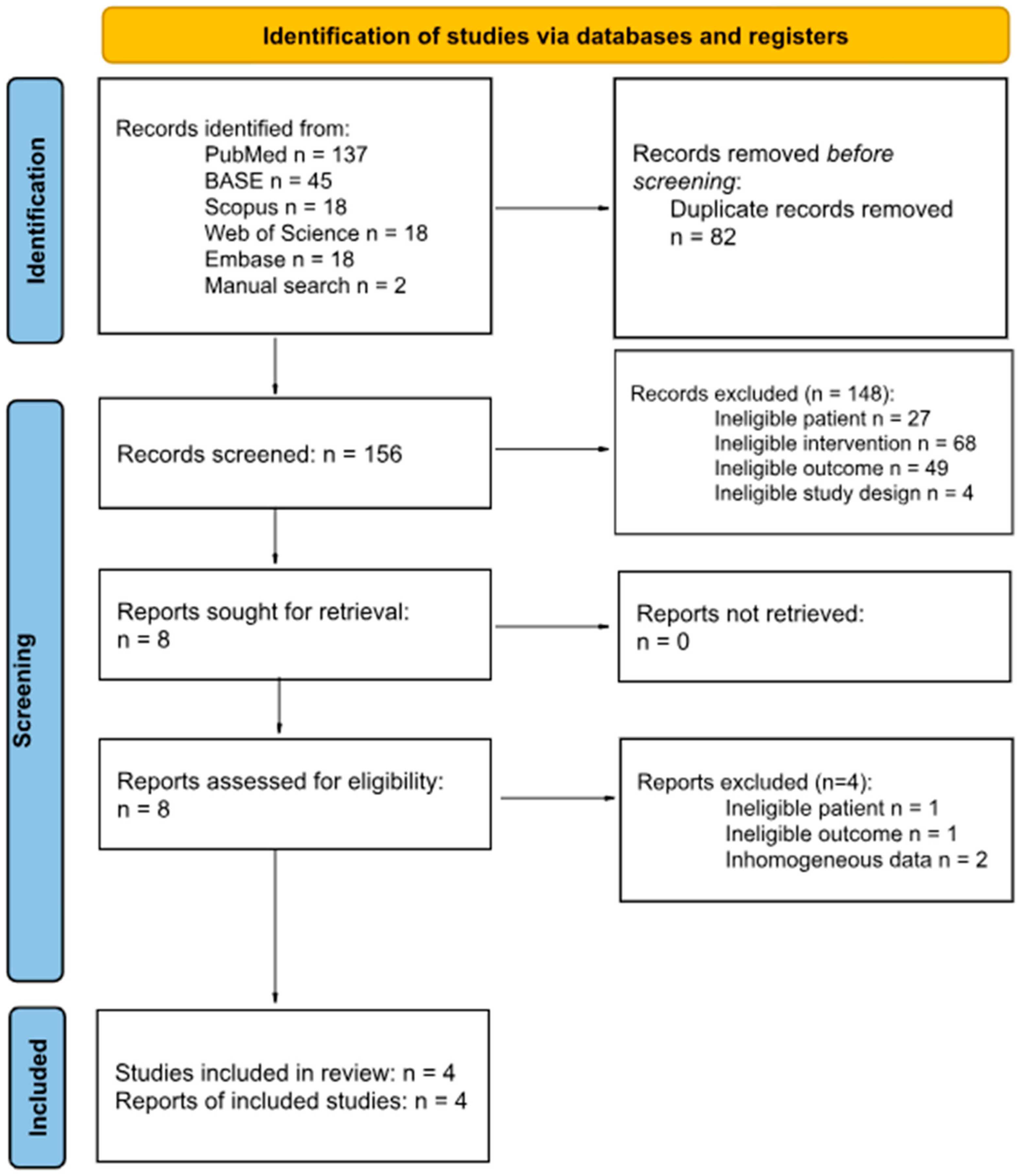
3.1. Study Selection
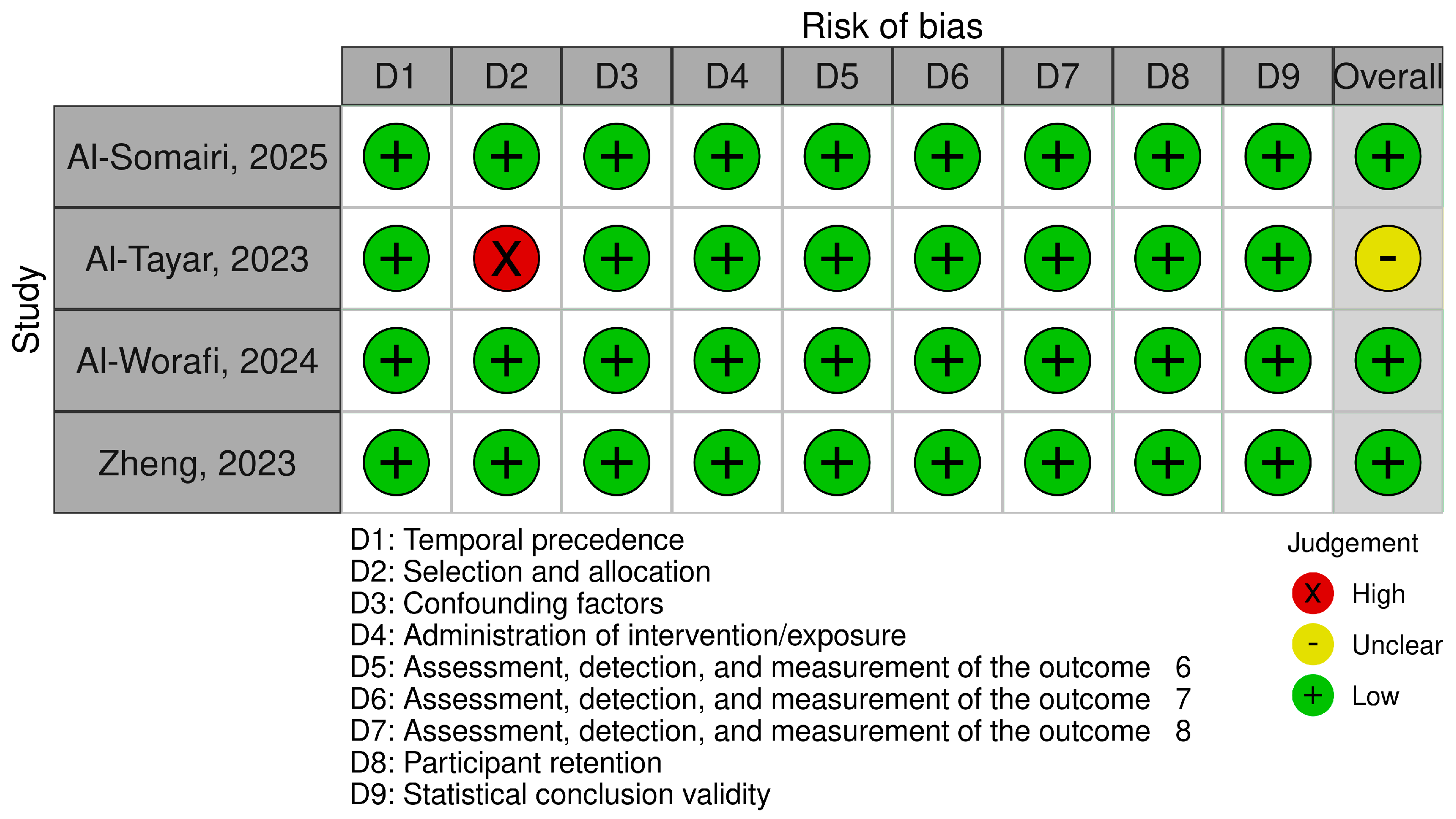
3.2. Risk of Bias in Studies
3.3. Results of Individual Studies
3.4. Results of Syntheses
3.5. Reporting Biases
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| AJS | Anterior Joint Space |
| CAs | Clear Aligners |
| CBCT | Cone Beam Computed Tomography |
| CL | Condylar Length |
| CW | Condylar Width |
| FAs | Fixed Appliances |
| MFH | Mandibular Fossa Height |
| MFW | Mandibular Fossa Width |
| MJS | Medial Joint Space |
| N/A | Not Applicable |
| PJS | Posterior Joint Space |
| SD | Standard Deviation |
| SJS | Superior Joint Space |
| TMDs | Temporomandibular Disorders |
| TMJ | Temporomandibular Joint |
Appendix A
| Engine | Scope, records |
|---|---|
| Embase | over 45,600,000 |
| Web of Science | over 235 million |
| BASE | 418.356.513 |
| PubMed | over 38 million |
| Scopus | over 100 million |
| First Author, Publication Year | Identifier | Reason for Exclusion |
|---|---|---|
| [65] | https://pubmed.ncbi.nlm.nih.gov/36643222/ (accessed on 16 April 2025) | Inhomogeneous data |
| [66] | https://www.sciencedirect.com/science/article/pii/S2666430524001055 (accessed on 16 April 2025) | Inhomogeneous data |
| [67] | https://bmcoralhealth.biomedcentral.com/articles/10.1186/s12903-022-02526-2 (accessed on 18 April 2025) | Outcome |
| [68] | https://repository.ucc.edu.co/entities/publication/64c941ba-d029-4157-a214-0ebf71612e20 (accessed on 18 April 2025) | Patient |
References
- Silva, R.G.; Kang, D.S. Prevalence of Malocclusion among Latino Adolescents. Am. J. Orthod. Dentofac. Orthop. 2001, 119, 313–315. [Google Scholar] [CrossRef] [PubMed]
- Lew, K.K.; Foong, W.C.; Loh, E. Malocclusion Prevalence in an Ethnic Chinese Population. Aust. Dent. J. 1993, 38, 442–449. [Google Scholar] [CrossRef]
