Adolescent ACL Reconstruction Using Quadriceps or Hamstring Tendon Autografts: A Comparative Study of Muscle Strength and Patient-Reported Outcomes
Abstract
1. Introduction
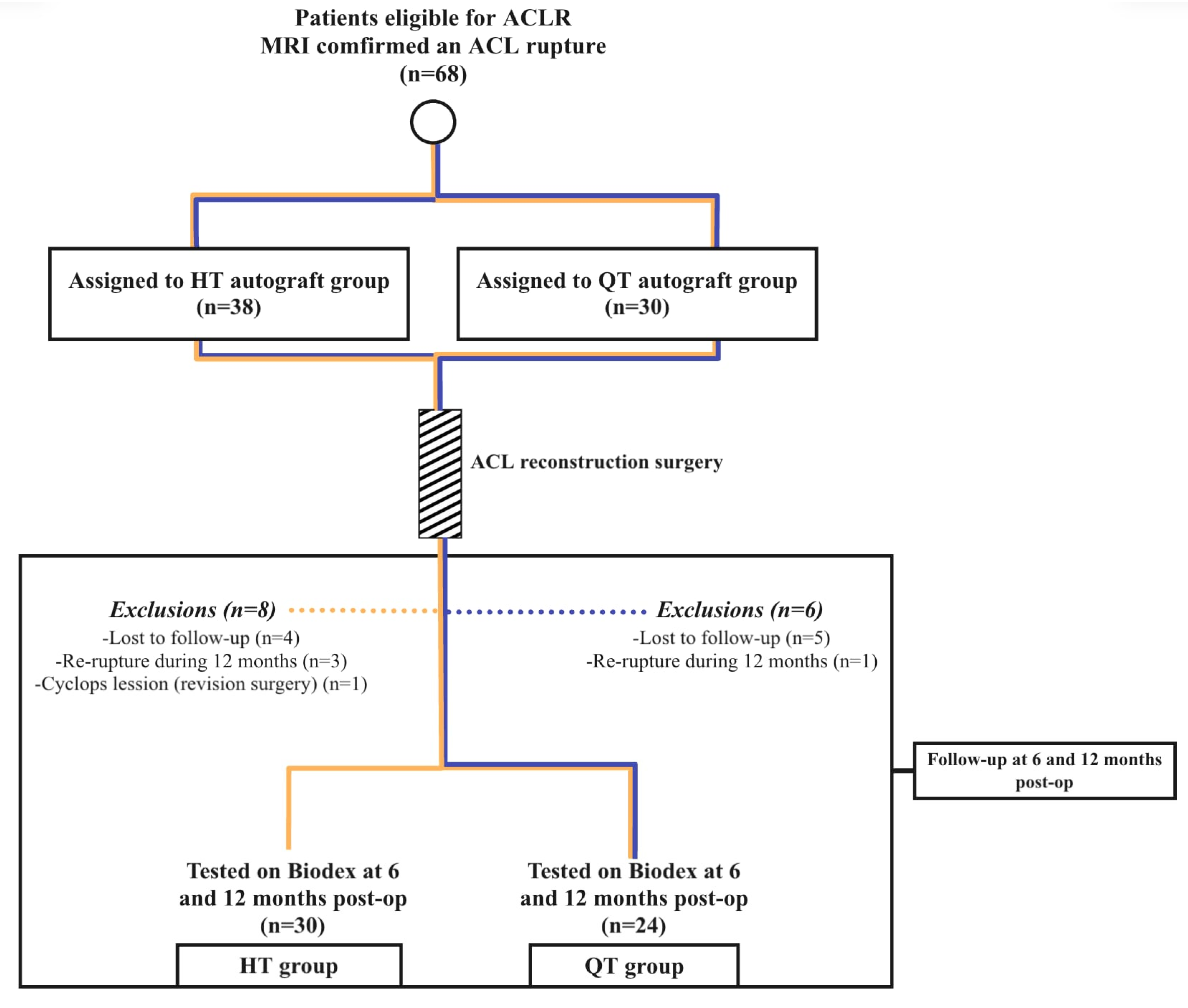
2. Materials and Methods
2.1. Participants and Surgical Technique
2.2. Muscle Strength Evaluation (Isokinetic Measurement) by Biodex
2.3. Satisfaction Evaluation
2.4. Statistical Analysis
3. Results
3.1. Sample Characteristics
3.2. Muscle Strength Outcomes Between the Groups
3.3. Muscle Strength Outcomes Comparing Involved and Uninvolved Legs Between the Groups
3.4. Satisfaction Outcomes Between the Groups
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| ACL | Anterior cruciate ligament |
| ACLR | Anterior cruciate ligament reconstruction |
| QT | Quadriceps tendon |
| HT | Hamstring tendons |
| IQR | Interquartile range |
| H/Q | Hamstring-to-quadriceps ratio |
| TQ/BW | Peak torque to body weight ratio |
| IKDC | International Knee Documentation Committee score |
| ACL-RSI | Anterior cruciate ligament return to sport after injury scale |
References
- De Petrillo, G.; Pauyo, T.; Franklin, C.C.; Chafetz, R.S.; Nault, M.-L.; Veilleux, L.-N. Limited evidence for graft selection in pediatric ACL Reconstruction: A narrative review. J. Exp. Orthop. 2022, 9, 9. [Google Scholar] [CrossRef] [PubMed]
- D’Ambrosi, R.; Kambhampati, S.B.; Meena, A.; Milinkovic, D.D.; Abermann, E.; Fink, C. The “Golden Age” of quadriceps tendon grafts for the anterior cruciate ligament: A bibliometric analysis. J. ISAKOS Jt. Disord. Orthop. Sports Med. 2024, 9, 672–681. [Google Scholar] [CrossRef] [PubMed]
- Hurley, E.T.; Mojica, E.S.; Kanakamedala, A.C.; Meislin, R.J.; Strauss, E.J.; Campbell, K.A.; Alaia, M.J. Quadriceps tendon has a lower re-rupture rate than hamstring tendon autograft for anterior cruciate ligament reconstruction—A meta-analysis. J. ISAKOS Jt. Disord. Orthop. Sports Med. 2022, 7, 87–93. [Google Scholar] [CrossRef]
- Runer, A.; Csapo, R.; Hepperger, C.; Herbort, M.; Hoser, C.; Fink, C. Anterior cruciate ligament reconstructions with quadriceps tendon autograft result in lower graft rupture rates but similar patient-reported outcomes as compared with hamstring tendon autograft: A comparison of 875 patients. Am. J. Sports Med. 2020, 48, 2195–2204. [Google Scholar] [CrossRef]
