When the Mind Meets the Ear: A Scoping Review on Tinnitus and Clinically Measured Psychiatric Comorbidities
Abstract
1. Introduction
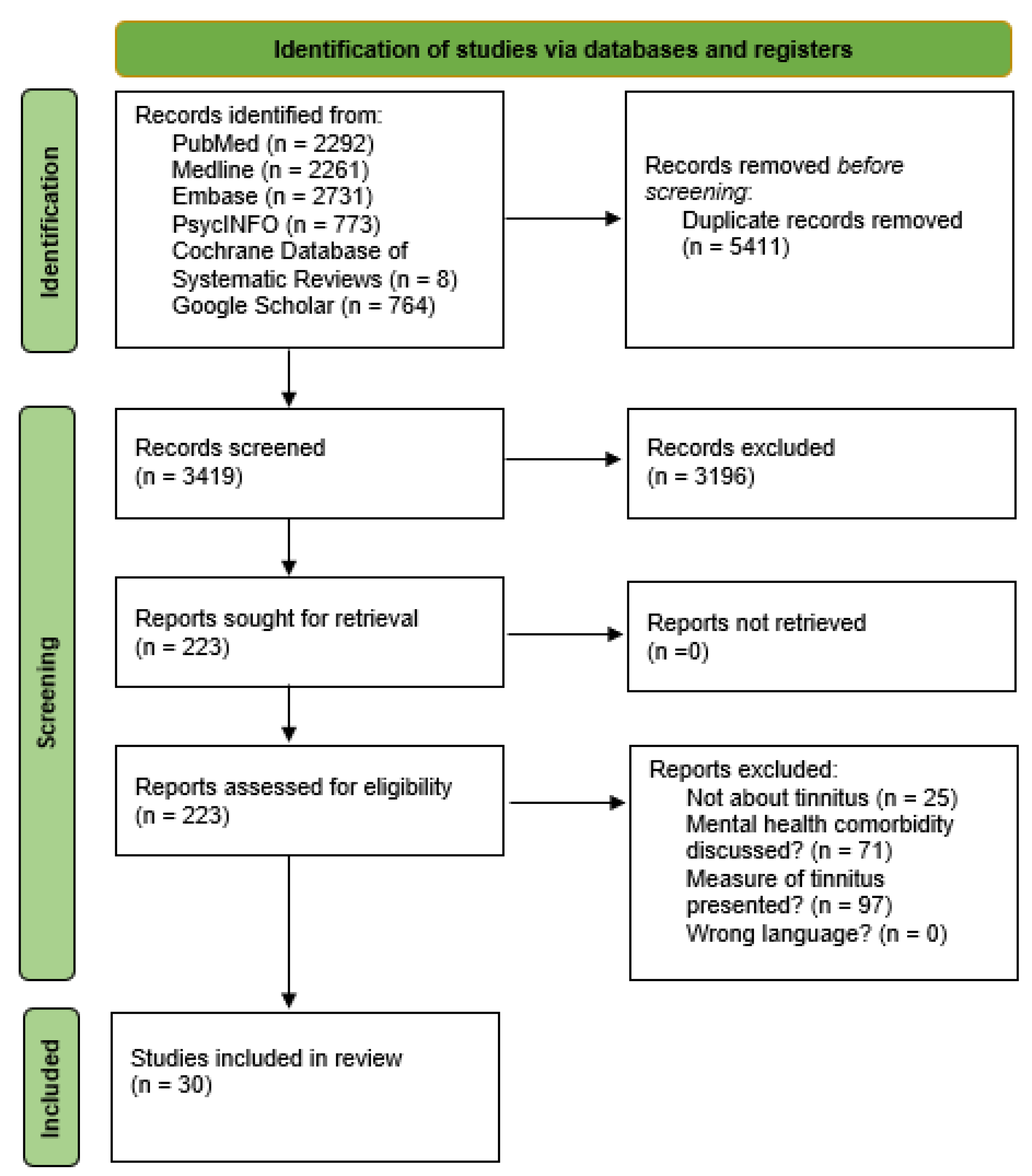
2. Materials and Methods
2.1. Search Strategies
2.2. Study Eligibility Criteria
2.3. Data Extraction
2.4. Quality Assessment
3. Results
3.1. Description of the Identified Studies
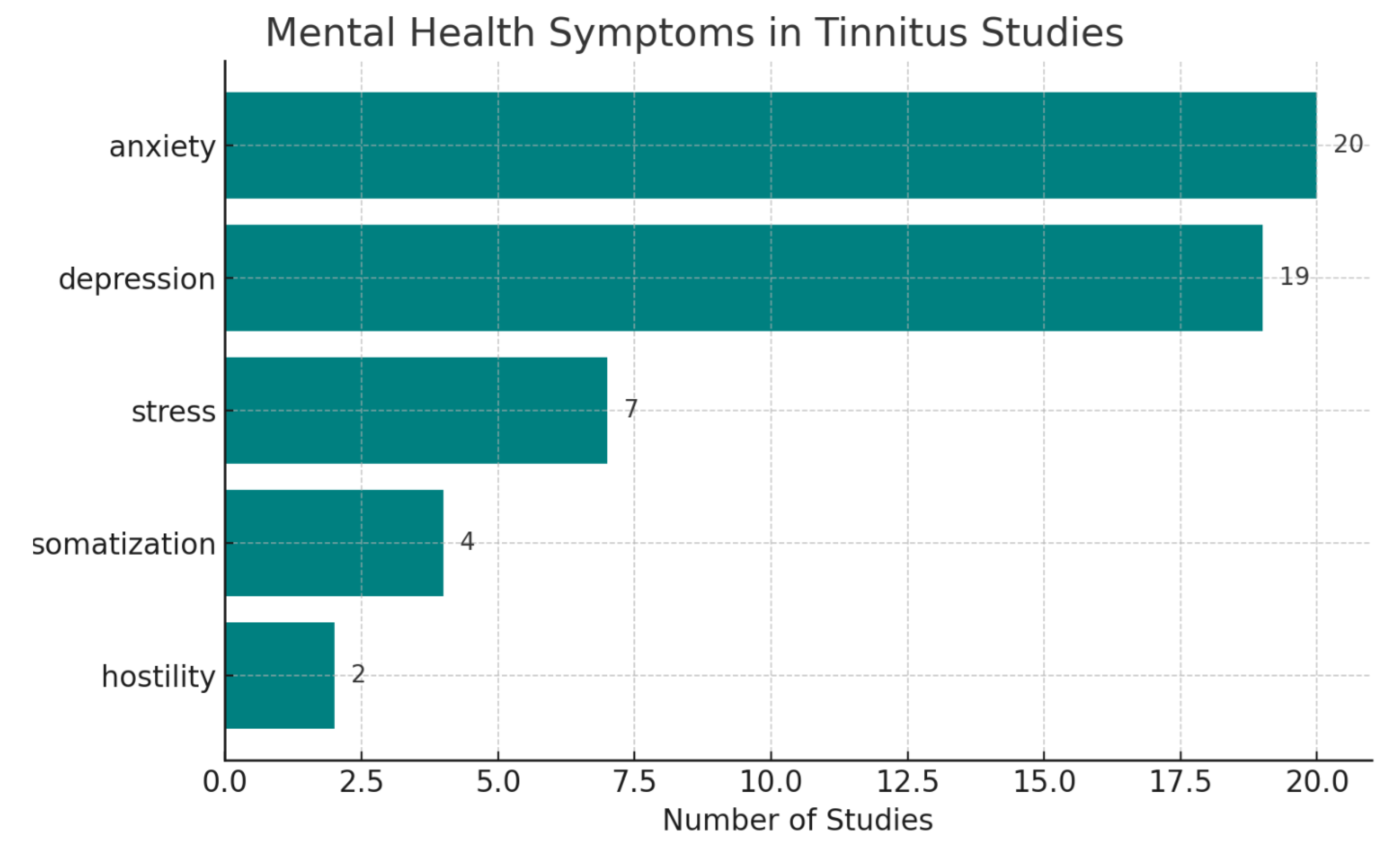
3.2. Associations Between Tinnitus and Psychiatric Comorbidities
3.3. Tinnitus Treatments and Their Impact on Psychiatric Comorbidities
3.4. Psychiatric Comorbidities Treatments and Their Impact on Tinnitus
3.5. Quality Assessment of the Identified Studies
4. Discussion
4.1. Principal Results and Comparison with Prior Works
4.2. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
Abbreviations
| CBT | Cognitive behavioral therapy |
| CBTi | CBT for insomnia |
| EMDR | Eye movement desensitization and reprocessing |
| ENT | Ear, Nose, Throat |
| GWAS | Genome-wide association study |
| HADS | Hospital Anxiety and Depression Scale |
| JBI | Joanna Briggs Institute |
| MMAT | Mixed Methods Appraisal Tool |
| PRISMA-ScR | Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews |
| PTSD | Post-traumatic stress disorder |
| SAS | Self-Rating Anxiety Scale |
| SDS | Self-Rating Depression Scale |
| SSRI | Selective Serotonin Reuptake Inhibitor |
| THI | Tinnitus Handicap Inventory |
References
- Baguley, D.; McFerran, D.; Hall, D. Tinnitus. Lancet 2013, 382, 1600–1607. [Google Scholar] [CrossRef] [PubMed]
- Langguth, B.; Kreuzer, P.M.; Kleinjung, T.; De Ridder, D. Tinnitus: Causes and clinical management. Lancet Neurol. 2013, 12, 920–930. [Google Scholar] [CrossRef] [PubMed]
- Shore, S.E.; Roberts, L.E.; Langguth, B. Maladaptive plasticity in tinnitus--triggers, mechanisms and treatment. Nat. Rev. Neurol. 2016, 12, 150–160. [Google Scholar] [CrossRef] [PubMed]
- Henry, J.A.; Dennis, K.C.; Schechter, M.A. General review of tinnitus: Prevalence, mechanisms, effects, and management. J. Speech Lang. Hear. Res. 2005, 48, 1204–1235. [Google Scholar] [CrossRef]
- Leaver, A.M.; Seydell-Greenwald, A.; Rauschecker, J.P. Auditory-limbic interactions in chronic tinnitus: Challenges for neuroimaging research. Hear Res. 2016, 334, 49–57. [Google Scholar] [CrossRef]
