Effects of an Early Exercise Program with Cryotherapy on Range of Motion, Pain, Swelling, and Gait in Patients with Total Knee Arthroplasty: A Randomized Controlled Trial
Abstract
1. Introduction
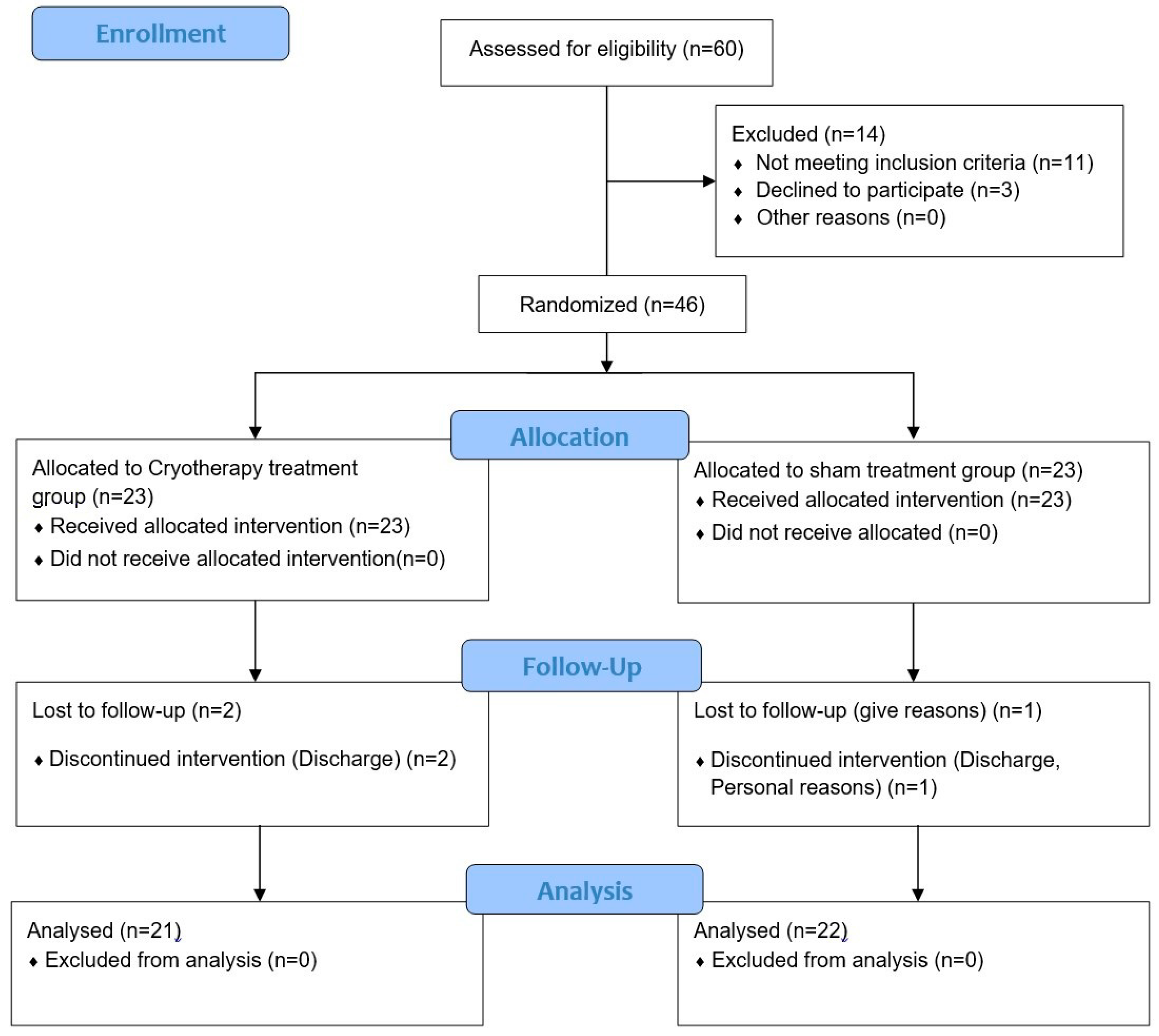
2. Materials and Methods
2.1. Participants
2.2. Procedure
2.3. Intervention
2.3.1. Cryotherapy Treatment
2.3.2. Initial Rehabilitation Program
2.3.3. Continuous Passive Movement
2.4. Outcome Measures
2.4.1. Joint Range of Motion Measurement
2.4.2. Pain Measurement
2.4.3. Edema Measurement
2.4.4. The 10 MWT
2.5. Statistical Analysis
3. Results
3.1. Knee Joint Rage of Motion
3.2. Pain
3.3. Edema
3.4. Gait
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Farquhar, S.J.; Reisman, D.S.; Snyder-Mackler, L. Persistence of altered movement patterns during a sit-to-stand task 1 year following unilateral total knee arthroplasty. Phys. Ther. 2008, 88, 567–579. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Nguyen, U.S.D.; Lane, N.E.; Lu, N.; Wei, J.; Lei, G.; Zeng, C.; Zhang, Y. Knee osteoarthritis, potential mediators, and risk of all-cause mortality: Data from the Osteoarthritis Initiative. Arthritis Care Res. 2021, 73, 566–573. [Google Scholar] [CrossRef] [PubMed]
- Bijlsma, J.W.; Berenbaum, F.; Lafeber, F.P. Osteoarthritis: An update with relevance for clinical practice. Lancet 2011, 377, 2115–2126. [Google Scholar] [CrossRef]
- Pang, J.; Cao, Y.-L.; Zheng, Y.-X.; Gao, N.-Y.; Wang, X.-Z.; Chen, B.; Gu, X.-F.; Yuan, W.; Zhang, M.; Liu, T. Influence of pain severity on health-related quality of life in Chinese knee osteoarthritis patients. Int. J. Clin. Exp. Med. 2015, 8, 4472. [Google Scholar] [PubMed]
- Strasser, E.M.; Draskovits, T.; Praschak, M.; Quittan, M.; Graf, A. Association between ultrasound measurements of muscle thickness, pennation angle, echogenicity and skeletal muscle strength in the elderly. Age 2013, 35, 2377–2388. [Google Scholar] [CrossRef] [PubMed]
- Harato, K.; Otani, T.; Nakayama, N.; Watarai, H.; Wada, M.; Yoshimine, F. When does postoperative standing function after total knee arthroplasty improve beyond preoperative level of function? Knee 2009, 16, 112–115. [Google Scholar] [CrossRef] [PubMed]
- Sextro, G.S.; Berry, D.J.; Rand, J.A. Total knee arthroplasty using cruciate-retaining kinematic condylar prosthesis. Clin. Orthop. Relat. Res. 2001, 388, 33–40. [Google Scholar] [CrossRef]
- Gao, J.; Xing, D.; Dong, S.; Lin, J. The primary total knee arthroplasty: A global analysis. J. Orthop. Surg. Res. 2020, 15, 190. [Google Scholar] [CrossRef]
