Diabetes Is Associated with Lower In-Hospital Mortality in Patients Undergoing Surgical Repair for Aortic Aneurysm Rupture
Abstract
1. Introduction
2. Patients and Methods
2.1. Data Source
2.2. Study Population and Outcomes
2.3. Statistical Analysis
3. Results
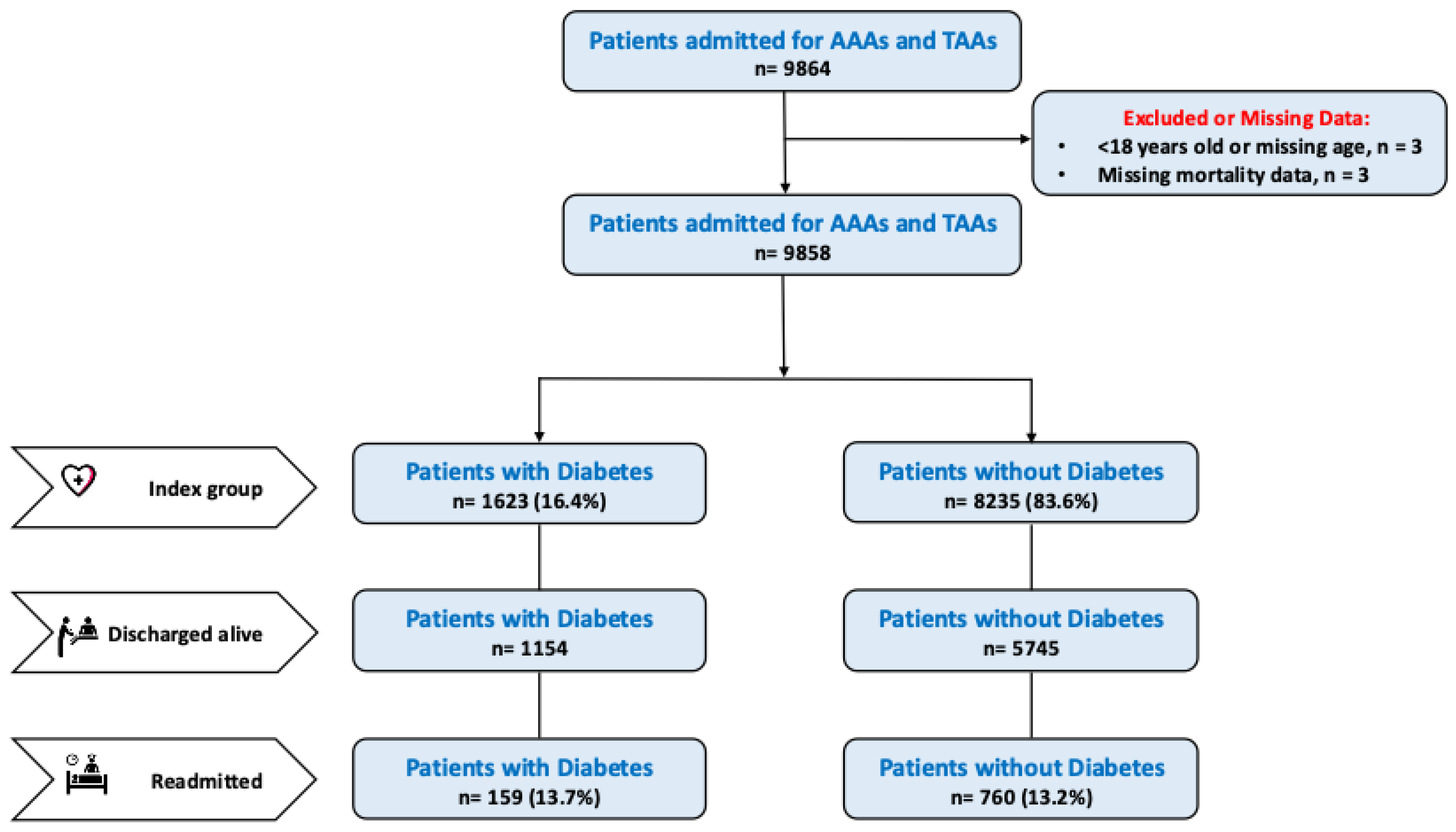
3.1. Study Population
3.2. In-Hospital Outcome
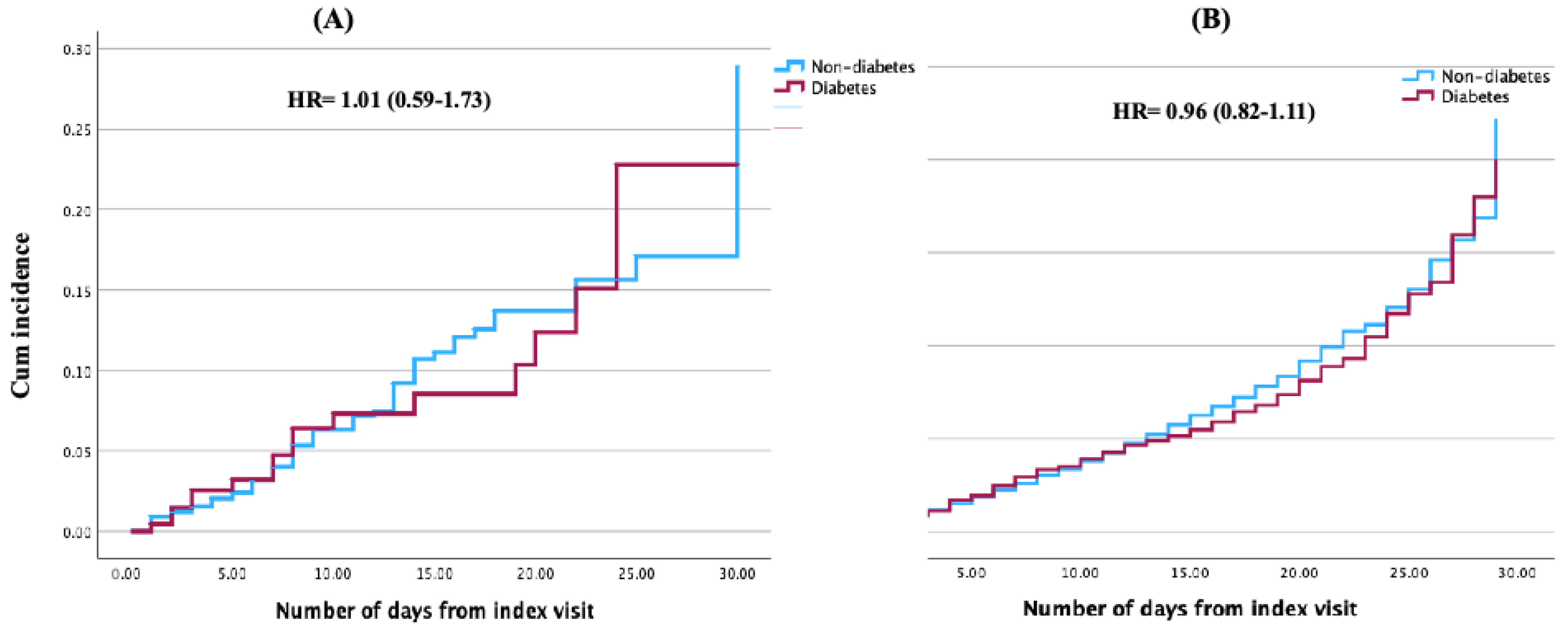
3.3. Readmission
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| AAA | Abdominal Aortic Aneurysm |
| AF | Atrial fibrillation |
| ARF | Acute renal failure |
| TAO | Thoracic Aortic Aneurysm |
| T2D | Type 2 diabetes |
| CVD | Cardiovascular disease |
| NRD | National Readmission Database |
References
- Haque, K.; Bhargava, P. Abdominal Aortic Aneurysm. Am. Fam. Physician 2022, 106, 165–172. [Google Scholar] [PubMed]
- Mathur, A.; Mohan, V.; Ameta, D.; Gaurav, B.; Haranahalli, P. Aortic aneurysm. J. Transl. Int. Med. 2016, 4, 35–41. [Google Scholar] [CrossRef] [PubMed]
- Isselbacher, E.M. Thoracic and abdominal aortic aneurysms. Circulation 2005, 111, 816–828. [Google Scholar] [CrossRef]
- Gouveia, E.M.R.; Silva Duarte, G.; Lopes, A.; Alves, M.; Caldeira, D.; Fernandes, E.F.R.; Mendes Pedro, L. Incidence and Prevalence of Thoracic Aortic Aneurysms: A Systematic Review and Meta-Analysis of Population-Based Studies. Semin. Thorac. Cardiovasc. Surg. 2022, 34, 1–16. [Google Scholar] [CrossRef]
- Huang, D.; Refaat, M.; Mohammedi, K.; Jayyousi, A.; Al Suwaidi, J.; Abi Khalil, C. Macrovascular Complications in Patients with Diabetes and Prediabetes. Biomed. Res. Int. 2017, 2017, 7839101. [Google Scholar] [CrossRef]
- Raffort, J.; Lareyre, F.; Clément, M.; Hassen-Khodja, R.; Chinetti, G.; Mallat, Z. Diabetes and aortic aneurysm: Current state of the art. Cardiovasc. Res. 2018, 114, 1702–1713. [Google Scholar] [CrossRef] [PubMed]
- Anagnostakos, J.; Lal, B.K. Abdominal aortic aneurysms. Prog. Cardiovasc. Dis. 2021, 65, 34–43. [Google Scholar] [CrossRef]
- Agana, D.F.G.; Striley, C.W.; Cook, R.L.; Cruz-Almeida, Y.; Carek, P.J.; Salemi, J.L. A Novel Approach to Characterizing Readmission Patterns Following Hospitalization for Ambulatory Care-Sensitive Conditions. J. Gen. Intern. Med. 2020, 35, 1060–1068. [Google Scholar] [CrossRef]
