Long-Term Outcomes of Maxillary Alveolar Process Trauma and Primary Incisor Injury in Early Childhood: A Case Report
Abstract
1. Introduction
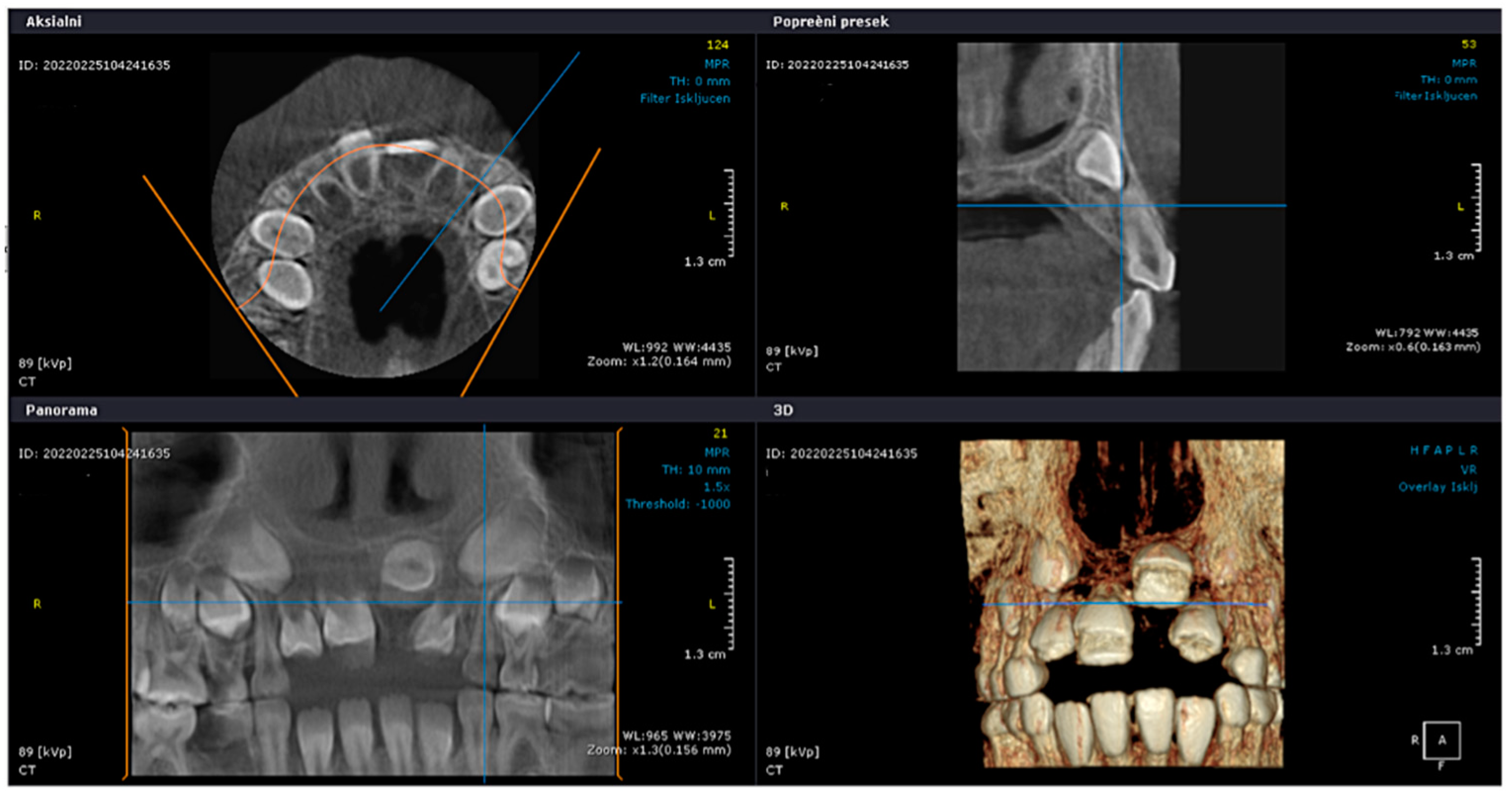
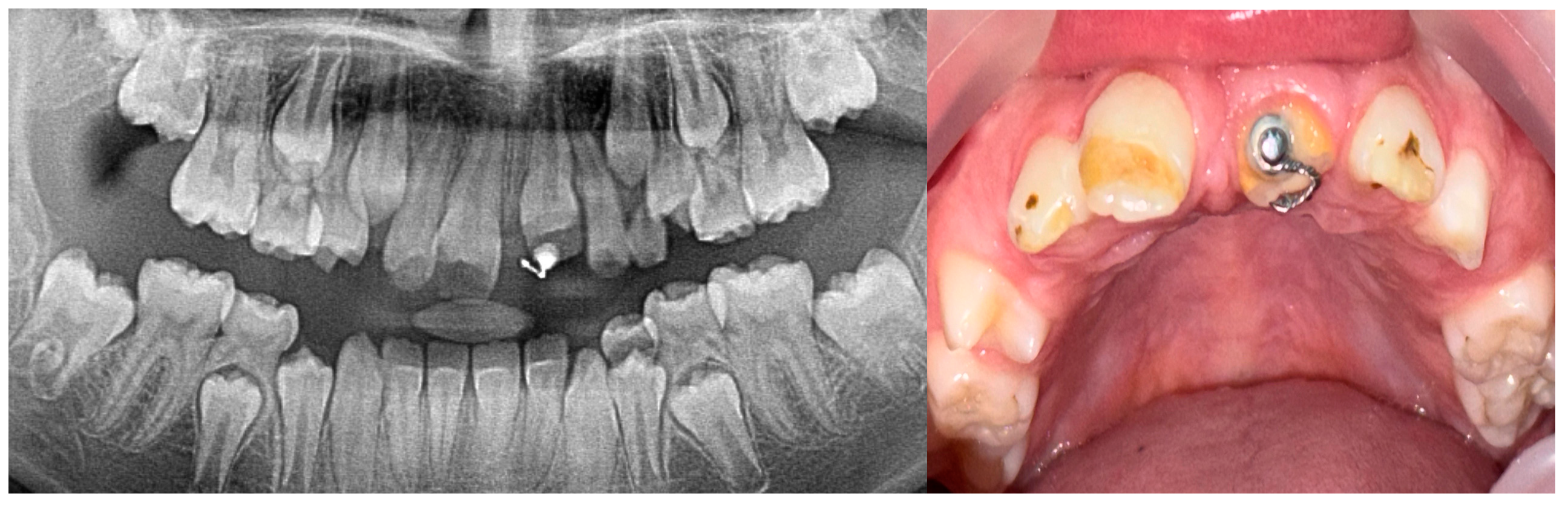
2. Case Presentation
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Flores, M.T.; Onetto, J.E. How Does Orofacial Trauma in Children Affect the Developing Dentition? Long-term Treatment and Associated Complications. J. Endod. 2019, 45 (Suppl. S12), S1–S12. [Google Scholar] [CrossRef]
- Kevci, M.; Lauridsen, E.; Andersson, L. Risk of Healing Complications Following Alveolar Process Fractures in the Primary Dentition: A Retrospective Clinical Cohort Study. Dent. Traumatol. 2025, 41, 29–36. [Google Scholar] [CrossRef] [PubMed]
- Caeiro-Villasenín, L.; Serna-Muñoz, C.; Pérez-Silva, A.; Vicente-Hernández, A.; Poza-Pascual, A.; Ortiz-Ruiz, A.J. Developmental Dental Defects in Permanent Teeth Resulting from Trauma in Primary Dentition: A Systematic Review. Int. J. Environ. Res. Public Health 2022, 19, 754. [Google Scholar] [CrossRef]
- Da Silva Assunção, L.R.; Ferelle, A.; Iwakura, M.L.H.; Cunha, R.F. Effects on permanent teeth after luxation injuries to the primary predecessors: A study in children assisted at an emergency service. Dent. Traumatol. 2009, 25, 165–170. [Google Scholar] [CrossRef] [PubMed]
- Sennhenn-Kirchner, S.; Jacobs, H.-G. Traumatic injuries to the primary dentition and effects on the permanent successors—A clinical follow-up study. Dent. Traumatol. 2006, 22, 237–241. [Google Scholar] [CrossRef] [PubMed]
- Țenț, P.A.; Juncar, R.I.; Moca, A.E.; Moca, R.T.; Juncar, M. The Etiology and Epidemiology of Pediatric Facial Fractures in North-Western Romania: A 10-Year Retrospective Study. Children 2022, 9, 932. [Google Scholar] [CrossRef]
- Juncar, M.; Tent, P.A.; Juncar, R.I.; Harangus, A.; Mircea, R. An epidemiological analysis of maxillofacial fractures: A 10-year cross-sectional cohort retrospective study of 1007 patients. BMC Oral. Health 2021, 21, 128. [Google Scholar] [CrossRef]
- Akin, A.; Uysal, S.; Cehreli, Z.C. Segmental alveolar process fracture involving primary incisors: Treatment and 24-month follow up. Dent. Traumatol. 2011, 27, 63–66. [Google Scholar] [CrossRef]
