Does a Dual-Mobility Cup Offer Better Stability than Conventional Bearings in Hip Arthroplasty Following Femoral Neck Fracture?
Abstract
1. Introduction
2. Methods
2.1. Study Design
2.2. Data Collection and Outcomes Measures
2.3. Statistical Analysis:
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- The International Hip Fracture Research Collaborative; Bhandari, M.; Devereaux, P.J.; Tornetta, P.; Swiontkowski, M.F.; Berry, D.J.; Haidukewych, G.; Schemitsch, E.H.; Hanson, B.P.; Koval, K.; et al. Operative Management of Displaced Femoral Neck Fractures in Elderly Patients: An International Survey. J. Bone Jt. Surg. 2005, 87, 2122. [Google Scholar] [CrossRef] [PubMed]
- Stirton, J.B.; Maier, J.C.; Nandi, S. Total hip arthroplasty for the management of hip fracture: A review of the literature. J. Orthop. 2019, 16, 141–144. [Google Scholar] [CrossRef]
- Moldovan, F.; Moldovan, L. A Modeling Study for Hip Fracture Rates in Romania. J. Clin. Med. 2025, 14, 3162. [Google Scholar] [CrossRef]
- Soong, M.; Rubash, H.E.; Macaulay, W. Dislocation After Total Hip Arthroplasty. JAAOS-J. Am. Acad. Orthop. Surg. 2004, 12, 314–321. Available online: https://journals.lww.com/jaaos/abstract/2004/09000/dislocation_after_total_hip_arthroplasty.6.aspx (accessed on 28 January 2025). [CrossRef]
- Iorio, R.; Healy, W.L.; Lemos, D.W.; Appleby, D.; Lucchesi, C.A.; Saleh, K.J. Displaced femoral neck fractures in the elderly: Outcomes and cost effectiveness. Clin. Orthop. Relat. Res. 2001, 383, 229–242. [Google Scholar] [CrossRef]
- Kurtz, S.M.; Ong, K.L.; Schmier, J.; Mowat, F.; Saleh, K.; Dybvik, E.; Kärrholm, J.; Garellick, G.; Havelin, L.I.; Furnes, O.; et al. Future Clinical and Economic Impact of Revision Total Hip and Knee Arthroplasty. J. Bone Jt. Surg. 2007, 89 (Suppl. S3), 144. [Google Scholar] [CrossRef]
- Shearer, D.W.; Youm, J.; Bozic, K.J. Short-term Complications Have More Effect on Cost-effectiveness of THA than Implant Longevity. Clin. Orthop. Relat. Res. 2015, 473, 1702–1708. [Google Scholar] [CrossRef]