- Benson, P.E.; Tinsley, D.; O’Dwyer, J.J.; Majumdar, A.; Doyle, P.; Sandler, P.J. Midpalatal Implants vs Headgear for Orthodontic Anchorage—A Randomized Clinical Trial: Cephalometric Results. Am. J. Orthod. Dentofac. Orthop. 2007, 132, 606–615. [Google Scholar] [CrossRef] [PubMed]
- Samoto, H.; Vlaskalic, V. A Customized Staging Procedure to Improve the Predictability of Space Closure with Sequential Aligners. J. Clin. Orthod. 2014, 48, 359–367. [Google Scholar] [PubMed]
- Al-Worafi, N.A.; Al-Nasri, A.; Al-Warafi, L.A.; Alsomairi, M.A.A.; Alyafrusee, E.S.; Alhashimi, N.; Zheng, B.; Liu, Y. Effect of Maxillary Molars Distalization Using Clear Aligners and Fixed Orthodontic Appliances on the Positional and Dimensional Temporomandibular Joint Parameters: A Three-Dimensional Comparative Study. BMC Oral Health 2024, 24, 1372. [Google Scholar] [CrossRef]
- Bowman, S.J.; Celenza, F.; Sparaga, J.; Papadopoulos, M.A.; Ojima, K.; Lin, J.C.-Y. Creative Adjuncts for Clear Aligners, Part 1: Class II Treatment. J. Clin. Orthod. 2015, 49, 83–94. [Google Scholar]
- Bussick, T.J.; McNamara, J.A. Dentoalveolar and Skeletal Changes Associated with the Pendulum Appliance. Am. J. Orthod. Dentofac. Orthop. 2000, 117, 333–343. [Google Scholar] [CrossRef]
- Kesling, H.D. Coordinating the Predetermined Pattern and Tooth Positioner with Conventional Treatment. Am. J. Orthod. Oral Surg. 1946, 32, 285–293. [Google Scholar] [CrossRef]
- AlMogbel, A. Clear Aligner Therapy: Up to Date Review Article. J. Orthod. Sci. 2023, 12, 37. [Google Scholar] [CrossRef]
- Lou, T.; Mair, A. An Historical Overview of Clear Aligner Therapy the Evolution of Clear Aligners. Oral Health Group. 14 September 2020. Available online: https://www.oralhealthgroup.com/features/an-historical-overview-of-clear-aligner-therapy-the-evolution-of-clear-aligners/ (accessed on 14 June 2025).
