Optimizing Imaging Techniques for Left Atrial Appendage Closure: Insights and Emerging Directions
Abstract
1. Introduction
2. Role of Imaging in Left Atrial Appendage Closure
2.1. Pre-Procedural Imaging: Anatomical Assessment and Patient Selection
- Chicken Wing: A dominant lobe bending <100° in its proximal segment.
- Cactus: A central lobe <40 mm with secondary lobes and recesses.
- Windsock: A dominant lobe >40 mm with secondary lobes bending >100 mm.
- Cauliflower: A short, irregular lobe <40 mm with multiple recesses.
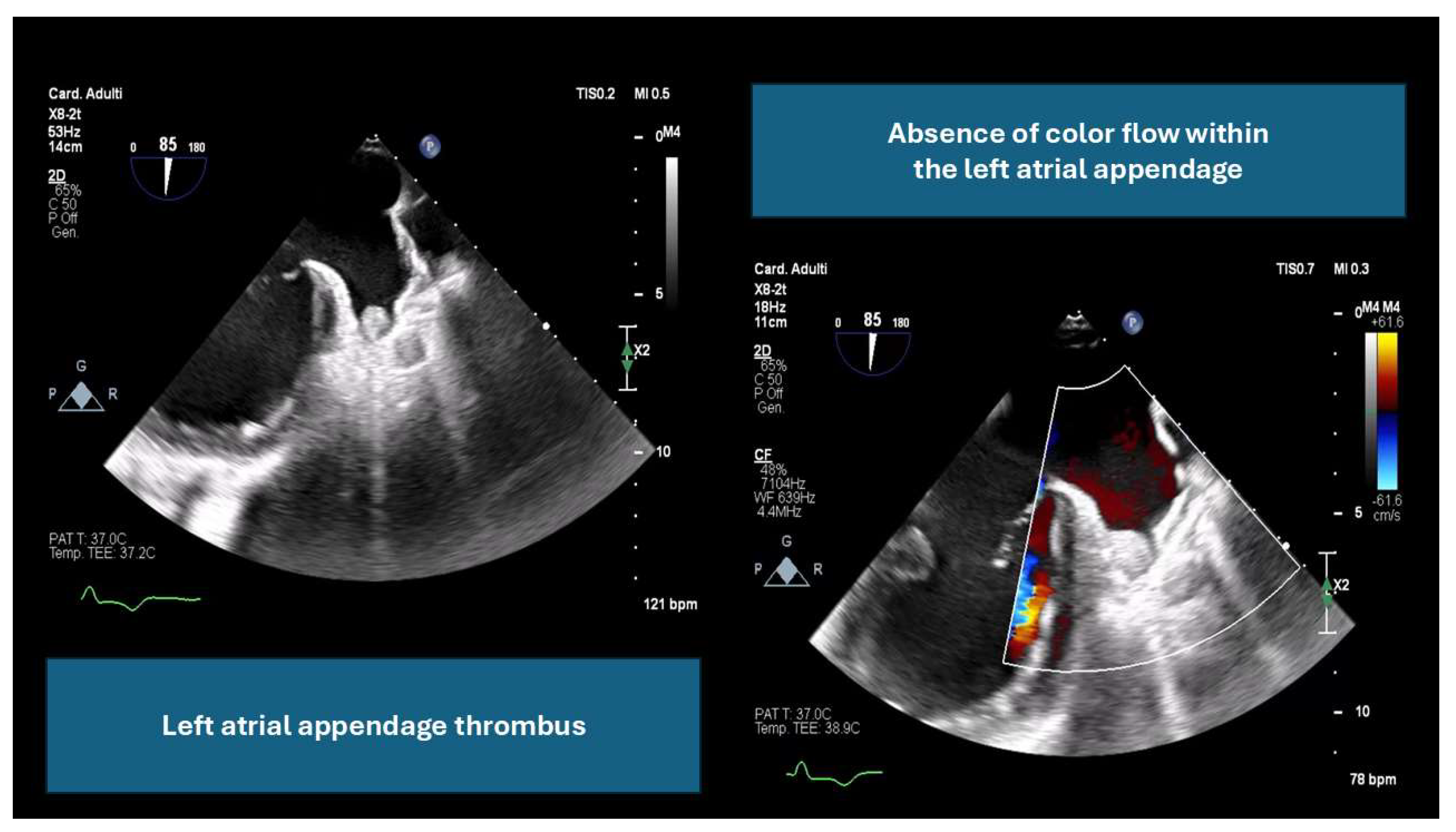
- By ruling out LAA thrombus, which can increase the risk of embolic events (an example is provided in Figure 1).
- By providing detailed anatomical assessment, including LAA dimensions, peak emptying velocity, and surrounding structures.