- Ko, L.M.; Hozack, W.J. The dual mobility cup: What problems does it solve? Bone Jt. J. 2016, 98-B (Suppl. SA), 60–63. [Google Scholar] [CrossRef]
- Darrith, B.; Courtney, P.M.; Valle, C.J.D. Outcomes of dual mobility components in total hip arthroplasty: A systematic review of the literature. Bone Jt. J. 2018, 100-B, 11–19. [Google Scholar] [CrossRef] [PubMed]
- Horriat, S.; Haddad, F.S. Dual mobility in hip arthroplasty: What evidence do we need? Bone Jt. Res. 2018, 7, 508–510. [Google Scholar] [CrossRef] [PubMed]
- Ochi, H.; Baba, T.; Homma, Y.; Matsumoto, M.; Watari, T.; Ozaki, Y.; Kobayashi, H.; Kaneko, K. Total hip arthroplasty via the direct anterior approach with a dual mobility cup for displaced femoral neck fracture in patients with a high risk of dislocation. SICOT-J. 2017, 3, 56. [Google Scholar] [CrossRef]
- Tarasevicius, S.; Busevicius, M.; Robertsson, O.; Wingstrand, H. Dual mobility cup reduces dislocation rate after arthroplasty for femoral neck fracture. BMC Musculoskelet. Disord. 2010, 11, 175. [Google Scholar] [CrossRef]
- Zagorov, M.; Mihov, K.; Dobrilov, S.; Tabakov, A.; Gospodinov, A.; Nenova, G. Dual mobility cups reduce dislocation rate in total hip arthroplasty for displaced femoral neck fractures. J. IMAB—Annu. Proceeding Sci. Pap. 2018, 24, 2077–2081. [Google Scholar] [CrossRef]
- Albanese, K.M.; Deshmane, P.; Patil, N.; Larsen, D.A.; Ordway, N.R. Dual-Mobility Articulations in Femoral Neck Fractures: A Systematic Review of the Literature and Meta-analysis of the Outcomes. JAAOS—J. Am. Acad. Orthop. Surg. 2021, 29, e618. [Google Scholar] [CrossRef]
- Kang, M.J.; Kim, B.R.; Lee, S.Y.; Beom, J.; Choi, J.H.; Lim, J.Y. Factors predictive of functional outcomes and quality of life in patients with fragility hip fracture: A retrospective cohort study. Medicine 2023, 102, e32909. [Google Scholar] [CrossRef]
- Birkner, D.; Pigorsch, M.; Riedlinger, D.; Möckel, M.; Lindner, T.; Schenk, L.; Deutschbein, J. The vulnerability of hip fracture patients with cognitive impairment: An analysis of health conditions, hospital care, and outcomes. BMC Geriatr. 2025, 25, 99. [Google Scholar] [CrossRef]