- Güzel, N.; Yılmaz, A.K.; Genç, A.S.; Karaduman, E.; Kehribar, L. Pre- and post-operative hamstring autograft ACL reconstruction isokinetic knee strength assessments of recreational athletes. J. Clin. Med. 2022, 12, 63. [Google Scholar] [CrossRef]
- Güzel, N.; Genç, A.S.; Yılmaz, A.K.; Kehribar, L. The Relationship between lower extremity functional performance and balance after anterior cruciate ligament reconstruction: Results of patients treated with the modified all-inside technique. J. Pers. Med. 2023, 13, 466. [Google Scholar] [CrossRef]
- Shani, R.H.; Umpierez, E.; Nasert, M.; Hiza, E.A.; Xerogeanes, J. Biomechanical comparison of quadriceps and patellar tendon grafts in Anterior Cruciate Ligament Reconstruction. Arthrosc. J. Arthrosc. Relat. Surg. 2016, 32, 71–75. [Google Scholar] [CrossRef]
- Hadjicostas, P.T.; Soucacos, P.N.; Berger, I.; Koleganova, N.; Paessler, H.H. Comparative Analysis of the Morphologic Structure of Quadriceps and Patellar Tendon: A Descriptive Laboratory Study. Arthrosc. J. Arthrosc. Relat. Surg. 2007, 23, 744–750. [Google Scholar] [CrossRef]
- Hadjicostas, P.T.; Soucacos, P.N.; Paessler, H.H.; Koleganova, N.; Berger, I. Morphologic and Histologic Comparison Between the Patella and Hamstring Tendons Grafts: A Descriptive and Anatomic Study. Arthrosc. J. Arthrosc. Relat. Surg. 2007, 23, 751–756. [Google Scholar] [CrossRef]
- Rakauskas, R.; Šiupšinskas, L.; Streckis, V.; Balevičiūtė, J.; Galinskas, L.; Malcius, D.; Čekanauskas, E. Hamstring vs. all-soft-tissue quadriceps tendon autograft for anterior cruciate ligament reconstruction in adolescent athletes: Early follow-up results of a prospective study. Appl. Sci. 2023, 13, 6715. [Google Scholar] [CrossRef]
- Toor, A.S.; Limpisvasti, O.; Ihn, H.E.; McGarry, M.H.; Banffy, M.; Lee, T.Q. The significant effect of the medial hamstrings on dynamic knee stability. Knee Surg. Sports Traumatol. Arthrosc. 2018, 27, 2608–2616. [Google Scholar] [CrossRef] [PubMed]
- Delextrat, A.; Bateman, J.; Ross, C.; Harman, J.; Davis, L.; Vanrenterghem, J.; Cohen, D.D. Changes in torque-angle profiles of the hamstrings and hamstrings-to-quadriceps ratio after two hamstring strengthening exercise interventions in female hockey players. J. Strength Cond. Res. 2020, 34, 396–405. [Google Scholar] [CrossRef] [PubMed]
- Kong, P.W.; Burns, S.F. Bilateral difference in hamstrings to quadriceps ratio in healthy males and females. Phys. Ther. Sport 2010, 11, 12–17. [Google Scholar] [CrossRef] [PubMed]