- Turgut, M.D.; Tekçiçek, M.; Canoǧlu, H. An unusual developmental disturbance of an unerupted permanent incisor due to trauma to its predecessor—A case report. Dent. Traumatol. 2006, 22, 283–286. [Google Scholar] [CrossRef]
- Yonezawa, H.; Yanamoto, S.; Hoshino, T.; Yamada, S.; Fujiwara, T.; Umeda, M. Management of maxillary alveolar bone fracture and severely intruded maxillary central incisor: Report of a case. Dent. Traumatol. 2013, 29, 416–419. [Google Scholar] [CrossRef]
- Andreasen, J.O.; Lauridsen, E. Alveolar process fractures in the permanent dentition. Part 1. Etiology and clinical characteristics. A retrospective analysis of 299 cases involving 815 teeth. Dent. Traumatol. 2015, 31, 442–447. [Google Scholar] [CrossRef] [PubMed]
- Levin, L.; Day, P.F.; Hicks, L.; O’Connell, A.; Fouad, A.F.; Bourguignon, C.; Abbott, P.V. International Association of Dental Traumatology guidelines for the management of traumatic dental injuries: General introduction. Dent. Traumatol. 2020, 36, 309–313. [Google Scholar] [CrossRef]
- Sha, X.; Jin, L.; Han, J.; Li, Y.; Zhang, L.; Qi, S. Comparison between periapical radiography and cone beam computed tomography for the diagnosis of anterior maxillary trauma in children and adolescents. Dent. Traumatol. 2022, 38, 62–70. [Google Scholar] [CrossRef] [PubMed]
- Do Espírito Santo Jácomo, D.R.; Campos, V. Prevalence of sequelae in the permanent anterior teeth after trauma in their predecessors: A longitudinal study of 8 years. Dent. Traumatol. 2009, 25, 300–304. [Google Scholar] [CrossRef]
- Gfeller, D.; von Arx, T. Retrospective Analysis of Dento-alveolar Injuries at a Swiss University Clinic (2011–2015). Swiss Dent. J. SSO—Sci. Clin. Top. 2021, 131, 500–510. [Google Scholar] [CrossRef]
- de Fátima Guedes de Amorim, L.; Estrela, C.; da Costa, L.R.R.S. Effects of traumatic dental injuries to primary teeth on permanent teeth—A clinical follow-up study. Dent. Traumatol. 2011, 27, 117–121. [Google Scholar] [CrossRef] [PubMed]
- Budak, L.; Levin, L. Long-Term Management of Dental Trauma, Mitigating Risk Factors, and Optimizing Treatment Outcomes. Dent. Traumatol. 2025, 41, 1–4. [Google Scholar] [CrossRef]
- Singhal, R.; Negi, S.; Namdev, R.; Kakran, A. Effect of root immaturity and depth of intrusion on spontaneous re-eruption and healing complications: A retrospective analysis. Dent. Traumatol. 2024, 40, 243–250. [Google Scholar] [CrossRef]