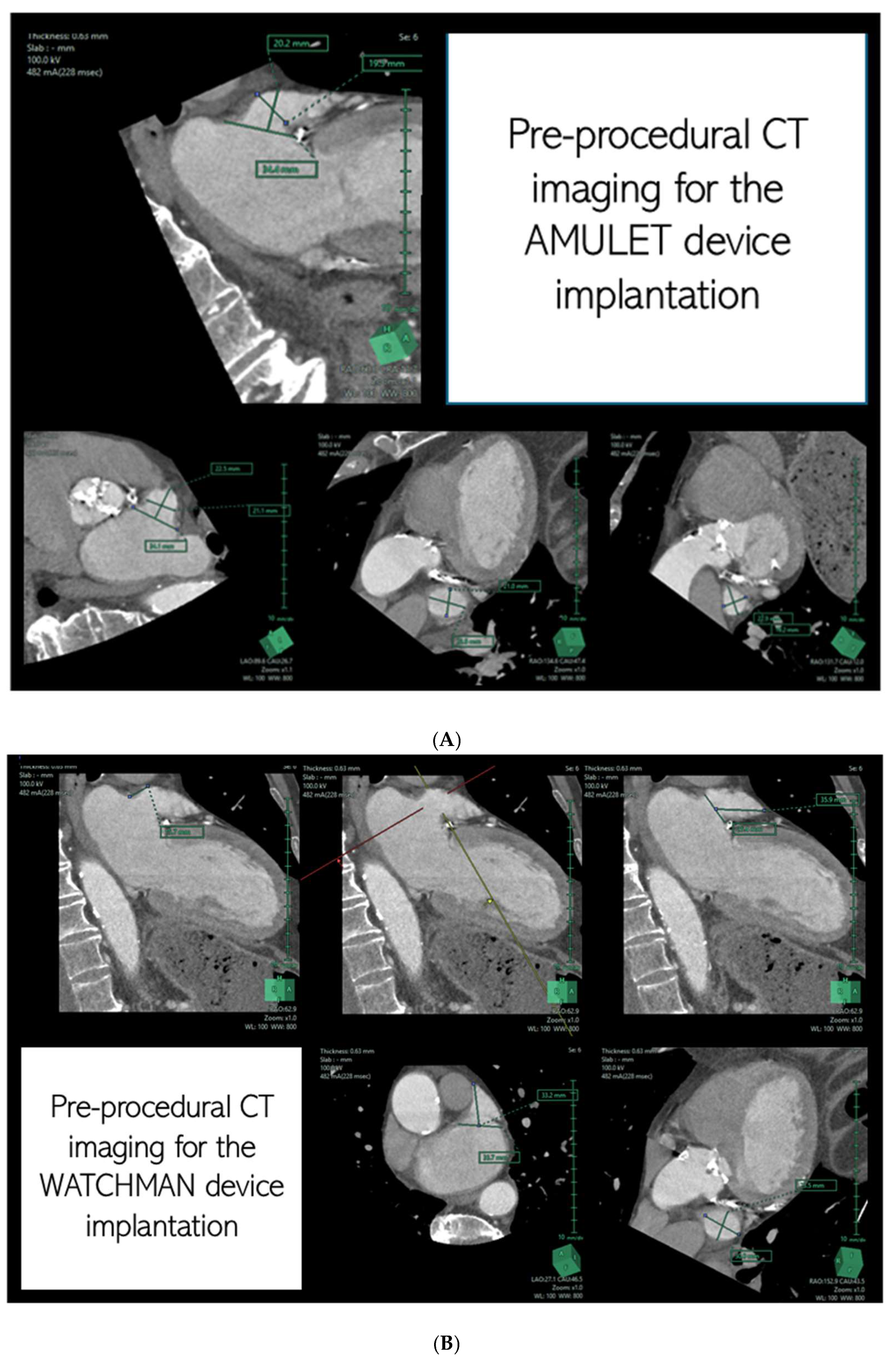
- By determining optimal fluoroscopic angles and guiding transseptal puncture locations for accurate device delivery.
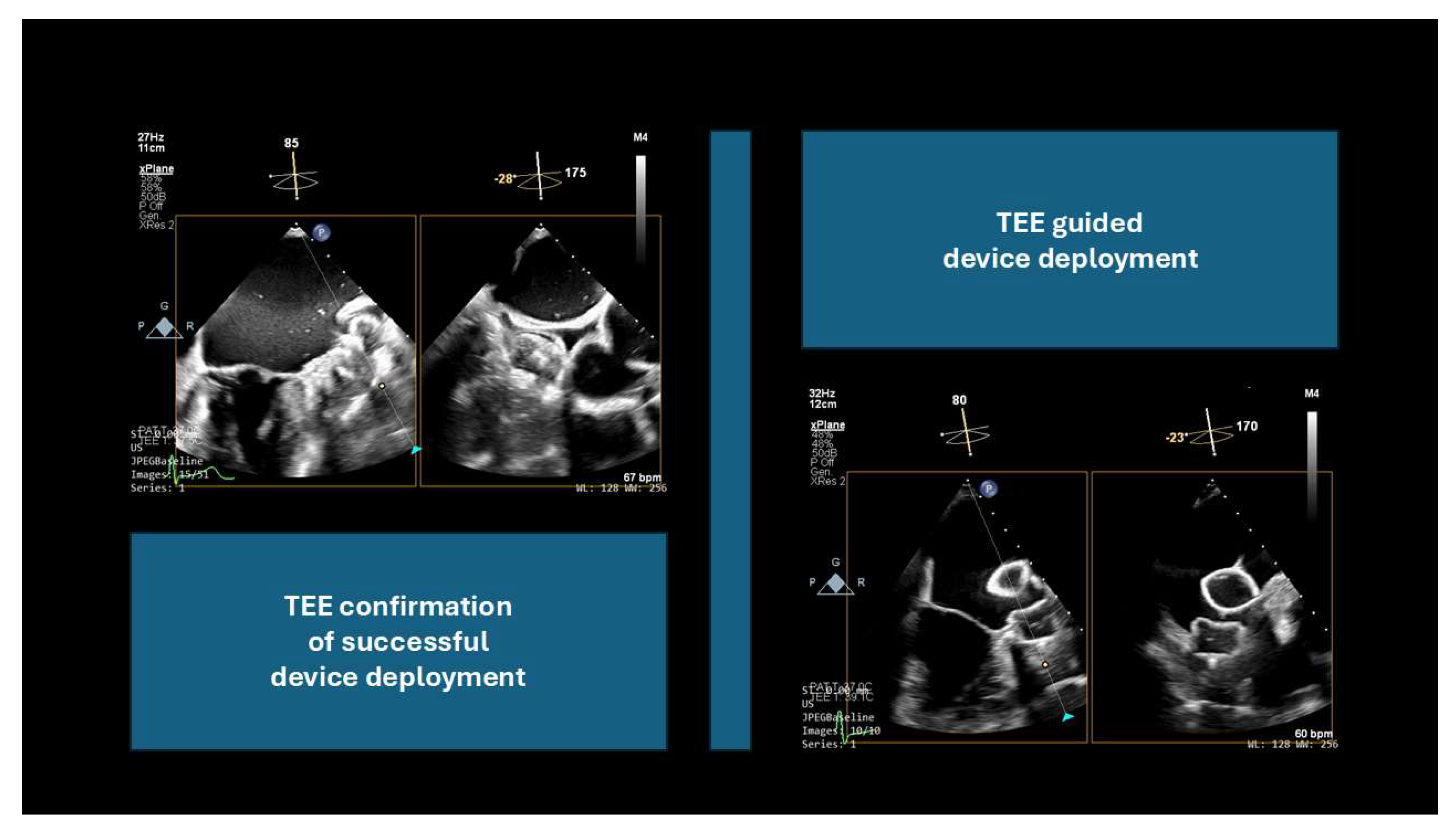
2.2. Intra-Procedural Imaging: Guidance During the Intervention
2.3. Post-Procedural Imaging: Evaluating Success and Follow-Up
3. Current Imaging Techniques: Strengths and Limitations
TEE Versus CT: Technical Challenges and Practical Considerations
- Reduced total fluoroscopy time;
- Lower risk of periprosthetic leaks;
- Fewer devices used and shorter procedural times;
- Comparable device implantation success rates.
- Reduced anesthesia-related risks (avoiding endotracheal intubation);
- Shorter procedural times (from femoral access to completion);
- Faster patient recovery;
- Decreased number of personnel in the operating room (eliminating the need for an anesthesiologist and imaging cardiologist).