- Introduction to the Hcup Nationwide Readmissions Database (Nrd). 2020. Available online: https://hcup-us.ahrq.gov/db/nation/nrd/Introduction_NRD_2020.jsp#:~:text=These%20States%20are%20geographically%20dispersed,for%20data%20years%202010%2D2020 (accessed on 17 June 2024).
- Chaudhry, H.; Dargham, S.; Jayyousi, A.; Al Suwaidi, J.; Abi Khalil, C. Diabetes does not increase in-hospital or short-term mortality in patients undergoing surgical repair for type A aortic dissection: Insight from the national readmission database. Cardiovasc. Diabetol. 2024, 23, 436. [Google Scholar] [CrossRef]
- Takagi, H.; Umemoto, T.; Group, A. Negative association of diabetes with rupture of abdominal aortic aneurysm. Diab Vasc. Dis. Res. 2016, 13, 341–347. [Google Scholar] [CrossRef]
- Theivacumar, N.S.; Stephenson, M.A.; Mistry, H.; Valenti, D. Diabetes mellitus and aortic aneurysm rupture: A favorable association? Vasc. Endovasc. Surg. 2014, 48, 45–50. [Google Scholar] [CrossRef] [PubMed]
- Raffort, J.; Lareyre, F.; Fabre, R.; Mallat, Z.; Pradier, C.; Bailly, L. Nationwide study in France investigating the impact of diabetes on mortality in patients undergoing abdominal aortic aneurysm repair. Sci. Rep. 2021, 11, 19395. [Google Scholar] [CrossRef] [PubMed]
- Taimour, S.; Franzen, S.; Zarrouk, M.; Acosta, S.; Nilsson, P.; Miftaraj, M.; Eliasson, B.; Svensson, A.M.; Gottsater, A. Nationwide comparison of long-term survival and cardiovascular morbidity after acute aortic aneurysm repair in patients with and without type 2 diabetes. J. Vasc. Surg. 2020, 71, 30–38.e3. [Google Scholar] [CrossRef] [PubMed]
- Malayala, S.V.; Raza, A.; Vanaparthy, R. Gender-Based Differences in Abdominal Aortic Aneurysm Rupture: A Retrospective Study. J. Clin. Med. Res. 2020, 12, 794–802. [Google Scholar] [CrossRef]
- Kim, E.J.; Ha, K.H.; Kim, D.J.; Choi, Y.H. Diabetes and the Risk of Infection: A National Cohort Study. Diabetes Metab. J. 2019, 43, 804–814. [Google Scholar] [CrossRef]
- Huang, Z.; Su, H.; Zhang, T.; Li, Y. Double-edged sword of diabetes mellitus for abdominal aortic aneurysm. Front. Endocrinol. 2022, 13, 1095608. [Google Scholar] [CrossRef]
