Acute Pancreatitis and Type 2 Diabetes Mellitus: The Chicken–Egg Paradox—A Seven-Year Experience of a Large Tertiary Center
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Filtering
2.2. Statistical Analysis and Software Deployment
3. Results
3.1. Population Characteristics
3.2. Severity
3.3. ICU Admission
3.4. Secondary Aims
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| CE | Christ (common) era |
| AP | acute pancreatitis |
| DM | diabetes mellitus |
| T2DM | type 2 diabetes mellitus |
| NLRP3 | Nucleotide-binding domain, leucine-rich-containing family, pyrin domain-containing 3 |
| RCT | randomized clinical trial |
| ICU | intensive care unit |
| BUC-API | Bucharest Acute Pancreatitis Index |
| ICD-10 | International Classification of Diseases, 10th edition |
| EHR | electronic health record |
| RAP | recurrent acute pancreatitis |
| RON | International Organization for Standardization code of Romanian leu (currency of Romania) |
| DCH | daily cost of hospitalization |
| LoS | length of stay |
| APFC | acute peripancreatic fluid collection |
| ANC | acute necrotic collection |
| WON | walled-off necrosis |
| ASR | adjusted standardized residual |
| OAP | other known cause of acute pancreatitis |
| AoCP | acute-on-chronic pancreatitis |
References
- Ong, K.L.; Stafford, L.K.; McLaughlin, S.A.; Boyko, E.J.; Vollset, S.E.; Smith, A.E.; Dalton, B.E.; Duprey, J.; Cruz, J.A.; Hagins, H.; et al. Global, Regional, and National Burden of Diabetes from 1990 to 2021, with Projections of Prevalence to 2050: A Systematic Analysis for the Global Burden of Disease Study 2021. Lancet 2023, 402, 203–234. [Google Scholar] [CrossRef]
- Iannuzzi, J.P.; King, J.A.; Leong, J.H.; Quan, J.; Windsor, J.W.; Tanyingoh, D.; Coward, S.; Forbes, N.; Heitman, S.J.; Shaheen, A.-A.; et al. Global Incidence of Acute Pancreatitis Is Increasing over Time: A Systematic Review and Meta-Analysis. Gastroenterology 2022, 162, 122–134. [Google Scholar] [CrossRef]
- Girman, C.J.; Kou, T.D.; Cai, B.; Alexander, C.M.; O’neill, E.A.; Williams-Herman, D.E.; Katz, L. Patients with type 2 diabetes mellitus have higher risk for acute pancreatitis compared with those without diabetes. Diabetes Obes. Metab. 2010, 12, 766–771. [Google Scholar] [CrossRef]
- Lai, S.-W.; Muo, C.-H.; Liao, K.-F.; Sung, F.-C.; Chen, P.-C. Risk of acute pancreatitis in type 2 diabetes and risk reduction on anti-diabetic drugs: A population-based cohort study in Taiwan. Am. J. Gastroenterol. 2011, 106, 1697–1704. [Google Scholar] [CrossRef]
- Zechner, D.; Spitzner, M.; Bobrowski, A.; Knapp, N.; Kuhla, A.; Vollmar, B. Diabetes aggravates acute pancreatitis and inhibits pancreas regeneration in mice. Diabetologia 2012, 55, 1526–1534. [Google Scholar] [CrossRef]
- Gao, L.; Lu, G.-T.; Lu, Y.-Y.; Xiao, W.-M.; Mao, W.-J.; Tong, Z.-H.; Yang, N.; Li, B.-Q.; Yang, Q.; Ding, Y.-B.; et al. Diabetes aggravates acute pancreatitis possibly via activation of NLRP3 inflammasome in db/db mice. Am. J. Transl. Res. 2018, 10, 2015–2025. [Google Scholar]
- Mikó, A.; Farkas, N.; Garami, A.; Szabó, I.; Vincze, Á.; Veres, G.; Bajor, J.; Alizadeh, H.; Rakonczay, Z.; Vigh, É.; et al. Preexisting diabetes elevates risk of local and systemic complications in acute pancreatitis. Pancreas 2018, 47, 917–923. [Google Scholar] [CrossRef]
- Huh, J.H.; Jeon, H.; Park, S.M.; Choi, E.; Lee, G.S.; Kim, J.W.; Lee, K.J. Diabetes mellitus is associated with mortality in acute pancreatitis. J. Clin. Gastroenterol. 2018, 52, 178–183. [Google Scholar] [CrossRef]
- Type 2 Diabetes Mellitus and the Risk of Acute Pancreatitis: A Meta-Analysis—Web of Science Core Collection. Available online: https://www.webofscience.com/wos/woscc/full-record/WOS:000312794400015 (accessed on 25 July 2023).
