Perspective on Perinatal Birth Canal Injuries: An Analysis of Risk Factors, Injury Mechanisms, Treatment Methods, and Patients’ Quality of Life: A Literature Review
Abstract
1. Introduction
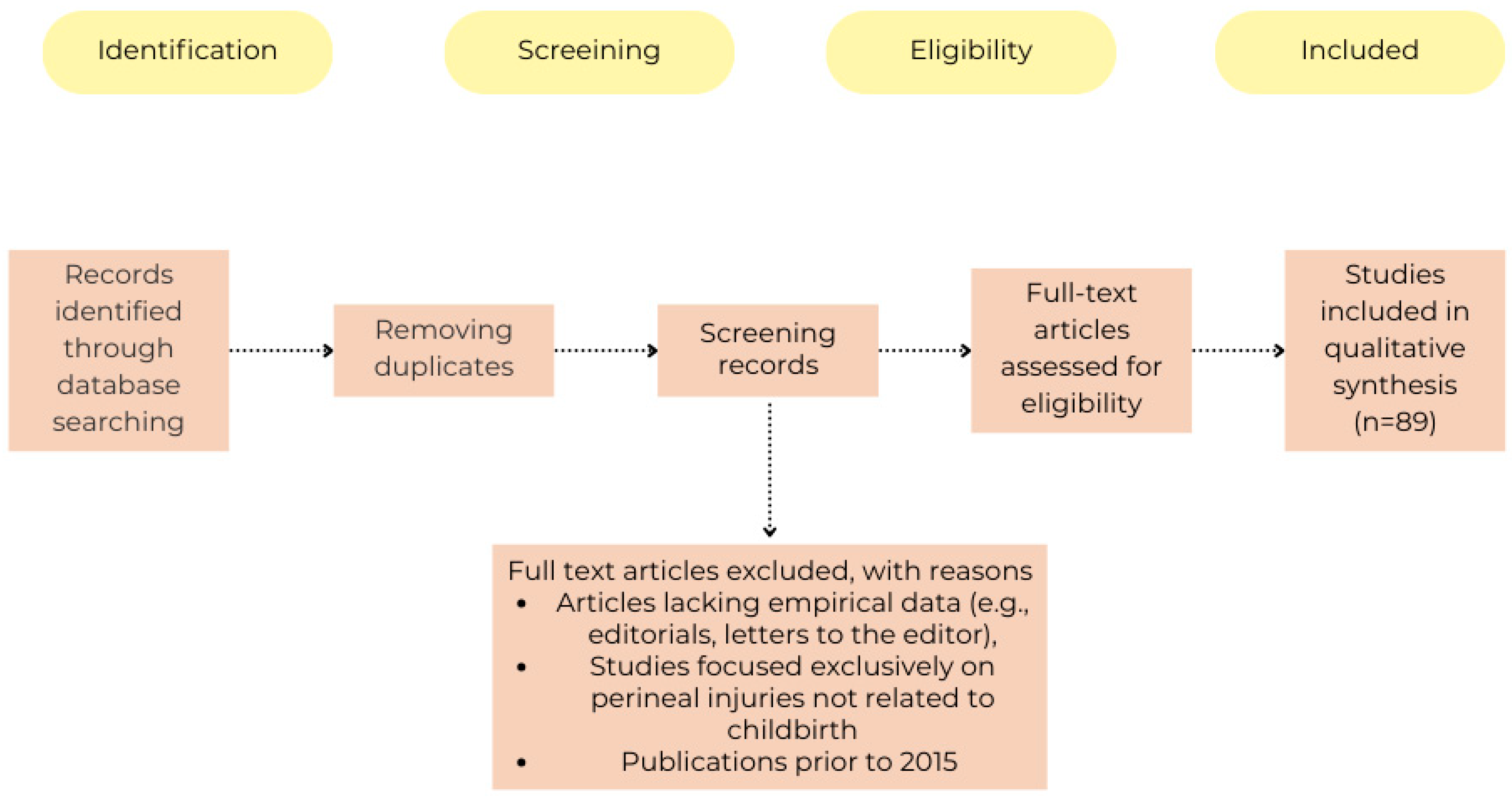
2. Methods
- Publications in English.
- Studies involving women giving birth vaginally.
- Papers discussing risk factors, prevention, classification, and consequences of perineal trauma related to childbirth.
- Articles lacking empirical data (e.g., editorials, letters to the editor).
- Studies focused exclusively on perineal injuries not related to childbirth.
- Publications prior to 2015.
3. Anatomy and Physiology of Childbirth
- First stage:
- ○
- Latent phase: Lasting approximately 8 h, during which uterine contractions are irregular, and the cervix is not yet dilated.
- ○
- Active phase: Characterised by stronger and more regular contractions leading to cervical dilation. This stage ends when the cervix is fully dilated to 10 cm [9].
- Second stage: Begins with full cervical dilation. During this stage, the foetus descends into the birth canal, assisted by the mother’s efforts. For first-time mothers (primiparas), this stage usually lasts up to 3 h, while for women with previous deliveries (multiparas), it lasts less than 2 h. Exceeding these times is considered prolonged. This stage ends with the birth of the baby [9].
- Third stage: Covers the time from the baby’s birth to the expulsion of the placenta. It typically lasts 5 to 30 min; delays beyond 30 min increase the risk of postpartum haemorrhage and may require medical intervention [9].