- A steep learning curve, particularly for interventional cardiologists unfamiliar with left atrial imaging;
- High costs of ICE catheters and equipment;
- Uncertainty regarding device release criteria as TEE has traditionally been the gold standard for confirming device positioning.
4. Innovation and Emerging Development
4.1. Three-Dimensional and Four-Dimensional Ultrasound
4.2. Three-Dimensional Printing
4.3. Fusion Imaging
4.4. AI and Deep Learning
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Van Gelder, I.C.; Rienstra, M.; Bunting, K.V.; Casado-Arroyo, R.; Caso, V.; Crijns, H.J.G.M.; De Potter, T.J.R.; Dwight, J.; Guasti, L.; Hanke, T.; et al. 2024 ESC Guidelines for the management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS). Eur. Heart J. 2024, 45, 3314–3414. [Google Scholar] [CrossRef] [PubMed]
- Holmes, D.R.; Reddy, V.Y.; Turi, Z.G.; Doshi, S.K.; Sievert, H.; Buchbinder, M.; Mullin, C.M.; Sick, P.; PROTECT AF Investigators. Percutaneous closure of the left atrial appendage versus warfarin therapy for prevention of stroke in patients with atrial fibrillation: A randomised non-inferiority trial. Lancet 2009, 374, 534–542, Erratum in Lancet 2009, 374, 1596. [Google Scholar] [CrossRef] [PubMed]
- Osmancik, P.; Herman, D.; Neuzil, P.; Hala, P.; Taborsky, M.; Kala, P.; Poloczek, M.; Stasek, J.; Haman, L.; Branny, M.; et al. Left Atrial Appendage Closure Versus Direct Oral Anticoagulants in High-Risk Patients with Atrial Fibrillation. J. Am. Coll. Cardiol. 2020, 75, 3122–3135. [Google Scholar] [CrossRef] [PubMed]
- Lakkireddy, D.; Thaler, D.; Ellis, C.R.; Swarup, V.; Sondergaard, L.; Carroll, J.; Gold, M.R.; Hermiller, J.; Diener, H.C.; Schmidt, B.; et al. Amplatzer Amulet Left Atrial Appendage Occluder Versus Watchman Device for Stroke Prophylaxis (Amulet IDE): A Randomized, Controlled Trial. Circulation 2021, 144, 1543–1552. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Joglar, J.A.; Chung, M.K.; Armbruster, A.L.; Benjamin, E.J.; Chyou, J.Y.; Cronin, E.M.; Deswal, A.; Eckhardt, L.L.; Goldberger, Z.D.; Gopinathannair, R.; et al. 2023 ACC/AHA/ACCP/HRS Guideline for the Diagnosis and Management of Atrial Fibrillation: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation 2024, 149, e1–e156. [Google Scholar] [CrossRef] [PubMed]
- Chao, T.F.; Joung, B.; Takahashi, Y.; Lim, T.W.; Choi, E.K.; Chan, Y.H.; Guo, Y.; Sriratanasathavorn, C.; Oh, S.; Okumura, K.; et al. 2021 Focused Update Consensus Guidelines of the Asia Pacific Heart Rhythm Society on Stroke Prevention in Atrial Fibrillation: Executive Summary. Thromb. Haemost. 2022, 122, 20–47. [Google Scholar] [CrossRef] [PubMed]
- Garg, J.; Kabra, R.; Gopinathannair, R.; Di Biase, L.; Wang, D.D.; Saw, J.; Hahn, R.; Freeman, J.V.; Ellis, C.R.; Lakkireddy, D. State of the Art in Left Atrial Appendage Occlusion. JACC Clin. Electrophysiol. 2024, 11, 602–641. [Google Scholar] [CrossRef] [PubMed]
- Martinsen, B.J.; Lohr, J.L. Cardiac development. In Handbook of Cardiac Anatomy, Physiology, and Devices; Iaizzo, P., Ed.; Humana Press: New York, NY, USA, 2005; pp. 15–23. [Google Scholar]
- Wang, Y.; Di Biase, L.; Horton, R.P.; Nguyen, T.; Morhanty, P.; Natale, A. Left atrial appendage studied by computed tomography to help planning for appendage closure device placement. J. Cardiovasc. Electrophysiol. 2010, 21, 973–982. [Google Scholar] [CrossRef] [PubMed]
- Cresti, A.; Camara, O. Left Atrial Thrombus-Are All Atria and Appendages Equal? Interv. Cardiol. Clin. 2022, 11, 121–134. [Google Scholar] [CrossRef] [PubMed]
- Berti, S.; Paradossi, U.; Meucci, F.; Trianni, G.; Tzikas, A.; Rezzaghi, M.; Stolkova, M.; Palmieri, C.; Mori, F.; Santoro, G. Periprocedural intracardiac echocardiography for left atrial appendage closure: A dual-center experience. JACC Cardiovasc. Interv. 2014, 7, 1036–1044. [Google Scholar] [CrossRef] [PubMed]
- Wang, B.; Zhang, L.; Sun, W.; He, L.; Wang, X.; Lv, Q.; Li, Y.; Xie, M. Transnasal Transesophageal Echocardiography Guidance for Percutaneous Left Atrial Appendage Closure. Ann. Thorac. Surg. 2019, 108, e161–e164. [Google Scholar] [CrossRef] [PubMed]
- Hajhosseiny, R.; Ariff, B.; Cole, G.; Koa-Wing, M.; Pabari, P.; Sutaria, N.; Qureshi, N.; Kanagaratnam, P.; Rana, B. Advancements in 3D Transoesophageal Echocardiography (TOE) and Computed Tomography (CT) for Stroke Prevention in Left Atrial Appendage Occlusion Interventions. J. Clin. Med. 2024, 13, 6899. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Yosefy, C.; Laish-Farkash, A.; Azhibekov, Y.; Khalameizer, V.; Brodkin, B.; Katz, A. A New Method for Direct Three-Dimensional Measurement of Left Atrial Appendage Dimensions during Transesophageal Echocardiography. Echocardiography 2016, 33, 69–76. [Google Scholar] [CrossRef] [PubMed]
- Serpa, F.; Rivera, A.; Fernandes, J.M.; Braga, M.A.P.; Araújo, B.; Ferreira Felix, I.; Ferro, E.G.; Zimetbaum, P.J.; d’Avila, A.; Kramer, D.B. Intracardiac vs transesophageal echocardiography for left atrial appendage occlusion: An updated systematic review and meta-analysis. Heart Rhythm. 2025, 22, 786–795. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Q.; Song, H.; Zhang, L.; Deng, Q.; Chen, J.; Hu, B.; Wang, Y.; Guo, R. Roles of real-time three-dimensional transesophageal echocardiography in peri-operation of transcatheter left atrial appendage closure. Medicine 2017, 96, e5637. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Schmidt-Salzmann, M.; Meincke, F.; Kreidel, F.; Spangenberg, T.; Ghanem, A.; Kuck, K.H.; Bergmann, M.W. Improved Algorithm for Ostium Size Assessment in Watchman Left Atrial Appendage Occlusion Using Three-Dimensional Echocardiography. J. Invasive Cardiol. 2017, 29, 232–238. [Google Scholar] [PubMed]
