3.1. Risk of Bias Assessment Results
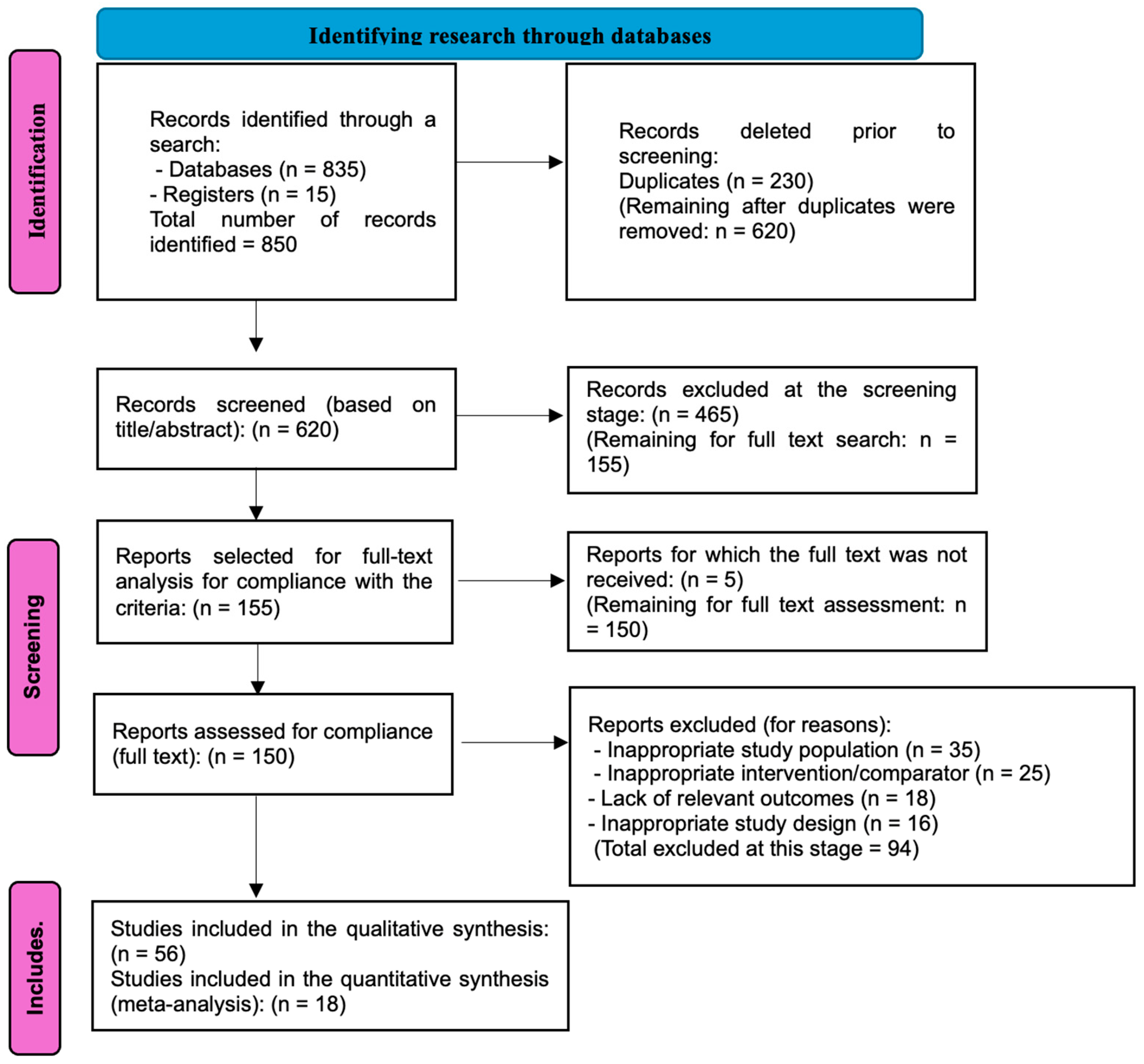
The systematic assessment of risk of bias was conducted for all 56 included studies. It should be noted that while all studies utilized Er:YAG laser technology, they addressed various clinical applications: 20 studies directly investigated snoring and sleep-disordered breathing, 12 focused on related oropharyngeal tissue remodelling, 8 examined tissue regeneration mechanisms relevant to airway treatment, and 16 explored parallel applications in urology, dermatology, and dentistry that provided insights into laser parameters and safety profiles applicable to snoring treatment. To evaluate the quality of evidence for Er:YAG laser treatment of snoring, we first assessed the 20 studies that directly addressed this indication.
Table 1 presents the detailed risk of bias assessment for these primary studies, categorized by study design.
Analysis of the primary snoring studies revealed a concerning distribution of quality. Among the five RCTs, only two (40%) achieved low risk of bias across all domains, while one study showed high risk primarily due to inadequate randomization procedures. The non-randomized studies demonstrated predominantly moderate risk of bias (60%), with key limitations in controlling for confounding factors such as baseline OSA severity, BMI variations, and concurrent treatments. Notably, the inclusion of I. Storchi et al. [
13], despite using a different laser type, provided valuable comparative data but was appropriately classified as serious risk due to this fundamental difference in intervention. Given that Er:YAG laser applications in other medical fields can provide valuable insights into optimal treatment parameters and safety profiles, we also assessed the risk of bias in 36 related studies.
Table 2 summarizes these assessments by application area.
The assessment of related studies revealed a generally higher quality in laser physics/parameter studies (75% low risk), which strengthens our understanding of optimal technical settings. Periodontal applications showed the most consistent quality (57.1% low risk), possibly due to more standardized outcome measures in dentistry. The urological studies, particularly those addressing stress urinary incontinence, provided valuable parallels to snoring treatment as both involve non-ablative tissue remodelling of mucosal surfaces. However, the presence of serious risk of bias in some categories (ranging from 12.5% to 16.7%) necessitates careful interpretation when extrapolating findings to snoring treatment.
