Abstract
Background/Objectives: The rapid ageing of the European population presents growing challenges for mental health, highlighting the need to identify factors that can prevent or delay psychological decline and promote a higher quality of life in later life. This study aims to provide an updated and comprehensive overview of mental health among older adults in Europe by examining the prevalence of depressive symptoms and identifying key associated factors. Methods: We analysed data from individuals (n = 45,601) aged 65 years and older across 27 European countries and Israel who participated in Wave 9 of the Survey of Health, Ageing and Retirement in Europe (SHARE). This study assessed the prevalence of depressive symptoms, which were evaluated using the EURO-D scale (score range: 0–12), with a cut-off of ≥4 indicating clinically relevant symptoms. It also explored associations with sociodemographic characteristics, physical health, behavioural factors, social participation, internet skills and living conditions. Results: Our findings confirm that depressive symptoms remain highly prevalent among older adults in Europe, with 35.1% of women and 21.5% of men affected, reflecting persistent gender disparities in mental health. Depression in later life was significantly associated with poor physical health, loneliness and lower quality of life. Conversely, moderate involvement in grandchild care and in social participation emerged as potential protective factors. Conclusions: Late-life depression has substantial implications for both mental and physical well-being. Our findings suggest that social integration, gender related factors and physical health are closely associated with depressive symptoms in older adults. These associations highlight the importance of considering these domains when designing interventions and policies aimed at promoting mental health in ageing populations.
1. Introduction
A significant accomplishment of the last century has been the increase in average life expectancy due to advancements in healthcare, technology and overall living conditions [1,2]. However, the gap between life expectancy and healthy life expectancy continues to grow in Europe, with many individuals living considerable years in poor health [3]. The increase in life expectancy and the declining fertility rates has led to the rapid ageing of the European population, which presents significant challenges for public health, such as a growing prevalence of mental health issues among older adults [4,5].
According to the World Health Organization [6], mental health is more than just the absence of mental disorders, it encompasses both the prevention of negative mental states and the promotion of positive psychological well-being. Depression remains a major mental health concern in older adults. It is estimated that over one-third of the older population experiences depression [7], but this condition is often underrecognized and undertreated in older individuals [8,9,10,11]. When left untreated or inadequately managed, late-life depression is associated with higher mortality rates, dementia and suicide [10,12].
Social isolation and loneliness comprise one of the main factors contributing to the risk of depressive symptoms in aged individuals, especially in high-income countries [13,14,15]. Ageing often leads to reduced social participation due to declining physical and psychological functioning [16,17]. Compared to younger adults, seniors usually have smaller social networks composed mainly of close family members or long-term friends, and the increasing tendency to live alone or separate from family increases the risk of loneliness [18,19,20].
Societal changes, including evolving family structures and intergenerational dynamics, limit meaningful social interactions among older adults, thereby increasing loneliness [8,18,21,22]. Participation in intergenerational activities, such as those involving grandchildren, has been associated with enhanced emotional well-being and reduced depressive symptoms [23,24,25].
In this context, digital technologies have emerged as a potential means to reduce social isolation and promote mental health among seniors [26,27]. Research indicates [28,29,30] that internet use can have positive effects on mental health by reducing loneliness and depressive symptoms in seniors. However, barriers such as limited digital literacy, restricted access to technology [31,32,33], mobility limitations [34], hearing and vision impairment [35], rural residency [36] and socioeconomic disparities [8,37] still hinder the effective use of such tools.
Thus, understanding these diverse and multifaceted events is essential to identify factors that prevent or delay mental health decline and that promote a higher quality of life for older adults, maintaining the long-term sustainability of European healthcare and financial systems [5].
Previous research often focuses on isolated variables when evaluating mental health in the older population. Thus, this study analyses multiple interconnected factors including sociodemographic characteristics, physical health, behavioural factors, social participation, internet skills and living conditions. Our aim is to provide an updated and comprehensive overview of the mental health landscape in Europe, using data from Wave 9 of the Survey of Health, Ageing and Retirement in Europe (SHARE), by examining the prevalence of depressive symptoms among older adults across 27 European countries and Israel and identifying the main associated factors.
2. Materials and Methods
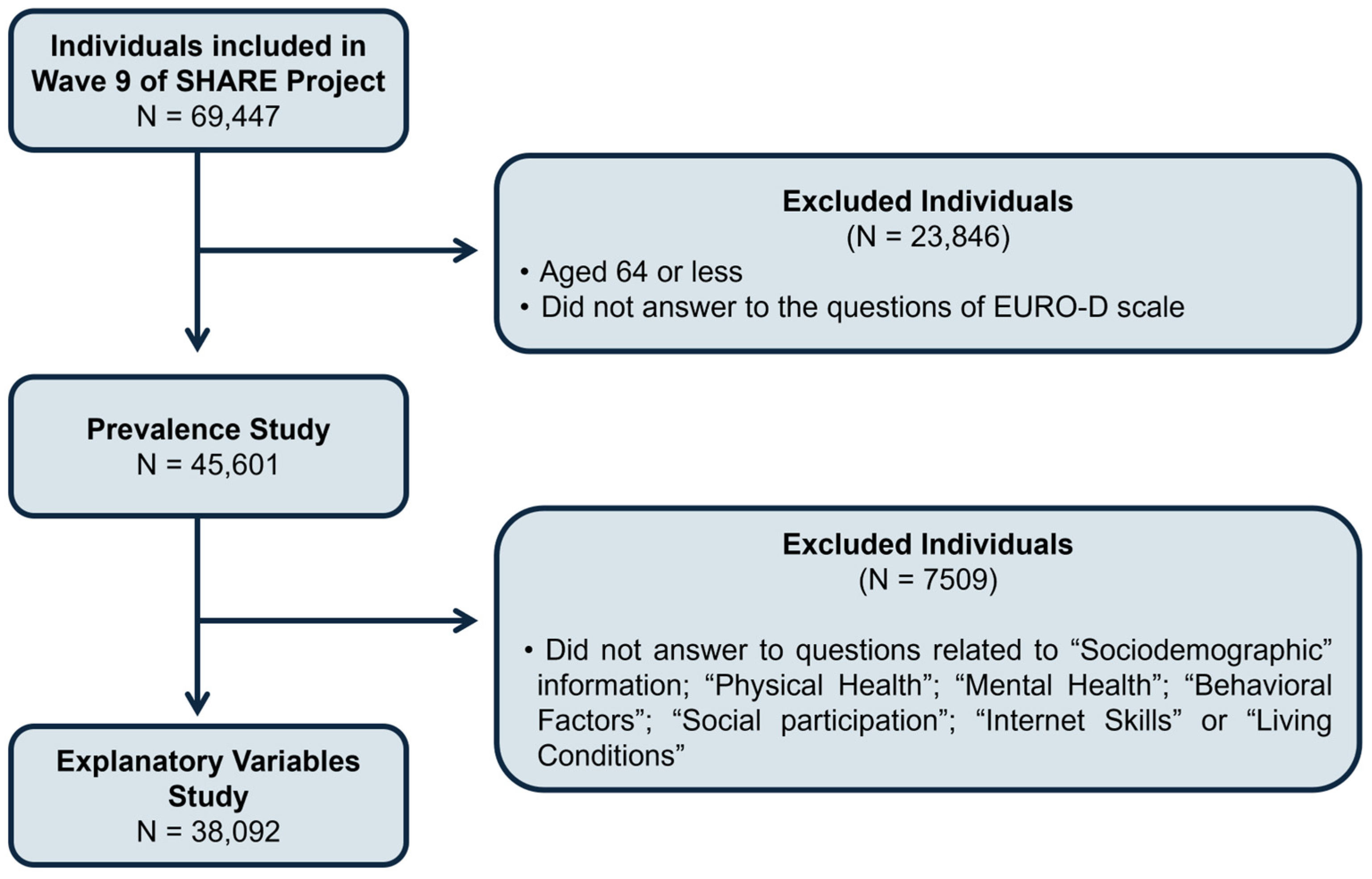
This work used data from the SHARE Wave 9 database, which is an international and multidisciplinary database of detailed information about demographics, health, socioeconomic status and social and family networks from representative samples of community-based populations from 27 European countries (Austria, Belgium, Bulgaria, Croatia, Cyprus, the Czech Republic, Denmark, Estonia, Finland, France, Germany, Greece, Hungary, Italy, Latvia, Lithuania, Luxembourg, Malta, the Netherlands, Poland, Portugal, Romania, Slovakia, Slovenia, Spain, Sweden and Switzerland) and Israel. For statistical analysis proposes, we grouped these countries into four regions: northern (Denmark, Estonia, Finland, Latvia, Lithuania and Sweden), southern (Croatia, Cyprus, Greece, Italy, Malta, Portugal, Slovenia, Spain and Israel), western (Austria, Belgium, France, Germany, Luxembourg, Netherlands and Switzerland) and eastern (Bulgaria, Czech Republic, Hungary, Poland, Romania and Slovakia). This project is an important source of data for ageing research in Europe [38]. SHARE data was collected through computer-assisted personal interviewing conducted face-to-face by trained interviewers, and participants were recruited from the general population based on specific eligibility criteria: individuals aged 50 years and older who resided regularly in the participating SHARE country. Exclusions applied to individuals who were incarcerated, hospitalized for the entire fieldwork period, had moved abroad or to an unknown address or who could not speak the national language(s). Wave 9 data were collected between October 2021 and September 2022 from 69,447 individuals, aged between 20 and 106 years. For this work, we analysed individuals aged 65 years or older, who were categorised into three groups: 65–74 years, 75–84 years and 85 years or older (Figure 1).