4. Risk Factors
4.1. Maternal Risk Factors
4.2. Foetal Risk Factors
4.3. Labour-Related Risk Factors
| Category | Risk Factors | Key Factors | Reference |
|---|---|---|---|
| Maternal Factors | Advanced maternal age | Traditionally associated with an increased risk of perineal trauma [11]. However, some studies suggest that maternal age over 35 may have a protective effect against obstetric anal sphincter injuries (OASIs) [12]. | [11,12] |
| Abnormal collagen production | Potentially weakens perineal tissue, increasing risk. | [2] | |
| Inadequate nutritional state | May affect tissue integrity and healing. | [2] | |
| Higher socio-economic background | Linked to an increased risk of severe perineal trauma. | [2] | |
| Ethnicity | Asian descent is a risk factor [2,10,15] while Black and Latina women have a lower rate of perineal laceration compared to White women [15]. | [2,10,15] | |
| First vaginal birth and VBAC | Increased risk of OASI. | [16] | |
| Perineal length | A perineal body of 3 cm or less is significantly associated with third- or fourth-degree lacerations. | [17] | |
| BMI | Increased BMI does not influence genital tract trauma risk but is linked to a reduced incidence of minor perineal trauma; no correlation with OASIs. | [18] | |
| Gestational age | Women with OASIs delivered at a slightly later gestation. However, gestational age was not a significant risk factor in regression models. | [12] | |
| Foetal Factors | Birth weight > 3 kg | Associated with a higher risk of perineal trauma. | [10] |
| Occipito-posterior position | Increased perineal trauma. | [19] | |
| Shoulder dystocia | Causes delayed foetal descent and internal rotation, leading to increased perineal trauma. Woods’ screw and reverse Woods’ screw manoeuvres are linked to a higher incidence of OASIs. | [20] | |
| Labour-Related Factors | Previous perineal damage | Higher risk of perineal tears in subsequent deliveries. | [22] |
| Instrumental delivery | Higher risk of perineal tears with forceps than vacuum. | [10,24] | |
| Episiotomy | Restrictive episiotomy leads to less severe perineal trauma than routine use [25]. Midline episiotomy increases the risk of birth trauma. Lateral/mediolateral episiotomy reduces OASI risk in operative vaginal delivery [26]. | [25,26] | |
| Episiotomy technique | A suture angle of 40–60° reduces OASI risk. Incisions deeper than 16 mm, longer than 17 mm, and more than 9 mm lateral to the midpoint are protective. | [14] | |
| Maternal position | Higher trauma rates in lithotomy/stirrups positions; lower rates in semi-sitting, lateral, or squatting positions. | [31] | |
| Prolonged second stage of labour | Risk increases after 2 h, significantly higher after 3 h. | [32] | |
| Oxytocin augmentation | Significantly associated with severe perineal trauma. | [19] | |
| Epidural analgesia | Associated with an increased risk of perineal laceration. | [33] |
5. Perineal Injuries
- First-degree tear: Superficial injury to the vaginal mucosa, which may also involve the perineal skin without affecting pelvic floor muscles.
- Second-degree tear: Injury characteristic of first-degree tear but extending to the perineal muscles.
- Third-degree tear: A second-degree tear with additional injury to the anal sphincter complex, further divided into three subcategories:
- ○
- Grade 3a—injury to less than 50% of the external anal sphincter,
- ○
- Grade 3b—injury to more than 50% of the external anal sphincter,
- ○
- Grade 3c—complete rupture of both the external and internal anal sphincters.