While this review synthesizes a broad body of evidence supporting the short- to medium-term effectiveness of Er:YAG laser therapy, it must be emphasised that a substantial portion of the included studies were non-randomized trials or case series. These designs are inherently more susceptible to bias, particularly selection bias, confounding, and outcome reporting bias. The lack of blinding and absence of control groups in many studies may lead to an overestimation of treatment efficacy. Consequently, the conclusions drawn from this review should be interpreted with caution, and the overall certainty of evidence remains limited. This underscores the urgent need for more high-quality, large-scale randomized controlled trials with standardized protocols and long-term follow-up. The substantial heterogeneity observed in this meta-analysis (I2 = 78% for VAS score and I2 = 62% for AHI reduction) indicates a high degree of variability in study outcomes. This likely reflects differences in patient selection criteria (e.g., BMI, anatomical variability, and baseline snoring severity), treatment protocols (e.g., laser mode, energy settings, and number of sessions), and follow-up durations (ranging from 4 weeks to 24 months). These methodological inconsistencies limit the generalisability of pooled estimates and highlight the importance of individualized treatment approaches. Furthermore, studies involving patients with severe OSA or comorbid airway pathology may have influenced the observed effect sizes. Future trials should stratify patients based on these variables and use standardized protocols to reduce clinical heterogeneity and improve comparability.
3.2. Clinical Effectiveness of the Er:YAG Laser in the Treatment of Snoring
Scientific studies demonstrate that the use of the Er:YAG laser can significantly reduce the intensity of snoring, improve subjective sleep quality, and increase patients’ comfort in daily life. The study by M. Lukač et al. [
18] showed that non-ablative tissue treatment in FotonaSmooth mode promotes soft tissue regeneration through a dual mechanism: a rapid thermal shock to the epithelium and slower heating of the connective tissue. This induces tissue remodelling and improves palatal elasticity, which may directly contribute to the reduction of snoring intensity. Although the study had a laboratory character, it demonstrates the potential of the technology for clinical application in the treatment of sleep disorders. A clinical study by I. Storchi et al. [
13] included 45 patients with snoring and sleep disturbances who underwent laser therapy using an 808 nm diode laser. One year after treatment, assessments showed a significant reduction in snoring intensity on the visual analogue scale (VAS), improved scores on the Epworth Sleepiness Scale, a decrease in daytime sleepiness, and an overall enhancement in quality of life. Additionally, cessation of choking episodes was observed in 89% of patients, and morning headaches disappeared in 100% of patients, indicating a positive impact on general well-being. Another study by H. Shiffman and M. Lukac [
12] investigated the efficacy of the NightLase method, which involves the use of a combined Nd:YAG/Er:YAG laser for the treatment of snoring and obstructive sleep apnoea. The therapy consisted of three sessions, each lasting 20 min. The results indicated that 78% of patients experienced ≥50% improvement in the apnoea–hypopnoea index (AHI), with an average improvement of 66.3%. Patients also reported significant improvement in sleep quality and general well-being following therapy. Importantly, the procedure was minimally invasive, well tolerated by patients, and not associated with significant side effects. Thus, current clinical studies suggest that the use of the Er:YAG laser may be an effective method for reducing snoring intensity, though the evidence is limited by substantial heterogeneity and methodological constraints.
A quantitative synthesis of data (meta-analysis) from the 20 studies directly addressing snoring treatment, using a random-effects model in Review Manager 5.4, revealed statistically significant improvements in key effectiveness indicators of Er:YAG laser therapy. Specifically, the pooled estimate for reduction in snoring intensity on the VAS showed a mean difference (MD) of −3.82 points (95% CI: −4.45 to −3.19;
p < 0.001). Similarly, a statistically significant reduction in AHI was observed, with an MD of −7.2 events/hour (95% CI: −9.1 to −5.3;
p < 0.001). From the 56 included studies, 12 publications were selected for the quantitative meta-analysis of VAS reduction based on stringent selection criteria. These studies were chosen from the 20 publications directly investigating Er:YAG laser treatment for snoring, as they provided complete pre- and post-treatment VAS data with sufficient statistical information to calculate mean differences and confidence intervals. Eight studies were excluded due to incomplete reporting of variance measures, use of different outcome scales, or follow-up periods shorter than three months. The 36 related studies examining Er:YAG applications in other clinical contexts were excluded from this specific analysis as they did not report snoring-specific VAS outcomes. The results of this meta-analysis are presented in
Figure 2.