- da Costa, V.P.P.; Almeida, F.V.; Demarco, G.T.; da Motta, M.G.L.S.; de Fátima Zanchin Baldissera, E.; Silva, A.E.R.; de Oliveira Langlois, C.; Goettems, M. Effects of traumatic dental injuries of the primary dentition to the developing permanent teeth: A retrospective cohort study of 14 years. Res. Sq. 2023, 2023. [Google Scholar] [CrossRef]
- Cozza, P.; Mucedero, M.; Ballanti, F.; De Toffol, L. A case of an unerupted maxillary central incisor for indirect trauma localized horizontally on the anterior nasal spine. J. Clin. Pediatr. Dent. 2005, 29, 201–203. [Google Scholar] [CrossRef]
- Andreasen, J.O.; Ravn, J.J. Enamel changes in permanent teeth after trauma to their primary predecessors. Scand. J. Dent. Res. 1973, 81, 203–209. [Google Scholar] [CrossRef] [PubMed]
- Jeong, J.K.; Kim, T.; Choi, H.; Cho, E.S. Impaired breakdown of Herwig’s epithelial root sheath disturbs tooth root development. Dev. Dyn. 2024, 253, 423–434. [Google Scholar] [CrossRef]
- Patel, S.; Brown, J.; Semper, M.; Abella, F.; Mannocci, F. European Society of Endodontology position statement: Use of cone beam computed tomography in Endodontics: European Society of Endodontology (ESE) developed by. Int. Endod. J. 2019, 52, 1675–1678. [Google Scholar] [CrossRef] [PubMed]
- Cohenca, N.; Simon, J.H.; Roges, R.; Morag, Y.; Malfaz, J.M. Clinical indications for digital imaging in dento-alveolar trauma. Part 1: Traumatic injuries. Dent. Traumatol. 2007, 23, 95–104. [Google Scholar] [CrossRef]
- Andreasen, J.; Fm, A.; Lk, B.; Flores, M.; Andersson, L. Traumatic Dental Injuries: A Manual; Wiley-Blackwell: Hoboken, NJ, USA, 2011. [Google Scholar]
- Seehra, J.; Yaqoob, O.; Patel, S.; O’Neill, J.; Bryant, C.; Noar, J.; Morris, D.; Cobourne, M.T. National clinical guidelines for the management of unerupted maxillary incisors in children. Br. Dent. J. 2018, 224, 779–785. [Google Scholar] [CrossRef] [PubMed]
- Day, P.F.; Kindelan, S.A.; Spencer, J.R.; Kindelan, J.D.; Duggal, M.S. Dental trauma: Part 2. Managing poor prognosis anterior teeth--treatment options for the subsequent space in a growing patient. J. Orthod. 2008, 35, 143–155. [Google Scholar] [CrossRef]
- Berlin-Broner, Y.; Al Bawaliz, L.; Levin, L. Implications of Post-Traumatic Treatment of Immature Maxillary Incisors. Int. Dent. J. 2023, 73, 337–345. [Google Scholar] [CrossRef]