- Bade, M.J.; Kohrt, W.M.; Stevens-Lapsley, J.E. Outcomes before and after total knee arthroplasty compared to healthy adults. J. Orthop. Sports Phys. Ther. 2010, 40, 559–567. [Google Scholar] [CrossRef]
- Akeson, W.; Amiel, D.; Abel, M.; Garfin, S.; Woo, S.L. Effects of immobilization on joints. Clin. Orthop. Relat. Res. 1987, 219, 28–37. [Google Scholar] [CrossRef]
- Potter, P.J.; Kirby, R.L.; MacLeod, D.A. The effects of simulated knee flexion contractures on standing balance. J. Biomech. 1989, 22, 1070. [Google Scholar] [CrossRef]
- Yun, J.Y.; Lee, J.K. Effects of a thera-band exercise program on pain, knee flexion ROM, and psychological parameters following total knee arthroplasty. J. Korean Acad. Nurs. 2015, 45, 823–833. [Google Scholar] [CrossRef] [PubMed]
- Piva, S.R.; Gil, A.B.; Almeida, G.J.; DiGioia, A.M., III; Levison, T.J.; Fitzgerald, G.K. A balance exercise program appears to improve function for patients with total knee arthroplasty: A randomized clinical trial. Phys. Ther. 2010, 90, 880–894. [Google Scholar] [CrossRef]
- Kim, I.-B.; Kim, Y.-S. The effect of PROM and AAROM exercise after TKA on increasing the knee range of motion. J. Korean Phys. Ther. Sci. 2009, 16, 11–17. [Google Scholar]
- Goh, S.-L.; Persson, M.S.; Stocks, J.; Hou, Y.; Welton, N.J.; Lin, J.; Hall, M.C.; Doherty, M.; Zhang, W. Relative efficacy of different exercises for pain, function, performance and quality of life in knee and hip osteoarthritis: Systematic review and network meta-analysis. Sports Med. 2019, 49, 743–761. [Google Scholar] [CrossRef] [PubMed]
- Chesterton, L.S.; Foster, N.E.; Ross, L. Skin temperature response to cryotherapy. Arch. Phys. Med. Rehabil. 2002, 83, 543–549. [Google Scholar] [CrossRef]
- Lee, J.-H.; Lee, J.-H.; Min, D.-K.; Lee, J.-K.; Kim, J.-W. The Effects of Cryotherapy Treatment with Leg Elevation on Swelling of Patient Who had an TKA. J. Korean Acad. Orthop. Man. Phys. Ther. 2017, 23, 45–49. [Google Scholar]
- Lee, J.G.; Kim, M.J.; Park, S.B.; Kim, Y.H. Changes in the Visual Analogue Scale Score Following Freezing Cold Air Application in Knee Joint Pain. J. Korean Acad. Rehabil. Med. 1999, 23, 124–128. [Google Scholar]
- Kim, H.-B. Effect of Cryotherapy on Soft Tissue Injuries. J. Korean Phys. Ther. Assoc. 1988, 9, 13–17. [Google Scholar]
- Cameron, M.H. Physical Agents in Rehabilitation: From Research to Practice; Elsevier Health Sciences: Philadelphia, PA, USA, 2012. [Google Scholar]