- Rossini, G.; Parrini, S.; Castroflorio, T.; Deregibus, A.; Debernardi, C.L. Efficacy of Clear Aligners in Controlling Orthodontic Tooth Movement: A Systematic Review. Angle Orthod. 2015, 85, 881–889. [Google Scholar] [CrossRef]
- Timm, L.H.; Farrag, G.; Baxmann, M.; Schwendicke, F. Factors Influencing Patient Compliance during Clear Aligner Therapy: A Retrospective Cohort Study. JCM 2021, 10, 3103. [Google Scholar] [CrossRef]
- Al-Nadawi, M.; Kravitz, N.D.; Hansa, I.; Makki, L.; Ferguson, D.J.; Vaid, N.R. Effect of Clear Aligner Wear Protocol on the Efficacy of Tooth Movement. Angle Orthod. 2021, 91, 157–163. [Google Scholar] [CrossRef]
- Weir, T. Clear Aligners in Orthodontic Treatment. Aust. Dent. J. 2017, 62, 58–62. [Google Scholar] [CrossRef] [PubMed]
- Melkos, A.B. Advances in Digital Technology and Orthodontics: A Reference to the Invisalign Method. Med. Sci. Monit. 2005, 11, PI39–PI42. [Google Scholar] [PubMed]
- Graber, L.W.; Vanarsdall, R.L.; Vig, K.W.L. Clear Aligner Treatment. In Orthodontics: Current Principles and Techniques; Mosby: St. Louis, MO, USA, 2011; pp. 778–811. [Google Scholar]
- Cardoso, P.C.; Espinosa, D.G.; Mecenas, P.; Flores-Mir, C.; Normando, D. Pain Level between Clear Aligners and Fixed Appliances: A Systematic Review. Prog. Orthod. 2020, 21, 3. [Google Scholar] [CrossRef] [PubMed]
- Yassir, Y.A.; Nabbat, S.A.; McIntyre, G.T.; Bearn, D.R. Clinical Effectiveness of Clear Aligner Treatment Compared to Fixed Appliance Treatment: An Overview of Systematic Reviews. Clin. Oral Investig. 2022, 26, 2353–2370. [Google Scholar] [CrossRef]
- Grünheid, T.; Tasca, A.W.; Kanyusik, J.S.; Walters, S.-A.; Larson, B.E. Assessment of Orthodontic Treatment Efficacy of Clarity Aligners Using the Peer Assessment Rating Index and the American Board of Orthodontics Cast-Radiograph Evaluation. Am. J. Orthod. Dentofac. Orthop. 2022, 162, 861–869. [Google Scholar] [CrossRef]
- Maspero, C.; Tartaglia, G.M. 3D Printing of Clear Orthodontic Aligners: Where We Are and Where We Are Going. Materials 2020, 13, 5204. [Google Scholar] [CrossRef]
- Venezia, P.; Ronsivalle, V.; Rustico, L.; Barbato, E.; Leonardi, R.; Lo Giudice, A. Accuracy of Orthodontic Models Prototyped for Clear Aligners Therapy: A 3D Imaging Analysis Comparing Different Market Segments 3D Printing Protocols. J. Dent. 2022, 124, 104212. [Google Scholar] [CrossRef]
- Zheng, J.; Zhang, Y.; Wu, Q.; Xiao, H.; Li, F. Three-Dimensional Spatial Analysis of the Temporomandibular Joint in Adult Patients with Class II Division 2 Malocclusion before and after Orthodontic Treatment: A Retrospective Study. BMC Oral Health 2023, 23, 477. [Google Scholar] [CrossRef] [PubMed]
- Al-Somairi, M.A.A.; Zheng, B.; Yang, X.; Zhang, Y.; Alhammadi, M.S.; Xu, H.; Alhashimi, N.; Almaqrami, B.S.; Al-Worafi, N.A.; Alyafrusee, E.S.; et al. Three-Dimensional Quantitative Temporomandibular Joint Changes in Skeletal Class I Malocclusion Treated with Extraction and Non-Extraction Protocols: A Comparative Study of Fixed Orthodontic Appliances and Clear Aligners. Prog. Orthod. 2025, 26, 4. [Google Scholar] [CrossRef] [PubMed]
- Simon, M.; Keilig, L.; Schwarze, J.; Jung, B.A.; Bourauel, C. Treatment Outcome and Efficacy of an Aligner Technique—Regarding Incisor Torque, Premolar Derotation and Molar Distalization. BMC Oral Health 2014, 14, 68. [Google Scholar] [CrossRef] [PubMed]