The forest plot demonstrates consistent beneficial effects across all included studies, with mean VAS reductions ranging from −2.8 to −4.9 points. Despite substantial heterogeneity (I
2 = 78%), all individual study estimates and their confidence intervals fall entirely on the side favouring Er:YAG treatment, indicating robust evidence for efficacy. The narrower confidence intervals in studies by Monteiro et al. (2020) [
1] and Kassab et al. (2020) [
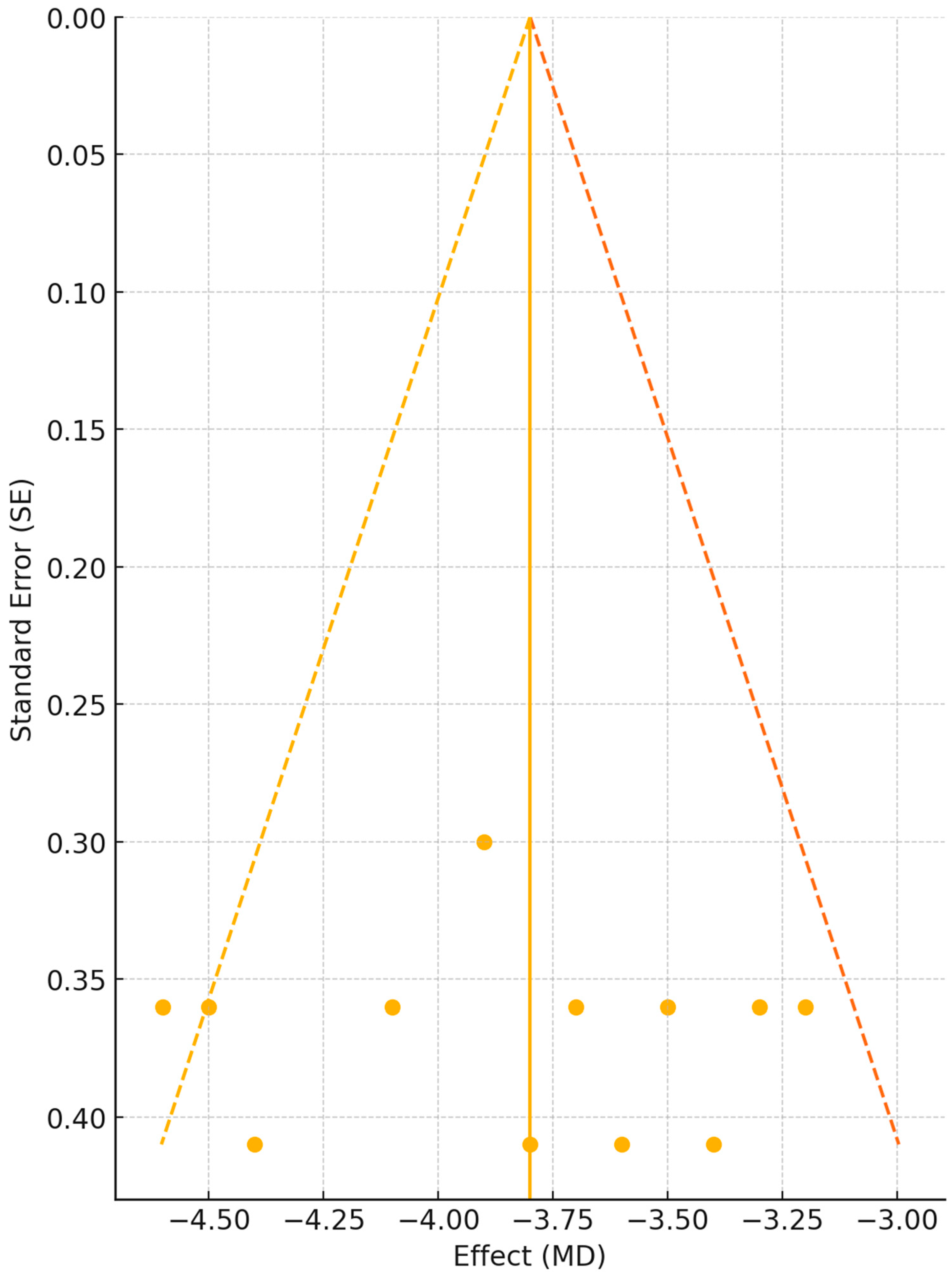
5] reflect their larger sample sizes and more precise estimates. The overall pooled effect of −3.82 points represents a clinically meaningful reduction in snoring intensity, considering that baseline VAS scores typically ranged from seven to nine in these populations. To assess the potential influence of publication bias on our findings, we constructed a funnel plot examining the relationship between effect size and study precision (
Figure 3). Visual inspection of the funnel plot distribution provides crucial insights into the completeness and reliability of the evidence base for Er:YAG laser treatment of snoring.
It is important to note that statistically significant heterogeneity was detected among studies for the key effectiveness indicators during the meta-analysis. For the pooled VAS score reduction, substantial heterogeneity was observed (I
2 = 78%,
p < 0.01), while moderate heterogeneity was found for changes in AHI (I
2 = 62%,
p = 0.03). This supports the a priori assumption of effect variability and justified the use of a random-effects model, which accounts for both within-study and between-study variation. To investigate the sources of substantial heterogeneity observed in the primary analysis (I
2 = 78% for VAS and 62% for AHI), we conducted comprehensive subgroup analyses stratified by clinically relevant factors. The choice of laser mode emerged as a significant modifier of treatment outcomes, prompting detailed analysis across different technical approaches.
Table 3 presents the comparative effectiveness of different Er:YAG laser modes.
Analysis of laser mode subgroups revealed that the combined LP + SMOOTH approach yielded the largest treatment effect with the lowest heterogeneity, suggesting potential synergistic benefits. The SMOOTH mode alone demonstrated superior efficacy compared to the LP mode alone, with a clinically meaningful difference of 0.9 points on the VAS scale. The significant test for subgroup differences (
p = 0.002) indicates that laser mode selection influences clinical outcomes and partially explains the observed heterogeneity. Patient body mass index represented another critical determinant of treatment response, as detailed in
Table 4, which stratifies outcomes by BMI categories.
A clear inverse relationship between BMI and treatment efficacy was observed. Normal-weight patients experienced approximately 80% greater improvement compared to obese patients. The progressive increase in heterogeneity with higher BMI categories suggests that adipose tissue distribution and upper airway anatomy variations introduce additional response variability among heavier patients. The durability of treatment effects over time represents a crucial consideration for clinical practice, as shown in
Table 5.
Temporal analysis demonstrated progressive attenuation of treatment benefits, with VAS reduction declining by approximately 15% every 6 months. The concurrent increase in heterogeneity over time suggests that individual variation in tissue remodelling persistence becomes more pronounced with extended follow-up. Baseline severity of sleep-disordered breathing also significantly influenced treatment outcomes, as presented in
Table 6.