- Fourth-degree tear: Tear involving the anal sphincter and the anorectal mucosa [8]. The National Institute for Health and Care Excellence (NICE) recommends suturing first-degree tears to prevent wound dehiscence and promote proper healing unless the wound edges are naturally well aligned [35]. However, surgical suturing may lead to increased sensitivity and localised pain. To mitigate these issues, some studies propose the use of surgical glue, while others suggest refraining from surgical intervention altogether for such tears [36]. Surgical glue has been recognised as an effective method for repairing Grade I perineal tears in physiological deliveries, reducing procedure time, garnering higher patient satisfaction, and providing safe and aesthetically favourable outcomes [37,38].
- 2a: damage involving less than 50% of the perineal muscle,
- 2b: damage involving more than 50% of the perineal muscle,
- 2c: damage involving the entire perineal muscle [42].
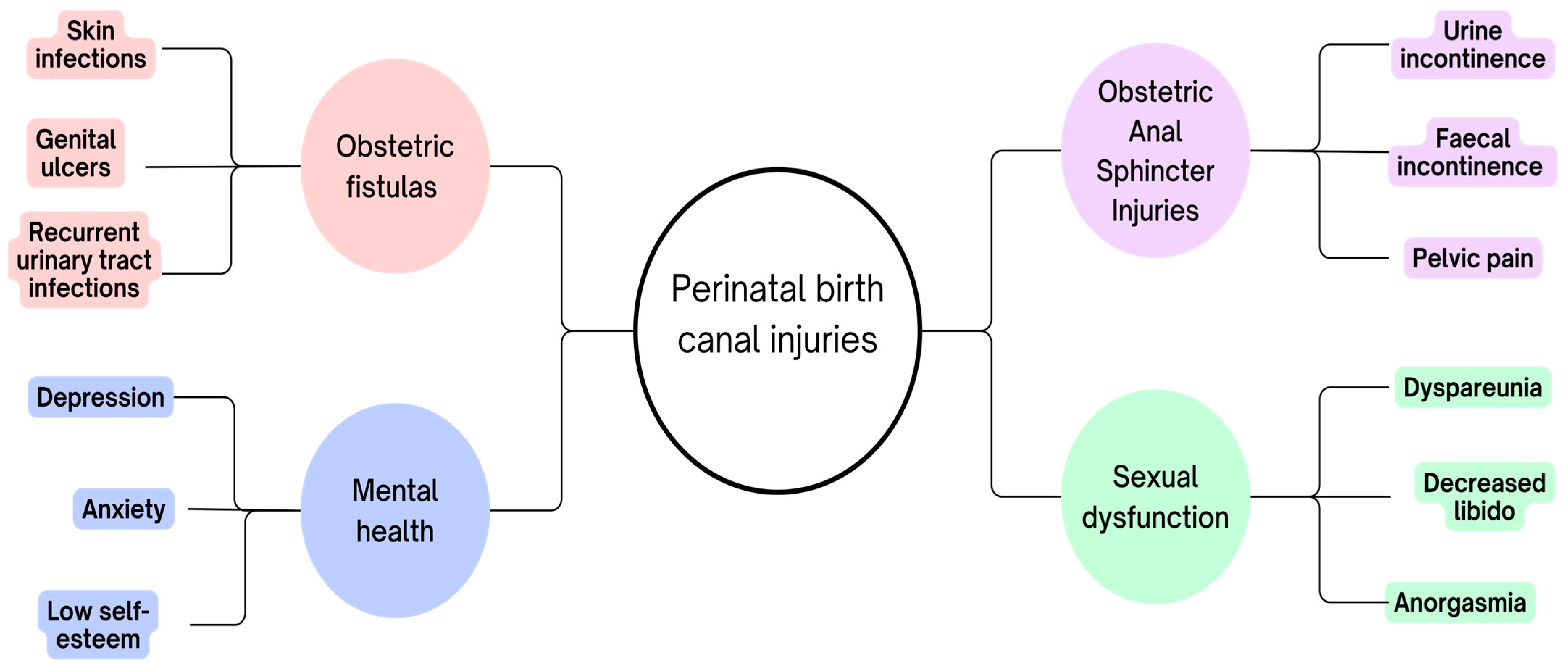
6. Childbirth-Related Complications
7. Pathophysiology of Injuries
8. Methods of Treating Perinatal Genital Tract Injuries
8.1. Conservative Treatment and Prevention
8.2. Surgical Techniques
8.3. Modern Technologies and Therapies
8.4. Postoperative Care
9. Quality of Life Assessment
10. Effectiveness of Treatment
11. Ethical Aspects of Perinatal Birth Canal Injury
12. Limitations and Future Directions of Research
13. Conclusions and Perspectives
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| OASIs | Obstetric anal sphincter injuries |
| RCOG | Royal College of Obstetricians and Gynaecologists |
| VBAC | First vaginal birth after caesarean |
| FSI | Female Sexual Functioning Index |
| GRISS | Golombok Rust Inventory of Sexual Satisfaction |
References
- Siccardi, M.A.; Bordoni, B. Anatomy, Abdomen and Pelvis, Perineal Body. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2019. [Google Scholar]
- Frohlich, J.; Kettle, C. Perineal care. BMJ Clin. Evid. 2015, 2015, 1401. [Google Scholar] [PubMed]
- Jansson, M.H.; Franzén, K.; Hiyoshi, A.; Tegerstedt, G.; Dahlgren, H.; Nilsson, K. Risk factors for perineal and vaginal tears in primiparous women—The prospective POPRACT-cohort study. BMC Pregnancy Childbirth 2020, 20, 749. [Google Scholar] [CrossRef]
- Vale de Castro Monteiro, M.; Pereira, G.M.V.; Aguiar, R.A.P.; Azevedo, R.L.; Correia-Junior, M.D.; Reis, Z.S.N. Risk factors for severe obstetric perineal lacerations. Int. Urogynecol. J. 2016, 27, 61–67. [Google Scholar] [CrossRef]
- Opondo, C.; Harrison, S.; Sanders, J.; Quigley, M.A.; Alderdice, F. The relationship between perineal trauma and postpartum psychological outcomes: A secondary analysis of a population-based survey. BMC Pregnancy Childbirth 2023, 23, 639. [Google Scholar] [CrossRef]
- Mamede, L.; Marano, D.; Dias, M.A.B.; Junior, P.R.B.d.S. Prevalence and factors associated with the perception of perineal laceration: A cross-sectional study with data from the Nascer no Brasil Survey, 2011 and 2012. Epidemiol. Serv. Saúde 2024, 33, e2023621. [Google Scholar] [CrossRef]
- Huang, J.; Lu, H.; Zang, Y.; Ren, L.; Li, C.; Wang, J. The effects of hands on and hands off/poised techniques on maternal outcomes: A systematic review and meta-analysis. Midwifery 2020, 87, 102712. [Google Scholar] [CrossRef]
- Royal College of Obstetricians and Gynaecologists. The Management of Third- and Fourth- Degree Perineal Tears; Green-Top Guideline No 29; Royal College of Obstetricians and Gynaecologists: London, UK, 2015. [Google Scholar]
- Bauman, B.L.; Ko, J.Y.; Cox, S.; D’Angelo, M.P.H.D.V.; Warner, L.; Folger, S.; Tevendale, H.D.; Coy, K.C.; Harrison, L.; Barfield, W.D. Vital Signs: Postpartum Depressive Symptoms and Provider Discussions About Perinatal Depression—United States, 2018. Morb. Mortal. Wkly. Rep. 2020, 69, 575–581. [Google Scholar] [CrossRef]