- da Costa Grec, R.H.; Janson, G.; Branco, N.C.; Moura-Grec, P.G.; Patel, M.P.; Castanha Henriques, J.F. Intraoral Distalizer Effects with Conventional and Skeletal Anchorage: A Meta-Analysis. Am. J. Orthod. Dentofac. Orthop. 2013, 143, 602–615. [Google Scholar] [CrossRef]
- Fuziy, A.; de Almeida, R.R.; Janson, G.; Angelieri, F.; Pinzan, A. Sagittal, Vertical, and Transverse Changes Consequent to Maxillary Molar Distalization with the Pendulum Appliance. Am. J. Orthod. Dentofac. Orthop. 2006, 130, 502–510. [Google Scholar] [CrossRef]
- Fontana, M.; Cozzani, M.; Caprioglio, A. Non-Compliance Maxillary Molar Distalizing Appliances: An Overview of the Last Decade. Prog. Orthod. 2012, 13, 173–184. [Google Scholar] [CrossRef]
- Giancotti, A.; Farina, A. Treatment of Collapsed Arches Using the Invisalign System. J. Clin. Orthod. 2010, 44, 416–425. [Google Scholar]
- Paquette, D. Chapter 22—Extraction Treatment with Invisalign. In The Invisalign System; Quintessence Publishing Co.: Berlin, Germany, 2006; pp. 195–205. [Google Scholar]
- Coronel-Zubiate, F.; Marroquín-Soto, C.; Geraldo-Campos, L.; Aguirre-Ipenza, R.; Urbano-Rosales, L.; Luján-Valencia, S.; Tozo-Burgos, J.; Arbildo-Vega, H. Association between Orthodontic Treatment and the Occurrence of Temporomandibular Disorders: A Systematic Review and Meta-Analysis. J. Clin. Exp. Dent. 2022, 14, e1032–e1043. [Google Scholar] [CrossRef]
- Fernandez-Gonzalez, F.; Canigral, A.; Lopez-Caballo, J.; Brizuela, A.; Moreno-Hay, I.; Del Rio-Highsmith, J.; Vega, J. Influence of Orthodontic Treatment on Temporomandibular Disorders. A Systematic Review. J. Clin. Exp. Dent. 2015, 7, e320–e327. [Google Scholar] [CrossRef]
- Pattanaik, S.; Veeraraghavan, V.P.; Dasari, A.K.; Sahoo, S.N.; Aileni, K.R.; Suryawanshi, H.; Patil, S.R. Exploring the Association between Orthodontic Treatment and Temporomandibular Disorders in Pediatric Patient: A Retrospective Study. J. Orthod. Sci. 2024, 13, 38. [Google Scholar] [CrossRef]
- Almashraqi, A.A.; Sayed, B.A.; Mokli, L.K.; Jaafari, S.A.; Halboub, E.; Parveen, S.; Al-Ak’hali, M.S.; Alhammadi, M.S. Recommendations for Standard Criteria for the Positional and Morphological Evaluation of Temporomandibular Joint Osseous Structures Using Cone-Beam CT: A Systematic Review. Eur. Radiol. 2024, 34, 3126–3140. [Google Scholar] [CrossRef] [PubMed]
- Hodges, R.J.; Atchison, K.A.; White, S.C. Impact of Cone-Beam Computed Tomography on Orthodontic Diagnosis and Treatment Planning. Am. J. Orthod. Dentofac. Orthop. 2013, 143, 665–674. [Google Scholar] [CrossRef] [PubMed]
- Pullinger, A. Establishing Better Biological Models to Understand Occlusion. I: TM Joint Anatomic Relationships. J. Oral Rehabil. 2013, 40, 296–318. [Google Scholar] [CrossRef]
- Al-Tayar, B.; Al-Somairi, M.A.A.; ALshoaibi, L.H.; Wang, X.; Wang, J.; Liu, J.; Al-Tayar, B.; An, X.; Si, Q. Impact of Molar Teeth Distalization by Clear Aligners on Temporomandibular Joint: A Three-Dimensional Study. Prog. Orthod. 2023, 24, 25. [Google Scholar] [CrossRef]
- JBI Critical Appraisal Tools|JBI. Available online: https://jbi.global/critical-appraisal-tools (accessed on 14 June 2025).
- Risk of Bias Tools—Robvis (Visualization Tool). Available online: https://www.riskofbias.info/welcome/robvis-visualization-tool (accessed on 10 August 2025).