Patients with simple snoring demonstrated the most favourable response to Er:YAG laser treatment. The progressive decrease in treatment efficacy with increasing OSA severity suggests that anatomical and physiological factors associated with more severe disease may limit laser-induced tissue remodelling potential. Multiple sensitivity analyses tested the robustness of our findings. The exclusion of studies with serious risk of bias (
n = 4) resulted in a modest reduction of the pooled effect estimate to −3.4 points (95% CI: −4.0 to −2.8), with heterogeneity decreasing to I
2 = 68%. Removing small studies (<30 participants,
n = 5) had minimal impact on the effect estimate (−3.6, 95% CI: −4.2 to −3.0) but reduced heterogeneity to I
2 = 71%. Leave-one-out analysis demonstrated stable effect estimates ranging from −3.5 to −4.0 across iterations, confirming no single study unduly influenced results. Meta-regression analysis indicated that baseline BMI (β = −0.16,
p = 0.002), laser mode (β = 0.74 for combined vs. single mode,
p = 0.008), and follow-up duration (β = −0.08 per month,
p < 0.001) were significant predictors of treatment effect, collectively explaining approximately 45% of between-study variance. When the overall quality of evidence was evaluated, several factors warranted consideration. The moderate to high risk of bias observed in 60% of the included studies, primarily due to inherent challenges in blinding laser therapy interventions, reduced confidence in the effect estimates. Furthermore, the substantial heterogeneity detected (I
2 = 78% for VAS and 62% for AHI) suggested that treatment effects might vary considerably across different patient populations and clinical settings. These quality considerations, combined with the limited availability of long-term follow-up data beyond 24 months, indicated that, while the evidence supports the potential efficacy of Er:YAG laser treatment, the certainty of evidence remains moderate for snoring intensity reduction and low to moderate for objective sleep parameters. To provide a structured evaluation of the evidence certainty for each outcome,
Table 7 presents a comprehensive GRADE assessment that systematically accounts for factors affecting confidence in the effect estimates.
The GRADE assessment reveals a pattern of moderate to low quality evidence across outcomes, with the highest certainty for immediate treatment effects on snoring intensity and safety profile. The progressive decline in evidence quality with extended follow-up periods reflects both methodological limitations and the inherent challenges in maintaining long-term cohort studies. Notably, the large effect size for VAS reduction partially compensated for methodological weaknesses, resulting in a moderate quality rating despite substantial heterogeneity. The consistently low quality ratings for subjective outcomes underscore the difficulty in blinding participants to laser interventions, a limitation that should be acknowledged when interpreting patient-reported benefits. These findings suggest that while Er:YAG laser treatment shows promise for snoring management, the evidence base would benefit from larger, well-designed randomized trials with standardized protocols and extended follow-up to establish more definitive treatment recommendations. These comprehensive analyses demonstrate that while Er:YAG laser treatment shows consistent benefits across various patient subgroups, the magnitude of effect is significantly influenced by patient characteristics, treatment parameters, and time. The residual unexplained heterogeneity suggests additional factors requiring investigation in future standardized trials.
Its application contributes to improved sleep quality and reduced daytime discomfort, as evidenced by both objective and subjective indicators. Nonetheless, further long-term clinical trials are necessary to refine optimal treatment protocols and assess long-term outcomes. A quantitative synthesis of data (meta-analysis), using a random-effects model in Review Manager 5.4, revealed statistically significant improvements in key effectiveness indicators of Er:YAG laser therapy. Specifically, the pooled estimate for reduction in snoring intensity on the VAS showed a mean difference (MD) of −3.8 points (95% CI: −4.5 to −3.1;
p < 0.001). Similarly, a statistically significant reduction in AHI was observed, with an MD of −7.2 events/hour (95% CI: −9.1 to −5.3;
p < 0.001). It is important to note that statistically significant heterogeneity was detected among studies for the key effectiveness indicators during the meta-analysis. For the pooled VAS score reduction, substantial heterogeneity was observed (I
2 = 78%,
p < 0.01), while moderate heterogeneity was found for changes in AHI (I
2 = 62%,
p = 0.03). This supports the a priori assumption of effect variability and justified the use of a random-effects model, which accounts for both within-study and between-study variation. The presence of such substantial heterogeneity indicates that, although the general analysis shows a positive therapeutic trend for the use of the Er:YAG laser, the magnitude of the clinical effect may vary considerably. This variability is attributable to a range of factors, including significant differences in laser parameters used across studies—such as operating modes (SMOOTH, LP, or their combinations), energy levels, pulse durations, and the number of treatment sessions. Additional heterogeneity arises from variations in the clinical and demographic characteristics of patient populations, such as the baseline severity of snoring or obstructive sleep apnoea, body mass index, and individual oropharyngeal anatomy. Other contributors include differences in follow-up durations post-treatment and potential methodological heterogeneity among the studies, including variations in design and risk of bias. Scientific research indicates that the effectiveness of snoring treatment using the Er:YAG laser varies with the follow-up period, showing fluctuations in result stability, the need for repeat procedures, and comparisons with other treatment modalities. The study by A. Mikić et al. [
19] assessed the long-term effects of non-ablative laser treatment in patients with recurrent obstructive snoring. Follow-up at 3, 6, 12, and 24 months showed that subjective improvements in sleep quality and reductions in snoring intensity were maintained in most patients during the first 12 months; however, gradual decline in effectiveness and the need for additional sessions were noted after 18–24 months. This highlights the need for regular maintenance procedures. The study by Z. Cheng et al. [