Figure 1.
Flow diagram illustrating the selection process of participants for the prevalence and explanatory variables analysis.
2.1. Prevalence of Depressive Symptoms
Depressive symptoms were evaluated using the EURO-D scale that measures current levels of depression based on 12 items: depressed mood, pessimism, suicidality, guilt, sleep, interest, irritability, appetite, fatigue, concentration, enjoyment and tearfulness. Every item is scored 1 if present and 0 if absent. The final scores ranged from 0 (“not depressed”) to 12 (“highly depressed”) and were dichotomised into “Without depressive symptoms” (scores < 4) and “With depressive symptoms” (scores ≥ 4) [39,40]. The specific questions of the EURO-D scale can be found in the Supplementary Materials section.
2.2. Explanatory Variables
As a result of the large amount of information available in the SHARE database, we were able to evaluate a diverse set of putative explanatory variables in this study. These variables were organised into seven groups: Sociodemographic, Physical Health, Mental Health, Behavioural Factors, Social Participation, Internet Skills and Living Conditions. Detailed information about questions and answer options for each variable can be obtained from the Supplementary Materials section.
2.2.1. Sociodemographic
The variables “Gender”, “Age”, “Marital Status”, “Years of Education”, “Shortage of Money” and “Job Situation” were included in this group. “Gender” was identified as either male or female. “Age” was calculated by subtracting the participants’ reported birth year from 2022 and grouped into three categories, 65–74 years, 75–84 years and 85 years or older, as previously defined [40]. “Marital Status” and “Job Situation” were evaluated based on self-reported information and categorised accordingly, as described in [8,40]. The education level (“Years of Education”) was measured by the total number of years spent in full-time education and categorised into four levels [40]. Socioeconomic status (“Shortage of Money”) was assessed through a question about financial difficulties impacting daily activities, in line with previous research [40].
2.2.2. Physical Health
This group incorporated the following variables: “Number of Chronic Diseases”, “Number of Limitations in Activities of Daily Living (ADLs)”, “Number of Limitations in Instrumental Activities of Daily Living (iADLs)”, “Limitation in Activities because of Health”, “Hearing”, “Vision”, “Pain”, “Receive Professional Health Services” and “Hospital Stays in the Last 12 months”. The “Number of Chronic Diseases”, “Limitation in Activities because of Health”, “Hearing”, “Vision” and “Pain” variables were evaluated based on self-reported diagnoses by each individual and categorised according to previous studies [35,40]. The number of ADLs and iADLs were calculated by summing reported difficulties in different tasks and recoded into three levels, in line with previous research [40]. “Hospital Stays in the Last 12 months” and “Received Professional Health Services” were recorded as binary variables, as previously described [40].
2.2.3. Mental Health
Besides the depressive symptoms, mental health in older adults was also addressed by self-evaluation questions about the quality of life, well-being and loneliness. “Quality of Life and Well-Being” was determined through the Control, Autonomy, Self-realisation and Pleasure (CASP-12) scale, a 12-item self-assessment questionnaire that measures quality of life [41,42]. Each question is rated from 1 (never) to 4 (often), and the total score ranges from 12 to 48, with higher scores meaning better quality of life. “Loneliness” was evaluated by the Three-Item Loneliness Scale, which measures indirect loneliness based on questions about companionship, feeling left out and isolation [43,44]. Total scores range from 3 to 9, and the final answers were grouped into two categories [8]: “Not lonely” for scores between 3 and 5, and “Lonely” for scores of 6 or higher.
2.2.4. Behavioural Factors
The variables “Physical Inactivity”, “Alcohol Intake” and “Ever Smoked Daily” were included in this group. “Physical Inactivity” was assessed through questions about engaging in vigorous or moderate physical activity, and it was recoded into two categories, “Engage in vigorous or moderate physical activity” and “Never engage in vigorous or moderate physical activity”, as previous defined [8]. “Ever Smoked Daily” and “Alcohol Intake” were recorded as binary variables [40].
2.2.5. Social Participation
To identify older adults’ social participation in activities, social networks and intergenerational relationships, the variables “Number of Social Activities”, “Satisfaction with Social Activities”, “Network Satisfaction” and “Looking after Grandchildren” were assessed and categorised as described in [21,22]. The “Number of Social Activities” was calculated by asking the participants which social activities they had engaged in the last year, and answers were grouped into three levels. “Satisfaction with Social Activities” and “Network Satisfaction” were evaluated on a scale from 0 to 10, where 0 means completely dissatisfied and 10 means completely satisfied. “Looking after Grandchildren” was assessed based on questions about having grandchildren and looking after them regularly or occasionally, and answers were grouped into three categories.
2.2.6. Internet Skills
Internet skills were determined by asking the participants if they used the internet for several purposes during the last week. Responses were recorded as “Yes” and “No”, as previously described [33].
2.2.7. Living Conditions
Living conditions were evaluated using two variables: “Area of Building” and “Type of Building”. Both variables were based on self-reported information from each participant about the place where they live and categorised according to previous research [40].
2.3. Statistical Analysis
IBM SPSS Statistics 29 for Windows (SPSS Inc., Chicago, IL, USA) software was used for statistical analysis. A descriptive analysis was conducted to estimate the proportion of individuals experiencing depressive symptoms across 28 countries. The age and gender standardised prevalence of depressive symptoms in each country was calculated, along with the corresponding 95% confidence intervals (95% CI). The 2013 European standard population was used to standardise all prevalence results. Considering the multilevel nature of the data, with individuals grouped within countries, a multilevel logistic regression model was employed, treating depressive symptoms as the dependent variable. Initially, multilevel univariable logistic regression models were conducted to evaluate the relationship between each individual covariate and depressive symptoms (unadjusted model). Given the multilevel structure and the focus on the final multivariable multilevel model where covariates were mutually adjusted, we did not apply formal correction for multiple comparisons in the univariable analyses. Covariates found to be statistically significant were subsequently entered into a multivariable multilevel logistic regression model (adjusted model) [45,46]. To assess whether the association between explanatory variables and depressive symptoms varied by age group or by cultural differences between European regions, stratified analysis (bivariate logistic regression) was performed to evaluate the association between them across different age groups (Table S1) and different regions (Table S2). All the results were presented as odds ratios (OR) with a corresponding 95% CI. A p < 0.05 value was considered statistically significant.