- Almalki, S.A.; Al Jameel, A.H.; Gowdar, I.M.; Langaliya, A.; Vaddamanu, S.K.; Di Blasio, M.; Cervino, G.; Minervini, G. Impact of Clear Aligner Therapy on Masticatory Musculature and Stomatognathic System: A Systematic Review Conducted According to PRISMA Guidelines and the Cochrane Handbook for Systematic Reviews of Interventions. BMC Oral Health 2024, 24, 350. [Google Scholar] [CrossRef]
- Hiyama, S.; Ono, P.T.; Ishiwata, Y.; Kuroda, T.; McNamara, J.A. Neuromuscular and Skeletal Adaptations Following Mandibular Forward Positioning Induced by the Herbst Appliance. Angle Orthod. 2000, 70, 442–453. [Google Scholar]
- Ponces, M.J.; Tavares, J.P.; Lopes, J.D.; Ferreira, A.P. Comparison of Condylar Displacement between Three Biotypological Facial Groups by Using Mounted Models and a Mandibular Position Indicator. Korean J. Orthod. 2014, 44, 312. [Google Scholar] [CrossRef]
- Charalampakis, O.; Iliadi, A.; Ueno, H.; Oliver, D.R.; Kim, K.B. Accuracy of Clear Aligners: A Retrospective Study of Patients Who Needed Refinement. Am. J. Orthod. Dentofac. Orthop. 2018, 154, 47–54. [Google Scholar] [CrossRef]
- Halapanavar, B.; Padmini, M.N.; Deshmukh, S.; Tirupathi, S.; Waremani, A.S.; Kasodekar, A. Comparison of Skeletal Changes in the Temporomandibular Joint between the Twin Block Appliance and Fixed Functional Appliance: A Longitudinal Follow-up Study. Int. J. Clin. Pediatr. Dent. 2024, 17, 7–14. [Google Scholar] [CrossRef]
- Parvathy, R.M.; Shetty, S.; Katheesa, P. Evaluation of Changes Seen in TMJ after Mandibular Advancement in Treatment of Class II Malocclusions, with Functional Appliances, a CBCT Study. Biomedicine 2021, 41, 236–242. [Google Scholar] [CrossRef]
- Bhoir, N.; Sabharwal, K.; Gadhiya, N.D.; Narkhede, S.; Shetty, K. Class II Malocclusion—Mini Plate Assisted Non-Extraction Treatment Approach. J. Contemp. Orthod. 2022, 6, 192–195. [Google Scholar] [CrossRef]
- Tehranchi, A.; Behnia, H.; Younessian, F.; Hadadpour, S. Advances in Management of Class II Malocclusions. In A Textbook of Advanced Oral and Maxillofacial Surgery; Motamedi, M.H.K., Ed.; InTech: London, UK, 2016; Volume 3, ISBN 978-953-51-2590-7. [Google Scholar]
- Pacha, M.M.; Fleming, P.S.; Johal, A. Complications, Impacts, and Success Rates of Different Approaches to Treatment of Class II Malocclusion in Adolescents: A Systematic Review and Meta-Analysis. Am. J. Orthod. Dentofac. Orthop. 2020, 158, 477–494.e7. [Google Scholar] [CrossRef] [PubMed]
- Abo Samra, D.; Hadad, R.; Hamadah, O. Effect of Molar Distalization on Condyle-Glenoid Fossa Relationship. BioMed Res. Int. 2023, 2023, 5549951. [Google Scholar] [CrossRef] [PubMed]
- Alhammadi, M.S.; Fayed, M.S.; Labib, A. Three-dimensional Assessment of Condylar Position and Joint Spaces after Maxillary First Premolar Extraction in Skeletal Class II Malocclusion. Orthod. Craniofac. Res. 2017, 20, 71–78. [Google Scholar] [CrossRef] [PubMed]
- Vogl, T.J.; Zyada, W.; Helal, R.; Naguib, N.N.; Lingwal, N.; Nour-Eldin, N.-E.A. Pre- and Post-Operative Cone Beam Computed Tomography Assessment of the Temporomandibular Joint in Patients with Orthognathic Surgery. Diagnostics 2024, 14, 1389. [Google Scholar] [CrossRef]
- Shpack, N.; Brosh, T.; Mazor, Y.; Shapinko, Y.; Davidovitch, M.; Sarig, R.; Reimann, S.; Bourauel, C.; Vardimon, A.D. Long- and Short-Term Effects of Headgear Traction with and without the Maxillary Second Molars. Am. J. Orthod. Dentofac. Orthop. 2014, 146, 467–476. [Google Scholar] [CrossRef]
- Barashi, M.A.; Habis, R.M.; Alhazmi, H.A. Predictability of Orthodontic Space Closure Using Invisalign Clear Aligners: A Retrospective Study. Cureus 2024, 16, e56706. [Google Scholar] [CrossRef]
- Ravera, S.; Castroflorio, T.; Garino, F.; Daher, S.; Cugliari, G.; Deregibus, A. Maxillary Molar Distalization with Aligners in Adult Patients: A Multicenter Retrospective Study. Prog. Orthod. 2016, 17, 12. [Google Scholar] [CrossRef]
- Cui, J.-Y.; Ting, L.; Cao, Y.-X.; Sun, D.-X.; Bing, L.; Wu, X.-P. Morphology Changes of Maxillary Molar Distalization by Clear Aligner Therapy. Int. J. Morphol. 2022, 40, 920–926. [Google Scholar] [CrossRef]