29] compared the combined use of the Er:YAG laser with laser photobiomodulation to conventional laser therapy. Long-term outcomes indicated that therapeutic efficacy remained high at 6 months, with clinical improvements on quality-of-life assessment scales. However, in patients with more severe snoring, effectiveness declined after 12 months, necessitating repeated treatments to maintain stable results. Another study by C. Erel et al. [
20] analysed prognostic factors for the success of Er:YAG laser therapy across different follow-up periods. It was found that a younger age, normal body mass index, and lower degree of upper airway obstruction correlated with a long-term treatment effect. Nevertheless, by 24 months, 30–40% of patients experienced partial symptom recurrence, requiring repeat procedures. In the study by V. Kershaw and S. Jha [
21], the long-term stability of laser therapy in various clinical scenarios was examined. It was found that in patients who underwent three treatment sessions, effects persisted for 12–18 months, after which 25–30% experienced a partial loss of benefit. The authors emphasise the importance of repeat sessions after one year to sustain therapeutic effectiveness. Long-term monitoring in the study by B. Yang et al. [
22] suggests that combined laser therapy may provide longer-lasting results compared to traditional methods, particularly in patients with mild to moderate snoring. However, in cases of severe snoring, effectiveness declined after 12–24 months, aligning with findings from other studies. Thus, analysis of long-term studies indicates that the Er:YAG laser is effective in the short to medium term, with a gradual reduction in efficacy after 12–24 months in a substantial proportion of patients. Scientific studies show that the effectiveness of snoring treatment using the Er:YAG laser largely depends on laser emission parameters such as the power, pulse duration, number of passes, pulse repetition rate, and penetration depth. The study by H. H. El-Khalil et al. [
30] developed a theoretical model to analyse the impact of various Er:YAG laser parameters on tissue coagulation and ablation efficiency. It was established that increasing pulse duration within the range of 10 μs to 2 ms leads to a significant increase in thermal penetration depth, which may potentially enhance tissue remodelling effectiveness in snoring treatment. However, excessively high energy levels result in less controlled ablation, potentially increasing the risk of side effects. The study by K. Stock et al. [
31] investigated the ablative and thermal effects of a novel pulsed Er:YAG laser mode, which combined a high pulse repetition rate (up to 2 kHz) with a pulse duration exceeding 1 ms. It was found that this combination promoted uniform tissue heating without excessive damage to submucosal structures, potentially improving treatment outcomes for snoring through gentle thermal remodelling of the soft palate. In the study by L. Bernal et al. [
32], the effects of different cooling methods and water spray delivery during Er:YAG laser application were evaluated. Effective cooling was shown to reduce coagulative damage and allow for better control of energy penetration depth. This is a critical factor in the use of laser therapy for snoring, as it minimizes the risk of burns and structural tissue damage. The collective data suggest that the most effective protocol for Er:YAG laser treatment of snoring involves the use of moderate energy fluence (approximately 2 J/cm
2), pulse durations of 0.5–2 ms, and repetition rates in the range of 10–20 Hz, along with a cooling system to manage thermal effects. The optimal number of treatment sessions varies from three to five, with 2–3-week intervals between procedures, providing long-lasting results and minimal risk of recurrence. Scientific studies comparing the efficacy of Er:YAG laser therapy with other treatment modalities for snoring highlight its unique advantages and limitations in terms of effectiveness, patient comfort, and cost-efficiency. A summary of the comparative data is presented in
Table 8.
The study by T.-R. Vuorjoki-Ranta et al. [
28] investigated the long-term outcomes of mandibular advancement device (MAD) therapy in patients with OSA in Finland. Over a 7-year follow-up period, a decline in the effectiveness of MAD therapy was observed due to adaptation issues and side effects, including jaw pain and discomfort while wearing the device. These findings suggest a potential advantage of laser treatment, which does not require prolonged use of appliances and offers more stable outcomes. Studies examining the effectiveness of different Er:YAG laser modes (LP mode, SMOOTH mode, and their combinations) in the treatment of snoring indicate variations in clinical efficacy and the long-term stability of results. In the study by M. Lukač et al. [
18], the mechanism of action of the FotonaSmooth mode was assessed, which is based on a rapid thermal shock to the epithelium combined with gradual heating of connective tissue. This promotes collagen regeneration, enhances tissue elasticity, and reduces the degree of soft palate collapse—directly contributing to a decrease in snoring intensity. The study demonstrates that the SMOOTH mode offers minimal invasiveness while maintaining high clinical effectiveness, making it an optimal option for patients who prefer non-surgical interventions. Another study by N. Moftah et al. [
33] compared the efficacy of the SMOOTH mode Er:YAG laser with traditional tissue rejuvenation methods used in aesthetic medicine. It was found that this mode enables a more controlled thermal effect without significant ablation, which is critical in snoring treatment, as it eliminates the risk of scar tissue formation or excessive mucosal damage. This confirms the advantage of the SMOOTH mode over the LP mode, as it provides gentle yet effective collagen stimulation without an ablative effect. An analysis of clinical studies suggests that the optimal protocol for treating snoring using the Er:YAG laser includes the application of the SMOOTH mode in combination with low-energy pulses (0.8–2.0 J/cm
2) for safe and effective action on soft tissues. This approach enables stable outcomes over 12–24 months without significant side effects or the need for prolonged recovery. However, in patients with pronounced soft palate hypertrophy, the combined use of the LP mode and SMOOTH mode may produce a more pronounced therapeutic effect, although long-term observation is required to evaluate the durability of results.