- Le, M.T.; Jamrozik, K.; Davis, T.M.; Norman, P.E. Negative association between infra-renal aortic diameter and glycaemia: The Health in Men Study. Eur. J. Vasc. Endovasc. Surg. 2007, 33, 599–604. [Google Scholar] [CrossRef]
- Kristensen, K.L.; Dahl, M.; Rasmussen, L.M.; Lindholt, J.S. Glycated Hemoglobin Is Associated with the Growth Rate of Abdominal Aortic Aneurysms: A Substudy from the VIVA (Viborg Vascular) Randomized Screening Trial. Arterioscler. Thromb. Vasc. Biol. 2017, 37, 730–736. [Google Scholar] [CrossRef]
- Shanmuganathan, G.; Agrawal, D.K. Diabetes and Abdominal Aortic Aneurysm: Is the Protective Effect on AAA Due to Antidiabetic Medications Alone, Due to the Disease Alone, or Both? Arch. Intern. Med. Res. 2024, 7, 104–113. [Google Scholar] [CrossRef]
- Unosson, J.; Wågsäter, D.; Bjarnegård, N.; De Basso, R.; Welander, M.; Mani, K.; Gottsäter, A.; Wanhainen, A. Metformin Prescription Associated with Reduced Abdominal Aortic Aneurysm Growth Rate and Reduced Chemokine Expression in a Swedish Cohort. Ann. Vasc. Surg. 2021, 70, 425–433. [Google Scholar] [CrossRef]
- Ortega, R.; Collado, A.; Selles, F.; Gonzalez-Navarro, H.; Sanz, M.J.; Real, J.T.; Piqueras, L. SGLT-2 (Sodium-Glucose Cotransporter 2) Inhibition Reduces Ang II (Angiotensin II)-Induced Dissecting Abdominal Aortic Aneurysm in ApoE (Apolipoprotein E) Knockout Mice. Arterioscler. Thromb. Vasc. Biol. 2019, 39, 1614–1628. [Google Scholar] [CrossRef] [PubMed]
- Yu, J.; Morimoto, K.; Bao, W.; Yu, Z.; Okita, Y.; Okada, K. Glucagon-like peptide-1 prevented abdominal aortic aneurysm development in rats. Surg. Today 2016, 46, 1099–1107. [Google Scholar] [CrossRef] [PubMed]
- Charolidi, N.; Pirianov, G.; Torsney, E.; Pearce, S.; Laing, K.; Nohturfft, A.; Cockerill, G.W. Pioglitazone Identifies a New Target for Aneurysm Treatment: Role of Egr1 in an Experimental Murine Model of Aortic Aneurysm. J. Vasc. Res. 2015, 52, 81–93. [Google Scholar] [CrossRef] [PubMed]
- Sajithlal, G.B.; Chithra, P.; Chandrakasan, G. Advanced glycation end products induce crosslinking of collagen in vitro. Biochim. Biophys. Acta (BBA)-Mol. Basis Dis. 1998, 1407, 215–224. [Google Scholar] [CrossRef]