- Rauschecker, J.P.; Leaver, A.M.; Mühlau, M. Tuning out the noise: Limbic-auditory interactions in tinnitus. Neuron 2010, 66, 819–826. [Google Scholar] [CrossRef]
- Jastreboff, P.J. Tinnitus retraining therapy. Prog Brain Res. 2007, 166, 415–423. [Google Scholar] [CrossRef]
- Zöger, S.; Svedlund, J.; Holgers, K.M. Relationship between tinnitus severity and psychiatric disorders. Psychosomatics 2006, 47, 282–288. [Google Scholar] [CrossRef]
- Geocze, L.; Mucci, S.; Abranches, D.C.; Marco, M.A.; Penido Nde, O. Systematic review on the evidences of an association between tinnitus and depression. Braz. J. Otorhinolaryngol. 2013, 79, 106–111. [Google Scholar] [CrossRef]
- Pattyn, T.; Van Den Eede, F.; Vanneste, S.; Cassiers, L.; Veltman, D.J.; Van De Heyning, P.; Sabbe, B.C.G. Tinnitus and anxiety disorders: A review. Hear Res. 2016, 333, 255–265. [Google Scholar] [CrossRef]
- Hesser, H.; Weise, C.; Rief, W.; Andersson, G. The effect of waiting: A meta-analysis of wait-list control groups in trials for tinnitus distress. J. Psychosom. Res. 2011, 70, 378–384. [Google Scholar] [CrossRef] [PubMed]
- Langguth, B. Treatment of tinnitus. Curr. Opin. Otolaryngol. Head Neck Surg. 2015, 23, 361–368. [Google Scholar] [CrossRef] [PubMed]
- De Ridder, D.; Vanneste, S.; Weisz, N.; Londero, A.; Schlee, W.; Elgoyhen, A.B.; Langguth, B. An integrative model of auditory phantom perception: Tinnitus as a unified percept of interacting separable subnetworks. Neurosci. Biobehav. Rev. 2014, 44, 16–32. [Google Scholar] [CrossRef]
- Hiller, W.; Goebel, G. Factors influencing tinnitus loudness and annoyance. Arch. Otolaryngol. Head Neck Surg. 2006, 132, 1323–1330. [Google Scholar] [CrossRef]
- Cima, R.F.; Andersson, G.; Schmidt, C.J.; Henry, J.A. Cognitive-behavioral treatments for tinnitus: A review of the literature. J. Am. Acad. Audiol. 2014, 25, 29–61. [Google Scholar] [CrossRef]
- Hoare, D.J.; Kowalkowski, V.L.; Kang, S.; Hall, D.A. Systematic review and meta-analyses of randomized controlled trials examining tinnitus management. Laryngoscope 2011, 121, 1555–1564. [Google Scholar] [CrossRef]