- Velagapudi, P.; Turagam, M.K.; Kolte, D.; Khera, S.; Gupta, T.; Garg, J.; Abbott, J.D.; George, I.; Khalique, O.; Vahl, T.; et al. Intracardiac vs transesophageal echocardiography for percutaneous left atrial appendage occlusion: A meta-analysis. J. Cardiovasc. Electrophysiol. 2019, 30, 461–467. [Google Scholar] [CrossRef] [PubMed]
- Glikson, M.; Wolff, R.; Hindricks, G.; Mandrola, J.; Camm, A.J.; Lip, G.Y.H.; Fauchier, L.; Betts, T.R.; Lewalter, T.; Saw, J.; et al. EHRA/EAPCI expert consensus statement on catheter-based left atrial appendage occlusion—An update. EuroIntervention 2020, 15, 1133–1180. [Google Scholar] [CrossRef] [PubMed]
- Holmes, D.R.; Korsholm, K.; Rodés-Cabau, J.; Saw, J.; Berti, S.; Alkhouli, M.A. Left atrial appendage occlusion. EuroIntervention 2023, 18, e1038–e1065. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ciobotaru, V.; Combes, N.; Martin, C.A.; Marijon, E.; Maupas, E.; Bortone, A.; Bruguière, E.; Thambo, J.B.; Teiger, E.; Pujadas-Berthault, P.; et al. Left atrial appendage occlusion simulation based on three-dimensional printing: New insights into outcome and technique. EuroIntervention 2018, 14, 176–184. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Qingyao; Bingshen; Shu, M.; Lizhong; Wang, X.; Song, Z. Application of 3D printing technology to left atrial appendage occlusion. Int. J. Cardiol. 2017, 231, 258–263. [Google Scholar] [CrossRef] [PubMed]
- Eng, M.H.; Wang, D.D.; Greenbaum, A.B.; Gheewala, N.; Kupsky, D.; Aka, T.; Song, T.; Kendall, B.J.; Wyman, J.; Myers, E.; et al. Prospective, randomized comparison of 3-dimensional computed tomography guidance versus TEE data for left atrial appendage occlusion (PRO3DLAAO). Catheter. Cardiovasc. Interv. 2018, 92, 401–407. [Google Scholar] [CrossRef] [PubMed]
- Croix, G.S.; Zaidi, S.I.; Loescher, V.S.; Mihos, C.G. Computed Tomography-Derived Three-Dimensional Printed Models versus Two-Dimensional Transesophageal Echocardiography for Left Atrial Appendage Occlusion Device Planning: A Systematic Review and Meta-Analysis. J. Atr. Fibrillation 2020, 13, 2433. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Korsholm, K.; Jensen, J.M.; Nielsen-Kudsk, J.E. Cardiac Computed Tomography for Left Atrial Appendage Occlusion: Acquisition, Analysis, Advantages, and Limitations. Interv. Cardiol. Clin. 2018, 7, 229–242. [Google Scholar] [CrossRef] [PubMed]
- Korsholm, K.; Jensen, J.M.; Nørgaard, B.L.; Samaras, A.; Saw, J.; Berti, S.; Tzikas, A.; Nielsen-Kudsk, J.E. Peridevice Leak Following Amplatzer Left Atrial Appendage Occlusion: Cardiac Computed Tomography Classification and Clinical Outcomes. JACC Cardiovasc. Interv. 2021, 14, 83–93. [Google Scholar] [CrossRef] [PubMed]
- Martinez, M.W.; Kirsch, J.; Williamson, E.E.; Syed, I.S.; Feng, D.; Ommen, S.; Packer, D.L.; Brady, P.A. Utility of nongated multidetector computed tomography for detection of left atrial thrombus in patients undergoing catheter ablation of atrial fibrillation. JACC Cardiovasc. Imaging. 2009, 2, 69–76. [Google Scholar] [CrossRef] [PubMed]
- Korsholm, K.; Berti, S.; Iriart, X.; Saw, J.; Wang, D.D.; Cochet, H.; Chow, D.; Clemente, A.; De Backer, O.; Møller Jensen, J.; et al. Expert Recommendations on Cardiac Computed Tomography for Planning Transcatheter Left Atrial Appendage Occlusion. JACC Cardiovasc. Interv. 2020, 13, 277–292. [Google Scholar] [CrossRef] [PubMed]
- Kaafarani, M.; Saw, J.; Daniels, M.; Song, T.; Rollet, M.; Kesinovic, S.; Lamorgese, T.; Kubiak, K.; Qi, Z.; Pantelic, M.; et al. Role of CT imaging in left atrial appendage occlusion for the WATCHMAN™ device. Cardiovasc. Diagn. Ther. 2020, 10, 45–58. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Taylor, S.A.; Carucci, L.R. The role of imaging in obesity special feature. Br. J. Radiol. 2018, 91, 20189002. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Hemam, M.E.; Kuroki, K.; Schurmann, P.A.; Dave, A.S.; Rodríguez, D.A.; Sáenz, L.C.; Reddy, V.Y.; Valderrábano, M. Left atrial appendage closure with the Watchman device using intracardiac vs transesophageal echocardiography: Procedural and cost considerations. Heart Rhythm. 2019, 16, 334–342. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Freitas-Ferraz, A.B.; Bernier, M.; Vaillancourt, R.; Ugalde, P.A.; Nicodème, F.; Paradis, J.M.; Champagne, J.; O’Hara, G.; Junquera, L.; Del Val, D.; et al. Safety of Transesophageal Echocardiography to Guide Structural Cardiac Interventions. J. Am. Coll. Cardiol. 2020, 75, 3164–3173. [Google Scholar] [CrossRef] [PubMed]
- Ferro, E.G.; Alkhouli, M.; Nair, D.G.; Kapadia, S.R.; Hsu, J.C.; Gibson, D.N.; Freeman, J.V.; Price, M.J.; Roy, K.; Allocco, D.J.; et al. Intracardiac vs. Transesophageal Echocardiography for Left Atrial Appendage Occlusion with Watchman FLX in the U.S. JACC Clin. Electrophysiol. 2023, 9, 2587–2599. [Google Scholar] [CrossRef] [PubMed]