3. Results
3.1. Prevalence Study
For this study, from all the participants in Wave 9 of the SHARE survey, we selected those aged 65 years or older who answered questions related to “Age”, “Gender” and to the EURO-D scale, which resulted in a total of 45,601 individuals (Figure 1).
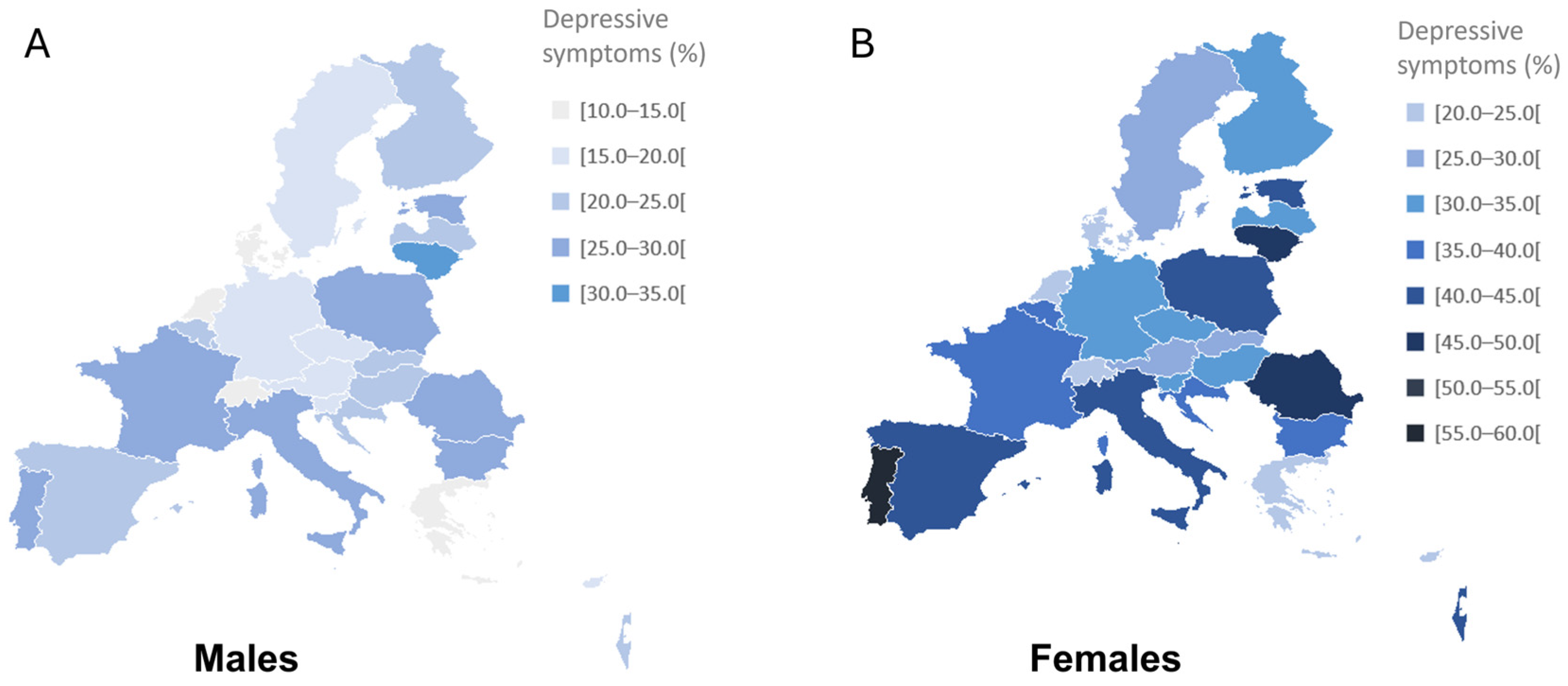
Participants presented a mean age of 74.9 ± 7.0, and 56.7% were female. The geographical distribution of depressive symptoms was evaluated across different European countries and Israel, and the results are represented in Figure 2.
Figure 2.
Prevalence of depressive symptoms among European older adults (≥65 years) in 27 European countries and Israel, by gender: males (A) and females (B). Data are presented as percentages.
The overall prevalence of depressive symptoms was 29.2%, with prevalence rates varying from 18.4% to 44.5%. Portugal (44.5%) presented the highest prevalence of depressive symptoms, followed by Lithuania (42.6%) and Romania (38.6%), while Denmark (18.4%), the Netherlands (19.1%) and Switzerland (19.1%) showed the lowest rates (Table 1). The presence of depressive symptoms was higher in women than men (35.1% and 21.5%, respectively) for all age groups and countries, except for people over 85 years in Bulgaria (59.1% and 46.9% for males and females) and Luxembourg (27.8% and 25.0% for males and females) and people living in Cyprus between 65 and 74 years (16.8% and 15.0% for males and females). Overall, the likelihood of experiencing depressive symptoms increased with age (24.2%, 31.9% and 43.6% for people aged 65–74 years, 75–84 years and ≥85 years, respectively). This tendency was also observed in both men (17.3%, 23.2% and 34.7% for people aged 65–74 years, 75–84 years and ≥85 years, respectively) and women (29.6%, 38.3% and 49.4% for people aged 65–74 years, 75–84 years and ≥85 years, respectively).

Table 1.
Prevalence of depressive symptoms specified by age, gender and country, according to the EURO-D scale, among the 28 countries included in Wave 9 of the Survey of Health, Age and Retirement in Europe (SHARE).
3.2. Association of Depressive Symptoms with Explanatory Variables
Participants from the prevalence study who answered all the questions related to the explanatory variables were included in the evaluation of the relationship between those variables and depressive symptoms. This process resulted in a total of 38,092 participants (Figure 1) with an average age of 74.8 ± 6.9 years, and 21,838 (42.7%) were female.
Using unadjusted models across all participating countries, a significant relationship was found between depressive symptoms and most of the exploratory variables studied (Table 2). “Area of Building” was the only variable that showed no association with depressive symptoms (Table 2).

Table 2.
Association of explanatory variables with depressive symptoms (unadjusted and adjusted models).
The adjusted model (Table 2) revealed a significant association with all variables in the “Sociodemographic” group except for “Job Situation”. Women were nearly two times more prone to report depressive symptoms compared to men (OR = 1.980, 95% CI: 1.862–2.106), while participants aged 85 years were less prone to report depressive symptomatology (OR = 0.834, 95% CI: 0.754–0.922). Using the adjusted model, married individuals or those in a registered partnership, compared to those who were single, were more prone to have depressive symptoms (OR = 1.188, 95% CI: 1.025–1.378). However, this association was found to be influenced by regional heterogeneity (Table S2) and by age, since a significant association between marital status and depressive symptoms was observed only among individuals aged 75 to 84 (Table S1). “Years of Education” was identified as a variable with statistical significance only for individuals with high education (OR = 1.134, 95% CI: 1.043–1.233), but the association between “Years of Education” and depressive symptoms was observed exclusively in individuals aged 75 to 84 years (Table S1) and was found to depend on regional heterogeneity (Table S2). “Shortage of Money” was significantly associated with depressive symptoms once depressive symptoms decreased when financial difficulties increased (Tables S1, S2 and Table 2).