- Barca, J.A.; Bravo, C.; Pintado-Recarte, M.P.; Cueto-Hernández, I.; Ruiz-Labarta, J.; Cuñarro, Y.; Buján, J.; Alvarez-Mon, M.; Ortega, M.A.; De León-Luis, J.A. Risk factors in third and fourth degree perineal tears in women in a tertiary centre: An observational ambispective cohort study. J. Pers. Med. 2021, 11, 685. [Google Scholar] [CrossRef]
- Bączek, G.; Rzońca, E.; Sys, D.; Rychlewicz, S.; Durka, A.; Rzońca, P.; Bień, A. Spontaneous Perineal Trauma during Non-Operative Childbirth—Retrospective Analysis of Perineal Laceration Risk Factors. Int. J. Environ. Res. Public Health 2022, 19, 7653. [Google Scholar] [CrossRef]
- Nolan, C.E.; O’Leary, B.D.; Ciprike, V. Is the older perineum a safer perineum? Risk factors for obstetric anal sphincter injury. Ir. J. Med. Sci. 2021, 190, 693–699. [Google Scholar] [CrossRef]
- Gurol-Urganci, I.; Cromwell, D.A.; Edozien, L.C.; Mahmood, T.A.; Adams, E.J.; Richmond, D.H.; Templeton, A.; Van Der Meulen, J.H. Third- and fourth-degree perineal tears among primiparous women in England between 2000 and 2012: Time trends and risk factors. BJOG Int. J. Obstet. Gynaecol. 2013, 120, 1516–1525. [Google Scholar] [CrossRef] [PubMed]
- Kapoor, D.S.; Thakar, R.; Sultan, A.H. Obstetric anal sphincter injuries: Review of anatomical factors and modifiable second stage interventions. Int. Urogynecol. J. 2015, 26, 1725–1734. [Google Scholar] [CrossRef] [PubMed]
- Williams, A.; Gonzalez, B.; Fitzgerald, C.; Brincat, C. Racial/Ethnic Differences in Perineal Lacerations in a Diverse Urban Healthcare System. Female Pelvic Med. Reconstr. Surg. 2019, 25, 15–21. [Google Scholar] [CrossRef] [PubMed]
- Uebergang, J.; Hiscock, R.; Hastie, R.; Middleton, A.; Pritchard, N.; Walker, S.; Tong, S.; Lindquist, A. Risk of obstetric anal sphincter injury among women who birth vaginally after a prior caesarean section: A state-wide cohort study. BJOG Int. J. Obstet. Gynaecol. 2022, 129, 1325–1332. [Google Scholar] [CrossRef]
- Djusad, S.; Purwosunu, Y.; Hidayat, F. Relationship between Perineal Body Length and Degree of Perineal Tears in Primigravidas Undergoing Vaginal Delivery with Episiotomy. Obstet. Gynecol. Int. 2021, 2021, 2621872. [Google Scholar] [CrossRef]
- Durnea, C.M.; Jaffery, A.E.; Gauthaman, N.; Doumouchtsis, S.K. Effect of body mass index on the incidence of perineal trauma. Int. J. Gynecol. Obstet. 2018, 141, 166–170. [Google Scholar] [CrossRef]
- Webb, S.; Sherburn, M.; Ismail, K.M.K. Managing perineal trauma after childbirth. BMJ 2014, 349, g6829. [Google Scholar] [CrossRef]
- Gauthaman, N.; Walters, S.; Tribe, I.A.; Goldsmith, L.; Doumouchtsis, S.K. Shoulder dystocia and associated manoeuvres as risk factors for perineal trauma. Int. Urogynecol. J. 2016, 27, 571–577. [Google Scholar] [CrossRef]
- Hill, D.A.; Lense, J.; Roepcke, F. Shoulder Dystocia: Managing an Obstetric Emergency. Am. Fam. Physician 2020, 102, 84–90. [Google Scholar]
- Barba, M.; Bernasconi, D.P.; Manodoro, S.; Frigerio, M. Risk factors for obstetric anal sphincter injury recurrence: A systematic review and meta-analysis. Int. J. Gynecol. Obstet. 2022, 158, 27–34. [Google Scholar] [CrossRef]
- Abbas, R.A.; Qadi, Y.H.; Bukhari, R.; Shams, T. Maternal and Neonatal Complications Resulting From Vacuum-Assisted and Normal Vaginal Deliveries. Cureus 2021, 13, e14962. [Google Scholar] [CrossRef] [PubMed]
- Okeahialam, N.A.; Sultan, A.H.; Thakar, R. The prevention of perineal trauma during vaginal birth. Am. J. Obstet. Gynecol. 2024, 230, S991–S1004. [Google Scholar] [CrossRef] [PubMed]
- Jiang, H.; Qian, X.; Carroli, G.; Garner, P. Selective versus routine use of episiotomy for vaginal birth. Cochrane Database Syst. Rev. 2017, 2017, CD000081. [Google Scholar] [CrossRef]
- Ramar, C.N.; Vadakekut, E.S.; Grimes, W.R. Perineal Lacerations; StatPearls Publishing: Treasure Island, FL, USA, 2024. Available online: https://www.ncbi.nlm.nih.gov/books/NBK559068/ (accessed on 17 May 2025).