- Choi, Y.; Jung, B.; Hwang, B. Effects of skin temperature change, cold pain and muscle activity by Cold Air Application type on the induced delayed onset muscle soreness. J. Korean Soc. Radiol. 2013, 7, 99–106. [Google Scholar] [CrossRef][Green Version]
- Kim, Y.-H.; Yang, G.-T.; Jang, Y.-H.; Park, S.-B.; Ryu, J.-S. The Development of a Cryotherapy System. J. Biomed. Eng. Res. 1998, 19, 617–622. [Google Scholar]
- Yoon, A.J. Effect of Cryo Therapy after One-Side TKR on ESR, CRP, Pian and Swelling Over Time. Master’s Thesis, Korea University, Seoul, Republic of Korea, 2014. [Google Scholar]
- Hirvonen, H.; Mikkelsson, M.; Kautiainen, H.; Pohjolainen, T.; Leirisalo-Repo, M. Effectiveness of different cryotherapies on pain and disease activity in active rheumatoid arthritis. A randomised single blinded controlled trial. Clin. Exp. Rheumatol. 2006, 24, 295. [Google Scholar]
- Bade, M.J.; Stevens-Lapsley, J.E. Early high-intensity rehabilitation following total knee arthroplasty improves outcomes. J. Orthop. Sports Phys. Ther. 2011, 41, 932–941. [Google Scholar] [CrossRef]
- Lee, J.; Min, D.; Lee, S. The Effect of an Exercise Program with Patella Mobilization on Range of Motion, Muscle Strength and Gait in Patients with Total Knee Arthroplasty. J. Korean Soc. Integr. Med. 2020, 8, 1–14. [Google Scholar]
- Moon, D.-H.; Oh, D.-H.; Zhang, S.-A.; Lee, J.-K. Effect of backward walking exercise on ROM, VAS score and proprioception in anterior cruciate ligament reconstruction patients. J. Korea Acad.-Ind. Coop. Soc. 2016, 17, 522–529. [Google Scholar]
- Huskisson, E.C. Measurement of pain. Lancet 1974, 304, 1127–1131. [Google Scholar] [CrossRef]
- Shim, E. A Study on the Effects of Structures Cryotherapy on Pain, Inflammation, Range of Motion and Edema in Patients with Total Knee Arthroplasty. Unpublished. Master’s Thesis, Chonnam National University, Daejeon, Republic of Korea, 2014. [Google Scholar]
- Choi, Y.; Seo, K. Correlation among bioimpedance analysis, sonographic and circumferential measurement in assessment of breast cancer-related arm lymphedema. Lymphology 2014, 47, 123–133. [Google Scholar] [PubMed]
- Wirz, M.; Van Hedel, H.J.; Rupp, R.; Curt, A.; Dietz, V. Muscle force and gait performance: Relationships after spinal cord injury. Arch. Phys. Med. Rehabil. 2006, 87, 1218–1222. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.-K. The Effects of a 12-Week Exercise Training Program on Ligament Stability, Knee Function, and Lysholm Score after Anterior Cruciate Ligament Reconstruction; Seoul National University: Seoul, Republic of Korea, 2002. [Google Scholar]