In the “Physical Health” group, a significant relationship was observed between depressive symptoms and all studied variables (Table 2). The likelihood of reporting depressive symptoms increased with the “Number of Chronic Diseases” in the northern and western regions (Table 2 and Table S2). Number of limitations performing “iADLs” (OR = 1.325, 95% CI: 1.230–1.428), “Hearing” (OR = 1.233, 95% CI: 1.155–1.317) and “Stayed Overnight in Hospital” (OR = 1.344, 95% CI: 1.248–1.447) had a significant association with depressive symptoms. “Received Professional Services” presented a significant relation with depressive symptoms (OR = 1.099, 95% CI: 1.004–1.204) but only for participants aged 75 to 84 years old (Table S1) and in the southern region (Table S2). “Pain” was significantly associated with depressive symptoms, as higher levels of pain were correlated with increased depressive symptoms. Conversely, fewer “Limitations in Activities because of Health” were associated with lower levels of depressive symptoms. Number of limitations performing “ADLs” (OR = 1.206, 95% CI: 1.103–1.318) and “Vision” (OR = 1.211, 95% CI: 1.136–1.292) were also significantly associated with depressive symptoms but were dependent on the cultural differences between regions (Table S2).
Regarding the “Mental Health” group, individuals presenting signs of “Loneliness” reported twice the number of depressive symptoms (OR = 2.111, 95% CI: 1.967–2.267), and higher “Quality of Life and Well-Being” (OR = 0.864, 95% CI: 0.859–0.870) were correlated with lower levels of depressive symptoms (Table 2).
Among the “Behavioural Factors”, only the variable “Ever Smoked Daily” showed a significant negative relationship with depressive symptoms (OR = 0.890, 95% CI: 0.839–0.945) just for individuals between 65 and 74 years old (Table S1) and for the northern, southern and eastern regions.
All variables in the “Social Participation” group presented a significant association with depressive symptoms (Table 2). “Satisfaction with Social Activities” (OR = 0.933, 95% CI: 0.920–0.946) was negatively associated with depressive symptoms, whereas an increase in the “Number of Social Activities” corresponded to higher levels of depression only for the northern region (Table S2). “Network Satisfaction” (OR = 0.975, 95% CI: 0.955–0.995) was also negatively correlated with depressive symptoms but only for participants aged 65–74 and 75–84 (Table S1) and for the northern region. “Looking after Grandchildren” was identified as a variable with statistical significance only for individuals who had grandchildren and contact with them (OR = 1.143, 95% CI: 1.038–1.260) but only for individuals between 65 and 74 years old (Table S1) and for the southern and western regions (Table S2).
“Internet skills” showed no association with depressive symptoms, and the variable “Type of Building” revealed a positive relationship only for participants who lived in a building with three or more floors (OR = 1.136, 95% CI: 1.014–1.273), were aged 85 or more and lived in the southern, western or eastern regions (Table 2, Tables S1 and S2).
4. Discussion
Depressive symptoms among older adults represent a significant public health concern, particularly in ageing populations across Europe [7]. In this study, the overall prevalence of depressive symptoms in the older European and Israeli population was found to be 29.2%. This finding is consistent with recent evidence from a meta-analysis [47] as well as with a recent study [48] using multiple waves of the SHARE dataset, both of which reported a similar prevalence of depressive symptoms among older adults of approximately 28%.
We observed a higher prevalence of depressive symptoms in women compared to men across all age groups and in every country analysed (Figure 1 and Table 1). Although women generally outlive men, they also tend to report poorer overall health, including higher rates of psychological distress [49]. Our study confirmed the consistent and marked gender difference in depressive symptoms among older adults, findings that are well documented in previous research [48,50,51,52]. However, there is still limited understanding of the underlying causes of this disparity in later life, and whether the mechanisms behind it are the same as those observed in younger populations [53]. Nevertheless, previous analyses of specific EURO-D items [54,55] suggest that this disparity is driven largely by higher rates of tearfulness, depressed mood and sleep-related complaints among women. These disparities call for gender-sensitive mental health interventions.
Overall, the prevalence of depressive symptoms in participants over the age of 85 was higher for both men and women (Table 1), as previously reported [56]. However, after using the adjusted model, we observed a lower prevalence of depressive symptoms among individuals aged 85 and older (Table 2). Some studies [57,58] propose that individuals who reach very old age tend to exhibit greater physical and psychological resilience and increasingly prioritise emotionally meaningful experiences while developing more effective coping strategies, which may help to protect against depressive symptoms.
Interestingly, individuals who were married or in a relationship reported higher levels of depressive symptoms compared to those who were single for individuals aged 75 to 84 (Table 2). This contrasts with most previous findings, which generally suggest that being married or in a relationship has a beneficial effect on mental health [50,53]. However, many of these studies did not stratify by gender, despite growing evidence that the mental health impact of marriage differs between men and women, especially in older adults [59,60]. In fact, gender roles within marriage were often traditional, with women more likely to have sacrificed educational and professional opportunities to maintain the household. In contrast, men’s educational or occupational trajectories were generally unaffected by marriage. Moreover, marital status alone may not accurately reflect relationship quality: individuals in unsatisfying or conflictual relationships may experience higher levels of depressive symptoms [61].
A higher number of “Years of Education” was associated with lower depressive symptoms, as is well documented in the literature [62], but when the adjusted model was applied, individuals with higher education exhibited more depressive symptoms for participants between 75 and 84 years old (Table 2). Some studies [63] reveal that older adults with higher education may have greater life expectations regarding career, financial security or social status and that unmet expectations in later life could lead to increased psychological distress. Another hypothesis [64] is that more educated individuals may be more cognitively aware of their own functional or social decline, which could exacerbate depressive symptoms. Nevertheless, it is also important to note that both the association between depressive symptoms with “Marital Status” and “Years of Education” were influenced by cultural differences between countries, which could explain these unexpected results.
Financial status affects health in several ways, including reduced access to health care, poor health-related choices and limited opportunities for treatments, all of which contribute to an increased risk of disability in old age [65]. Consistent with these findings, we found that a higher “Shortage of Money” was associated with an increased prevalence of depressive symptoms (Table 2). Nevertheless, it is important to note that the “Job Situation”, often linked to financial capacity, was excluded from the adjusted model, since its effects were deemed insignificant after adjusting for all variables.
There is broad consensus that physical health influences mental health, even among older adults [64], and our findings support this association. Participants with poorer physical health consistently reported higher levels of depressive symptoms (Table 2). Specifically, depressive symptoms were more prevalent among those with a higher “Number of Chronic Diseases” belonging to the northern and western regions, greater limitations in “ADLs” (except for the western region) and “iADLs”, more frequent “Limitations in Activities because of Health”, increased levels of “Pain” and greater difficulties with “Vision” (except for the northern region) and “Hearing” (Table 2). Individuals aged 75 to 84 and individuals from the southern region who stated, “Receiving Professional Health Services” and participants having “Stayed Overnight in a Hospital” also reported higher levels of depressive symptoms. These findings are in line with prior research [66,67,68,69] showing that in later life, poor physical health is a significant predictor of depressive symptoms. It is important to mention that medication use can also have a significant influence on depressive symptoms; however, although data on polypharmacy are available in the SHARE database, they do not allow for detailed information on specific medications use on depressive symptoms.
Depression significantly impacts health and risk behaviours, as it can decrease or inhibit the motivation to engage in healthy habits and prioritise one’s well-being [21]. Although “Alcohol Intake” and “Physical Inactivity” did not significantly correlate with depressive symptoms, when the adjusted model was applied, we observed that individuals between 65 and 74 years old who do not smoke daily reported lower depressive symptoms (except those from the western region) (Table 2). On the other hand, a high quality of life and well-being can contribute to better health by promoting a sense of optimism that encourages individuals to adopt and maintain healthy behaviours [70]. In fact, in our study, participants who reported more depressive symptoms also tended to report a lower “Quality of Life and Well-Being” (Table 2), reinforcing the critical role of depressive symptoms as a key determinant of perceived quality of life in older populations [71].