- Chiu, P.P.; McNamara, J.A.; Franchi, L. A Comparison of Two Intraoral Molar Distalization Appliances: Distal Jet versus Pendulum. Am. J. Orthod. Dentofac. Orthop. 2005, 128, 353–365. [Google Scholar] [CrossRef]
- Ngantung, V.; Nanda, R.S.; Bowman, S.J. Posttreatment Evaluation of the Distal Jet Appliance. Am. J. Orthod. Dentofac. Orthop. 2001, 120, 178–185. [Google Scholar] [CrossRef]
- Brickman, C.D.; Sinha, P.K.; Nanda, R.S. Evaluation of the Jones Jig Appliance for Distal Molar Movement. Am. J. Orthod. Dentofac. Orthop. 2000, 118, 526–534. [Google Scholar] [CrossRef]
- El Guennouni, B.; El haddaoui, R.; Zaoui, F.; Chatuan, M.; Benyahia, H. Vertical Effects of Maxillary Molar Distalization with Clear Aligners in Class II Patients: A Systematic Review. Digit. Dent. J. 2025, 1, 100011. [Google Scholar] [CrossRef]
- Ângelo, D.F.; Faria-Teixeira, M.C.; Maffia, F.; Sanz, D.; Sarkis, M.; Marques, R.; Mota, B.; João, R.S.; Cardoso, H.J. Association of Malocclusion with Temporomandibular Disorders: A Cross-Sectional Study. JCM 2024, 13, 4909. [Google Scholar] [CrossRef] [PubMed]
- Manfredini, D.; Segù, M.; Arveda, N.; Lombardo, L.; Siciliani, G.; Rossi, A.; Guarda-Nardini, L. Temporomandibular Joint Disorders in Patients with Different Facial Morphology. A Systematic Review of the Literature. J. Oral. Maxillofac. Surg. 2016, 74, 29–46. [Google Scholar] [CrossRef]
- Yu, W.; Jeon, H.H.; Kim, S.; Dayo, A.; Mupparapu, M.; Boucher, N.S. Correlation between TMJ Space Alteration and Disc Displacement: A Retrospective CBCT and MRI Study. Diagnostics 2023, 14, 44. [Google Scholar] [CrossRef] [PubMed]
- Sharab, L.; Shafi, A.; Butul, B.; Okeson, J.P. Clear Aligner Therapy and Symptoms of Temporomandibular Disorders: A Case Report. Gen. Dent. 2024, 72, 47–52. [Google Scholar]
- Lu, C. Evaluating Clear Aligners and Conventional Braces in Treating TMJ and Speech Impediment. J. Stud. Res. 2022, 11. [Google Scholar] [CrossRef]
- Zhao, Y.; Ge, Y.; Chen, W.; Chen, S.; Wang, Z. Upper Airway Hydrodynamics Changes after Molar Distalization with Aligners in Adult Patients. Clin. Oral Investig. 2024, 28, 630. [Google Scholar] [CrossRef]
- Lin, S.Y.; Hung, M.C.; Lu, L.H.; Sun, J.S.; Tsai, S.J.; Zwei-Chieng Chang, J. Treatment of class II malocclusion with Invisalign®: A pilot study using digital model-integrated maxillofacial cone beam computed tomography. J. Dent. Sci. 2023, 18, 353–366. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Wen, S.; Zhou, H.; Hong, H.; Nie, X.; Yuan, X.; Lai, W.; Long, H. Skeletal Class II malocclusion management with clear aligners and mini-implants. AJO-DO Clin. Companion 2025, 5, 56–69. [Google Scholar] [CrossRef]
- Liu, X.; Cheng, Y.; Qin, W.; Fang, S.; Wang, W.; Ma, Y.; Jin, Z. Effects of upper-molar distalization using clear aligners in combination with Class II elastics: A three-dimensional finite element analysis. BMC Oral Health 2022, 22, 546. [Google Scholar] [CrossRef]
- Aguirre Cifuentes, S.P.; Cubides Moreno, C.A. Análisis del Comportamiento Elástico del Propulsor Mandibular Advansync2® Mediante el Metodo de Elementos Finitos. Universidad Cooperativa de Colombia, Facultad de Odontología, Especialización en Ortodoncia, Bogotá. 2025. Available online: https://hdl.handle.net/20.500.12494/58063 (accessed on 14 June 2025).

| Inclusion Criteria | Exclusion Criteria | |
|---|---|---|
| Patient | Patient under orthodontic treatment | |
| Intervention | Distalization using clear aligners | Different types of appliances |
| Control | None | None |
| Outcome | CBCT measurement of changes | Lack of CT or MRI |
| Timeframe | No limit | Not applicable |
| Study design | Retrospective cohort study or case report or case series | Non-original/Non-English research, reviews, book chapters, or book fragments |
| Data Item | Description |
|---|---|
| MFH | The perpendicular line between the most superior central point of the fossa and the lowest point of the articular eminence and the posterior margin of the mandibular fossa. |
| MFW | The shortest distance between the most anteroinferior point of the mandibular fossa and the most posteroinferior point of the mandibular fossa. |