- Lehmann, J.F.; Warren, C.G.; Scham, S.M. Therapeutic heat and cold. Clin. Orthop. Relat. Res. 1974, 99, 207–245. [Google Scholar] [CrossRef]
- Kullenberg, B.; Ylipää, S.; Söderlund, K.; Resch, S. Postoperative cryotherapy after total knee arthroplasty: A prospective study of 86 patients. J. Arthroplast. 2006, 21, 1175–1179. [Google Scholar] [CrossRef]
- Rowe, P.; Myles, C.; Walker, C.; Nutton, R. Knee joint kinematics in gait and other functional activities measured using flexible electrogoniometry: How much knee motion is sufficient for normal daily life? Gait Posture 2000, 12, 143–155. [Google Scholar] [CrossRef]
- Eller, L.S. Guided imagery interventions for symptom management. Annu. Rev. Nurs. Res. 1999, 17, 57–84. [Google Scholar] [CrossRef]
- Hwang, H.S.; Kim, H.H.; Shin, J.W.; Leem, C.G.; Lee, C.; Yang, H.S.; Lee, D.M. Comparison of analgesic requirements for postoperative pain control in patients undergoing major orthopedic surgery. J. Korean Pain Soc. 2004, 17, 228–233. [Google Scholar] [CrossRef]
- Yeo, H.N.; Kim, Y.K.; Kang, M.; Shin, J.S. Effects of elastic band exercise on pain, range of motion, and fear of falling in patients with total knee replacement. J. Korean Clin. Nurs. Res. 2015, 21, 266–275. [Google Scholar]
- Chatap, G.; De Sousa, A.; Giraud, K.; Vincent, J.-P.; Acute Pain in the Elderly Study Group. Pain in the elderly: Prospective study of hyperbaric CO2 cryotherapy (neurocryostimulation). Jt. Bone Spine 2007, 74, 617–621. [Google Scholar] [CrossRef] [PubMed]
- Karaduman, Z.O.; Turhal, O.; Turhan, Y.; Orhan, Z.; Arican, M.; Uslu, M.; Cangur, S. Evaluation of the clinical efficacy of using thermal camera for cryotherapy in patients with total knee arthroplasty: A prospective study. Medicina 2019, 55, 661. [Google Scholar] [CrossRef] [PubMed]
- Hart, J.M.; Kuenze, C.M.; Diduch, D.R.; Ingersoll, C.D. Quadriceps muscle function after rehabilitation with cryotherapy in patients with anterior cruciate ligament reconstruction. J. Athl. Train. 2014, 49, 733–739. [Google Scholar] [CrossRef] [PubMed]
- Daniel, D.M.; Stone, M.L.; Arendt, D.L. The effect of cold therapy on pain, swelling, and range of motion after anterior cruciate ligament reconstructive surgery. Arthrosc. J. Arthrosc. Relat. Surg. 1994, 10, 530–533. [Google Scholar] [CrossRef]