Social isolation and loneliness are a significant threat to the mental health and well-being of older adults, as advancing age is often accompanied by a decrease in social networks and an increased likelihood of living alone, both of which heighten the risk of depression [17,22,72]. Consequently, maintaining meaningful social relationships and engaging in social activities are consistently associated with greater psychological resilience [21]. In line with this evidence, our findings show that older adults who report signs of loneliness experience twice as many depressive symptoms, while individuals who express higher satisfaction with their social networks (only the ones living in the northern region) and social activities report fewer symptoms (Table 2).
However, an unexpected finding in our study was that a higher “Number of Social Activities” was associated with increased depressive symptoms for participants living in the northern region (Table 2). Aside from cultural differences between Northern Europe and other regions, this seemingly paradoxical result aligns with some research [21,73] that suggests a natural limit to human social network size, that is, when individuals exceed this limit, social overcommitment may occur, potentially leading to emotional fatigue and poorer mental health outcomes.
Intergenerational contact has been identified as reducing loneliness in older age [25]. In this context, grandparent–grandchild interactions—such as caring for grandchildren on weekends, after school hours, or during specific occasions—are frequently associated with enhanced psychological well-being [25,74]. However, other studies have cautioned against the potential physical and psychological burdens of caregiving, particularly when the responsibility is frequent or sustained, as excessive involvement may become a source of stress rather than support [75,76]. Our findings align with this latter perspective, as we observed that individuals aged 65 to 74 and participants living in the southern and western regions who maintain regular contact with grandchildren exhibit higher levels of depressive symptoms.
The use of the internet and digital technologies has been widely recognised as a potential tool to reduce loneliness and enhance social connectedness among older adults, thereby contributing to lower levels of depressive symptoms [27,77]. In our study, initial analyses suggested that older adults who did not use the internet reported higher depressive symptoms, but after adjusting for all variables, this effect was considered insignificant. This may indicate that the protective effects of technology use are mediated by other factors, such as social support or cognitive function, rather than exerting a direct influence. Nevertheless, it is important to note that the “Use of Internet in Past 7 Days” variable measures only the internet usage over the past week, which can be reductive, as it does not distinguish between types of use or actual digital skills.
Finally, we found a connection between depressive symptoms and the “Type of Building” individuals live in but not with the “Area of Building”. Older adults who are 85 years old or more and who live in a building with three or more floors reported higher depressive symptoms (except for the ones living in the northern region) (Table 2). This finding contrasts with the existing literature [78], which typically indicates a higher rate of depression among nursing home residents compared to residents in private households. One possible explanation is that those living independently in private apartments may face greater social withdrawal despite living in the community [79]. In fact, social isolation in private homes, particularly in urban settings like apartment buildings, can go unnoticed, as neighbours often have limited interaction. Moreover, mobility constraints that hinder access to social spaces or services and environmental stressors such as noise, lack of green space and poor building conditions have been associated with worsened mental health in older populations [80].
Although this study has notable strengths, including a large sample size and its international cross-sectional design, which provides a broader perspective on the variables studied, some limitations should be addressed. First, all data from the SHARE survey are self-reported, which introduces the risk of self-report bias. Additionally, individuals who agree to participate in research studies like SHARE are often more motivated and in better health than those who decline or are unable to participate. As a result, a significant portion of older adults with comorbidities may have been underrepresented in the sample. It is also important to note that although several associations identified in this study were statistically significant, these findings should be interpreted with caution due to the large sample size. In such contexts, even very small differences or associations can reach statistical significance, without necessarily reflecting meaningful or practically relevant effects.
In conclusion, our findings confirm that late-life depression continues to disproportionately affect older women across Europe, underscoring persistent gender disparities in mental health. Depressive symptoms in older adults are not only detrimental to psychological well-being but also negatively impact physical health; thus, recognising and addressing both physical and mental health needs is essential for improving overall well-being in aged populations. Our results also highlight the importance of social integration in later life, especially to reduce loneliness, with moderate involvement in grandchild care and in social participation, which emerge as potential protective factors for mental health.
From a clinical and public health perspective, the findings of this study highlight the importance of addressing multiple sociodemographic and contextual factors in the prevention and management of depressive symptoms among older adults in Europe. These results suggest that mental health strategies should go beyond medical treatment and incorporate broader social and environmental interventions. Understanding the prevalence and key determinants of depressive symptoms is vital for designing targeted interventions and effective health policies, ultimately contributing to the sustainability of Europe’s health and social care systems in the face of demographic ageing.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/jcm14155340/s1, Supplementary Materials and Methods; Table S1: Association between explanatory variables and depressive symptoms by age group; Table S2: Association between explanatory variables and depressive symptoms by European regions.
Author Contributions
Conceptualization, D.M., L.M. and E.C.; methodology, D.M. and L.M.; validation, D.M. and L.M.; formal analysis, D.M. and L.M.; investigation, D.M. and L.M.; writing—original draft preparation, D.M.; writing—review and editing, L.M., I.M., L.A., T.F., J.C. and E.C.; visualization, D.M. and L.M.; supervision, E.C.; project administration, E.C. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Ethical review and approval were waived because the study was conducted using publicly available data.
Informed Consent Statement
Individual consent was waived because the study was conducted using publicly available data.
Data Availability Statement
The data presented in this study are openly available in http://www.share-project.org/ (accessed on 27 February 2025) (SHARE Wave 9—https://doi.org/10.6103/SHARE.w9.900).
Acknowledgments
This paper uses data from SHARE Wave 9—https://doi.org/10.6103/SHARE.w9.900. The SHARE data collection was funded by the European Commission, DG RTD through FP5 (QLK6-CT-2001-00360), FP6 (SHARE-I3: RII-CT-2006-062193, COMPARE: CIT5-CT-2005-028857, SHARELIFE: CIT4-CT-2006-028812), FP7 (SHARE-PREP: GA N°211909, SHARE-LEAP: GA N°227822, SHARE M4: GA N°261982, DASISH: GA N°283646) and Horizon 2020 (SHARE-DEV3: GA N°676536, SHARE-COHESION: GA N°870628, SERISS: GA N°654221, SSHOC: GA N°823782, SHARE-COVID19: GA N°101015924) and by DG Employment, Social Affairs & Inclusion through VS 2015/0195, VS 2016/0135, VS 2018/0285, VS 2019/0332, VS 2020/0313, SHARE-EUCOV: GA N°101052589 and EUCOVII: GA N°101102412. Additional funding from the German Federal Ministry of Education and Research (01UW1301, 01UW1801, 01UW2202), the Max Planck Society for the Advancement of Science, the U.S. National Institute on Ageing (U01_AG09740-13S2, P01_AG005842, P01_AG08291, P30_AG12815, R21_AG025169, Y1-AG-4553-01, IAG_BSR06-11, OGHA_04-064, BSR12-04, R01_AG052527-02, R01_AG056329-02, R01_AG063944, HHSN271201300071C, RAG052527A) and from various national funding sources is gratefully acknowledged (see www.share-eric.eu). The authors acknowledge Teodora Figueiredo’s PhD grant 2024.02137.BD, financed by FCT.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| SHARE | Survey of Health, Ageing and Retirement in Europe |
| ADLs | Activities of Daily Living |
| iADLs | Instrumental Activities of Daily Living |
References
- GBD 2021 Europe Life Expectancy Collaborators. Changing life expectancy in European countries 1990–2021: A subanalysis of causes and risk factors from the Global Burden of Disease Study 2021. Lancet Public Health 2025, 10, e172–e188. [Google Scholar] [CrossRef] [PubMed]
- Athanasakis, K. ‘Inclusive’ health systems increase healthy life expectancy. Rural. Remote Health 2022, 22, 7014. [Google Scholar] [CrossRef] [PubMed]
- Choi, M.; Sempungu, J.K.; Lee, E.H.; Lee, Y.H. Living longer but in poor health: Healthcare system responses to ageing populations in industrialised countries based on the Findings from the Global Burden of Disease Study 2019. BMC Public Health 2024, 24, 576. [Google Scholar] [CrossRef]
- Deuschl, G.; Beghi, E.; Fazekas, F.; Varga, T.; Christoforidi, K.A.; Sipido, E.; Bassetti, C.L.; Vos, T.; Feigin, V.L. The burden of neurological diseases in Europe: An analysis for the Global Burden of Disease Study 2017. Lancet Public Health 2020, 5, e551–e567. [Google Scholar] [CrossRef]
- Prince, M.J.; Wu, F.; Guo, Y.; Gutierrez Robledo, L.M.; O’Donnell, M.; Sullivan, R.; Yusuf, S. The burden of disease in older people and implications for health policy and practice. Lancet 2015, 385, 549–562. [Google Scholar] [CrossRef]
- World Health Organization. World Mental Health Report: Transforming Mental Health for All; World Health Organization: Geneva, Switzerland, 2022. Available online: https://www.who.int/publications/i/item/9789240049338 (accessed on 6 May 2025).