- Orchard, J.; Marsden, J.; Lord, S.; Garlick, D. Preseason hamstring muscle weakness associated with hamstring muscle injury in Australian footballers. Am. J. Sports Med. 1997, 25, 81–85. [Google Scholar] [CrossRef]
- Haillotte, G.; Hardy, A.; Granger, B.; Noailles, T.; Khiami, F. Early strength recovery after anterior cruciate ligament reconstruction using the fascia lata. Orthop. Traumatol. Surg. Res. 2017, 103, 1021–1025. [Google Scholar] [CrossRef]
- Fischer, F.; Fink, C.; Herbst, E.; Hoser, C.; Hepperger, C.; Blank, C.; Gföller, P. Higher hamstring-to-quadriceps isokinetic strength ratio during the first post-operative months in patients with quadriceps tendon compared to hamstring tendon graft following ACL reconstruction. Knee Surg. Sports Traumatol. Arthrosc. 2017, 26, 418–425. [Google Scholar] [CrossRef]
- Martin-Alguacil, J.L.; Arroyo-Morales, M.; Martín-Gomez, J.L.; Monje-Cabrera, I.M.; Abellán-Guillén, J.F.; Esparza-Ros, F.; Lozano, M.L.; Cantarero-Villanueva, I. Strength recovery after anterior cruciate ligament reconstruction with quadriceps tendon versus hamstring tendon autografts in soccer players: A randomized controlled trial. Knee 2018, 25, 704–714. [Google Scholar] [CrossRef]
- Hughes, J.D.; Burnham, J.M.; Hirsh, A.; Musahl, V.; Fu, F.H.; Irrgang, J.J.; Lynch, A.D. Comparison of short-term biodex results after anatomic anterior cruciate ligament reconstruction among 3 autografts. Orthop. J. Sports Med. 2019, 7, 2325967119847630. [Google Scholar] [CrossRef]
- Kay, J.; Liotta, E.S.; Sugimoto, D.; Heyworth, B.E. Assessment of return to sport after acl reconstruction with soft tissue autograft in adolescent athletes: Quadriceps versus hamstring tendon. Orthop. J. Sports Med. 2023, 11, 23259671231207113. [Google Scholar] [CrossRef]
- Horteur, C.; Duval, B.R.; Merlin, A.; Cognault, J.; Ollivier, M.; Pailhe, R. COMPARISON of knee extensor strength after anterior cruciate ligament reconstruction using either quadriceps tendon or hamstring tendon autografts. Eur. J. Orthop. Surg. Traumatol. 2021, 32, 857–865. [Google Scholar] [CrossRef]
- Setuain, I.; Izquierdo, M.; Idoate, F.; Bikandi, E.; Gorostiaga, E.M.; Aagaard, P.; Cadore, E.L.; Alfaro-Adrián, J. Differential effects of 2 rehabilitation programs following Anterior Cruciate Ligament Reconstruction. J. Sport Rehabil. 2017, 26, 544–555. [Google Scholar] [CrossRef] [PubMed]