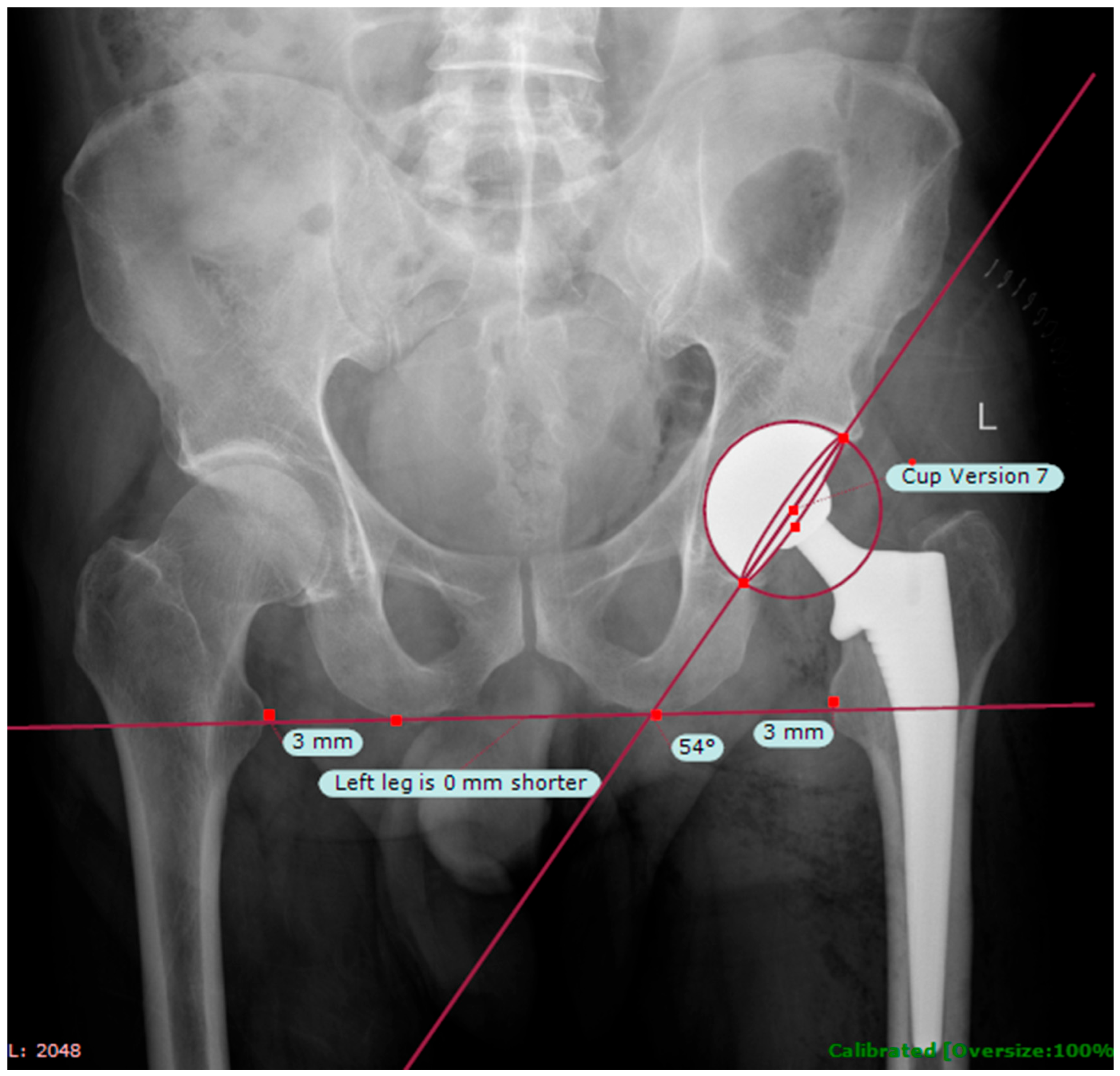
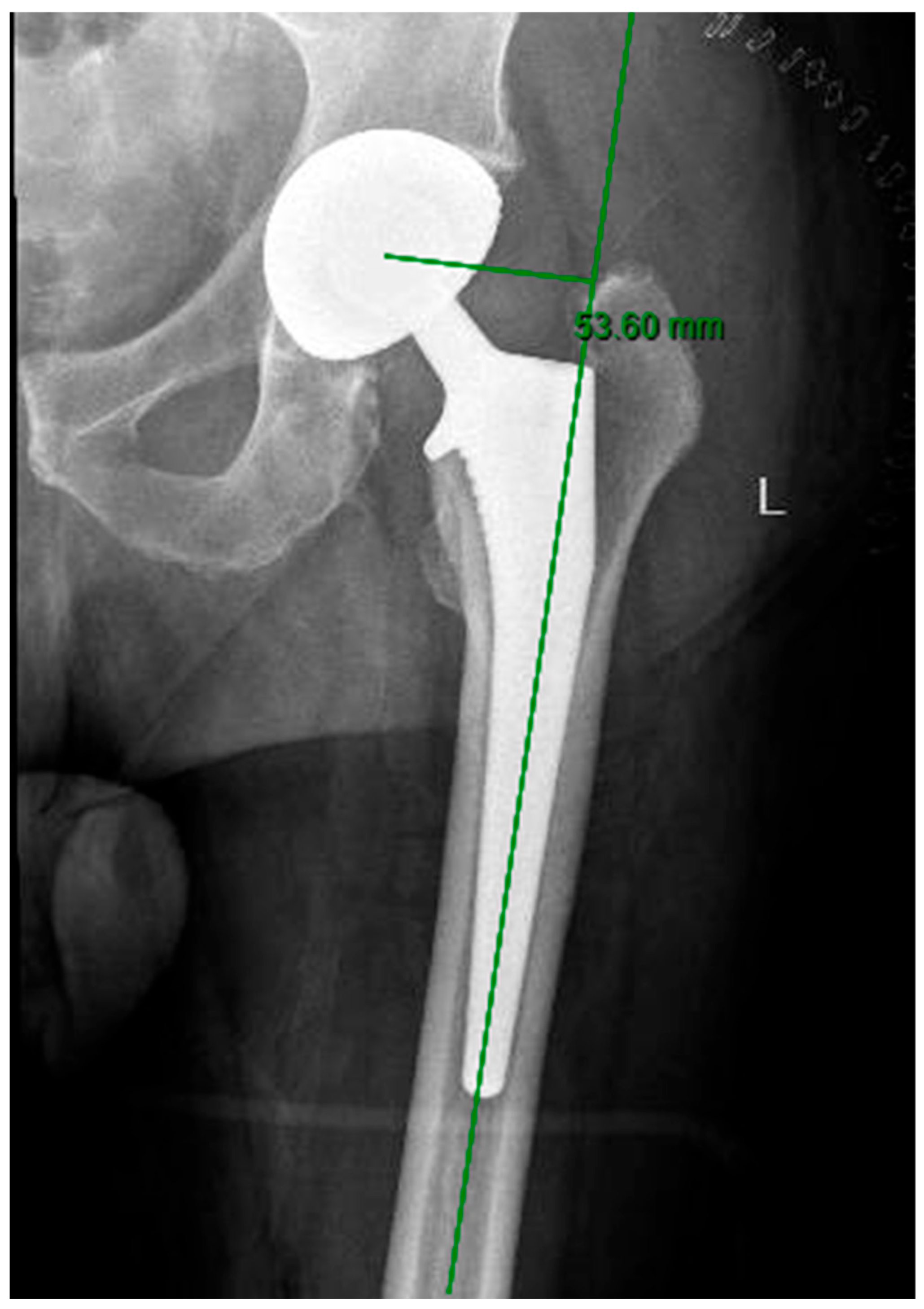
- Kumar, P.G.A.; Kirmani, S.J.; Humberg, H.; Kavarthapu, V.; Li, P. Reproducibility and accuracy of templating uncemented THA with digital radiographic and digital TraumaCad templating software. Orthopedics 2009, 32, 815. [Google Scholar] [CrossRef] [PubMed]
- Westacott, D.J.; McArthur, J.; King, R.J.; Foguet, P. Assessment of cup orientation in hip resurfacing: A comparison of TraumaCad and computed tomography. J. Orthop. Surg. Res. 2013, 8, 8. [Google Scholar] [CrossRef] [PubMed]
- Lecerf, G.; Fessy, M.H.; Philippot, R.; Massin, P.; Giraud, F.; Flecher, X.; Girard, J.; Mertl, P.; Marchetti, E.; Stindel, E. Femoral offset: Anatomical concept, definition, assessment, implications for preoperative templating and hip arthroplasty. Orthop. Traumatol. Surg. Res. 2009, 95, 210–219. [Google Scholar] [CrossRef] [PubMed]
- Hoggett, L.; Alexander, D.; Helm, A.; NWORC Collaborative. Post-operative complications following total hip arthroplasty for trauma: A multicentre cohort study comparing dual mobility with conventional acetabular bearings. J. Orthop. 2023, 40, 34–37. [Google Scholar] [CrossRef] [PubMed]
- van Erp, J.H.J.; Hüsken, M.F.T.; Filipe, M.D.; Snijders, T.E.; Kruyt, M.C.; de Gast, A.; Schlösser, T.P.C. Did the dislocation risk after primary total hip arthroplasty decrease over time? A meta-analysis across six decades. Arch. Orthop. Trauma Surg. 2023, 143, 4491–4500. [Google Scholar] [CrossRef]
- Lu-Yao, G.L.; Keller, R.B.; Littenberg, B.; Wennberg, J.E. Outcomes after displaced fractures of the femoral neck. A meta-analysis of one hundred and six published reports. J. Bone Jt. Surg. Am. 1994, 76, 15–25. [Google Scholar] [CrossRef]
- Prudhon, J.L.; Ferreira, A.; Verdier, R. Dual mobility cup: Dislocation rate and survivorship at ten years of follow-up. Int. Orthop. 2013, 37, 2345–2350. [Google Scholar] [CrossRef]
- Epinette, J.A.; Béracassat, R.; Tracol, P.; Pagazani, G.; Vandenbussche, E. Are Modern Dual Mobility Cups a Valuable Option in Reducing Instability After Primary Hip Arthroplasty, Even in Younger Patients? J. Arthroplast. 2014, 29, 1323–1328. [Google Scholar] [CrossRef]