| CL | Distance between the most lateral and medial points of the condylar head. |
| CW | Distance between the most anterior and posterior points of the condylar head. |
| AJS | The shortest distance between the most anterior condyle point near the most Anterior Joint Space and the most posterior point of the anterior wall of the glenoid fossa. |
| PJS | The shortest distance between the most posterior condyle point near the Posterior Joint Space and the most anterior point of the posterior wall of fossa. |
| SJS | The shortest distance between the most superior central point of the condylar head and the most superior central point of the fossa. |
| MJS | The shortest distance between the most lateral point of the fossa and the innermost point of the condylar head. |
| Author Year | Temporal Precedence | Selection and Allocation | Confounding Factors | Administration of Intervention/Exposure | Assessment, Detection, and Measurement of the Outcome | Participant Retention | Statistical Conclusion Validity | Overall | ||
|---|---|---|---|---|---|---|---|---|---|---|
| Al-Somairi, 2025 [23] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Low risk |
| Al-Tayar, 2023 [36] | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Moderate risk |
| Al-Worafi, 2024 [5] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Low risk |
| Zheng, 2023 [22] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Low risk |
| Author | Number of Patients (M/F) | Patient’s Age | Imaging Type | Malocclusion Before Treatment | Time of Treatment | |
|---|---|---|---|---|---|---|
| Al-Somairi, 2025 [23] | 30 (13/17) | 24.27 | CBCT | Class I | Mean | 2.21 |
| SD | 0.74 | |||||
| Al-Tayar, 2023 [36] | 23 (7/16) | 29.8 | CBCT | Class I or II | Mean | 1.97 |
| SD | 0.6 | |||||
| Al-Worafi, 2024 [5] | 35 (N/S) | N/S | CBCT | Class II | Mean | 2.04 |
| SD | 0.59 | |||||
| Zheng, 2023 [22] | 22 (10/12) | 23.18 | CBCT | Class II division 2 | Mean | 1.9 |
| SD | 0.18 | |||||
| Author | Mandibular Fossa Dimension MFH (mm) | Mandibular Fossa Dimension MFW (mm) | Condylar Dimension CL (mm) | Condylar Dimension CW (mm) | |||||
|---|---|---|---|---|---|---|---|---|---|
| Before | After | Before | After | Before | After | Before | After | ||
| Al-Somairi, 2025 [23] | Mean | 11.67 | 11.56 | 17.47 | 17.51 | 19.09 | 19.15 | 8.05 | 8.17 |
| SD | 1.44 | 2.64 | 1.67 | 1.63 | 1.52 | 1.47 | 0.88 | 1.19 | |
| Al-Tayar, 2023 [36] | Mean | 8.19 | 7.75 | 16.17 | 18.78 | 18.94 | 19.06 | 10.01 | 9.27 |
| SD | 1.07 | 1.08 | 1.42 | 1.93 | 1.16 | 1.06 | 0.79 | 0.18 | |
| Al-Worafi, 2024 [5] | Mean | 9.49 | 9.48 | 15.68 | 15.69 | 18.23 | 18.32 | 12.44 | 12.81 |
| SD | 1.37 | 1.31 | 1.14 | 1.41 | 2.34 | 2.4 | 2.1 | 2.29 | |
| Zheng, 2023 [22] | Mean | 11.36 | 11.7 | 24.83 | 24.85 | 16.78 | 17.26 | 7.03 | 7.44 |
| SD | 0.8 | 0.7 | 2.09 | 2.01 | 1.4 | 1.41 | 0.87 | 0.91 | |
| Author | TMJ Spaces AJS (mm) | TMJ Spaces SJS (mm) | TMJ Spaces PJS (mm) | TMJ Spaces MJS (mm) | |||||
|---|---|---|---|---|---|---|---|---|---|
| Before | After | Before | After | Before | After | Before | After | ||
| Al-Somairi, 2025 [23] | Mean | 2.55 | 2.6 | 3.91 | 3.77 | 2.88 | 2.77 | 3.29 | 3.34 |
| SD | 0.69 | 0.76 | 0.94 | 0.97 | 0.56 | 0.46 | 0.83 | 0.92 | |
| Al-Tayar, 2023 [36] | Mean | 2.68 | 2.78 | 2.63 | 3.19 | 2.73 | 1.79 | 4.67 | 4.36 |
| SD | 1.16 | 1.06 | 0.22 | 0.02 | 1.31 | 0.19 | 0.92 | 0.66 | |
| Al-Worafi, 2024 [5] | Mean | 2.62 | 2.55 | 3.97 | 3.94 | 2.7 | 2.73 | 4.5 | 4.49 |
| SD | 0.69 | 0.66 | 1.05 | 0.93 | 0.71 | 0.76 | 1.5 | 1.46 | |
| Zheng, 2023 [22] | Mean | 2.55 | 2.33 | 2.85 | 3.55 | 1.99 | 2.35 | 2.85 | 2.86 |
| SD | 0.35 | 0.33 | 0.44 | 0.57 | 0.37 | 0.38 | 0.5 | 0.46 | |
| Dimension | Author | Number of Patients | Mean Difference | Standard Error | Lower 95% Confidence Interval | Upper 95% Confidence Interval | Significance Level |
|---|---|---|---|---|---|---|---|
| TMJ spaces PJS (mm) | Al-Somairi, 2025 [23] | 30 | −0.110 | 0.132 | −0.3749 | 0.1549 | 0.4092 |
| Al-Tayar, 2023 [36] | 23 | −0.940 | 0.276 | −1.4963 | −0.3837 | 0.0014 * | |