- Zhi, M.; Zhu, X.; Lugea, A.; Waldron, R.T.; Pandol, S.J.; Li, L. Incidence of new onset diabetes mellitus secondary to acute pancreatitis: A systematic review and meta-analysis. Front. Physiol. 2019, 10, 637. [Google Scholar] [CrossRef]
- Paragomi, P.; Papachristou, G.I.; Jeong, K.; Hinton, A.; Pothoulakis, I.; Talukdar, R.; Kochhar, R.; Goenka, M.K.; Gulla, A.; Gonzalez, J.A.; et al. The relationship between pre-existing diabetes mellitus and the severity of acute pancreatitis: Report from a large international registry. Pancreatology 2022, 22, 85–91. [Google Scholar] [CrossRef]
- Qayed, E.; Shahnavaz, N. Sleisenger and Fordtran’s Gastrointestinal and Liver Disease Review and Assessment; Elsevier: Amsterdam, The Netherlands, 2021; Available online: https://www.eu.elsevierhealth.com/sleisenger-and-fordtrans-gastrointestinal-and-liver-disease-review-and-assessment-9780323636599.html (accessed on 15 July 2023).
- Banks, P.A.; Bollen, T.L.; Dervenis, C.; Gooszen, H.G.; Johnson, C.D.; Sarr, M.G.; Tsiotos, G.G.; Vege, S.S.; Acute Pancreatitis Classification Working Group. Classification of acute pancreatitis—2012: Revision of the Atlanta classification and definitions by international consensus. Gut 2013, 62, 102–111. [Google Scholar] [CrossRef]
- Ghiță, A.I.; Pahomeanu, M.R.; Negreanu, L. Epidemiological trends in acute pancreatitis: A retrospective cohort in a tertiary center over a seven year period. World J. Methodol. 2023, 13, 118–126. [Google Scholar] [CrossRef]
- American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care 2011, 34 (Suppl. S1), S62–S69. [Google Scholar] [CrossRef]
- Nawaz, H.; O’Connell, M.; Papachristou, G.I.; Yadav, D. Severity and natural history of acute pancreatitis in diabetic patients. Pancreatology 2015, 15, 247–252. [Google Scholar] [CrossRef] [PubMed]
- Shen, H.; Chang, Y.; Chen, H.; Lu, C.; Li, C. Increased risk of severe acute pancreatitis in patients with diabetes: Diabetes and severe acute pancreatitis. Diabet. Med. 2012, 29, 1419–1424. [Google Scholar] [CrossRef] [PubMed]
- Shen, H.-N.; Lu, C.-L.; Li, C.-Y. Effect of diabetes on severity and hospital mortality in patients with acute pancreatitis: A national population-based study. Diabetes Care 2012, 35, 1061–1066. [Google Scholar] [CrossRef] [PubMed]