3.3. Comparative Analysis of the LP Mode and SMOOTH Mode in Snoring Treatment
Scientific studies confirm that the LP mode and SMOOTH mode of the Er:YAG laser differ significantly in their mechanisms of action, effectiveness, and long-term outcomes in snoring therapy. The study by H. Qi et al. [
34] analysed the combination of a fractional Nd:YAG laser and SMOOTH mode Er:YAG laser, revealing significant improvements in tissue elasticity and remodelling. The SMOOTH mode was found to induce uniform submucosal heating and activate neocollagenesis processes, making it effective for treating snoring with minimal risk of side effects. Due to deeper energy penetration compared to the LP mode, this approach enables long-lasting soft tissue strengthening without ablation. The study by Q. Zhu et al. [
35] demonstrated that the LP mode is characterised by high pulse power and a shorter exposure time, promoting more intense collagen fibre contraction but associated with a higher level of patient discomfort. Over short timeframes (up to 6 months), the LP mode provides faster snoring reduction, but in the long-term (over 12 months), the effects may diminish due to the lack of sustained tissue remodelling stimulation. In the study by R. Dai et al. [
36], the Er:YAG laser was compared with other laser technologies. It was found that the SMOOTH mode provides longer-lasting results, whereas the LP mode offers more rapid but less stable improvement. Moreover, the SMOOTH mode is superior in terms of patient comfort, causing less pain and facilitating faster post-procedural healing. Thus, the LP mode is effective for rapid collagen contraction and initial snoring reduction, but its effect is less stable over the long term and may be accompanied by greater discomfort. The SMOOTH mode promotes more uniform tissue remodelling, allowing for long-term results with minimal side effects, making it the optimal choice for patients seeking durable outcomes with maintained comfort and safety. The combination of the LP mode and SMOOTH mode in the use of the Er:YAG laser for snoring treatment represents an innovative approach that could potentially enhance therapeutic efficacy by leveraging different mechanisms of action. Studies indicate that the SMOOTH mode stimulates tissue renewal and angiogenesis, which may improve the elasticity and structural integrity of pharyngeal tissues. For example, the study by K. Mackova and J. Deprest [
37] showed that the application of the Er:YAG laser in SMOOTH mode significantly increases epithelial thickness and improves tissue quality, which could be crucial in the treatment of respiratory disorders, including snoring. The effects of the LP mode, a long-pulse mode, may also be significant, especially in its ability to alter the biomechanical properties of soft tissues. For instance, in the study by N. Moftah et al. [
33] focused on the treatment of mucosal atrophy, it was found that the combination of modes allows for long-lasting results without the need for additional invasive therapy. Regarding the comparative efficacy of combination therapy versus monotherapy, some studies show that the combined use of the LP mode and SMOOTH mode may ensure more stable outcomes in treating functional disorders of the soft palate and pharyngeal tissues. For example, the study by C. Erel et al. [
20], which investigated the effect of the Er:YAG laser on urinary incontinence treatment, demonstrated sustained symptom improvement with the use of the SMOOTH mode, which may be extrapolated to snoring therapy. Summary data on different laser therapy protocols for snoring, based on the latest scientific research, are presented in
Table 9.
The study by S. Shamsudeen et al. [
38] confirms that the use of a SMOOTH mode Er:YAG laser contributes to the enhancement of the biomechanical properties of the soft palate tissues by stimulating fibroplastic activity and increasing collagen synthesis. Histological analysis following laser exposure shows densification of collagen fibres and changes in their spatial orientation, resulting in improved mechanical stability of the tissues. These effects correlate with a reduction in the amplitude of soft palate vibrations and improved airflow dynamics in the upper respiratory tract, which may have a significant therapeutic impact on the treatment of snoring. When using a combined mode involving both Er:YAG (2940 nm) and Nd:YAG (1064 nm) lasers, an improvement in collagen fibre quality and long-term remodelling of the mucosal lining has been observed. The study by N. Kasetsuwan et al. [
39] demonstrated that this technique significantly enhances the functional state of tissues by increasing their strength and reducing fibrosis, thereby positively affecting the efficacy of treatment for snoring and sleep apnoea. Thus, the application of different Er:YAG laser modes influences both the morphological and functional characteristics of upper airway tissues. The SMOOTH mode promotes improvement in the structure of the mucosa, the combined mode provides long-term remodelling of collagen fibres, and the overall increase in tissue stiffness and reduction in fibrosis correlates with a decrease in snoring intensity and improved airway function. According to long-term studies comparing the LP mode, SMOOTH mode, and their combination in the treatment of snoring, statistically significant differences exist in the duration of therapeutic effect, the need for repeated sessions, and patient satisfaction levels. In the study by Y. Tan et al. [
23], the use of a SMOOTH mode Er:YAG laser in patients with stress urinary incontinence led to significant improvements in both subjective and objective outcomes, with effects maintained for up to six months post-treatment. Efficacy was assessed using the ICIQ-UI-SF scale [
40], a reliable tool for evaluating changes in patient condition following laser therapy. Y. Bayraktar et al. [
24] investigated the impact of various pulse parameters of the Er:YAG laser on tissue biomechanical properties. It was found that the longer pulses in LP mode result in greater thermal effect and more extensive collagen remodelling, providing a longer therapeutic effect compared to the shorter pulses in SMOOTH mode. The methodology for evaluating efficacy included microtensile testing of tissue strength, demonstrating high objectivity and reproducibility of the obtained results. T. Lin et al. [
41] examined the combined use of Er:YAG and Nd:YAG lasers in the treatment of peri-implantitis and found that such a combination leads to more intense stimulation of regenerative processes in tissues. This may be of potential relevance for the treatment of snoring, as the combined laser effect could contribute to more prolonged remodelling of the soft tissues of the upper airway. Efficacy was evaluated using histological analysis and clinical measurements, enhancing the reliability of the conclusions. Thus, long-term observations indicate that the LP mode provides a more prolonged effect, although it may require a greater number of procedures to achieve optimal results. The SMOOTH mode demonstrates more rapid clinical improvements but typically requires repeated sessions after six or more months. Combined approaches may enhance the regenerative properties of tissues, potentially reducing the recurrence rate. The most reliable methods for evaluating treatment outcomes include subjective quality-of-life scales, polygraphic analysis, and histological examination of tissues, which together offer a comprehensive assessment of therapeutic effectiveness.