- Carati, C.J.; Anderson, S.N.; Gannon, B.J.; Piller, N.B. Treatment of postmastectomy lymphedema with low-level laser therapy: A double blind, placebo-controlled trial. Cancer Interdiscip. Int. J. Am. Cancer Soc. 2003, 98, 1114–1122. [Google Scholar] [CrossRef]
- Mora, S.; Zalavras, C.G.; Wang, L.; Thordarson, D.B. The role of pulsatile cold compression in edema resolution following ankle fractures: A randomized clinical trial. Foot Ankle Int. 2002, 23, 999–1002. [Google Scholar] [CrossRef] [PubMed]
- Webb, J.; Williams, D.; Ivory, J.; Day, S.; Williamson, D. The use of cold compression dressings after total knee replacement: A randomized controlled trial. Orthopedics 1998, 21, 59–61. [Google Scholar] [CrossRef] [PubMed]
- Ohkoshi, Y.; Ohkoshi, M.; Nagasaki, S.; Ono, A.; Hashimoto, T.; Yamane, S. The effect of cryotherapy on intraarticular temperature and postoperative care after anterior cruciate ligament reconstruction. Am. J. Sports Med. 1999, 27, 357–362. [Google Scholar] [CrossRef] [PubMed]
- Saari, T.; Tranberg, R.; Zügner, R.; Uvehammer, J.; Kärrholm, J. Changed gait pattern in patients with total knee arthroplasty but minimal influence of tibial insert design: Gait analysis during level walking in 39 TKR patients and 18 healthy controls. Acta Orthop. 2005, 76, 253–260. [Google Scholar] [CrossRef] [PubMed]
- Okoro, T.; Ibrahim, Y.; Mansour, N.; Alderman, P.; Evans, A. The use of cryotherapy in the early postoperative period after total hip arthroplasty. Ortop. Traumatol. Rehabil. 2019, 21, 341–345. [Google Scholar] [CrossRef]
- Su, E.; Perna, M.; Boettner, F.; Mayman, D.; Gerlinger, T.; Barsoum, W.; Randolph, J.; Lee, G. A prospective, multi-center, randomised trial to evaluate the efficacy of a cryopneumatic device on total knee arthroplasty recovery. J. Bone Jt. Surg. Br. Vol. 2012, 94, 153–156. [Google Scholar] [CrossRef]
- Yoo, M. New perspectives of treatment of osteoarthritis. J. Muscle Jt. Health 1995, 2, 227–229. [Google Scholar]
| ROM | CRYO (n = 21) | Non-CRYO (n = 22) | t (p) |
|---|---|---|---|
| Gender (male/female) | 3/18 | 4/18 | 0.120 (0.527) |
| Age (year) | 72.4 ± 5.83 a | 71.0 ± 7.20 | 0.823 (0.466) |
| Height (cm) | 154.0 ± 6.90 | 154.0 ± 8.30 | 0.728 (0.968) |
| Weight (kg) | 60.4 ± 7.87 | 64.7 ± 12.50 | 1.790 (0.187) |
| BMI (kg/m2) | 26.0 ± 3.24 | 26.3 ± 3.41 | 0.034 (0.752) |
| ROM | CRYO (n = 21) | Non-CRYO (n = 22) | t (p) | |
|---|---|---|---|---|
| ROM-Flex (°) | Pre- | 52.24 ± 9.19 a | 62.73 ± 12.20 | - |
| Post- | 115.69 ± 9.58 | 100.75 ± 12.40 | - | |
| Difference | −63.45 ± 15.99 | −38.02 ± 16.29 | 5.167 (0.000) * | |
| t (p) | −18.185 (0.000) | −10.963 (0.000) | ||