- Hu, Y.; Lu, H.; Huang, Q.; Ren, L.; Wang, N.; Huang, J.; Yang, M.; Cao, L. Risk factors for severe perineal lacerations during childbirth: A systematic review and meta-analysis of cohort studies. J. Clin. Nurs. 2023, 32, 3248–3265. [Google Scholar] [CrossRef]
- Okeahialam, N.A.; Wong, K.W.; Jha, S.; Sultan, A.H.; Thakar, R. Mediolateral/lateral episiotomy with operative vaginal delivery and the risk reduction of obstetric anal sphincter injury (OASI): A systematic review and meta-analysis. Int. Urogynecol. J. 2022, 33, 1393–1405. [Google Scholar] [CrossRef]
- Verghese, T.S.; Champaneria, R.; Kapoor, D.S.; Latthe, P.M. Obstetric anal sphincter injuries after episiotomy: Systematic review and meta-analysis. Int. Urogynecol. J. 2016, 27, 1459–1467. [Google Scholar] [CrossRef]
- Tariq, A.A.F.; Alharthy, R.A.; Alsolimani, R.M.; Alshawmali, G.M.; Bin Jabal, N.A.; Alrowaizen, S.B.; Felemban, A.S.; Alsubhi, S.H.; Khatry, A.M.; Al Dokhi, A.A. An Overview on Episiotomy: Indications, Risk Factors, and Complications. Int. J. Pharm. Res. Allied Sci. 2020, 9, 39–42. [Google Scholar]
- Lodge, F.; Haith-Cooper, M. The effect of maternal position at birth on perineal trauma: A systematic review. Br. J. Midwifery 2016, 24, 172–180. [Google Scholar] [CrossRef]
- Simic, M.; Cnattingius, S.; Petersson, G.; Sandström, A.; Stephansson, O. Duration of second stage of labor and instrumental delivery as risk factors for severe perineal lacerations: Population-based study. BMC Pregnancy Childbirth 2017, 17, 72. [Google Scholar] [CrossRef]
- Baczek, G.; Rychlewicz, S.; Sys, D.; Teliga-Czajkowska, J. Epidural anesthesia during childbirth—Retrospective analysis of maternal and neonatal results. Ginekol. Pol. 2022, 93, 847–855. [Google Scholar] [CrossRef]
- Lopes, L.G.; Balsells, M.M.D.; Vasconcelos, C.T.M.; de Araújo, T.L.; Lima, F.E.T.; Aquino, P.d.S. Can pelvic floor muscle training prevent perineal laceration? A systematic review and meta-analysis. Int. J. Gynecol. Obstet. 2022, 157, 248–254. [Google Scholar] [CrossRef] [PubMed]
- National Institute for Health and Care Excellence (NICE). Intrapartum Care; NICE: London, UK, 2023. [Google Scholar]
- Ochiai, A.M.; Araújo, N.M.; Moraes, S.D.T.A.; Caroci-Becker, A.; Sparvoli, L.G.; Teixeira, T.T.; Carvalho, R.R. The use of non-surgical glue to repair perineal first-degree lacerations in normal birth: A non-inferiority randomised trial. Women Birth 2021, 34, e514–e519. [Google Scholar] [CrossRef] [PubMed]
- Caroci-Becker, A.; Brunelli, W.S.; Lima, M.d.O.P.; Ochiai, A.M.; Oliveira, S.G.; Riesco, M.L. Use of surgical glue versus suture to repair perineal tears: A randomised controlled trial. BMC Pregnancy Childbirth 2023, 23, 246. [Google Scholar] [CrossRef] [PubMed]
- Dasrilsyah, R.A.; Kalok, A.; Ng, B.K.; Ali, A.; Chew, K.T.; Lim, P.S. Perineal skin tear repair following vaginal birth; skin adhesive versus conventional suture—A randomised controlled trial. J. Obstet. Gynaecol. 2021, 41, 242–247. [Google Scholar] [CrossRef]
- Arnold, M.J.; Sadler, K.; Leli, K.A. Obstetric Lacerations: Prevention and Repair. Am. Fam. Physician 2021, 103, 745–752. [Google Scholar]
- Edqvist, M.; Ajne, G.; Teleman, P.; Tegerstedt, G.; Rubertsson, C. Postpartum perineal pain and its association with sub-classified second-degree tears and perineal trauma—A follow-up of a randomized controlled trial. Acta Obstet. Gynecol. Scand. 2024, 103, 2314–2323. [Google Scholar] [CrossRef]
- Lindberg, I.; Persson, M.; Nilsson, M.; Uustal, E.; Lindqvist, M. “Taken by surprise”—Women’s experiences of the first eight weeks after a second degree perineal tear at childbirth. Midwifery 2020, 87, 102748. [Google Scholar] [CrossRef]
- Macedo, M.D.; Ellström Engh, M.; Siafarikas, F. Detailed classification of second-degree perineal tears in the delivery ward: An inter-rater agreement study. Acta Obstet. Gynecol. Scand. 2022, 101, 880–888. [Google Scholar] [CrossRef]
- Risløkken, J.; Dalevoll Macedo, M.; Bø, K.; Ellström Engh, M.; Siafarikas, F. The severity of second-degree perineal tears and perineal pain during three months postpartum: A prospective cohort study. Midwifery 2024, 131, 103930. [Google Scholar] [CrossRef]
- Ismail, S.I.M.F. The management of obstetric anal sphincter injuries (OASIS): A national postal questionnaire survey in hospitals in the UK. J. Obstet. Gynaecol. 2015, 35, 229–234. [Google Scholar] [CrossRef]
- Cichowski, S.; Rogers, R. ACOG Practice Bulletin No. 198: Prevention and Management of Obstetric Lacerations at Vaginal Delivery. Obstet. Gynecol. 2018, 132, e87–e102. [Google Scholar] [CrossRef]
- Hickman, L.C.; Propst, K. Accurate diagnosis and repair of obstetric anal sphincter injuries: Why and how. Am. J. Obstet. Gynecol. 2020, 222, 580.e1–580.e5. [Google Scholar] [CrossRef]
- Meister, M.R.; Rosenbloom, J.I.; Lowder, J.L.; Cahill, A.G. Techniques for Repair of Obstetric Anal Sphincter Injuries. Obstet. Gynecol. Surv. 2018, 73, 33–39. [Google Scholar] [CrossRef]