- Fuller, T.; Cima, R.; Langguth, B.; Mazurek, B.; Vlaeyen, J.W.; Hoare, D.J. Cognitive behavioural therapy for tinnitus. Cochrane Database Syst. Rev. 2020, 1, CD012614. [Google Scholar] [CrossRef]
- Hong, Q.N.; Pluye, P.; Fàbregues, S.; Bartlett, G.; Boardman, F.; Cargo, M.; Dagenais, P.; Gagnon, M.P.; Griffiths, F.; Nicolau, B.; et al. Improving the content validity of the mixed methods appraisal tool: A modified e-Delphi study. J. Clin. Epidemiol. 2019, 111, 49–59.e1. [Google Scholar] [CrossRef]
- Munn, Z.; Stone, J.C.; Aromataris, E.; Klugar, M.; Sears, K.; Leonardi-Bee, J.; Barker, T.H. Assessing the risk of bias of quantitative analytical studies: Introducing the vision for critical appraisal within JBI systematic reviews. JBI Evid. Synth. 2023, 21, 467–471. [Google Scholar] [CrossRef]
- Abbas, J.; Aqeel, M.; Jaffar, A.; Nurunnabi, M.; Bano, S. Tinnitus perception mediates the relationship between physiological and psychological problems among patients. J. Exp. Psychopathol. 2019, 10, 2043808719858559. [Google Scholar] [CrossRef]
- Aqeel, M.; Ahmed, A.; Akhtar, T. The mediating role of tinnitus perception between hearing impairment and development of psychological problems in male and female tinnitus patients. Int. J. Human Rights Healthc. 2017, 10, 332–343. [Google Scholar] [CrossRef]
- Han, T.S.; Jeong, J.E.; Park, S.N.; Kim, J.J. Gender Differences Affecting Psychiatric Distress and Tinnitus Severity. Clin. Psychopharmacol. Neurosci. 2019, 17, 113–120. [Google Scholar] [CrossRef] [PubMed]
- Park, E.; Kim, H.; Choi, I.H.; Han, H.M.; Han, K.; Jung, H.H.; Im, G.J. Psychiatric Distress as a Common Risk Factor for Tinnitus and Joint Pain: A National Population-Based Survey. Clin. Exp. Otorhinolaryngol. 2020, 13, 234–240. [Google Scholar] [CrossRef] [PubMed]
- Hackenberg, B.; Döge, J.; O’Brien, K.; Bohnert, A.; Lackner, K.J.; Beutel, M.E.; Michal, M.; Münzel, T.; Wild, P.S.; Pfeiffer, N.; et al. Tinnitus and its relation to depression, anxiety, and stress—A population-based cohort study. J. Clin. Med. 2023, 12, 1169. [Google Scholar] [CrossRef]
- Bhatt, I.S.; Wilson, N.; Dias, R.; Torkamani, A. A genome-wide association study of tinnitus reveals shared genetic links to neuropsychiatric disorders. Sci. Rep. 2022, 12, 22511. [Google Scholar] [CrossRef]