| ROM-Ext (°) | Pre- | 11.76 ± 3.71 | 12.80 ± 4.14 | - |
| Post- | 5.24 ± 1.09 | 6.23 ± 1.99 | - | |
| Difference | 6.25 ± 3.86 | 6.57 ± 4.40 | 0.035 (0.972) | |
| t (p) | 7.755 (0.000) * | 7.005 (0.000) * |
| PAIN | CRYO (n = 21) | Non-CRYO (n = 22) | t (p) | |
|---|---|---|---|---|
| VAS | Pre- | 5.05 ± 1.36 a | 4.90 ± 1.41 | - |
| Post- | 2.00 ± 0.95 | 3.27 ± 1.67 | - | |
| Difference | 3.05 ± 1.50 | 1.64 ± 1.18 | −3.442 (0.001) * | |
| t (p) | 9.316 (0.000) * | 6.521 (0.000) * |
| ROM | CRYO (n = 21) | Non-CRYO (n = 22) | t (p) | |
|---|---|---|---|---|
| GIRTH-5 (cm) | Pre- | 42.09 ± 4.04 a | 41.81 ± 4.40 | |
| Post- | 38.40 ± 3.65 | 40.14 ± 5.08 | ||
| Difference | 3.68 ± 1.69 | 1.68 ± 1.64 | −3.961 (0.000) * | |
| t (p) | 10.007 (0.000) | 4.796 (0.000) | ||
| GIRTH-10 (cm) | Pre- | 44.36 ± 4.62 | 43.54 ± 5.05 | |
| Post- | 40.68 ± 3.96 | 41.87 ± 4.75 | ||
| Difference | 3.68 ± 1.95 | 1.66 ± 1.68 | −3.618 (0.001) * | |
| t (p) | 8.633 (0.000) * | 4.406 (0.000) * |
| CRYO (n = 21) | Non-CRYO (n = 22) | t (p) | ||
|---|---|---|---|---|
| 10 MWT (m/s) | Pre- | 20.85 ± 5.80 a | 19.52 ± 3.55 | |
| Post- | 11.79 ± 2.53 | 14.81 ± 3.66 | ||
| Difference | 9.06 ± 5.25 | 4.70 ± 2.79 | −3.422 (0.001) * | |
| t (p) | 7.913 (0.000) * | 7.922 (0.000) * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, B.; Yoon, D.; Yim, J. Effects of an Early Exercise Program with Cryotherapy on Range of Motion, Pain, Swelling, and Gait in Patients with Total Knee Arthroplasty: A Randomized Controlled Trial. J. Clin. Med. 2024, 13, 1420. https://doi.org/10.3390/jcm13051420
Lee B, Yoon D, Yim J. Effects of an Early Exercise Program with Cryotherapy on Range of Motion, Pain, Swelling, and Gait in Patients with Total Knee Arthroplasty: A Randomized Controlled Trial. Journal of Clinical Medicine. 2024; 13(5):1420. https://doi.org/10.3390/jcm13051420
Chicago/Turabian StyleLee, Bomi, Doyoo Yoon, and Jongeun Yim. 2024. "Effects of an Early Exercise Program with Cryotherapy on Range of Motion, Pain, Swelling, and Gait in Patients with Total Knee Arthroplasty: A Randomized Controlled Trial" Journal of Clinical Medicine 13, no. 5: 1420. https://doi.org/10.3390/jcm13051420
APA StyleLee, B., Yoon, D., & Yim, J. (2024). Effects of an Early Exercise Program with Cryotherapy on Range of Motion, Pain, Swelling, and Gait in Patients with Total Knee Arthroplasty: A Randomized Controlled Trial. Journal of Clinical Medicine, 13(5), 1420. https://doi.org/10.3390/jcm13051420