- Sultan, A.H.; Thakar, R. Diagnosis of Obstetric Anal Sphincter Injuries (OASIs). In Pelvic Floor, Perineal, and Anal Sphincter Trauma During Childbirth, 2nd ed.; Sultan, A.H., Thakar, R., Lewicky-Gaupp, C., Eds.; Springer International: Cham, Switzerland, 2024; pp. 37–48. [Google Scholar] [CrossRef]
- Harvey, M.A.; Pierce, M.; Walter, J.E.; Chou, Q.; Diamond, P.; Epp, A.; Geoffrion, R.; Larochelle, A.; Maslow, K.; Neustaedter, G.; et al. Obstetrical Anal Sphincter Injuries (OASIS): Prevention, Recognition, and Repair. J. Obstet. Gynaecol. Can. 2015, 37, 1131–1148. [Google Scholar] [CrossRef]
- Barjon, K.; Vadakekut, E.S.; Mahdy, H. Episiotomy; StatPearls Publishing: Treasure Island, FL, USA, 2025. [Google Scholar] [PubMed]
- Desplanches, T.; Marchand-Martin, L.; Szczepanski, E.D.; Ruillier, M.; Cottenet, J.; Semama, D.; Simon, E.; Quantin, C.; Sagot, P. Mediolateral episiotomy and risk of obstetric anal sphincter injuries and adverse neonatal outcomes during operative vaginal delivery in nulliparous women: A propensity-score analysis. BMC Pregnancy Childbirth 2022, 22, 48. [Google Scholar] [CrossRef]
- Soleimanzadeh Mousavi, S.H.; Miri, M.; Farzaneh, F. Episiotomy and Its Complications. Zahedan J. Res. Med. Sci. 2021, 23, e104127. [Google Scholar] [CrossRef]
- Hareru, H.E.; Ashuro, Z.; Debela, B.G.; Abebe, M. Obstetric fistula repair failure and its associated factors among women who underwent repair in sub-Saharan Africa. A systematic review and meta-analysis. PLoS ONE 2024, 19, e0295000. [Google Scholar] [CrossRef]
- Polan, M.L.; Sleemi, A.; Bedane, M.M.; Lozo, S.; Morgan, M.A. Obstetric Fistula. In Disease Control Priorities: Essential Surgery, 3rd ed.; Debas, H.T., Donkor, P., Gawande, A., Jamison, D.T., Kruk, M.E., Mock, C.N., Eds.; The World Bank: Washington, DA, USA, 2015; Volume 1, pp. 95–108. [Google Scholar]
- Srinivasan, R.; Cortes, G.; Richardson, I.; Guelfguat, M. Salpingovesical fistula mimicking an enterovaginal fistula. Radiol. Case Rep. 2020, 15, 1473–1476. [Google Scholar] [CrossRef]
- Medlen, H.; Barbier, H. Vesicovaginal Fistula; StatPearls Publishing: Treasure Island, FL, USA, 2025. [Google Scholar]
- Asmare, L.; Bayou, F.D.; Arefaynie, M.; Tsega, Y.; Endawkie, A.; Kebede, S.D.; Kebede, N.; Mihiretu, M.M.; Enyew, E.B.; Ayele, K. A systematic review and meta-analysis on the recovery time of obstetric fistula in Ethiopia, 2023. BMC Womens Health 2024, 24, 547. [Google Scholar] [CrossRef]
- Togioka, B.M.; Tonismae, T. Uterine Rupture; StatPearls Publishing: Treasure Island, FL, USA, 2025. [Google Scholar]
- Sugai, S.; Yamawaki, K.; Haino, K.; Yoshihara, K.; Nishijima, K. Incidence of Recurrent Uterine Rupture: A Systematic Review and Meta-analysis. Obstet. Gynecol. 2023, 142, 1365–1372. [Google Scholar] [CrossRef]
- Abdulmane, M.M.; Sheikhali, O.M.; Alhowaidi, R.M.; Qazi, A.; Ghazi, K. Diagnosis and Management of Uterine Rupture in the Third Trimester of Pregnancy: A Case Series and Literature Review. Cureus 2023, 15, e39861. [Google Scholar] [CrossRef]
- Banaei, M.; Kariman, N.; Ozgoli, G.; Nasiri, M.; Ghasemi, V.; Khiabani, A.; Dashti, S.; Mohamadkhani Shahri, L. Prevalence of postpartum dyspareunia: A systematic review and meta-analysis. Int. J. Gynecol. Obstet. 2021, 153, 14–24. [Google Scholar] [CrossRef]
- Hage-Fransen, M.A.H.; Wiezer, M.; Otto, A.; Wieffer-Platvoet, M.S.; Slotman, M.H.; Nijhuis-van der Sanden, M.W.G.; Pool-Goudzwaard, A.L. Pregnancy- and obstetric-related risk factors for urinary incontinence, fecal incontinence, or pelvic organ prolapse later in life: A systematic review and meta-analysis. Acta Obstet. Gynecol. Scand. 2021, 100, 373–382. [Google Scholar] [CrossRef]
- Grimes, W.R.; Stratton, M. Pelvic Floor Dysfunction; StatPearls Publishing: Treasure Island, FL, USA, 2025. [Google Scholar]
- Alshikh Ahmad, H.; Alkhatib, A.; Luo, J. Prevalence and risk factors of postpartum depression in the Middle East: A systematic review and meta-analysis. BMC Pregnancy Childbirth 2021, 21, 542. [Google Scholar] [CrossRef]
- Carlson, K.; Mughal, S.; Azhar, Y.; Siddiqui, W. Perinatal Depression; StatPearls Publishing: Treasure Island, FL, USA, 2025. [Google Scholar]
- Chechko, N.; Stickel, S.; Votinov, M. Neural responses to monetary incentives in postpartum women affected by baby blues. Psychoneuroendocrinology 2023, 148, 105991. [Google Scholar] [CrossRef]
- National Institute of Mental Health. Perinatal Depression; National Institute of Mental Health: Bethesda, MD, USA, 2023. [Google Scholar]
- Radoš, S.N.; Akik, B.K.; Žutić, M.; Rodriguez-Muñoz, M.F.; Uriko, K.; Motrico, E.; Moreno-Peral, P.; Apter, G.; Lambregtse-van den Berg, M. Diagnosis of peripartum depression disorder: Astate-of-the-art approach from the COST Action Riseup-PPD. Compr. Psychiatry 2024, 130, 152456. [Google Scholar] [CrossRef]
- de Tayrac, R.; Schantz, C. Childbirth pelvic floor trauma: Anatomy, physiology, pathophysiology and special situations—CNGOF perineal prevention and protection in obstetrics guidelines. Gynecol. Obstet. Fertil. Senol. 2018, 46, 900–912. [Google Scholar]