- Jobory, A.; Kärrholm, J.; Overgaard, S.; Pedersen, A.B.; Hallan, G.; Gjertsen, J.-E.; Mäkelä, K.; Rogmark, C. Reduced Revision Risk for Dual-Mobility Cup in Total Hip Replacement Due to Hip Fracture: A Matched-Pair Analysis of 9,040 Cases from the Nordic Arthroplasty Register Association (NARA). J. Bone Jt. Surg. 2019, 101, 1278. [Google Scholar] [CrossRef]
- Cha, Y.H.; Yoo, J.I.; Kim, J.T.; Park, C.-H.; Ahn, Y.-S.; Choy, W.-S.; Ha, Y.-C.; Koo, K.-H. Dual mobility total hip arthroplasty in the treatment of femoral neck fractures: Systematic review and meta-analysis. Bone Jt. J. 2020, 102-B, 1457–1466. [Google Scholar] [CrossRef]
- Murphy, W.S.; Yun, H.H.; Hayden, B.; Kowal, J.H.; Murphy, S.B. The Safe Zone Range for Cup Anteversion Is Narrower Than for Inclination in THA. Clin. Orthop. Relat. Res. 2018, 476, 325–335. [Google Scholar] [CrossRef] [PubMed]
- Ng, V.Y.; Mcshane, M.A. Understanding Acetabular Cup Orientation: The Importance of Convention and Defining the Safe Zone. Hip Int. 2011, 21, 646–652. [Google Scholar] [CrossRef] [PubMed]
- Lewinnek, G.E.; Lewis, J.L.; Tarr, R.; Compere, C.L.; Zimmerman, J.R. Dislocations after total hip-replacement arthroplasties. J. Bone Jt. Surg. Am. 1978, 60, 217–220. [Google Scholar] [CrossRef]
- Ohmori, T.; Kabata, T.; Maeda, T.; Kajino, Y.; Taga, T.; Hasegawa, K.; Inoue, D.; Yamamoto, T.; Takagi, T.; Tsuchiya, H. Increase in safe zone area of the acetabular cup using dual mobility cups in THA. Hip Int. 2017, 27, 361–367. [Google Scholar] [CrossRef]
- Seagrave, K.G.; Troelsen, A.; Anders, M.; Henrik, H.; Henrik Gromov, K. Acetabular cup position and risk of dislocation in primary total hip arthroplasty: A systematic review of the literature. Acta Orthop. 2017, 88, 10–17. [Google Scholar] [CrossRef] [PubMed]
- Tezuka, T.; Heckmann, N.D.; Bodner, R.J.; Dorr, L.D. Functional Safe Zone Is Superior to the Lewinnek Safe Zone for Total Hip Arthroplasty: Why the Lewinnek Safe Zone Is Not Always Predictive of Stability. J. Arthroplast. 2019, 34, 3–8. [Google Scholar] [CrossRef] [PubMed]