- Diaz, J.C.; Bastidas, O.; Duque, M.; Marín, J.E.; Aristizabal, J.; Niño, C.D.; Hoyos, C.; Matos, C.D.; Gabr, M.; Steiger, N.A.; et al. Impact of intracardiac echocardiography versus transesophageal echocardiography guidance on left atrial appendage occlusion procedures: A meta-analysis. J. Cardiovasc. Electrophysiol. 2024, 35, 44–57. [Google Scholar] [CrossRef] [PubMed]
- He, G.; Liu, H.; Huang, X.; Deng, X.; Yang, G.; Luo, D.; Cai, L. Intracardiac versus transesophageal echocardiography for diagnosis of left atrial appendage thrombosis in atrial fibrillation: A meta-analysis. Clin. Cardiol. 2021, 44, 1416–1421. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ellis, C.R.; Jackson, G.G.; Kanagasundram, A.N.; Mansour, M.; Sutton, B.; Houle, V.M.; Kar, S.; Doshi, S.; Osorio, J. Left atrial appendage closure in patients with prohibitive anatomy: Insights from PINNACLE FLX. Heart Rhythm. 2021, 18, 1153–1161. [Google Scholar] [CrossRef]
- Neuzner, J.; Dietze, T.; Paliege, R.; Möller, M.; Saeed, G.; Gradaus, R. Left atrial appendage closure with the Amplatzer™ Cardiac Plug: Rationale for a higher degree of device oversizing at implantation. Cardiol. J. 2015, 22, 201–205. [Google Scholar] [CrossRef]
- Ayhan, H.; Mohanty, S.; Gedikli, Ö.; Trivedi, C.; Canpolat, U.; Tapia, A.C.; Chen, Q.; Della Rocca, D.G.; Gianni, C.; Salwan, A.; et al. A simple method to detect leaks after left atrial appendage occlusion with Watchman. J. Cardiovasc. Electrophysiol. 2020, 31, 2338–2343. [Google Scholar] [CrossRef]
- Treb, W.; Mitręga, K.; Podolecki, T.; Szymała, M.; Leopold-Jadczyk, A.; Kukulski, T.; Kalarus, Z. Two-dimensional versus three-dimensional transesophageal echocardiography in percutaneous left atrial appendage occlusion. Cardiol. J. 2019, 26, 687–695. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Shah, S.J.; Bardo, D.M.; Sugeng, L.; Weinert, L.; Lodato, J.A.; Knight, B.P.; Lopez, J.J.; Lang, R.M. Real-time three-dimensional transesophageal echocardiography of the left atrial appendage: Initial experience in the clinical setting. J. Am. Soc. Echocardiogr. 2008, 21, 1362–1368. [Google Scholar] [CrossRef] [PubMed]
- Nucifora, G.; Faletra, F.F.; Regoli, F.; Pasotti, E.; Pedrazzini, G.; Moccetti, T.; Auricchio, A. Evaluation of the left atrial appendage with real-time 3-dimensional transesophageal echocardiography: Implications for catheter-based left atrial appendage closure. Circ. Cardiovasc. Imaging 2011, 4, 514–523. [Google Scholar] [CrossRef]
- Faletra, F.F.; Pedrazzini, G.; Pasotti, E.; Muzzarelli, S.; Dequarti, M.C.; Murzilli, R.; Schlossbauer, S.A.; Slater, I.P.; Moccetti, T. 3D TEE during catheter-based interventions. JACC Cardiovasc. Imaging 2014, 7, 292–308. [Google Scholar] [CrossRef] [PubMed]
- Liang, G.; Xu, B.; Wang, S.; Li, C.; Zhong, G. Imaging with intracardiac echocardiography compared to transesophageal echocardiography during left atrial appendage occlusion. Rev. Cardiovasc. Med. 2020, 21, 93–101. [Google Scholar] [CrossRef] [PubMed]
- Kerut, E.K.; Hanawalt, C.; McKinnie, J. Transesophageal echocardiography during pulmonary vein cryoballoon ablation for atrial fibrillation. Echocardiography 2015, 32, 281–290. [Google Scholar] [CrossRef]
- Wang, Y.; Zhao, Y.; Zhou, K.; Zei, P.C.; Wang, Y.; Cheng, H.; Chen, S.; Tao, Y.; Mao, Y.; Liu, Q.; et al. Intracardiac echocardiography is a safe and efective alternative to transesophageal echocardiography for lef atrial appendage thrombus evaluation at the time of atrial fbrillation ablation: Te ICE-TEE study. Pacing. Clin. Electrophysiol. 2023, 46, 3–10. [Google Scholar] [CrossRef]
- Ge, J.; Chen, T.; Ma, C.; Maduray, K.; Zhong, J. Can intracardiac echocardiography completely replace transesophageal echocardiography to guide lef atrial appendage closure?—The comparisons of intracardiac echocardiography with transesophageal echocardiography. J. Card. Surg. 2022, 37, 2766–2775. [Google Scholar] [CrossRef]
- Ma, Y.; Guo, L.; Li, J.; Liu, H.; Xu, J.; Du, H.; Wang, Y.; Li, H.; Yi, F. Iatrogenic atrial septal defect afer intracardiac echocardiography-guided lef atrial appendage closure: Incidence, size, and clinical outcomes. J. Clin. Med. 2022, 12, 160. [Google Scholar] [CrossRef]
- Sharma, A.; Bertog, S.; Tolakanahalli, V.; Mbai, M.; Chandrashekhar, Y.S. 4D intracardiac echocardiography-guided LA appendage closure under conscious sedation: Initial experience and procedural technique. JACC Cardiovasc. Imaging 2021, 14, 2254–2259. [Google Scholar] [CrossRef]
- Serpa, F.; Rivera, A.; Fernandes, J.M.; Braga, M.A.P.; Araújo, B.; Ferreira Felix, I.; Ferro, E.G.; Zimetbaum, P.J.; d’Avila, A.; Kramer, D.B. Intracardiac echocardiography versus transesophageal echocardiography for left atrial appendage closure: An updated meta-analysis and systematic review. Am. J. Cardiovasc. Dis. 2020, 10, 538–547. [Google Scholar]
- Gianni, C.; Horton, R.P.; Della Rocca, D.G.; Mohanty, S.; Al-Ahmad, A.; Bassiouny, M.A.; Burkhardt, J.D.; Gallinghouse, G.J.; Hranitzky, P.M.; Sanchez, J.E.; et al. Intracardiac echocardiography- versus transesophageal echocardiography-guided left atrial appendage occlusion with Watchman FLX. Cardiovasc. Electrophysiol. 2021, 32, 2781–2784. [Google Scholar] [CrossRef]
- Korsholm, K.; Jensen, J.M.; Nielsen-Kudsk, J.E. Intracardiac echocardiography from the left atrium for procedural guidance of transcatheter left atrial appendage occlusion. JACC Cardiovasc. Interv. 2017, 10, 2198–2206. [Google Scholar] [CrossRef]