- Grimm, M.J. Forces Involved with Labor and Delivery—A Biomechanical Perspective. Ann. Biomed. Eng. 2021, 49, 1819–1835. [Google Scholar] [CrossRef]
- Clark–Patterson, G.; Domingo, M.; Miller, K.S. Biomechanics of pregnancy and vaginal delivery. Curr. Opin. Biomed. Eng. 2022, 22, 100386. [Google Scholar] [CrossRef]
- Chen, L.L.; Gau, M.L.; Huang, M.Z.; Tsai, C.H.; Chang, F.T. The impact of reduced perineal lacerations during delivery: A systematic review. Health Sci. Rev. 2024, 13, 100204. [Google Scholar] [CrossRef]
- Aiken, C.E.; Aiken, A.R.; Prentice, A. Influence of the duration of the second stage of labor on the likelihood of obstetric anal sphincter injury. Birth 2015, 42, 86–93. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, P.C.; Fenner, D.E. Repair of episiotomy and obstetrical perineal lacerations (first–fourth). Am. J. Obstet. Gynecol. 2024, 230, S1005–S1013. [Google Scholar] [CrossRef] [PubMed]
- Stickelmann, A.L.; Kennes, L.N.; Hölscher, M.; Graef, C.; Kupec, T.; Wittenborn, J.; Stickeler, E.; Najjari, L. Obstetric anal sphincter injuries (OASIS): Using transperineal ultrasound (TPUS) for detecting, visualizing and monitoring the healing process. BMC Womens Health 2022, 22, 339. [Google Scholar] [CrossRef] [PubMed]
- Athanasiou, S.; Pitsouni, E.; Cardozo, L.; Zacharakis, D.; Petrakis, E.; Loutradis, D.; Grigoriadis, T. Can pelvic organ prolapse in postmenopausal women be treated with laser therapy? Climacteric 2021, 24, 101–106. [Google Scholar] [CrossRef]
- Okeahialam, N.A.; Taithongchai, A.; Thakar, R.; Sultan, A.H. The incidence of anal incontinence following obstetric anal sphincter injury graded using the Sultan classification: A network meta-analysis. Am. J. Obstet. Gynecol. 2023, 228, 675–688.e13. [Google Scholar] [CrossRef]
- Antonakou, A. The long-term physical, emotional and psychosexual outcomes related to anal incontinence after severe perineal trauma at childbirth. Eur. J. Midwifery 2018, 2, 8. [Google Scholar] [CrossRef]
- O’Shea, M.S.; Lewicky-Gaupp, C.; Gossett, D.R. Long-Term Sexual Function after Obstetric Anal Sphincter Injuries. Female Pelvic Med. Reconstr. Surg. 2018, 24, 82–86. [Google Scholar] [CrossRef]
- Fritel, X.; Gachon, B.; Saurel-Cubizolles, M.J.; Annesi-Maesano, I.; Bernard, J.Y.; Botton, J.; Charles, M.A.; Dargent-Molina, P.; de Lauzon-Guillain, B.; Ducimetière, P.; et al. Postpartum psychological distress associated with anal incontinence in the EDEN mother–child cohort. BJOG Int. J. Obstet. Gynaecol. 2020, 127, 619–627. [Google Scholar] [CrossRef]
- Zhang, D.; Bo, K.; Montejo, R.; Sánchez-Polán, M.; Silva-José, C.; Palacio, M.; Barakat, R. Influence of pelvic floor muscle training alone or as part of a general physical activity program during pregnancy on urinary incontinence, episiotomy and third- or fourth-degree perineal tear: Systematic review and meta-analysis of randomized clinical trials. Acta Obstet. Gynecol. Scand. 2024, 103, 1015–1027. [Google Scholar]
- Dhom, J.; Bloes, D.A.; Peschel, A.; Hofmann, U.K. Bacterial adhesion to suture material in a contaminated wound model: Comparison of monofilament, braided, and barbed sutures. J. Orthop. Res. 2017, 35, 925–933. [Google Scholar] [CrossRef]
- Molyneux, R.; Fowler, G.; Slade, P. The postnatal effects of perineal trauma on maternal psychological and emotional wellbeing: A longitudinal study. Eur. J. Obstet. Gynecol. Reprod. Biol. 2024, 294, 238–244. [Google Scholar] [CrossRef] [PubMed]
- Akhlaghi, F.; Sabeti Baygi, Z.; Miri, M.; Najaf Najafi, M. Effect of Perineal Massage on the Rate of Episiotomy. J. Fam. Reprod. Health 2019, 13, 160–166. [Google Scholar] [CrossRef]
- Rodrigues, S.; Silva, P.; Rocha, F.; Monterroso, L.; Silva, J.N.; de Sousa, N.Q.; Escuriet, R. Perineal massage and warm compresses—Randomised controlled trial for reduce perineal trauma during labor. Midwifery 2023, 124, 103763. [Google Scholar] [CrossRef]
- Koç, Ö.; Oğlak, S.C. The effect of respectful maternity care on the perception of traumatic birth among mothers in southern Türkiye. BMC Pregnancy Childbirth 2025, 25, 532. [Google Scholar] [CrossRef]
- Davis-Floyd, R. Obstetrics and midwifery in the United States: The tensions between the technocratic and midwifery models of maternity care. In A Companion to the Anthropology of Reproductive Medicine and Technology; John Wiley & Sons: Hoboken, NJ, USA, 2023. [Google Scholar]
- World Health Organization. WHO Recommendations: Intrapartum Care for a Positive Childbirth Experience; World Health Organization: Geneva, Switzerland, 2018. [Google Scholar]
- de Wet, M.; Hannon, S.; Hannon, K.; Axelin, A.; Uusitalo, S.; Bartels, I.; Eustace-Cook, J.; Escuriet, R.; Daly, D. Systematic review of ethical issues in perinatal mental health research. Nurs. Ethics 2023, 30, 482–499. [Google Scholar] [CrossRef]