- Park, Y.; Shin, S.H.; Byun, S.W.; Lee, Z.Y.; Lee, H.Y. Audiological and psychological assessment of tinnitus patients with normal hearing. Front. Neurol. 2023, 13, 1102294. [Google Scholar] [CrossRef]
- Beukes, E.W.; Chundu, S.; Ratinaud, P.; Andersson, G.; Manchaiah, V. Experiential Characteristics among Individuals with Tinnitus Seeking Online Psychological Interventions: A Cluster Analysis. Brain Sci. 2022, 12, 1221. [Google Scholar] [CrossRef]
- Chen, X.; Ren, L.; Xue, X.; Yu, N.; Liu, P.; Shen, W.; Zhou, H.; Wang, B.; Zhou, J.; Yang, S.; et al. The Comorbidity of Depression and Anxiety Symptoms in Tinnitus Sufferers: A Network Analysis. Brain Sci. 2023, 13, 583. [Google Scholar] [CrossRef]
- Sahlsten, H.; Taiminen, T.; Karukivi, M.; Sjösten, N.; Nikkilä, J.; Virtanen, J.; Paavola, J.; Joutsa, J.; Niinivirta-Joutsa, K.; Takala, M.; et al. Psychiatric (Axis I) and personality (Axis II) disorders and subjective psychiatric symptoms in chronic tinnitus. Int. J. Audiol. 2018, 57, 302–312. [Google Scholar] [CrossRef]
- Gül, A.I.; Özkırış, M.; Aydin, R.; Şimşek, G.; Saydam, L. Coexistence of anxiety sensitivity and psychiatric comorbidities in patients with chronic tinnitus. Neuropsychiatr. Dis. Treat. 2015, 11, 413–418. [Google Scholar] [CrossRef]
- Gomaa, M.A.; Elmagd, M.H.; Elbadry, M.M.; Kader, R.M. Depression, anxiety and stress scale in patients with tinnitus and hearing loss. Eur. Arch. Otorhinolaryngol. 2014, 271, 2177–2185. [Google Scholar] [CrossRef] [PubMed]
- Xu, Y.; Yao, J.; Zhang, Z.; Wang, W. Association between sleep quality and psychiatric disorders in patients with subjective tinnitus in China. Eur. Arch. Otorhinolaryngol. 2016, 273, 3063–3072. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Qi, M.; Zeng, X.; Cai, W.; Yin, G.; Zhang, S.; Cen, J.; Gu, J.; Yuan, L.; Fang, B.; et al. Social Support and Tinnitus Distress: The Importance of Developing Positive Psychological Qualities in Patients with Chronic Tinnitus. Audiol. Neurootol. 2021, 26, 246–256. [Google Scholar] [CrossRef]
- Koning, H.M. Psychosocial consequences of the loudness of tinnitus. Int. Tinnitus J. 2019, 23, 103–107. [Google Scholar] [CrossRef]