- Solie, B.; Monson, J.; Larson, C. Graft-Specific surgical and rehabilitation considerations for anterior cruciate ligament reconstruction with the quadriceps tendon autograft. Int. J. Sports Phys. Ther. 2023, 18, 493–512. [Google Scholar] [CrossRef] [PubMed]
- Leung, A.; DeSandis, B.; O’brien, L.; Hammoud, S.; Zarzycki, R. Postoperative considerations based on graft type after Anterior Cruciate Ligament Reconstruction a narrative review. Ann. Jt. 2023, 8, 26. [Google Scholar] [CrossRef]
- Eitzen, I.; Holm, I.; Risberg, M.A. Preoperative quadriceps strength is a significant predictor of knee function two years after anterior cruciate ligament reconstruction. Br. J. Sports Med. 2009, 43, 371–376. [Google Scholar] [CrossRef]
- Kahlenberg, C.A.; Nwachukwu, B.U.; Ferraro, R.A.; Schairer, W.W.; Steinhaus, M.E.; Allen, A.A. How are we measuring patient satisfaction after Anterior Cruciate Ligament Reconstruction? Orthop. J. Sports Med. 2016, 4, 2325967116673971. [Google Scholar] [CrossRef]
- Gorschewsky, O.; Klakow, A.; Pütz, A.; Mahn, H.; Neumann, W. Clinical comparison of the autologous quadriceps tendon (BQT) and the autologous patella tendon (BPTB) for the reconstruction of the Anterior Cruciate Ligament. Knee Surg. Sports Traumatol. Arthrosc. 2007, 15, 1284–1292. [Google Scholar] [CrossRef]
- Dadoo, S.; Herman, Z.J.; Nazzal, E.M.; Drain, N.P.; Finger, L.; Reddy, R.P.; Miller, L.; Lesniak, B.P.; Musahl, V.; Hughes, J.D. Outcomes after anterior cruciate ligament reconstruction with quadriceps tendon in adolescent athletes at mean follow-up of 4 years. Orthop. J. Sports Med. 2024, 12, 23259671241254795. [Google Scholar] [CrossRef]
- Fones, L.; Kostyun, R.O.; Cohen, A.D.; Pace, J.L. Patient-reported outcomes, return-to-sport status, and reinjury rates after anterior cruci ate ligament reconstruction in adolescent athletes: Minimum 2-year follow-up. Orthop. J. Sports Med. 2020, 8, 2325967120964471. [Google Scholar] [CrossRef]
- Geffroy, L.; Lefevre, N.; Thevenin-Lemoine, C.; Peyronnet, A.; Lakhal, W.; Fayard, J.M.; Chotel, F. Return to sport and re-tears after Anterior Cruciate Ligament Reconstruction in children and adolescents. Orthop. Traumatol. Surg. Res. 2018, 104, S183–S188. [Google Scholar] [CrossRef]
- Kay, J.; Memon, M.; Marx, R.G.; Peterson, D.; Simunovic, N.; Ayeni, O.R. Over 90% of children and adolescents return to sport after Anterior Cruciate Ligament Reconstruction: A systematic review and meta-analysis. Knee Surg. Sports Traumatol. Arthrosc. 2018, 26, 1019–1036. [Google Scholar] [CrossRef]