| Clinical Issue | Description/ Mechanism | Risk Factors | Diagnosis | Symptoms/ Consequences | References |
|---|---|---|---|---|---|
| Episiotomy | Surgical incision to widen vaginal opening during delivery [50] | Forceps or spatula delivery, primiparity, foetal distress [51] | Clinical judgment and maternal or foetal factors during labour [50] | Easier delivery, may cause discomfort during recovery, affect mobility and sexual activity postpartum [50,52] | [50,51,52] |
| Obstetric fistula | Abnormal connection between vagina and bladder/rectum [53] | Prolonged, obstructed labour, limited access to medical care [54] | Dye tampon test, clinical examination [55] cystoscopy with ureteral assessment, CT, MRI [56] | Urinary/faecal incontinence, genital ulcers, social stigma, infertility, recurrent urinary tract infections, lack of sexual activity, and amenorrhea [57] | [53,54,55,56,57] |
| Uterine rupture | Complete tear of the uterine wall, (perimetrium, myometrium, and endometrium) [58] | Previous C-section, myomectomy, advanced maternal age, prior rupture, TOLAC, or later pregnancy [59] | Haemoglobin or haematocrit is the most important initial test for diagnosing uterine rupture, with imaging reserved for stable patients to rule out other causes of bleeding [58,60] | Haemorrhage, vaginal bleeding, abdominal pain, changes in contraction patterns, or a non-reassuring foetal heart rate tracing [58] | [58,59,60] |
| Dyspareunia | Ongoing or recurrent genital pain experienced before, during, or after sexual intercourse [61] | Type of delivery, episiotomy, breastfeeding, dyspareunia before or during pregnancy, number of previous births, and timing of postpartum sexual activity resumption [61] | Self-report by the patient [61] | Painful intercourse, reduced sexual function, distress [61] | [61] |
| PFD—Pelvic floor disorders | Pelvic floor dysfunction (PFD) encompasses a range of urologic, gynaecologic, and colorectal symptoms caused by abnormal pelvic muscle function or support, including conditions like pelvic organ prolapse (POP) [62,63] | Mechanical injuries such as anal sphincter tears, prolonged second stage of labour, instrumental delivery, multiparity, advanced maternal age, obesity, heavy physical labour, and genetic predisposition [64] | Urodynamics, cystoscopy. Anorectal manometry, balloon expulsion test, electromyography (EMG), endoanal ultrasonography, defecography dynamic MRI [63] | Limit women’s daily activities, reduce quality of life, and result in significant societal costs [62] | [62,63,64] |
| Baby blues | Mild, short-term depressive symptoms in the first days to weeks after childbirth [65] | Hormonal shifts, neural circuit dysfunctions in the reward system, delivery-related stress [66] | No formal diagnosis necessary [66] | Tearfulness, mood swings, irritability, anxiety, fatigue, and poor appetite [65] | [65,66] |
| Postpartum depression | Depressive disorder lasting weeks to months postpartum, impairing function [67] | Young maternal age, low education, poverty, unplanned pregnancy, lack of social support, poor family relationships, pregnancy or infant complications, formula feeding, and limited access to mental health care [64] | Screening tools (e.g., EPDS), psychiatric evaluation [65,68] | Difficulty bonding with the baby, persistent sadness and anxiety lasting at least two weeks, trouble concentrating [64,65] | [64,65,67,68] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Głoćko, P.; Janczak, S.; Nowosielska-Ogórek, A.; Patora, W.; Wielgoszewska, O.; Kozłowski, M.; Cymbaluk-Płoska, A. Perspective on Perinatal Birth Canal Injuries: An Analysis of Risk Factors, Injury Mechanisms, Treatment Methods, and Patients’ Quality of Life: A Literature Review. J. Clin. Med. 2025, 14, 3583. https://doi.org/10.3390/jcm14103583
Głoćko P, Janczak S, Nowosielska-Ogórek A, Patora W, Wielgoszewska O, Kozłowski M, Cymbaluk-Płoska A. Perspective on Perinatal Birth Canal Injuries: An Analysis of Risk Factors, Injury Mechanisms, Treatment Methods, and Patients’ Quality of Life: A Literature Review. Journal of Clinical Medicine. 2025; 14(10):3583. https://doi.org/10.3390/jcm14103583
Chicago/Turabian StyleGłoćko, Patrycja, Sylwia Janczak, Agnieszka Nowosielska-Ogórek, Wiktoria Patora, Olga Wielgoszewska, Mateusz Kozłowski, and Aneta Cymbaluk-Płoska. 2025. "Perspective on Perinatal Birth Canal Injuries: An Analysis of Risk Factors, Injury Mechanisms, Treatment Methods, and Patients’ Quality of Life: A Literature Review" Journal of Clinical Medicine 14, no. 10: 3583. https://doi.org/10.3390/jcm14103583
APA StyleGłoćko, P., Janczak, S., Nowosielska-Ogórek, A., Patora, W., Wielgoszewska, O., Kozłowski, M., & Cymbaluk-Płoska, A. (2025). Perspective on Perinatal Birth Canal Injuries: An Analysis of Risk Factors, Injury Mechanisms, Treatment Methods, and Patients’ Quality of Life: A Literature Review. Journal of Clinical Medicine, 14(10), 3583. https://doi.org/10.3390/jcm14103583