- Masson, J.B.; Kouz, R.; Riahi, M.; Nguyen Thanh, H.K.; Potvin, J.; Naim, C.; Salem, R.; Raymond, J.M. Transcatheter left atrial appendage closure using intracardiac echocardiographic guidance from the left atrium. Can. J. Cardiol. 2015, 31, 1497.e7–1497.e14. [Google Scholar] [CrossRef]
- Della Rocca, D.G.; Magnocavallo, M.; Van Niekerk, C.J.; Gilhofer, T.; Ha, G.; D’Ambrosio, G.; Mohanty, S.; Gianni, C.; Galvin, J.; Vetta, G.; et al. Prognostic value of chronic kidney disease in patients undergoing left atrial append age occlusion. Europace 2023, 25, euad315. [Google Scholar] [CrossRef] [PubMed]
- Turagam, M.K.; Neuzil, P.; Petru, J.; Hala, P.; Mraz, T.; Baroch, J.; Lekesova, V.; Prokopova, M.; Dukkipati, S.R.; Reddy, V.Y. Intracardiac echocardiography-guided implantation of the Watchman FLX lef atrial appendage closure device. J. Cardiovasc. Electrophysiol. 2021, 32, 717–725. [Google Scholar] [CrossRef]
- Alqahtani, F.; Bhirud, A.; Aljohani, S.; Mills, J.; Kawsara, A.; Runkana, A.; Alkhouli, M. Intracardiac versus transesophageal echocardiography to guide transcatheter closure of interatrial communications: Nationwide trend and comparative analysis. J. Interv. Cardiol. 2017, 30, 234–241. [Google Scholar] [CrossRef] [PubMed]
- Khalili, H.; Patton, M.; Taii, H.A.; Bansal, P.; Brady, M.; Taylor, J.; Gurung, A.; Maini, B. 4D volume intracardiac echocardiography for intraprocedural guidance of transcatheter lef atrial appendage closure. J. Atr. Fibrillation. 2019, 12, 2200. [Google Scholar] [CrossRef]
- Della Rocca, D.G.; Magnocavallo, M.; Gianni, C.; Mohanty, S.; Al-Ahmad, A.; Bassiouny, M.; Denora, M.; La Fazia, V.M.; Lavalle, C.; Gallinghouse, G.J.; et al. Three-dimensional intracardiac echocardiography for left atrial appendage sizing and percutaneous occlusion guidance. Europace 2023, 26, euae010. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Flautt, T.; Da-Wariboko, A.; Lador, A.; Patel, A.; Guevara, M.; Valderrábano, M. Left atrial appendage occlusion without fluoroscopy. JACC Cardiovasc. Interv. 2022, 15, 1592–1594. [Google Scholar] [CrossRef]
- Magnocavallo, M.; Della Rocca, D.G.; Gianni, C.; Zagrodzky, W.; Lavalle, C.; Mohanty, S.; Chimenti, C.; Al-Ahmad, A.; Di Biase, L.; Horton, R.P.; et al. Zero contrast left atrial appendage occlusion and peridevice leak closure in patients with advanced kidney disease. Heart Rhythm. 2022, 19, 1013–1014. [Google Scholar] [CrossRef]
- Harb, S.C.; Rodriguez, L.L.; Vukicevic, M.; Kapadia, S.R.; Little, S.H. Three-Dimensional printing applications in percutaneous structural heart interventions. Circ. Cardiovasc. Imaging 2019, 12, e009014. [Google Scholar] [CrossRef]
- Wang, D.D.; Eng, M.; Kupsky, D.; Myers, E.; Forbes, M.; Rahman, M.; Zaidan, M.; Parikh, S.; Wyman, J.; Pantelic, M.; et al. Application of 3-dimensional computed tomographic image guidance to WATCHMAN implantation and impact on early operator learning curve: Single-center experience. JACC Cardiovasc. Interv. 2016, 9, 2329–2340. [Google Scholar] [CrossRef]
- Hachulla, A.L.; Noble, S.; Guglielmi, G.; Agulleiro, D.; Müller, H.; Vallée, J.P. 3D-printed heart model to guide LAA closure: Useful in clinical practice. Eur. Radiol. 2019, 29, 251–258. [Google Scholar] [CrossRef]
- Fan, Y.; Yang, F.; Cheung, G.S.; Chan, A.K.; Wang, D.D.; Lam, Y.Y.; Chow, M.C.; Leong, M.C.; Kam, K.K.; So, K.C.; et al. Device sizing guided by echocardiography-based three-dimensional printing is associated with superior outcome after percutaneous left atrial appendage occlusion. J. Am. Soc. Echocardiogr. 2019, 32, 708–719. [Google Scholar] [CrossRef] [PubMed]
- Pellegrino, P.L.; Fassini, G.; Di Biase, M.; Tondo, C. Left atrial appendage closure guided by 3D printed cardiac reconstruction: Emerging directions and future trends. J. Cardiovasc. Electrophysiol. 2016, 27, 768–771. [Google Scholar] [CrossRef] [PubMed]
- Athanassopoulos, G.D. 3D printing for left atrial appendage (LAA) modeling based on transesophageal echocardiography: A step forward in closure with LAA devices. Cardiology 2016, 135, 249–254. [Google Scholar] [CrossRef]
- Park, J.W.; Bethencourt, A.; Sievert, H.; Santoro, G.; Meier, B.; Walsh, K.; Lopez-Minguez, J.R.; Meerkin, D.; Valdés, M.; Ormerod, O.; et al. Left atrial appendage closure with amplatzer cardiac plug in atrial fibrillation: Initial European experience. Catheter. Cardiovasc. Interv. 2011, 77, 700–706. [Google Scholar] [CrossRef] [PubMed]
- Otton, J.M.; Spina, R.; Sulas, R.; Subbiah, R.N.; Jacobs, N.; Muller, D.W.; Gunalingam, B. Left atrial appendage closure guided by personalized 3D-printed cardiac reconstruction. JACC Cardiovasc. Interv. 2015, 8, 104–106. [Google Scholar] [CrossRef]
- Fan, Y.; Kwok, K.W.; Zhang, Y.; Cheung, G.S.H.; Chan, A.K.Y.; Lee, A.P.W. Three-dimensional printing for planning occlusion procedure for a double-lobed left atrial appendage. Circ. Cardiovasc. Interv. 2016, 9, 30–32. [Google Scholar] [CrossRef]
- Obasare, E.; Melendres, E.; Morris, D.L.; Mainigi, S.K.; Pressman, G.S. Patient specific 3D print of left atrial appendage for closure device. Int. J. Cardiovasc. Imaging. 2016, 32, 1495–1497. [Google Scholar] [CrossRef]
- Khalili, H.; Gentry, R.E.; Stevens, M.A.; Almany, S.L.; Banerjee, S.; Haines, D.E.; Hanzel, G.S. Rapid and affordable 3-dimensional prototyping for left atrial appendage closure planning. Circ. Cardiovasc. Interv. 2017, 10, e004710. [Google Scholar] [CrossRef]