- Jain, S.; Srivastava, A.S.; Madhu Maggu, G.; Pandey, M. Improvement of tinnitus with trifluoperazine in a patient with psychosis and ear disease. Asian J. Psychiatr. 2017, 30, 177–178. [Google Scholar] [CrossRef]
- Alberdi-Páramo, Í.; Ibáñez-Vizoso, J.E.; Saiz-González, M.D. Tinnitus Como Síntoma de Psicosis de Inicio Reciente. A Propósito de un caso. Psiquiatr. Biol. 2018, 25, 68–71. [Google Scholar] [CrossRef]
- Lucas, P. Tinnitus, paranoid psychosis, homicide and the identificate in an amiable man. Psychoanal. Psychother. 2020, 34, 205–227. [Google Scholar] [CrossRef]
- Ibraheem, O.A.; Hassaan, M.R. Psychoacoustic Characteristics of Tinnitus versus Temporal Resolution in Subjects with Normal Hearing Sensitivity. Int. Arch. Otorhinolaryngol. 2017, 21, 144–150. [Google Scholar] [CrossRef][Green Version]
- Weise, C.; Kleinstäuber, M.; Andersson, G. Internet-Delivered Cognitive-Behavior Therapy for Tinnitus: A Randomized Controlled Trial. Psychosom. Med. 2016, 78, 501–510. [Google Scholar] [CrossRef] [PubMed]
- Marks, E.; Hallsworth, C.; Vogt, F.; Klein, H.; McKenna, L. Cognitive behavioural therapy for insomnia (CBTi) as a treatment for tinnitus-related insomnia: A randomised controlled trial. Cogn. Behav. Ther. 2023, 52, 91–109. [Google Scholar] [CrossRef] [PubMed]
- McKenna, L.; Handscomb, L.; Hoare, D.J.; Hall, D.A. A scientific cognitive-behavioral model of tinnitus: Novel conceptualizations of tinnitus distress. Front. Neurol. 2014, 5, 196. [Google Scholar] [CrossRef] [PubMed]
- Luyten, T.R.; Jacquemin, L.; Van Looveren, N.; Declau, F.; Fransen, E.; Cardon, E.; De Bodt, M.; Topsakal, V.; Van de Heyning, P.; Van Rompaey, V.; et al. Bimodal Therapy for Chronic Subjective Tinnitus: A Randomized Controlled Trial of EMDR and TRT Versus CBT and TRT. Front. Psychol. 2020, 11, 2048. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Moore, T.; Phillips, J.S.; Erskine, S.E.; Nunney, I. What has EMDR taught us about the psychological characteristics of tinnitus patients? J. EMDR Pract. Res. 2020, 14, 229–240. [Google Scholar] [CrossRef]