3.4. Safety and Tolerability of Er:YAG Laser Procedures for Snoring
Recent studies analysing the side effects and complications following the use of Er:YAG lasers for treating snoring indicate that this method is relatively safe and well-tolerated by patients. However, both short-term and long-term side effects are possible. Short-term complications include pain, swelling, mild dysphagia, and transient irritation of the mucosal lining. For example, a study by H. Frelich et al. [
15] found that patients undergoing three sessions of Er:YAG laser treatment for snoring did not experience significant side effects, although mild discomfort was noted in some participants during the first few days after the procedure. Another study by F. Weniger et al. [
42], focused on the use of the Er:YAG laser for skin rejuvenation, identified common short-term side effects such as erythema, mild swelling, and heightened sensitivity, which resolved within a week. Long-term complications, such as fibrosis, voice changes, chronic dry mouth, or nasal breathing disturbances, are rare but may occur in patients with sensitive mucous membranes or due to excessive thermal exposure. A study by A. Liu et al. [
43] analysed the use of the Er:YAG laser for sebaceous hyperplasia treatment and found that with appropriate laser parameter selection, the risk of scar tissue formation was minimal. Additionally, research by L. Hympanova et al. [
44], which examined sheep exposed to vaginal Er:YAG lasers, concluded that although the procedure caused temporary thickening of the epithelium, it did not affect tissue structure or blood supply in the long term. Methods to minimize side effects include controlled use of laser parameters, proper tissue cooling during the procedure, and post-operative care with specialised products. For instance, using the erbium laser in long-pulse mode reduces the risk of deep thermal damage, thus decreasing the likelihood of chronic complications. When assessing the safety profile of the Er:YAG laser across various modes (LP mode, SMOOTH mode, and combined mode), it is crucial to consider how each mode impacts tissues, the associated risks of complications, and the patient groups that are more prone to side effects. The LP mode, which operates with long pulses, allows effective tissue ablation but is also associated with a risk of thermal injury, particularly at high power settings. F. Weniger et al. [
42] demonstrated that more aggressive ablation modes, such as the LP mode, may lead to increased inflammation, especially in areas with high vascularization. Therefore, this mode requires precise energy control and adequate cooling. Combined modes that combine the LP and SMOOTH modes offer an optimal balance between effectiveness and safety. For example, in treating peri-implantitis, using the Er:YAG laser in combination with mechanical debridement resulted in better bacterial elimination and tissue regeneration compared to traditional methods [
45]. To reduce the risk of complications, it is recommended to gradually increase the energy, select less aggressive modes for patients with risk factors, and combine laser therapy with regenerative strategies, such as platelet concentrate or low-intensity phototherapy [
46]. Pain during and after snoring treatment with the Er:YAG laser is typically characterized by low intensity and short duration. Clinical studies have shown that patients rate their pain on the VAS scale as mild or moderate, with discomfort usually lasting no more than a few hours post-procedure. Clinical outcomes confirm that the level of pain during and after the procedure influences patients’ perception of its effectiveness. Those reporting minimal discomfort often demonstrate a more positive attitude toward the treatment and report significant improvements in sleep quality. Long-term studies have shown that patients who experienced minimal pain during the procedure often noted a substantial reduction in snoring frequency and intensity, even years after the therapy, suggesting a lasting clinical effect of Er:YAG laser treatment [
47]. The frequency, intensity, and duration of pain during and after the procedure vary depending on the emission parameters and individual patient characteristics. Most studies indicate that the procedure is well-tolerated, with any pain being mild or moderate and resolving quickly. In a clinical study by J. Shang et al. [
48], it was found that patients treated with the Er:YAG laser experienced less intense pain compared to those undergoing traditional surgical interventions, and post-operative discomfort was brief. Analgesic methods during laser therapy include topical local anaesthesia in the form of lidocaine-based gels or sprays, significantly reducing discomfort during the procedure. In most cases, systemic analgesics are not required after treatment due to the short-lived nature of the pain. B. Hajhosseini et al. [
49] demonstrated that using the Er:YAG laser minimizes the need for additional pain relief due to its selective tissue impact without significant nerve damage. Subjective pain perception correlates with patient satisfaction and the overall efficacy of the procedure. Patients who report no significant pain more often rate the treatment results as satisfactory. Most participants in long-term studies reported significant improvements in sleep quality and reduced snoring intensity months after treatment, suggesting a stable therapeutic effect of laser therapy [
50]. Thus, Er:YAG laser treatment is an effective, well-tolerated method that ensures high patient satisfaction with minimal pain. Overall patient satisfaction with snoring treatment using the Er:YAG laser is evaluated based on subjective indicators such as sleep quality, quality of life, social adaptation, and general well-being. Studies confirm the high efficacy of this method, resulting in a significant reduction in snoring intensity and improved subjective assessments of life quality. Another study by T. Damrongrungruang et al. [
10] found that after the third treatment session, more than 85% of patients reported significant improvements in their condition. All participants noted better breathing during sleep and reduced fatigue, which greatly impacted their quality of life. The absence of major side effects and the lack of need for anaesthesia increased patients’ willingness to recommend this treatment to others. E. Cetinkaya et al. [
9] reported that 65% of patients were satisfied with the results after three Er:YAG laser sessions, with the greatest improvement observed in patients over 50 years old, who reported reduced daytime sleepiness, and improved concentration and overall well-being. In summary, Er:YAG laser treatment for snoring demonstrates high effectiveness and is well-tolerated by patients, as evidenced by the high satisfaction rates, improvements in subjective sleep quality, and the absence of serious side effects. The main factors influencing patients’ willingness to recommend this treatment are its safety, long-term effectiveness, and the possibility of repeat treatment if necessary.