| DM THA (n = 82) | Standard THA (n = 488) | p-Value | |
|---|---|---|---|
| Female Sex, n (%) | 55 (67) | 315 (64.5) | 0.674 |
| Mean age, years (SD) | 73.72 (8.39) | 72.45 (8.98) | 0.211 |
| Mean CCI (SD) | 3.71 (1.60) | 3.61 (1.61) | 0.648 |
| Mean BMI, Kg/m2 (SD) | 26.40 (5.15) | 25.33 (4.27) | 0.091 |
| ASA classification, n (%) | 0.567 | ||
| 1 | 1 (1.22) | 33 (6.76) | |
| 2 | 42 (51.22) | 292 (59.84) | |
| 3 | 35 (42.68) | 152 (31.15) | |
| 4 | 1 (1.22) | 8 (1.64) | |
| Mean LLD, mm (SD) | 0.72 (6.52) | 1.64 (7.30) | 0.384 |
| Mean Cup Anteversion, Deg (SD) | 11.34 (7.03) | 14.06 (5.34) | 0.006 |
| Mean Femoral Offset, mm (SD) | 44.92 (7.34) | 45.31 (5.88) | 0.697 |
| Dislocations, n (%) | 1 (1.22) | 5 (1.02) | 0.873 |
| Revision of any cause, n (%) | 1 (1.22) | 14 (2.87) | 0.387 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ron, I.; Ashkenazi, I.; Snir, N.; Warschawski, Y.; Gold, A. Does a Dual-Mobility Cup Offer Better Stability than Conventional Bearings in Hip Arthroplasty Following Femoral Neck Fracture? J. Clin. Med. 2025, 14, 5613. https://doi.org/10.3390/jcm14165613
Ron I, Ashkenazi I, Snir N, Warschawski Y, Gold A. Does a Dual-Mobility Cup Offer Better Stability than Conventional Bearings in Hip Arthroplasty Following Femoral Neck Fracture? Journal of Clinical Medicine. 2025; 14(16):5613. https://doi.org/10.3390/jcm14165613
Chicago/Turabian StyleRon, Itay, Itay Ashkenazi, Nimrod Snir, Yaniv Warschawski, and Aviram Gold. 2025. "Does a Dual-Mobility Cup Offer Better Stability than Conventional Bearings in Hip Arthroplasty Following Femoral Neck Fracture?" Journal of Clinical Medicine 14, no. 16: 5613. https://doi.org/10.3390/jcm14165613
APA StyleRon, I., Ashkenazi, I., Snir, N., Warschawski, Y., & Gold, A. (2025). Does a Dual-Mobility Cup Offer Better Stability than Conventional Bearings in Hip Arthroplasty Following Femoral Neck Fracture? Journal of Clinical Medicine, 14(16), 5613. https://doi.org/10.3390/jcm14165613