- Singh, V.P.; Bali, A.; Singh, N.; Jaggi, A.S. Advanced glycation end products and diabetic complications. Korean J. Physiol. Pharmacol. 2014, 18, 1–14. [Google Scholar] [CrossRef]
- Sticchi, A.; Cereda, A.; Toselli, M.; Esposito, A.; Palmisano, A.; Vignale, D.; Nicoletti, V.; Leone, R.; Gnasso, C.; Monello, A.; et al. Diabetes and mortality in patients with COVID-19: Are we missing the link? Anatol. J. Cardiol. 2021, 25, 376–379. [Google Scholar] [CrossRef]
- Antoniou, G.A.; Antoniou, S.A.; Torella, F. Editor’s Choice—Endovascular vs. Open Repair for Abdominal Aortic Aneurysm: Systematic Review and Meta-analysis of Updated Peri-operative and Long Term Data of Randomised Controlled Trials. Eur. J. Vasc. Endovasc. Surg. 2020, 59, 385–397. [Google Scholar] [CrossRef]
- Pandit, V.; Nelson, P.; Horst, V.; Hanna, K.; Jennings, W.; Kempe, K.; Kim, H. Racial and Ethnic Disparities in Patients with Ruptured Abdominal Aortic Aneurysm. J. Vasc. Surg. 2020, 72, e85. [Google Scholar] [CrossRef]
- Chen, S.W.; Chan, Y.H.; Lin, C.P.; Wu, V.C.; Cheng, Y.T.; Chen, D.Y.; Chang, S.H.; Hung, K.C.; Chu, P.H.; Chou, A.H. Association of Long-Term Use of Antihypertensive Medications with Late Outcomes Among Patients with Aortic Dissection. JAMA Netw. Open 2021, 4, e210469. [Google Scholar] [CrossRef]
- Alshaikh, H.N.; Canner, J.K.; Malas, M. Effect of Beta Blockers on Mortality After Open Repair of Abdominal Aortic Aneurysm. Ann. Surg. 2018, 267, 1185–1190. [Google Scholar] [CrossRef]
|
Diabetes n = 1623 |
Non-Diabetes n = 8235 | p-Value | |
|---|---|---|---|
| Age | |||
| <55 | 38 (2.3%) | 371 (4.5%) | <0.001 |
| 55–64 | 248 (15.3%) | 1291 (15.7%) | |
| 65–74 | 517 (31.9%) | 2493 (30.3%) | |
| 75–84 | 562 (34.6%) | 2396 (29.1%) | |
| >84 | 258 (15.9%) | 1684 (20.4%) | |
| Mean (SD) | 74.2 (9.8) | 73.8 (11.2) | 0.179 |
| Sex | |||
| Male | 1168 (72.1%) | 5711 (69.4%) | 0.036 |
| Income | |||
| Low | 430 (26.8%) | 2062 (25.4%) | 0.527 |
| Low-Mid | 464 (28.9%) | 2295 (28.3%) | |
| High-Mid | 401 (25.0%) | 2127 (26.2%) | |
| High | 311 (19.4%) | 1624 (20.0%) | |
| Comorbidities | |||
| Obesity | 312 (19.2%) | 910 (11.1%) | <0.001 |