- Crocetti, A.; Ambrosetti, U.; Del Bo, L. Flight or fight tinnitus? Tinnitus coping over time and psychophysiological reactions. Act. Nerv. Super. Rediviva 2018, 60, 49–54. [Google Scholar]
- Ketterer, M.C.; Knopke, S.; Häußler, S.M.; Hildenbrand, T.; Becker, C.; Gräbel, S.; Olze, H. Asymmetric hearing loss and the benefit of cochlear implantation regarding speech perception, tinnitus burden and psychological comorbidities: A prospective follow-up study. Eur. Arch. Otorhinolaryngol. 2018, 275, 2683–2693. [Google Scholar] [CrossRef]
- Frederiksen, T.W.; Ramlau-Hansen, C.H.; Stokholm, Z.A.; Grynderup, M.B.; Hansen, Å.M.; Lund, S.P.; Kristiansen, J.; Vestergaard, J.M.; Bonde, J.P.; Kolstad, H.A. Occupational noise exposure, psychosocial working conditions and the risk of tinnitus. Int. Arch. Occup. Environ. Health 2017, 90, 217–225. [Google Scholar] [CrossRef]
- Liu, J.; Liu, Y.; Ma, T.; Gao, M.; Zhang, R.; Wu, J.; Zou, J.; Liu, S.; Xie, H. Subjective perceptions and psychological distress associated with the deep underground: A cross-sectional study in a deep gold mine in China. Medicine 2019, 98, e15571. [Google Scholar] [CrossRef]
- Papazian, B. Acouphènes et phénomènes de séparation, un essai métapsychologique. Rev. Fr. Psychanal. 2015, 79, 538–546. [Google Scholar] [CrossRef]
- Salviati, M.; Bersani, F.S.; Terlizzi, S.; Melcore, C.; Panico, R.; Romano, G.F.; Valeriani, G.; Macrì, F.; Altissimi, G.; Mazzei, F.; et al. Tinnitus: Clinical experience of the psychosomatic connection. Neuropsychiatr. Dis. Treat. 2014, 10, 267–275. [Google Scholar] [CrossRef]
- Aazh, H.; Moore, B.C.J. Factors Associated With Depression in Patients With Tinnitus and Hyperacusis. Am. J. Audiol. 2017, 26, 562–569. [Google Scholar] [CrossRef]
- Jasper, K.; Weise, C.; Conrad, I.; Andersson, G.; Hiller, W.; Kleinstäuber, M. Internet-based guided self-help versus group cognitive behavioral therapy for chronic tinnitus: A randomized controlled trial. Psychother. Psychosom. 2014, 83, 234–246. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Seydel, C.; Zirke, N.; Haupt, H.; Szczepek, A.; Olze, H.; Mazurek, B. Psychometrische Testverfahren in der Tinnitusdiagnostik [Psychometric instruments for the diagnosis of tinnitus]. HNO 2012, 60, 732–742. [Google Scholar] [CrossRef] [PubMed]