- Cai, H.; Jin, Y.; Liu, R.; Zhang, Q.; Su, Z.; Ungvari, G.S.; Tang, Y.L.; Ng, C.H.; Li, X.H.; Xiang, Y.T. Global prevalence of depression in older adults: A systematic review and meta-analysis of epidemiological surveys. Asian J. Psychiatr. 2023, 80, 103417. [Google Scholar] [CrossRef]
- Wang, Y.; Liu, M.; Yang, F.; Chen, H.; Wang, Y.; Liu, J. The associations of socioeconomic status, social activities, and loneliness with depressive symptoms in adults aged 50 years and older across 24 countries: Findings from five prospective cohort studies. Lancet Healthy Longev. 2024, 5, 100618. [Google Scholar] [CrossRef]
- World Health Organization. Comprehensive Mental Health Action Plan 2013–2030; World Health Organization: Geneva, Switzerland, 2021. Available online: https://www.who.int/publications/i/item/9789240031029 (accessed on 6 May 2025).
- Morichi, V.; Dell’Aquila, G.; Trotta, F.; Belluigi, A.; Lattanzio, F.; Cherubini, A. Diagnosing and treating depression in older and oldest old. Curr. Pharm. Des. 2015, 21, 1690–1698. [Google Scholar] [CrossRef]
- Teresi, J.; Abrams, R.; Holmes, D.; Ramirez, M.; Eimicke, J. Prevalence of depression and depression recognition in nursing homes. Soc. Psychiatry Psychiatr. Epidemiol. 2001, 36, 613–620. [Google Scholar] [CrossRef] [PubMed]
- Aziz, R.; Steffens, D.C. What Are the Causes of Late-Life Depression? Psychiatr. Clin. N. Am. 2013, 36, 497–516. [Google Scholar] [CrossRef]
- Blazer, D.G. Depression and social support in late life: A clear but not obvious relationship. Aging Ment. Health 2005, 9, 497–499. [Google Scholar] [CrossRef]
- Zhu, S.; Kong, X.; Han, F.; Tian, H.; Sun, S.; Sun, Y.; Feng, W.; Wu, Y. Association between social isolation and depression: Evidence from longitudinal and Mendelian randomization analyses. J. Affect. Disord. 2024, 350, 182–187. [Google Scholar] [CrossRef]
- Zhang, Y.; Kuang, J.; Xin, Z.; Fang, J.; Song, R.; Yang, Y.; Song, P.; Wang, Y.; Wang, J. Loneliness, social isolation, depression and anxiety among the elderly in Shanghai: Findings from a longitudinal study. Arch. Gerontol. Geriatr. 2023, 110, 104980. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Rozelle, S.; Xu, Q.; Yu, N.; Zhou, T. Social Engagement and Elderly Health in China: Evidence from the China Health and Retirement Longitudinal Survey (CHARLS). Int. J. Environ. Res. Public Health 2019, 16, 278. [Google Scholar] [CrossRef] [PubMed]
- Wen, Z.; Peng, S.; Yang, L.; Wang, H.; Liao, X.; Liang, Q.; Zhang, X. Factors Associated with Social Isolation in Older Adults: A Systematic Review and Meta-Analysis. J. Am. Med. Dir. Assoc. 2023, 24, 322–330.e326. [Google Scholar] [CrossRef]
- Liu, B.C.-P.; Liu, R.H.-l. Early life adversities and discrimination, social activity, and loneliness among older adults in Europe: A moderated mediation analysis. Aging Ment. Health 2023, 27, 1627–1635. [Google Scholar] [CrossRef] [PubMed]
- Lin, S.A.; Xu, X.; Liu, Y.; Ai, B. Mechanism of the impacts of older adults social participation on their health. Front. Public Health 2024, 12, 1377305. [Google Scholar] [CrossRef]
- Soulières, M.; Charpentier, M. Are Older People Living Alone Socially Isolated? A Qualitative Study of Their Experiences. J. Gerontol. Soc. Work. 2022, 65, 664–677. [Google Scholar] [CrossRef]
- Santini, Z.I.; Jose, P.E.; Koyanagi, A.; Meilstrup, C.; Nielsen, L.; Madsen, K.R.; Hinrichsen, C.; Dunbar, R.I.M.; Koushede, V. The moderating role of social network size in the temporal association between formal social participation and mental health: A longitudinal analysis using two consecutive waves of the Survey of Health, Ageing and Retirement in Europe (SHARE). Soc. Psychiatry Psychiatr. Epidemiol. 2021, 56, 417–428. [Google Scholar] [CrossRef]
- Santini, Z.I.; Jose, P.E.; Koyanagi, A.; Meilstrup, C.; Nielsen, L.; Madsen, K.R.; Koushede, V. Formal social participation protects physical health through enhanced mental health: A longitudinal mediation analysis using three consecutive waves of the Survey of Health, Ageing and Retirement in Europe (SHARE). Soc. Sci. Med. 2020, 251, 112906. [Google Scholar] [CrossRef]
- Ku, L.J.; Stearns, S.C.; Van Houtven, C.H.; Lee, S.Y.; Dilworth-Anderson, P.; Konrad, T.R. Impact of caring for grandchildren on the health of grandparents in Taiwan. J. Gerontol. B Psycholo Sci. Soc. Sci. 2013, 68, 1009–1021. [Google Scholar] [CrossRef]
- Xu, H. Physical and mental health of Chinese grandparents caring for grandchildren and great-grandparents. Soc. Sci. Med. 2019, 229, 106–116. [Google Scholar] [CrossRef]
- Tsai, F.-J.; Motamed, S.; Rougemont, A. The protective effect of taking care of grandchildren on elders’ mental health? Associations between changing patterns of intergenerational exchanges and the reduction of elders’ loneliness and depression between 1993 and 2007 in Taiwan. BMC Public Health 2013, 13, 567. [Google Scholar] [CrossRef]
- Latikka, R.; Rubio-Hernández, R.; Lohan, E.S.; Rantala, J.; Nieto Fernández, F.; Laitinen, A.; Oksanen, A. Older Adults’ Loneliness, Social Isolation, and Physical Information and Communication Technology in the Era of Ambient Assisted Living: A Systematic Literature Review. J. Med. Internet Res. 2021, 23, e28022. [Google Scholar] [CrossRef]
- Chen, E.; Wood, D.; Ysseldyk, R. Online Social Networking and Mental Health among Older Adults: A Scoping Review. Can. J. Aging 2022, 41, 26–39. [Google Scholar] [CrossRef] [PubMed]
- Cotten, S.R.; Anderson, W.A.; McCullough, B.M. Impact of internet use on loneliness and contact with others among older adults: Cross-sectional analysis. J. Med. Internet Res. 2013, 15, e39. [Google Scholar] [CrossRef] [PubMed]
- Umoh, M.E.; Prichett, L.; Boyd, C.M.; Cudjoe, T.K.M. Impact of technology on social isolation: Longitudinal analysis from the National Health Aging Trends Study. J. Am. Geriatr. Soc. 2023, 71, 1117–1123. [Google Scholar] [CrossRef] [PubMed]