- Lygidakis, N.A.; Garot, E.; Somani, C.; Taylor, G.D.; Rouas, P.; Wong, F.S.L. Best clinical practice guidance for clinicians dealing with children presenting with molar-incisor-hypomineralisation (MIH): An updated European Academy of Paediatric Dentistry policy document. Eur. Arch. Paediatr. Dent. 2022, 23, 3–21. [Google Scholar] [CrossRef]
- Andreasen, J.O.; Lauridsen, E.; Andreasen, F.M. Contradictions in the treatment of traumatic dental injuries and ways to proceed in dental trauma research*. Dent. Traumatol. 2010, 26, 16–22. [Google Scholar] [CrossRef]
- Iida, S.; Matsuya, T. Paediatric maxillofacial fractures: Their aetiological characters and fracture patterns. J. Cranio-Maxillofac. Surg. 2002, 30, 237–241. [Google Scholar] [CrossRef]
- Das, P.; Mishra, L.; Jena, D.; Govind, S.; Panda, S.; Lapinska, B. Oral Health-Related Quality of Life in Children and Adolescents with a Traumatic Injury of Permanent Teeth and the Impact on Their Families: A Systematic Review. Int. J. Environ. Res. Public Health 2022, 19, 3087. [Google Scholar] [CrossRef] [PubMed]






Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vujkov, S.; Ivic, S.; Petrovic, B.; Blagojevic, D.; Neskovic, I.; Tadic, A.; Komsic, J. Long-Term Outcomes of Maxillary Alveolar Process Trauma and Primary Incisor Injury in Early Childhood: A Case Report. J. Clin. Med. 2025, 14, 3275. https://doi.org/10.3390/jcm14103275
Vujkov S, Ivic S, Petrovic B, Blagojevic D, Neskovic I, Tadic A, Komsic J. Long-Term Outcomes of Maxillary Alveolar Process Trauma and Primary Incisor Injury in Early Childhood: A Case Report. Journal of Clinical Medicine. 2025; 14(10):3275. https://doi.org/10.3390/jcm14103275
Chicago/Turabian StyleVujkov, Sanja, Stojan Ivic, Bojan Petrovic, Duska Blagojevic, Isidora Neskovic, Ana Tadic, and Jelena Komsic. 2025. "Long-Term Outcomes of Maxillary Alveolar Process Trauma and Primary Incisor Injury in Early Childhood: A Case Report" Journal of Clinical Medicine 14, no. 10: 3275. https://doi.org/10.3390/jcm14103275
APA StyleVujkov, S., Ivic, S., Petrovic, B., Blagojevic, D., Neskovic, I., Tadic, A., & Komsic, J. (2025). Long-Term Outcomes of Maxillary Alveolar Process Trauma and Primary Incisor Injury in Early Childhood: A Case Report. Journal of Clinical Medicine, 14(10), 3275. https://doi.org/10.3390/jcm14103275