- Hell, M.M.; Achenbach, S.; Yoo, I.S.; Franke, J.; Blachutzik, F.; Roether, J.; Graf, V.; Raaz-Schrauder, D.; Marwan, M.; Schlundt, C. 3D printing for sizing left atrial appendage closure device: Head-to-head comparison with computed tomography and transoesophageal echocardiography. EuroIntervention 2017, 13, 1234–1241. [Google Scholar] [CrossRef]
- Liu, P.; Liu, R.; Zhang, Y.; Liu, Y.; Tang, X.; Cheng, Y. The value of 3D printing models of left atrial appendage using real-time 3D transesophageal echocardiographic data in left atrial appendage occlusion: Applications toward an era of truly personalized Medicine. Cardiology 2016, 135, 255–261. [Google Scholar] [CrossRef] [PubMed]
- Vaquerizo, B.; Escabias, C.; Dubois, D.; Gómez, G.; Barreiro-Pérez, M.; Cruz-González, I. Patient-specific 3D-printed cardiac model for percutaneous left atrial appendage occlusion. Rev. Española Cardiol. 2018, 71, 762–764. [Google Scholar] [CrossRef]
- Obasare, E.; Mainigi, S.K.; Morris, D.L.; Slipczuk, L.; Goykhman, I.; Friend, E.; Ziccardi, M.R.; Pressman, G.S. CT based 3D printing is superior to transesophageal echocardiography for pre-procedure planning in left atrial appendage device closure. Int. J. Cardiovasc. Imaging 2018, 34, 821–831. [Google Scholar] [CrossRef]
- Bieliauskas, G.; Otton, J.; Chow, D.H.F.; Sawaya, F.J.; Kofoed, K.F.; Søndergaard, L.; De Backer, O. Use of 3-dimensional models to optimize pre-procedural planning of percutaneous left atrial appendage closure. JACC Cardiovasc. Interv. 2017, 10, 1067–1070. [Google Scholar] [CrossRef] [PubMed]
- Neill, J.; Chinnaduari, P.; Little, S.H.; Barker, C.M. Pre-procedural CT images after 2D3D image fusion to optimize trans-septal access during percutaneous mitral interventions. Struct. Heart. 2018, 2, 433–438. [Google Scholar] [CrossRef]
- Faletra, F.F.; Pozzoli, A.; Agricola, E.; Guidotti, A.; Biasco, L.; Leo, L.A.; Taramasso, M.; Pasotti, E.; Kuwata, S.; Moccetti, M.; et al. Echocardiographic-fluoroscopic fusion imaging for transcatheter mitral valve repair guidance. Eur. Heart J. Cardiovasc. Imag. 2018, 19, 715–726. [Google Scholar] [CrossRef]
- Roy, A.K.; Horvilleur, J.; Cormier, B.; Cazalas, M.; Fernandez, L.; Patane, M.; Neylon, A.; Spaziano, M.; Sawaya, F.J.; Arai, T.; et al. Novel integrated 3D multidetector computed tomography and fluoroscopy fusion for left atrial appendage occlusion procedures. Catheter. Cardiovasc. Interv. 2018, 91, 322–329. [Google Scholar] [CrossRef]
- Balzer, J.; Zeus, T.; Veulemans, V.; Kelm, M. Hybrid Imaging in the Catheter Laboratory: Real-time Fusion of Echocardiography and Fluoroscopy During Percutaneous Structural Heart Disease Interventions. Interv. Cardiol. 2016, 11, 59–64. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Nelles, D.; Schrickel, J.W.; Nickenig, G.; Sedaghat, A. Percutaneous left atrial appendage closure using the TrueFusion™ fusion-imaging technology. Clin. Res. Cardiol. 2020, 109, 646–648. [Google Scholar] [CrossRef] [PubMed]
- Aminian, A.; Lempereur, M.; Ben Yedder, M.; Dubois, P. Real-time fusion of echocardiograph and fluoroscopy allowing successful implantation of a WATCHMAN device without contrast injection. EuroIntervention 2018, 14, 174–175. [Google Scholar] [CrossRef]
- Afzal, S.; Piayda, K.; Hellhammer, K.; Veulemans, V.; Wolff, G.; Heidari, H.; Stüwe, D.; Kanschik, D.; Polzin, A.; Kelm, M.; et al. Real-time echocardiography-fluoroscopy fusion imaging for left atrial appendage closure: Prime time for fusion imaging? Acta Cardiol. 2021, 76, 1004–1012. [Google Scholar] [CrossRef] [PubMed]
- Ebelt, H.; Domagala, T.; Offhaus, A.; Wiora, M.; Schwenzky, A.; Hoyme, M.; Anacker, J.; Röhl, P. Fusion Imaging of X-ray and Transesophageal Echocardiography Improves the Procedure of Left Atrial Appendage Closure. Cardiovasc. Drugs Ther. 2020, 34, 781–787. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Jungen, C.; Zeus, T.; Balzer, J.; Eickholt, C.; Petersen, M.; Kehmeier, E.; Veuleman, V.; Kelm, M.; Willems, S.; Meyer, C. Left atrial appendage closure guided by integrated echocardiography and fluoroscopy imaging reduces radiation exposure. PLoS ONE 2015, 10, e0140386. [Google Scholar] [CrossRef]
- Burysz, M.; Batko, J.; Malec-Litwinowicz, M.H.; Kowalewski, M.; Litwinowicz, R.A.; Burysz, A.; Graczykowski, Ł.; Olejek, W. Combining echocardiography and fluoroscopy imaging in real time for left atrial appendage occlusion—Single center experience from Poland. Kardiochir. Torakochir. Pol. 2024, 21, 30–34. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Wang, D.D.; Qian, Z.; Vukicevic, M.; Engelhardt, S.; Kheradvar, A.; Zhang, C.; Little, S.H.; Verjans, J.; Comaniciu, D.; O’Neill, W.W.; et al. 3D Printing, Computational Modeling, and Artificial Intelligence for Structural Heart Disease. JACC Cardiovasc. Imaging 2021, 14, 41–60. [Google Scholar] [CrossRef] [PubMed]
- Michiels, K.; Heffinck, E.; Astudillo, P.; Wong, I.; Mortier, P.; Bavo, A.M. Automated MSCT Analysis for Planning Left Atrial Appendage Occlusion Using Artificial Intelligence. J. Interv. Cardiol. 2022, 2022, 5797431. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Bavo, A.M.; Wilkins, B.T.; Garot, P.; De Bock, S.; Saw, J.; Søndergaard, L.; De Backer, O.; Iannaccone, F. Validation of a computational model aiming to optimize preprocedural planning in percutaneous left atrial appendage closure. J. Cardiovasc. Comput Tomogr. 2020, 14, 149–154. [Google Scholar] [CrossRef] [PubMed]