- Webster, K.E.; McPherson, A.L.; Hewett, T.E.; Feller, J.A. Factors associated with a return to preinjury level of sport performance after Anterior Cruciate Ligament Reconstruction surgery. Am. J. Sports Med. 2019, 47, 2557–2562. [Google Scholar] [CrossRef]
| QT (n = 24) | HT (n = 30) | Test Statistic | p Value | |
|---|---|---|---|---|
| Age in years (median (IQR)) | 15.5 (15–16.75) | 15 (14–16) | |Z| = 1.306 | 0.192 |
| Sex (male/female) | 9/15 | 18/12 | χ2 = 1.875 | 0.171 |
| Height in cm (median (IQR)) | 173.5 (169–181.5) | 177.5 (161–180) | |Z| = 0.157 | 0.875 |
| Weight in kg (median (IQR)) | 65 (53.5–77.25) | 66.5 (62–78) | |Z| = 0.471 | 0.638 |
| BMI Z-score (median; (IQR)) | 0.14 (−0.456–0.79) | 0.43 (0.21–0.83) | |Z| = 1.255 | 0.209 |
| Meniscus (repaired/repair not required) | 12/12 | 15/15 | χ2 = 0 | 1 |
| QT (n = 24) (Median; IQR) | HT (n = 30) (Median; IQR) | Test Statistic | p Value | |
|---|---|---|---|---|
| 6 months post-surgery | ||||
| Extensors peak TQ/BW in % | 121.45 (92.05–191.4) | 156.9 (109.3–260) | |Z| = 2.353 | 0.019 |
| Flexors peak TQ/BW in % | 84.35 (49.65–110.56) | 75.2 (61.5–98) | |Z| = 0.471 | 0.638 |
| H/Q Ratio | 56.1 (41.93–102.43) | 43.75 (39–55.7) | |Z| = 2.353 | 0.019 |
| 12 months post-surgery | ||||
| Extensors peak TQ/BW in % | 208.55 (136.55–222.2) | 250.8 (168–332.1) | |Z| = 3.375 | <0.001 |
| Flexors peak TQ/BW in % | 115.3 (91.98–122.95) | 91.25 (80.7–123.4) | |Z| = 1.569 | 0.117 |
| H/Q Ratio | 57.2 (43.98–70.1) | 40.9 (37.2–49.7) | |Z| = 4.238 | <0.001 |
| QT (n = 24) (Median; IQR) | Test Statistic | p Value | ||
|---|---|---|---|---|
| 6 months post-surgery | ||||
| Involved | Uninvolved | |||
| Extensors peak TQ/BW in % | 121.45 (92.05–191.4) | 175.4 (162.2–256.65) | |Z| = 3.434 | <0.001 |
| Flexors peak TQ/BW in % | 84.35 (49.65–110.56) | 84.35 (49.63–126.33) | |Z| = 0.773 | 0.455 |
| H/Q Ratio | 56.1 (41.93–102.43) | 49.6 (39.7–56.9) | |Z| = 3.177 | <0.001 |
| 12 months post-surgery | ||||
| Involved | Uninvolved | |||
| Extensors peak TQ/BW in % | 208.55 (136.55–222.2) | 252.4 (204.18–290.28) | |Z| = 3.869 | <0.001 |
| Flexors peak TQ/BW in % | 115.3 (91.98–122.95) | 116 (89.53–145.05) | |Z| = 2.146 | 0.031 |
| H/Q Ratio | 57.2 (43.98–70.1) | 50.65 (45.2–55.78) | |Z| = 2.661 | 0.006 |
| HT (n = 30) (Median; IQR) | ||||
| 6 months post-surgery | ||||
| Involved | Uninvolved | |||