- Fu, Y.; Liu, X.; Cui, B.; Wang, C.; Liu, Z.; Zhao, B. Clinical characteristics of concomitant diabetic ketoacidosis in type 2 diabetes patients with acute pancreatitis. Diabetes Metab. Syndr. Obes. Targets Ther. 2022, 15, 111–119. [Google Scholar] [CrossRef] [PubMed]
- Weissman, S.; Pandol, S.J.; Ghaffar, U.; Boafo, M.; Ogbu, C.E.; Zahdeh, T.; Ashary, M.; Nagesh, V.K.; Kigga, A.; Bangolo, A.; et al. Impact of sex and comorbid diabetes on hospitalization outcomes in acute pancreatitis: A large United States population-based study. AIMS Public Health 2023, 10, 105–115. [Google Scholar] [CrossRef] [PubMed]
- Pendharkar, S.A.; Mathew, J.; Petrov, M.S. Age- and sex-specific prevalence of diabetes associated with diseases of the exocrine pancreas: A population-based study. Dig. Liver Dis. 2017, 49, 540–544. [Google Scholar] [CrossRef]
- Li, X.; Guo, X.; Ji, H.; Niu, J.; Gao, P. Relationships between metabolic comorbidities and occurrence, severity, and outcomes in patients with acute pancreatitis: A narrative review. BioMed Res. Int. 2019, 2019, 2645926. [Google Scholar] [CrossRef]
- Nøjgaard, C.; Matzen, P.; Bendtsen, F.; Andersen, J.R.; Christensen, E.; Becker, U. Factors associated with long-term mortality in acute pancreatitis. Scand. J. Gastroenterol. 2011, 46, 495–502. [Google Scholar] [CrossRef] [PubMed]
- Sun, Y.; Jin, J.; Zhu, A.; Hu, H.; Lu, Y.; Zeng, Y.; Jing, D. Risk factors for recurrent pancreatitis after first episode of acute pancreatitis. Int. J. Gen. Med. 2022, 15, 1319–1328. [Google Scholar] [CrossRef] [PubMed]
- Durmuş, E.T.; Akdağ, İ.; Yıldız, M. Diabetes is an independent predictor of severe acute pancreatitis. Postgrad. Med. 2022, 134, 711–716. [Google Scholar] [CrossRef] [PubMed]
- Xiao, B.; Xu, H.-B.; Jiang, Z.-Q.; Hu, J.-X.; Yang, G.-D. Acute pancreatitis in patients with a medical history of type 2 diabetes mellitus. Pancreas 2020, 49, 591–597. [Google Scholar] [CrossRef]
- Han, E.; Koea, J.; Hammill, C.; Srinivasa, S. The importance of smoking cessation in pancreatitis. ANZ J. Surg. 2022, 92, 2780–2781. [Google Scholar] [CrossRef]
- Aune, D.; Mahamat-Saleh, Y.; Norat, T.; Riboli, E. Tobacco smoking and the risk of pancreatitis: A systematic review and meta-analysis of prospective studies. Pancreatology 2019, 19, 1009–1022. [Google Scholar] [CrossRef]