- Kusumota, L.; Diniz, M.A.A.; Ribeiro, R.M.; Silva, I.; Figueira, A.L.G.; Rodrigues, F.R.; Rodrigues, R.A.P. Impact of digital social media on the perception of loneliness and social isolation in older adults. Rev. Lat. Am. Enferm. 2022, 30, e3573. [Google Scholar] [CrossRef]
- Wilson, J.; Heinsch, M.; Betts, D.; Booth, D.; Kay-Lambkin, F. Barriers and facilitators to the use of e-health by older adults: A scoping review. BMC Public Health 2021, 21, 1556. [Google Scholar] [CrossRef]
- Arcury, T.A.; Sandberg, J.C.; Melius, K.P.; Quandt, S.A.; Leng, X.; Latulipe, C.; Miller, D.P., Jr.; Smith, D.A.; Bertoni, A.G. Older Adult Internet Use and eHealth Literacy. J. Appl. Gerontol. 2020, 39, 141–150. [Google Scholar] [CrossRef]
- Midão, L.; Pedreiro, E.; Pinho, M.S.; Dias, I.; Almada, M.; Garcia, K.R.; Rodrigues, L.S.; Christensen, C.; Pereira, P.T.; Bertram, M. Computer skills among the community-dwelling 55+ European population based on survey of health, ageing, and retirement in Europe. IJDLDC 2020, 11, 31–45. [Google Scholar] [CrossRef]
- Gyasi, R.M.; Phillips, D.R.; Asante, F.; Boateng, S. Physical activity and predictors of loneliness in community-dwelling older adults: The role of social connectedness. Geriatr. Ñurs 2021, 42, 592–598. [Google Scholar] [CrossRef]
- Shukla, A.; Harper, M.; Pedersen, E.; Goman, A.; Suen, J.J.; Price, C.; Applebaum, J.; Hoyer, M.; Lin, F.R.; Reed, N.S. Hearing Loss, Loneliness, and Social Isolation: A Systematic Review. Otolaryngol. Head. Neck Surg. 2020, 162, 622–633. [Google Scholar] [CrossRef]
- Hussain, B.; Mirza, M.; Baines, R.; Burns, L.; Stevens, S.; Asthana, S.; Chatterjee, A. Loneliness and social networks of older adults in rural communities: A narrative synthesis systematic review. Front. Public Health 2023, 11, 1113864. [Google Scholar] [CrossRef]
- Vo, T.T.; Phu-Duyen, T.T. Mental health around retirement: Evidence of Ashenfelter’s dip. Glob. Health Res. Policy 2023, 8, 35. [Google Scholar] [CrossRef] [PubMed]
- Börsch-Supan, A.; Brandt, M.; Hunkler, C.; Kneip, T.; Korbmacher, J.; Malter, F.; Schaan, B.; Stuck, S.; Zuber, S.; on behalf of the SHARE Central Coordination Team. Data Resource Profile: The Survey of Health, Ageing and Retirement in Europe (SHARE). Int. J. Epidemiol. 2013, 42, 992–1001. [Google Scholar] [CrossRef] [PubMed]
- Prince, M.J.; Reischies, F.; Beekman, A.T.F.; Fuhrer, R.; Jonker, C.; Kivela, S.L.; Lawlor, B.A.; Lobo, A.; Magnusson, H.; Fichter, M.; et al. Development of the EURO–D scale—A European Union initiative to compare symptoms of depression in 14 European centres. Br. J. Psychiatry 1999, 174, 330–338. [Google Scholar] [CrossRef] [PubMed]
- Bonanno, E.G.; Figueiredo, T.; Mimoso, I.F.; Morgado, M.I.; Carrilho, J.; Midão, L.; Costa, E. Polypharmacy Prevalence Among Older Adults Based on the Survey of Health, Ageing and Retirement in Europe: An Update. J. Clin. Med. 2025, 14, 1330. [Google Scholar] [CrossRef]
- Hyde, M.; Wiggins, R.D.; Higgs, P.; Blane, D.B. A measure of quality of life in early old age: The theory, development and properties of a needs satisfaction model (CASP-19). Aging Ment. Health 2003, 7, 186–194. [Google Scholar] [CrossRef]
- Kim, G.R.; Gopalakrishnan, N.; David, B.; Anne, P.; Sofia, M.; Galina, S.; Ruzena, K.; Andrzej, P.; Simone, C.; Martin, B.; et al. Psychometric properties and confirmatory factor analysis of the CASP-19, a measure of quality of life in early old age: The HAPIEE study. Aging Ment. Health 2015, 19, 595–609. [Google Scholar] [CrossRef]
- Hughes, M.E.; Waite, L.J.; Hawkley, L.C.; Cacioppo, J.T. A Short Scale for Measuring Loneliness in Large Surveys: Results From Two Population-Based Studies. Res. Aging 2004, 26, 655–672. [Google Scholar] [CrossRef] [PubMed]
- Russell, D.; Anne, P.L.; Ferguson, M.L. Developing a Measure of Loneliness. J. Pers. Assess. 1978, 42, 290–294. [Google Scholar] [CrossRef] [PubMed]
- Calonico, S.; Cattaneo, M.D.; Farrell, M.H.; Titiunik, R. Regression Discontinuity Designs Using Covariates. Rev. Econ. Stat. 2019, 101, 442–451. [Google Scholar] [CrossRef]
- Lee, K.M.; Robertson, D.S.; Jaki, T.; Emsley, R. The benefits of covariate adjustment for adaptive multi-arm designs. Stat. Methods Med. Res. 2022, 31, 2104–2121. [Google Scholar] [CrossRef]
- Hu, T.; Zhao, X.; Wu, M.; Li, Z.; Luo, L.; Yang, C.; Yang, F. Prevalence of depression in older adults: A systematic review and meta-analysis. Psychiatry Res. 2022, 311, 114511. [Google Scholar] [CrossRef]
- Núñez-Cortés, R.; Calatayud, J.; Andersen, L.L.; Villafañe, J.H.; Suso-Martí, L.; López-Bueno, R. Trends in depression in the European population aged 50 years and older by geographic region. Am. J. Epidemiol. 2025, kwaf027. [Google Scholar] [CrossRef]
- Oksuzyan, A.; Juel, K.; Vaupel, J.W.; Christensen, K. Men: Good health and high mortality. Sex. Differ. Health Aging Clin. Exp. Res. 2008, 20, 91–102. [Google Scholar] [CrossRef]
- Olsen, C.D.H.; Möller, S.; Ahrenfeldt, L.J. Sex differences in quality of life and depressive symptoms among middle-aged and elderly Europeans: Results from the SHARE survey. Aging Ment. Health 2023, 27, 35–42. [Google Scholar] [CrossRef]
- Paĺsson, S.P.; Ostling, S.; Skoog, I. The incidence of first-onset depression in a population followed from the age of 70 to 85. Psychol. Med. 2001, 31, 1159–1168. [Google Scholar] [CrossRef]
- Mo, Z.Y.; Qin, Z.Z.; Ye, J.J.; Hu, X.X.; Wang, R.; Zhao, Y.Y.; Zheng, P.; Lu, Q.S.; Li, Q.; Tang, X.Y. The long-term spatio-temporal trends in burden and attributable risk factors of major depressive disorder at global, regional and national levels during 1990-2019: A systematic analysis for GBD 2019. Epidemiol. Psychiatr. Sci. 2024, 33, e28. [Google Scholar] [CrossRef]
- Girgus, J.S.; Yang, K.; Ferri, C.V. The Gender Difference in Depression: Are Elderly Women at Greater Risk for Depression Than Elderly Men? Geriatrics 2017, 2, 35. [Google Scholar] [CrossRef] [PubMed]