- De Backer, O.; Iriart, X.; Kefer, J.; Nielsen-Kudsk, J.E.; Aminian, A.; Rosseel, L.; Kofoed, K.F.; Odenstedt, J.; Berti, S.; Saw, J.; et al. Impact of Computational Modeling on Transcatheter Left Atrial Appendage Closure Efficiency and Outcomes. JACC Cardiovasc. Interv. 2023, 16, 655–666. [Google Scholar] [CrossRef] [PubMed]
- De Cock, E.; Lochy, S.; Rivero-Ayerza, M.; Lempereur, M.; Cornelis, K.; Debonnaire, P.; Vermeersch, P.; Christiaen, E.; Buysschaert, I. Decisional impact of CT-Based 3D computational modeling in left atrial appendage occlusion. Cardiovasc. Interv. 2024, 17, 2322–2323. [Google Scholar] [CrossRef]


| Method | Advantages | Disadvantages |
|---|---|---|
| Transesophageal Echocardiography (TEE) | Widely used and available. High-resolution imaging of cardiac structures, including the LAA walls, with 3D visualization. Good accuracy when evaluating LAA morphology, measuring the landing zone, depth, and ostium dimensions, and aiding in the visualization of peri-device leaks. The 3D TEE option provides significantly larger and more accurate measurements of the LAA ostium and landing zone diameters compared with 2D TEE. High temporal resolution, useful when monitoring and guiding periprocedural implantation. | Invasive, particularly for elderly patients. Contraindications include esophageal pathology, coagulopathies, and severe thrombocytopenia. Anatomical LAA and heart variants can impact optimal LAA visualization. Hemodynamic fluctuations and LAA contractile cycles may lead to an underestimation of the ostium size. May require general anesthesia and associated complications, including esophageal laceration, perforation, and hemorrhage. Requires a dedicated operator to manipulate the probe during image acquisition. |
| Contrast-Enhanced Computed Tomography (CECT) | Non-invasive alternative. High spatial resolution, enabling multiplanar and 3D reconstructions of the LAA and surrounding structures. Highly sensitive at detecting LAA thrombi. Dedicated software allows for device implantation simulation, access route planning, and overlay/fusion imaging. Pre-procedural CECT planning provides more accurate device sizing, reducing procedural time, contrast usage, and potential complications. Optimized transseptal puncture site planning facilitates coaxial alignment and fluoroscopic simulation determines the optimal intra-procedural C-arm projection. Three-dimensional modeling from CECT has demonstrated benefits, including reductions in the number of implanted prostheses, incidence of leaks, fluoroscopy time, and radiation dose. | Radiation exposure is a concern. Contrast requirements are unsuitable for patients with severe kidney impairment or allergies. False positives for LAA thrombi if image acquisition settings are not optimized. Heart beat synchronization, which may necessitate medication, or can result in motion artifacts in AF patients. Motion artifacts remain a concern (e.g., breathing during acquisition). Higher body mass index (BMI) can increase image noise and artifacts. |
| Intracardiac Echocardiography (ICE) | Feasible for a single-operator approach. Eliminates the need for general anesthesia and esophageal intubation while reducing patient discomfort and facilitates faster patient recovery. Enhances procedural efficiency and shortens procedural times. Reduces radiation exposure for medical staff. The 2D-ICE option is as safe and effective as TEE. The 4D-ICE option provide accurate volumetric measurements and real-time spatial orientation. Comparable accuracy to TEE in thrombus detection. | Technically more demanding, requiring greater operator expertise. Challenges for less experienced operators, with a higher risk of pericardial effusion early in the learning curve. Steep learning curve. High costs of ICE catheters and equipment. Uncertainty regarding device release criteria. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Barletta, V.; Alberti, M.; Agostini, R.; Pizzino, F.; Trimarchi, G.; D’Alfonso, M.G.; Solari, M.; Zucchelli, G.; Cresti, A. Optimizing Imaging Techniques for Left Atrial Appendage Closure: Insights and Emerging Directions. J. Clin. Med. 2025, 14, 3607. https://doi.org/10.3390/jcm14103607
Barletta V, Alberti M, Agostini R, Pizzino F, Trimarchi G, D’Alfonso MG, Solari M, Zucchelli G, Cresti A. Optimizing Imaging Techniques for Left Atrial Appendage Closure: Insights and Emerging Directions. Journal of Clinical Medicine. 2025; 14(10):3607. https://doi.org/10.3390/jcm14103607
Chicago/Turabian StyleBarletta, Valentina, Mattia Alberti, Riccardo Agostini, Fausto Pizzino, Giancarlo Trimarchi, Maria Grazia D’Alfonso, Marco Solari, Giulio Zucchelli, and Alberto Cresti. 2025. "Optimizing Imaging Techniques for Left Atrial Appendage Closure: Insights and Emerging Directions" Journal of Clinical Medicine 14, no. 10: 3607. https://doi.org/10.3390/jcm14103607
APA StyleBarletta, V., Alberti, M., Agostini, R., Pizzino, F., Trimarchi, G., D’Alfonso, M. G., Solari, M., Zucchelli, G., & Cresti, A. (2025). Optimizing Imaging Techniques for Left Atrial Appendage Closure: Insights and Emerging Directions. Journal of Clinical Medicine, 14(10), 3607. https://doi.org/10.3390/jcm14103607