- Majumder, S.; Gierisch, J.M.; Bastian, L.A. The association of smoking and acute pancreatitis: A systematic review and meta-analysis: A systematic review and meta-analysis. Pancreas 2015, 44, 540–546. [Google Scholar] [CrossRef]
- Birrell, L.; McGuinness, M.; Elliott, B.; Harmston, C. Effect of rurality and ethnicity in severity and outcomes in patients with acute pancreatitis. ANZ J. Surg. 2021, 91, 1558–1562. [Google Scholar] [CrossRef]
- Fan, J.; Ding, L.; Lu, Y.; Zheng, J.; Zeng, Y.; Huang, C. Epidemiology and etiology of acute pancreatitis in urban and suburban areas in Shanghai: A retrospective study. Gastroenterol. Res. Pract. 2018, 2018, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Pang, Y.; Kartsonaki, C.; Turnbull, I.; Guo, Y.; Yang, L.; Bian, Z.; Chen, Y.; Millwood, I.Y.; Bragg, F.; Gong, W.; et al. Metabolic and lifestyle risk factors for acute pancreatitis in Chinese adults: A prospective cohort study of 0.5 million people. PLOS Med. 2018, 15, e1002618. [Google Scholar] [CrossRef] [PubMed]
- Noel, R.A.; Braun, D.K.; Patterson, R.E.; Bloomgren, G.L. Increased risk of acute pancreatitis and biliary disease observed in patients with type 2 diabetes. Diabetes Care 2009, 32, 834–838. [Google Scholar] [CrossRef] [PubMed]
- Urushihara, H.; Taketsuna, M.; Liu, Y.; Oda, E.; Nakamura, M.; Nishiuma, S.; Maeda, R. Increased risk of acute pancreatitis in patients with type 2 diabetes: An observational study using a Japanese hospital database. PLoS ONE 2012, 7, e53224. [Google Scholar] [CrossRef] [PubMed]
- Méndez-Bailón, M.; Yanes, J.M.d.M.; Jiménez-García, R.; Hernández-Barrera, V.; Pérez-Farinós, N.; López-De-Andrés, A. National trends in incidence and outcomes of acute pancreatitis among type 2 diabetics and non-diabetics in Spain (2001–2011). Pancreatology 2015, 15, 64–70. [Google Scholar] [CrossRef] [PubMed]

| Acute pancreatitis (AP) and recurrent AP (RAP) cases | 1855 |
| Recurrence | |
| AP (first known attack) | 1536 (82.8%) |
| RAP | 319 (17.2%) |
| Age (years) | |
| Median | 57 (IQR = 26.0) |
| Mean | 56.9 (SD = 17.1) |
| Days of hospitalization | |
| Median | 7.0 (IQR = 6.0) |
| Mean | 8.8 (SD = 7.8) |
| Daily cost of hospitalization (RON) | |
| Median | 920.9 (IQR = 432.5) |