| Extensors peak TQ/BW in % | 156.9 (109.3–260) | 232.1 (193.1–261.8) | |Z| = 4.478 | <0.001 |
| Flexors peak TQ/BW in % | 75.2 (61.5–98) | 102.8 (89.2–126.2) | |Z| = 4.355 | <0.001 |
| H/Q Ratio | 43.75 (39–55.7) | 47.2 (43.1−48.4) | |Z| = 1.390 | 0.165 |
| 12 months post-surgery | ||||
| Involved | Uninvolved | |||
| Extensors peak TQ/BW in % | 250.8 (168–332.1) | 293 (249.1–322) | |Z| = 3.490 | <0.001 |
| Flexors peak TQ/BW in % | 91.25 (80.7–123.4) | 128.95 (97.8–153.6) | |Z| = 4.787 | <0.001 |
| H/Q Ratio | 40.9 (37.2–49.7) | 48.4 (44.9–50.2) | |Z| = 3.366 | <0.001 |
| QT (Median; IQR) | HT (Median; IQR) | Test Statistic | p Value | |
|---|---|---|---|---|
| IKDC | 87.94 (85.64–93.68) | 93.13 (88.51–98.85) | |Z| = 2.599 | 0.009 |
| Lysholm | 95 (91–100) | 98 (95–100) | |Z| = 1.487 | 0.137 |
| ACL-RSI | 70.67 (52.07–88.54) | 80.82 (70.83–92.5) | |Z| = 1.570 | 0.116 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rakauskas, R.; Šiupšinskas, L.; Streckis, V.; Galinskas, L.; Jurkonis, R.; Tomkevičiūtė, J.; Malcius, D.; Čekanauskas, E. Adolescent ACL Reconstruction Using Quadriceps or Hamstring Tendon Autografts: A Comparative Study of Muscle Strength and Patient-Reported Outcomes. J. Clin. Med. 2025, 14, 3842. https://doi.org/10.3390/jcm14113842
Rakauskas R, Šiupšinskas L, Streckis V, Galinskas L, Jurkonis R, Tomkevičiūtė J, Malcius D, Čekanauskas E. Adolescent ACL Reconstruction Using Quadriceps or Hamstring Tendon Autografts: A Comparative Study of Muscle Strength and Patient-Reported Outcomes. Journal of Clinical Medicine. 2025; 14(11):3842. https://doi.org/10.3390/jcm14113842
Chicago/Turabian StyleRakauskas, Ritauras, Laimonas Šiupšinskas, Vytautas Streckis, Laurynas Galinskas, Rokas Jurkonis, Jūratė Tomkevičiūtė, Dalius Malcius, and Emilis Čekanauskas. 2025. "Adolescent ACL Reconstruction Using Quadriceps or Hamstring Tendon Autografts: A Comparative Study of Muscle Strength and Patient-Reported Outcomes" Journal of Clinical Medicine 14, no. 11: 3842. https://doi.org/10.3390/jcm14113842
APA StyleRakauskas, R., Šiupšinskas, L., Streckis, V., Galinskas, L., Jurkonis, R., Tomkevičiūtė, J., Malcius, D., & Čekanauskas, E. (2025). Adolescent ACL Reconstruction Using Quadriceps or Hamstring Tendon Autografts: A Comparative Study of Muscle Strength and Patient-Reported Outcomes. Journal of Clinical Medicine, 14(11), 3842. https://doi.org/10.3390/jcm14113842