| Hypertension | 1437 (88.5%) | 6109 (74.2%) | <0.001 |
| Smoking | 502 (30.9%) | 2036 (24.7%) | <0.001 |
| Dyslipidemia | 892 (55.0%) | 3084 (37.4%) | <0.001 |
| VHD | 120 (7.4%) | 629 (7.6%) | 0.734 |
| CKD | 535 (33.0%) | 1723 (20.9%) | <0.001 |
| CAD | 9 (0.6%) | 16 (0.2%) | 0.008 |
| Location of Aneurysm | |||
| Abdominal Aorta | 1331 (82.0%) | 6770 (83.2%) | 0.849 |
| Thoracic Aorta | 292 (18.0%) | 1465 (17.8%) | |
| Length of Stay (days) | 6 (2–12) | 5 (1–10) | <0.001 |
| Number of Events | |||||
|---|---|---|---|---|---|
| Outcomes | Diabetes | Non-Diabetes | Unadjusted OR (95% CI) | Adjusted OR (95% CI) | p-Value |
| Mortality | 469 (28.9%) | 2940 (35.7%) | 0.73 (0.65–0.82) | 0.85 (0.75–0.96) | <0.001 |
| Atrial Fibrillation | 483 (29.8%) | 1887 (22.9%) | 1.43 (1.26–1.60) | 1.25 (1.11–1.42) | <0.001 |
| Acute Renal Failure | 725 (44.7%) | 3301 (40.1%) | 1.21 (1.08–1.34) | 1.17 (1.05–1.32) | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chaudhry, H.; Dargham, S.; Mahfoud, Z.; Jayyousi, A.; Al Suwaidi, J.; Abi Khalil, C. Diabetes Is Associated with Lower In-Hospital Mortality in Patients Undergoing Surgical Repair for Aortic Aneurysm Rupture. J. Clin. Med. 2025, 14, 4370. https://doi.org/10.3390/jcm14124370
Chaudhry H, Dargham S, Mahfoud Z, Jayyousi A, Al Suwaidi J, Abi Khalil C. Diabetes Is Associated with Lower In-Hospital Mortality in Patients Undergoing Surgical Repair for Aortic Aneurysm Rupture. Journal of Clinical Medicine. 2025; 14(12):4370. https://doi.org/10.3390/jcm14124370
Chicago/Turabian StyleChaudhry, Hamza, Soha Dargham, Ziyad Mahfoud, Amin Jayyousi, Jassim Al Suwaidi, and Charbel Abi Khalil. 2025. "Diabetes Is Associated with Lower In-Hospital Mortality in Patients Undergoing Surgical Repair for Aortic Aneurysm Rupture" Journal of Clinical Medicine 14, no. 12: 4370. https://doi.org/10.3390/jcm14124370
APA StyleChaudhry, H., Dargham, S., Mahfoud, Z., Jayyousi, A., Al Suwaidi, J., & Abi Khalil, C. (2025). Diabetes Is Associated with Lower In-Hospital Mortality in Patients Undergoing Surgical Repair for Aortic Aneurysm Rupture. Journal of Clinical Medicine, 14(12), 4370. https://doi.org/10.3390/jcm14124370