| Mean | 2153.1 (SD = 17,129.9) |
| Etiology | |
| Type 2 diabetes mellitus (T2DM) | 55 (3.0%) |
| Idiopathic | 283 (15.2%) |
| All other known causes, such as: | 1517 (81.8%) |
| 732 (39.5%) |
| 628 (33.9%) |
| 58 (3.1%) |
| 30 (1.6%) |
| 19 (1.0%) |
| 50 (2.7%) |
| Sex | |
| Male | 1098 (59.2%) |
| Female | 757 (40.8%) |
| Severity | |
| Mild | 954 (51.4%) |
| Moderate | 677 (36.5%) |
| Severe | 224 (12.1%) |
| Morphology | |
| Interstitial | 715 (38.5%) |
| Normal pancreas | 274 (14.8%) |
| APFC | 136 (7.3%) |
| ANC | 87 (4.7%) |
| Pseudocyst | 76 (4.1%) |
| WON | 5 (0.3%) |
| No data | 562 (30.3%) |
| Outcome | |
| Healed/ameliorated | 1540 (83.0%) |
| Discharged at will | 116 (6.3%) |
| Deceased | 108 (5.8%) |
| Transferred | 79 (4.3%) |
| Stationary | 12 (0.6%) |
| ICU | |
| No | 1676 (90.4%) |
| Yes | 179 (9.6%) |
| Tobacco smoking | |
| Active | 324 (17.5%) |
| Former (>4 weeks) | 90 (4.9%) |
| Never | 35 (1.9%) |
| No data | 1406 (75.8%) |
| Ward of origin | |
| Gastroenterology | 941 (50.7%) |
| Surgery | 914 (49.3%) |
| Place of origin | |
| Urban | 1332 (71.8%) |
| Rural | 507 (27.3%) |
| No data | 16 (0.9%) |
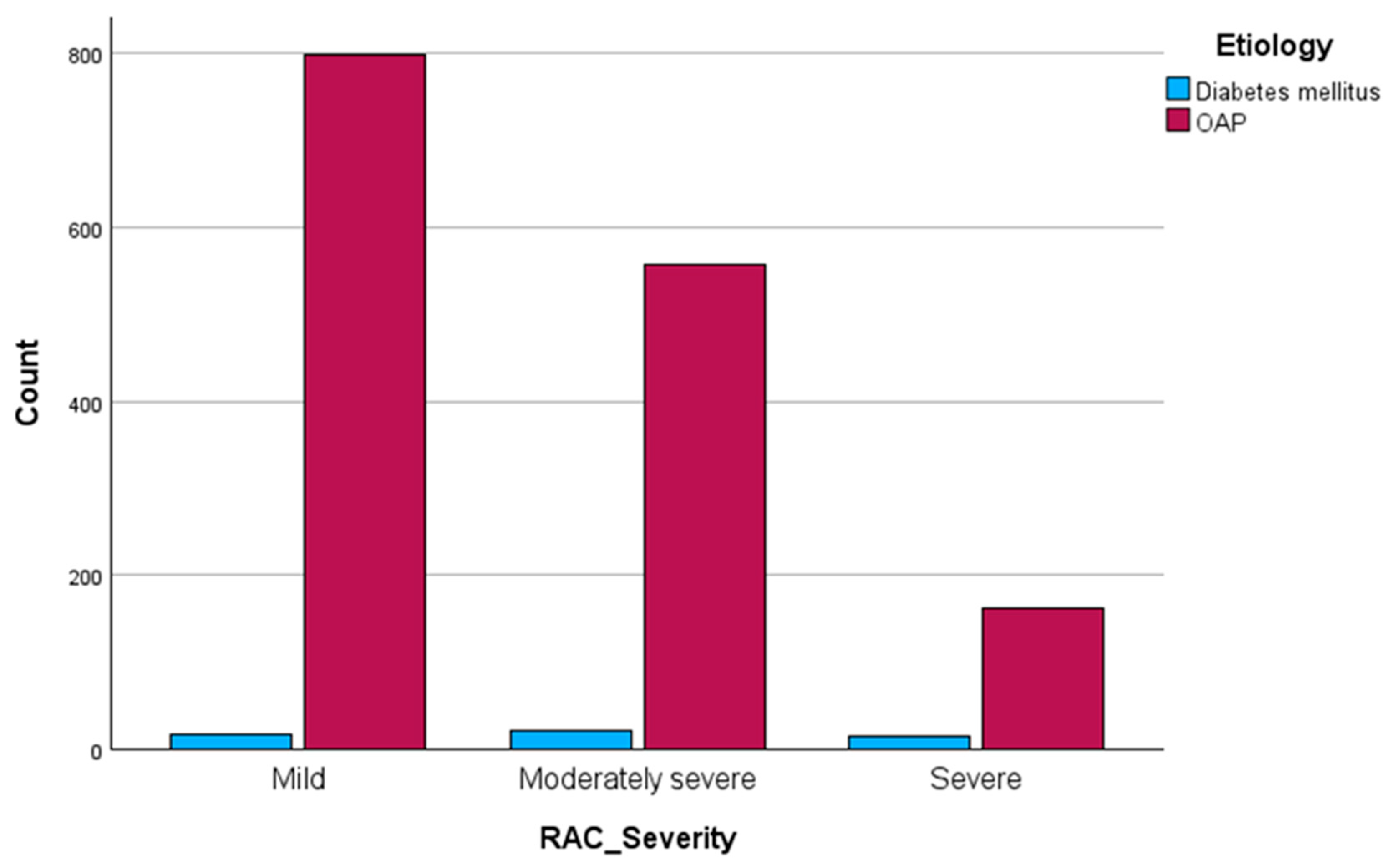
| T2DM-AP (n = 55) | OAP (n = 1517) | p Value | |
|---|---|---|---|
| Severity | |||
| Mild | 17 (30.9%) | 798 (52.6%) | p < 0.01 |
| Moderately severe | 22 (40.0%) | 557 (36.7%) | |
| Severe | 16 (29.1%) | 162 (10.7%) | |
| ICU | |||
| No | 43 (78.2%) | 1394 (91.9%) | p < 0.01 |
| Yes | 12 (21.8%) | 123 (8.1%) | |
| Ward of care | |||
| Gastroenterology | 29 (52.7%) | 757 (49.9%) | p = 0.68 |
| Surgery | 26 (47.3%) | 760 (50.1%) | |
| Gender | |||
| Male | 28 (50.9%) | 926 (61.0%) | p = 0.13 |
| Female | 27 (49.1%) | 591 (39.0%) | |
| Outcome | |||
| Healed/ameliorated | 45 (81.8%) | 1273 (83.9%) | p = 0.50 |
| Stationary | 0 (0.0%) | 11 (0.7%) | |
| Transferred | 2 (3.6%) | 71 (4.7%) | |
| Discharged at will | 3 (5.5%) | 97 (6.4%) | |
| Deceased | 5 (9.1%) | 65 (4.3%) | |
| Recurrence | |||
| First attack | 45 (81.8%) | 1244 (82.0%) | p = 0.97 |
| Recurrence | 10 (18.2%) | 273 (18.0%) | |
| Morphology | |||
| Interstitial | 21 (38.2%) | 602 (39.7%) | p = 0.64 |
| APFC | 4 (7.3%) | 115 (7.6%) | |
| Pseudocyst | 0 (0.0%) | 60 (4.0%) | |
| ANC | 4 (7.3%) | 57 (3.8%) | |