- Ziai, K.; Moshtaghi, O.; Mahboubi, H.; Djalilian, H.R. Tinnitus Patients Suffering from Anxiety and Depression: A Review. Int. Tinnitus J. 2017, 21, 68–73. [Google Scholar] [CrossRef] [PubMed]
- Salazar, J.W.; Meisel, K.; Smith, E.R.; Quiggle, A.; McCoy, D.B.; Amans, M.R. Depression in Patients with Tinnitus: A Systematic Review. Otolaryngol. Head Neck Surg. 2019, 161, 28–35. [Google Scholar] [CrossRef]
- De Ridder, D.; Schlee, W.; Vanneste, S.; Londero, A.; Weisz, N.; Kleinjung, T.; Shekhawat, G.S.; Elgoyhen, A.B.; Song, J.J.; Andersson, G.; et al. Tinnitus and tinnitus disorder: Theoretical and operational definitions (an international multidisciplinary proposal). Prog. Brain Res. 2021, 260, 1–25. [Google Scholar] [CrossRef] [PubMed]
- De Ridder, D.; Vanneste, S.; Song, J.J.; Adhia, D. Tinnitus and the Triple Network Model: A Perspective. Clin. Exp. Otorhinolaryngol. 2022, 15, 205–212. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Mazurek, B.; Szczepek, A.J.; Hebert, S. Stress and tinnitus. HNO 2015, 63, 258–265. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Arsenault, V.; Larouche, J.; Désilets, M.; Hudon, M.-A.; Hudon, A. When the Mind Meets the Ear: A Scoping Review on Tinnitus and Clinically Measured Psychiatric Comorbidities. J. Clin. Med. 2025, 14, 3785. https://doi.org/10.3390/jcm14113785
Arsenault V, Larouche J, Désilets M, Hudon M-A, Hudon A. When the Mind Meets the Ear: A Scoping Review on Tinnitus and Clinically Measured Psychiatric Comorbidities. Journal of Clinical Medicine. 2025; 14(11):3785. https://doi.org/10.3390/jcm14113785
Chicago/Turabian StyleArsenault, Virginie, Jacob Larouche, Marie Désilets, Marc-Antoine Hudon, and Alexandre Hudon. 2025. "When the Mind Meets the Ear: A Scoping Review on Tinnitus and Clinically Measured Psychiatric Comorbidities" Journal of Clinical Medicine 14, no. 11: 3785. https://doi.org/10.3390/jcm14113785
APA StyleArsenault, V., Larouche, J., Désilets, M., Hudon, M.-A., & Hudon, A. (2025). When the Mind Meets the Ear: A Scoping Review on Tinnitus and Clinically Measured Psychiatric Comorbidities. Journal of Clinical Medicine, 14(11), 3785. https://doi.org/10.3390/jcm14113785