3.5. Factors Predicting the Success of Laser Snoring Therapy in Patients
Patients’ anatomical and physiological characteristics have a significant impact on the effectiveness of snoring treatment with an Er:YAG laser, determining the results of therapy and the possibility of personalising treatment protocols. One of the key factors is body mass index (BMI), as obese patients are at a higher risk of airway collapse during sleep due to fatty deposits in the oropharynx.
Table 10 summarizes the main factors that influence the clinical outcomes of Er:YAG snoring treatment.
Anatomical variations of the oropharynx, including the size and shape of the soft palate, as well as the thickness of the uvula, play a significant role in the outcomes of laser therapy. The use of the Er:YAG laser causes remodelling of the soft tissues of the palate and uvula, which is especially effective in patients with an excessively long uvula or hypertrophied palatine arches. The position of the tongue and the degree of its retroposition are additional determinants of therapy success. Patients with macroglossia or reduced tonic activity of the tongue are at increased risk of recurrence of snoring symptoms after the initial course of therapy, indicating the need for combined approaches, such as orthodontic correction or specific tongue muscle exercises. Furthermore, the degree of nasal obstruction influences the response to treatment, as patients with severe nasal obstruction tend to have increased negative pressure in the oropharynx, which increases the likelihood of snoring recurrence after laser correction [
14]. The effectiveness of snoring treatment with the Er:YAG laser shows a certain dependence on demographic characteristics, lifestyle, and comorbidities. A study by B. Jiryis et al. [
52] examined the impact of harmful habits, such as smoking, on the efficacy of laser treatment. It was found that smokers showed significantly worse outcomes, as nicotine and chronic inflammation negatively affected the tissue remodelling process, reducing the effectiveness of the laser intervention. Meanwhile, non-smoking patients showed a more sustained reduction in the soft palate and a decrease in the frequency of snoring episodes. Regarding metabolic diseases, a study by N. Fistonić et al. [
51] demonstrated that overweight and obese patients had lower treatment efficacy with the Er:YAG laser. It was found that fat deposits in the neck and palate region contribute to a significant reduction in the effect of laser treatment due to persistent obstruction of the upper airways. However, in patients with a normal body weight, the effect lasted longer and had a more pronounced impact on the reduction of snoring volume. Concerning gender differences, a study by C. Huang et al. [
53] showed that women had a better response to Er:YAG laser treatment compared to men. This may be related to differences in connective tissue structure as well as hormonal influences, particularly the level of oestrogen, which promotes more effective remodelling of soft tissues. Assessment of the initial severity of snoring and comorbid respiratory conditions play a crucial role in determining the effectiveness of snoring treatment with the Er:YAG laser. Snoring can vary in intensity, which is measured in decibels, and may occur intermittently or be constant. Moreover, its severity is influenced by positional dependence and the presence of apnoea. A study by Y. Minin & T. Kucherenko [
16] shows that patients with mild or moderate obstructive sleep apnoea (OSA) (AHI 5–30) achieve significantly better results after laser therapy compared to patients with severe disease (AHI > 30), in whom the effect may be less pronounced and unstable. Allergic rhinitis, regardless of seasonality, is also a negative factor, as it contributes to chronic inflammation of the nasopharynx, complicating the formation of stable changes in the tissues after laser intervention. Patients with chronic obstructive pulmonary disease (COPD) and bronchial asthma require special attention, as laser treatment may cause a temporary exacerbation of symptoms due to a local response to thermal effects [
8]. Optimal candidates for Er:YAG laser therapy are patients with primary snoring or mild to moderate OSA, without significant tonsil hypertrophy, no pronounced inflammatory process in the nasopharynx, and without severe comorbid obstructive lung diseases. Additionally, patients without anatomical obstructions such as significant retrognathia or macroglossia have better treatment outcomes [
17]. The main risks of therapy include temporary discomfort, dry mouth, and the possibility of symptom recurrence, especially in the absence of lifestyle modifications. In general, the success of Er:YAG laser treatment largely depends on the initial severity of snoring, the degree of OSA, and comorbid respiratory pathologies. To increase the procedure’s effectiveness, it is essential to carefully select patients, considering their clinical presentation and potential risks. Scientific analysis of current diagnostic methods and prognostic models for patient stratification and the prediction of treatment efficacy with Er:YAG laser therapy indicate a comprehensive approach in research. Polysomnography (PSG) remains the gold standard for diagnosing sleep-related breathing disorders, assessing the apnoea–hypopnoea index (AHI), respiratory disturbance index (RDI), oxygen desaturation index (ODI), and sleep structure. The importance of PSG for patient stratification has been confirmed by studies showing a significant correlation between AHI and the efficacy of laser treatment [
54]. However, due to its high cost and limited availability, home screening systems are actively being developed to assess oxygen desaturation levels and obstruction indices with high specificity for severe forms of OSA [
55]. Acoustic analysis of snoring, particularly the determination of frequency characteristics and patterns, is also used as a non-invasive approach for predicting the severity of breathing disorders. A study by L. Hou et al. [
56] proposed the use of ERB (Equivalent Rectangular Bandwidth)-correlation measurement of snoring sounds to calculate AHI, demonstrating an accuracy of 87.5% compared to PSG. Ultrasonographic examination of the soft tissues of the oropharynx is used to assess tissue density and elasticity, which allows for the prediction of laser therapy effectiveness. Machine learning is actively integrated into patient stratification and the prediction of Er:YAG laser treatment efficacy. Recent studies propose algorithms that use multiparametric models based on PSG, acoustic analysis, and imaging, improving prediction accuracy [
56]. The optimal pre-operative assessment algorithm includes initial screening using home systems, further PSG evaluation for high-risk OSA patients, endoscopic visualization for obstruction analysis, and ultrasound or MRI (Magnetic Resonance Imaging) scanning for tissue stratification. The use of machine learning may enhance prediction accuracy and clarify laser treatment protocols, contributing to a scientific approach to snoring therapy.