| WON | 0 (0.0%) | 4 (0.3%) | |
| Normal pancreas | 8 (14.5%) | 234 (15.4%) | |
| No data | 18 (32.7%) | 445 (29.3%) | |
| Tobacco smoking | |||
| Active | 7 (12.7%) | 285 (18.8%) | p = 0.18 |
| Former | 1 (1.8%) | 80 (5.3%) | |
| Never | 2 (3.6%) | 24 (1.6%) | |
| No data | 45 (81.9%) | 1128 (74.3%) | |
| Rurality | |||
| Urban | 44 (80.0%) | 1070 (70.5%) | p = 0.28 |
| Rural | 11 (20.0%) | 432 (28.5%) | |
| No data | 0 (0.0%) | 15 (1.0%) | |
| Age (years) | |||
| Mean | 58.6 (SD = 13.7) | 56.7 (SD = 17.0) | p = 0.42 |
| Median | 58 (IQR = 20) | 56 (IQR = 25) | |
| Length of hospital stay (days) | |||
| Mean | 9.2 (SD = 7.6) | 8.7 (SD = 7.3) | p = 0.80 |
| Median | 6 (IQR = 7) | 7 (IQR = 5.5) | |
| Length of ICU stay (days) | |||
| Mean | 4.2 (SD = 4.3) | 5.3 (SD = 5.5) | p = 0.52 |
| Median | 3.5 (IQR = 2.7) | 3 (IQR = 5) | |
| Daily hospitalization cost (RON) | |||
| Mean | 1164.9 (SD = 1265.3) | 2173.9 (SD = 17,640.5) | p = 0.98 |
| Median | 874.3 (IQR = 518.5) | 930.9 (IQR = 420.5) | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pahomeanu, M.R.; Ojog, D.; Nițu, D.T.; Diaconu, I.Ș.; Nayyerani, H.; Negreanu, L. Acute Pancreatitis and Type 2 Diabetes Mellitus: The Chicken–Egg Paradox—A Seven-Year Experience of a Large Tertiary Center. J. Clin. Med. 2024, 13, 1213. https://doi.org/10.3390/jcm13051213
Pahomeanu MR, Ojog D, Nițu DT, Diaconu IȘ, Nayyerani H, Negreanu L. Acute Pancreatitis and Type 2 Diabetes Mellitus: The Chicken–Egg Paradox—A Seven-Year Experience of a Large Tertiary Center. Journal of Clinical Medicine. 2024; 13(5):1213. https://doi.org/10.3390/jcm13051213
Chicago/Turabian StylePahomeanu, Mihai Radu, Damiana Ojog, Diana Teodora Nițu, Irina Ștefania Diaconu, Hosein Nayyerani, and Lucian Negreanu. 2024. "Acute Pancreatitis and Type 2 Diabetes Mellitus: The Chicken–Egg Paradox—A Seven-Year Experience of a Large Tertiary Center" Journal of Clinical Medicine 13, no. 5: 1213. https://doi.org/10.3390/jcm13051213
APA StylePahomeanu, M. R., Ojog, D., Nițu, D. T., Diaconu, I. Ș., Nayyerani, H., & Negreanu, L. (2024). Acute Pancreatitis and Type 2 Diabetes Mellitus: The Chicken–Egg Paradox—A Seven-Year Experience of a Large Tertiary Center. Journal of Clinical Medicine, 13(5), 1213. https://doi.org/10.3390/jcm13051213