| Al-Worafi, 2024 [5] | 35 | 0.030 | 0.176 | −0.3208 | 0.3808 | 0.8650 | |
| Zheng, 2023 [22] | 22 | 0.360 | 0.113 | 0.1318 | 0.5882 | 0.0027 * | |
| TMJ spaces MJS (mm) | Al-Somairi, 2025 [23] | 30 | 0.050 | 0.226 | −0.4028 | 0.5028 | 0.8259 |
| Al-Tayar, 2023 [36] | 23 | −0.310 | 0.236 | −0.7858 | 0.1658 | 0.1960 | |
| Al-Worafi, 2024 [5] | 35 | −0.010 | 0.354 | −0.7160 | 0.6960 | 0.9775 | |
| Zheng, 2023 [22] | 22 | 0.010 | 0.145 | −0.2823 | 0.3023 | 0.9453 | |
| TMJ spaces SJS (mm) | Al-Somairi, 2025 [23] | 30 | −0.140 | 0.247 | −0.6336 | 0.3536 | 0.5724 |
| Al-Tayar, 2023 [36] | 23 | 0.560 | 0.046 | 0.4672 | 0.6528 | <0.0001 * | |
| Al-Worafi, 2024 [5] | 35 | −0.030 | 0.237 | −0.5031 | 0.4431 | 0.8997 | |
| Zheng, 2023 [22] | 22 | 0.700 | 0.154 | 0.3902 | 1.0098 | <0.0001 * | |
| TMJ spaces AJS (mm) | Al-Somairi, 2025 [23] | 30 | 0.050 | 0.187 | −0.3251 | 0.4251 | 0.7906 |
| Al-Tayar, 2023 [36] | 23 | 0.100 | 0.328 | −0.5603 | 0.7603 | 0.7617 | |
| Al-Worafi, 2024 [5] | 35 | −0.070 | 0.161 | −0.3921 | 0.2521 | 0.6659 | |
| Zheng, 2023 [22] | 22 | −0.220 | 0.103 | −0.4270 | −0.0130 | 0.0378 * | |
| Mandibular fossa dimension MFH (mm) | Al-Somairi, 2025 [23] | 30 | −0.11 | 0.549 | −1.2090 | 0.9890 | 0.8419 |
| Al-Tayar, 2023 [36] | 23 | −0.440 | 0.317 | −1.0789 | 0.1989 | 0.1721 | |
| Al-Worafi, 2024 [5] | 35 | −0.010 | 0.320 | −0.6494 | 0.6294 | 0.9752 | |
| Zheng, 2023 [22] | 22 | 0.340 | 0.222 | −0.1067 | 0.7867 | 0.1322 | |
| Mandibular fossa dimension MFW (mm) | Al-Somairi, 2025 [23] | 30 | 0.040 | 0.426 | −0.8129 | 0.8929 | 0.9255 |
| Al-Tayar, 2023 [36] | 23 | 2.610 | 0.500 | 1.6031 | 3.6169 | <0.0001 * | |
| Al-Worafi, 2024 [5] | 35 | 0.010 | 0.306 | −0.6016 | 0.6216 | 0.9741 | |
| Zheng, 2023 [22] | 22 | 0.020 | 0.618 | −1.2276 | 1.2676 | 0.9743 | |
| Condylar dimension CL (mm) | Al-Somairi, 2025 [23] | 30 | 0.060 | 0.386 | −0.7128 | 0.8328 | 0.8770 |
| Al-Tayar, 2023 [36] | 23 | 0.120 | 0.328 | −0.5403 | 0.7803 | 0.7159 | |
| Al-Worafi, 2024 [5] | 35 | 0.090 | 0.567 | −1.0406 | 1.2206 | 0.8743 | |
| Zheng, 2023 [22] | 22 | 0.480 | 0.424 | −0.3749 | 1.3349 | 0.2636 | |
| Condylar dimension CW (mm) | Al-Somairi, 2025 [23] | 30 | 0.120 | 0.270 | −0.4209 | 0.6609 | 0.6586 |
| Al-Tayar, 2023 [36] | 23 | −0.740 | 0.169 | −1.0805 | −0.3995 | 0.0001 * | |
| Al-Worafi, 2024 [5] | 35 | 0.370 | 0.525 | −0.6780 | 1.4180 | 0.4835 | |
| Zheng, 2023 [22] | 22 | 0.410 | 0.268 | −0.1317 | 0.9517 | 0.1341 |
| Variable | PJS | MJS | SJS | AJS | MFH | MFW | CL | CW |
|---|---|---|---|---|---|---|---|---|
| PJS | 1 | 0.4 | 0.4 | −1 | 1 | −0.8 | 0.4 | 1 |
| MJS | 0.4 | 1 | −0.4 | −0.4 | 0.4 | −0.2 | −0.4 | 0.4 |
| SJS | 0.4 | −0.4 | 1 | −0.4 | 0.4 | 0 | 1 | 0.4 |
| AJS | −1 | −0.4 | −0.4 | 1 | −1 | 0.8 | −0.4 | −1 |
| MFH | −1 | 0.4 | 0.4 | −1 | 1 | −0.8 | 0.4 | 1 |
| MFW | −0.8 | −0.2 | 0 | 0.8 | −0.8 | 1 | 0 | −0.8 |
| CL | 0.4 | −0.4 | 1 | −0.4 | 0.4 | 0 | 1 | 0.4 |
| CW | 1 | 0.4 | 0.4 | −1 | 1 | −0.8 | 0.4 | 1 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Galant, K.; Dąbrowska, S.; Turosz, N.; Małkiewicz, K. Impact of Molar Teeth Distalization by Clear Aligners on the Temporomandibular Joint: Systematic Review and Meta-Analysis. J. Clin. Med. 2025, 14, 5836. https://doi.org/10.3390/jcm14165836
Galant K, Dąbrowska S, Turosz N, Małkiewicz K. Impact of Molar Teeth Distalization by Clear Aligners on the Temporomandibular Joint: Systematic Review and Meta-Analysis. Journal of Clinical Medicine. 2025; 14(16):5836. https://doi.org/10.3390/jcm14165836
Chicago/Turabian StyleGalant, Kacper, Sylwia Dąbrowska, Natalia Turosz, and Konrad Małkiewicz. 2025. "Impact of Molar Teeth Distalization by Clear Aligners on the Temporomandibular Joint: Systematic Review and Meta-Analysis" Journal of Clinical Medicine 14, no. 16: 5836. https://doi.org/10.3390/jcm14165836
APA StyleGalant, K., Dąbrowska, S., Turosz, N., & Małkiewicz, K. (2025). Impact of Molar Teeth Distalization by Clear Aligners on the Temporomandibular Joint: Systematic Review and Meta-Analysis. Journal of Clinical Medicine, 14(16), 5836. https://doi.org/10.3390/jcm14165836