- Arber, S.; Bote, M.; Meadows, R. Gender and socio-economic patterning of self-reported sleep problems in Britain. Soc. Sci. Med. 2009, 68, 281–289. [Google Scholar] [CrossRef] [PubMed]
- Roberts, R.E.; Shema, S.J.; Kaplan, G.A.; Strawbridge, W.J. Sleep complaints and depression in an aging cohort: A prospective perspective. Am. J. Psychiatry 2000, 157, 81–88. [Google Scholar] [CrossRef] [PubMed]
- Abdoli, N.; Salari, N.; Darvishi, N.; Jafarpour, S.; Solaymani, M.; Mohammadi, M.; Shohaimi, S. The global prevalence of major depressive disorder among the elderly: A systematic review and meta-analysis. Neurosci. Biobehav. Rev. 2022, 132, 1067–1073. [Google Scholar] [CrossRef]
- Carstensen, L.L. Socioemotional Selectivity Theory: The Role of Perceived Endings in Human Motivation. Gerontologist 2021, 61, 1188–1196. [Google Scholar] [CrossRef]
- Segerstrom, S.C.; Combs, H.L.; Winning, A.; Boehm, J.K.; Kubzansky, L.D. The happy survivor? Effects of differential mortality on life satisfaction in older age. Psychol. Aging 2016, 31, 340–345. [Google Scholar] [CrossRef]
- St John, P.D.; Montgomery, P.R. Marital Status, Partner Satisfaction, and Depressive Symptoms in Older Men and Women. Can. J. Psychiatry 2009, 54, 487–492. [Google Scholar] [CrossRef]
- Patten, S.B.; Wang, J.L.; Williams, J.V.; Currie, S.; Beck, C.A.; Maxwell, C.J.; El-Guebaly, N. Descriptive epidemiology of major depression in Canada. Can. J. Psychiatry 2006, 51, 84–90. [Google Scholar] [CrossRef]
- Bookwala, J. The role of marital quality in physical health during the mature years. J. Aging Health 2005, 17, 85–104. [Google Scholar] [CrossRef]
- Li, L.; Sun, W.; Luo, J.; Huang, H. Associations between education levels and prevalence of depressive symptoms: NHANES (2005–2018). J. Affect. Disord. 2022, 301, 360–367. [Google Scholar] [CrossRef]
- Mirowsky, J.; Ross, C.E. Education, Social Status, and Health, 1st ed.; Routledge: New York, NY, USA, 2003. [Google Scholar] [CrossRef]
- Avila, R.; Moscoso, M.A.A.; Ribeiz, S.; Arrais, J.; Jaluul, O.; Bottino, C.M.C. Influence of education and depressive symptoms on cognitive function in the elderly. Int. Psychogeriatri 2009, 21, 560–567. [Google Scholar] [CrossRef] [PubMed]
- Murray, S. Poverty and health. CMAJ 2006, 174, 923. [Google Scholar] [CrossRef]
- Luo, M.S.; Tak, C.E.W.; Li, L.W. The Longitudinal Associations between Physical Health and Mental Health among Older Adults. Aging Ment. Health 2020, 24, 1990–1998. [Google Scholar] [CrossRef]
- Li, D.; Su, M.; Guo, X.; Liu, B.; Zhang, T. The association between chronic disease and depression in middle-aged and elderly people: The moderating effect of health insurance and health service quality. Front. Public. Health 2023, 11, 935969. [Google Scholar] [CrossRef]
- Liu, H.; Ma, Y.; Lin, L.; Sun, Z.; Li, Z.; Jiang, X. Association between activities of daily living and depressive symptoms among older adults in China: Evidence from the CHARLS. Front. Public. Health 2023, 11, 1249208. [Google Scholar] [CrossRef]
- Ogliari, G.; Ryg, J.; Andersen-Ranberg, K.; Scheel-Hincke, L.L.; Collins, J.T.; Cowley, A.; Di Lorito, C.; Booth, V.; Smit, R.A.J.; Akyea, R.K.; et al. Association between pain intensity and depressive symptoms in community-dwelling adults: Longitudinal findings from the Survey of Health, Ageing and Retirement in Europe (SHARE). Eur. Geriatr. Med. 2023, 14, 1111–1124. [Google Scholar] [CrossRef]
- Pressman, S.D.; Jenkins, B.N.; Moskowitz, J.T. Positive Affect and Health: What Do We Know and Where Next Should We Go? Annu. Rev. Psychol. 2019, 70, 627–650. [Google Scholar] [CrossRef]
- Ribeiro, O.; Teixeira, L.; Araújo, L.; Rodríguez-Blázquez, C.; Calderón-Larrañaga, A.; Forjaz, M.J. Anxiety, Depression and Quality of Life in Older Adults: Trajectories of Influence across Age. Int. J. Environ. Res. Public Health 2020, 17, 9039. [Google Scholar] [CrossRef]
- Taylor, H.O.; Taylor, R.J.; Nguyen, A.W.; Chatters, L. Social Isolation, Depression, and Psychological Distress Among Older Adults. J. Aging Health 2018, 30, 229–246. [Google Scholar] [CrossRef] [PubMed]
- Ellwardt, L.; Wittek, R.P.M.; Hawkley, L.C.; Cacioppo, J.T. Social Network Characteristics and Their Associations with Stress in Older Adults: Closure and Balance in a Population-Based Sample. J. Gerontol. B Psychol. Sci. Soc. Sci. 2020, 75, 1573–1584. [Google Scholar] [CrossRef] [PubMed]
- Grundy, E.M.; Albala, C.; Allen, E.; Dangour, A.D.; Elbourne, D.; Uauy, R. Grandparenting and psychosocial health among older Chileans: A longitudinal analysis. Aging Ment. Health 2012, 16, 1047–1057. [Google Scholar] [CrossRef]
- Blustein, J.; Chan, S.; Guanais, F.C. Elevated depressive symptoms among caregiving grandparents. Health Serv. Res. 2004, 39, 1671–1689. [Google Scholar] [CrossRef]
- Hughes, M.E.; Waite, L.J.; LaPierre, T.A.; Luo, Y. All in the family: The impact of caring for grandchildren on grandparents’ health. J. Gerontol. B Psychol. Sci. Soc. Sci. 2007, 62, S108–S119. [Google Scholar] [CrossRef]
- Augner, C. Digital divide in elderly: Self-rated computer skills are associated with higher education, better cognitive abilities and increased mental health. Eur. J. Psychiatry 2022, 36, 176–181. [Google Scholar] [CrossRef]
- Wang, Q.; Huang, X.; Liu, M.; Wang, C.; Sun, Z.; Huang, C.; Tang, S. Prevalence and risk factors of depression among elderly people in nursing homes from 2012 to 2022: A systematic review and meta-analysis. Aging Ment. Health 2024, 28, 1569–1580. [Google Scholar] [CrossRef] [PubMed]
- Cornwell, E.Y.; Waite, L.J. Social disconnectedness, perceived isolation, and health among older adults. J. Health Soc. Behav. 2009, 50, 31–48. [Google Scholar] [CrossRef]
- Evans, G.W. The built environment and mental health. J. Urban. 2003, 80, 536–555. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).