Moderate Intra-Abdominal Pressure Levels in Robot-Assisted Radical Prostatectomy Seem to Have No Negative Impact on Clinical Outcomes
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Data Curation
2.3. Statistics
3. Results
3.1. Characteristics of the Study Population
3.2. Characteristics of the RALRP Procedures Performed
- Number of trocars: 4;
- Trocar sizes: four 8 mm trocars (three trocars for the robotic arms and one for the camera/extraction), one 5 mm trocar (for assistant or suction), and one 12 mm trocar (for assistant or insufflation);
- Insufflation: high-flow, low-pressure pneumoperitoneum; standard IAP 10 mmHg, temporary increase to 15 mmHg during the manipulation of the prostatic plexus for 1–3 min, reduction to 5 mmHg during the lymphadenectomy in the final 20 min of the surgery.
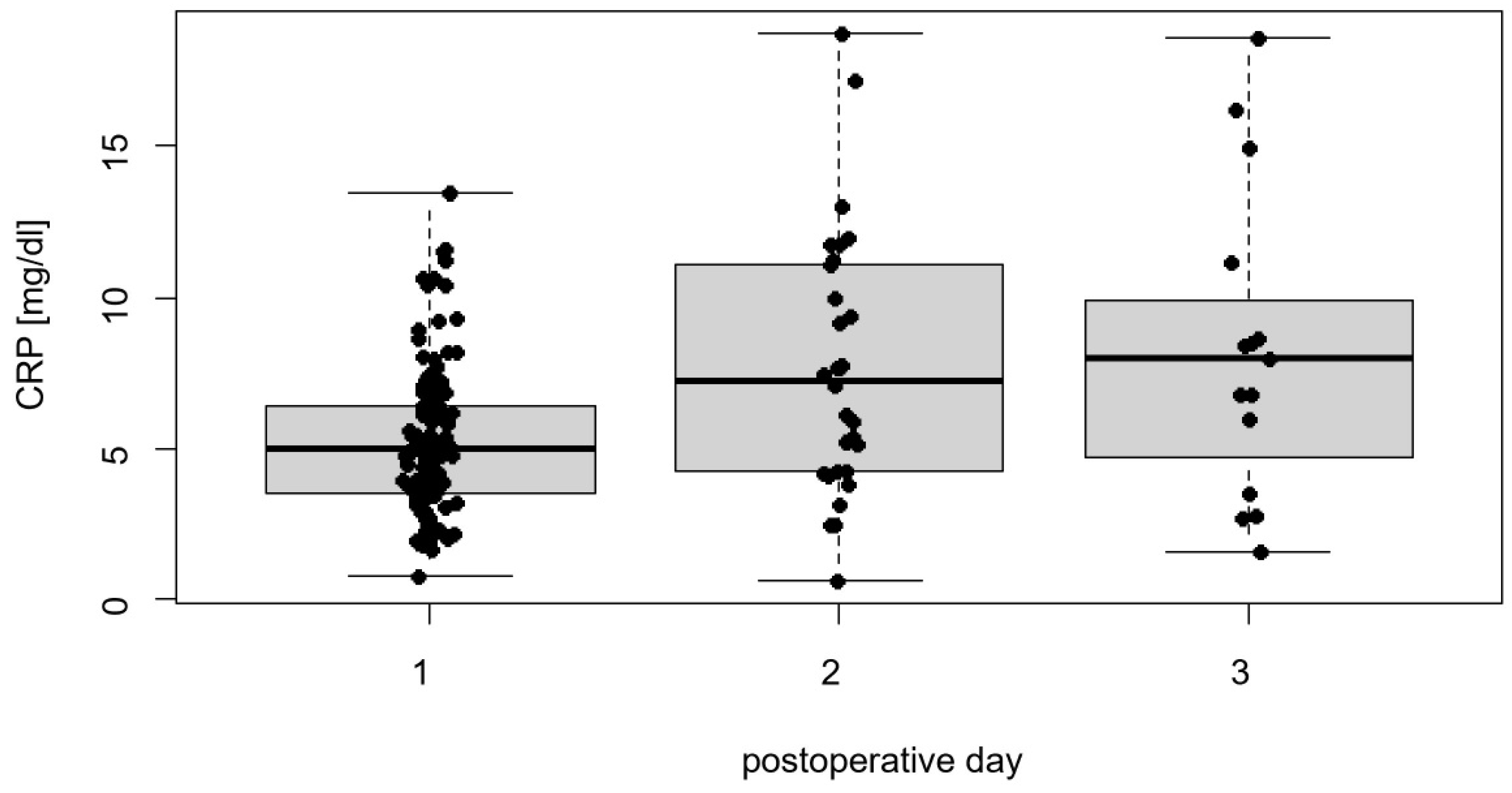
3.3. Postoperative Clinical Outcomes
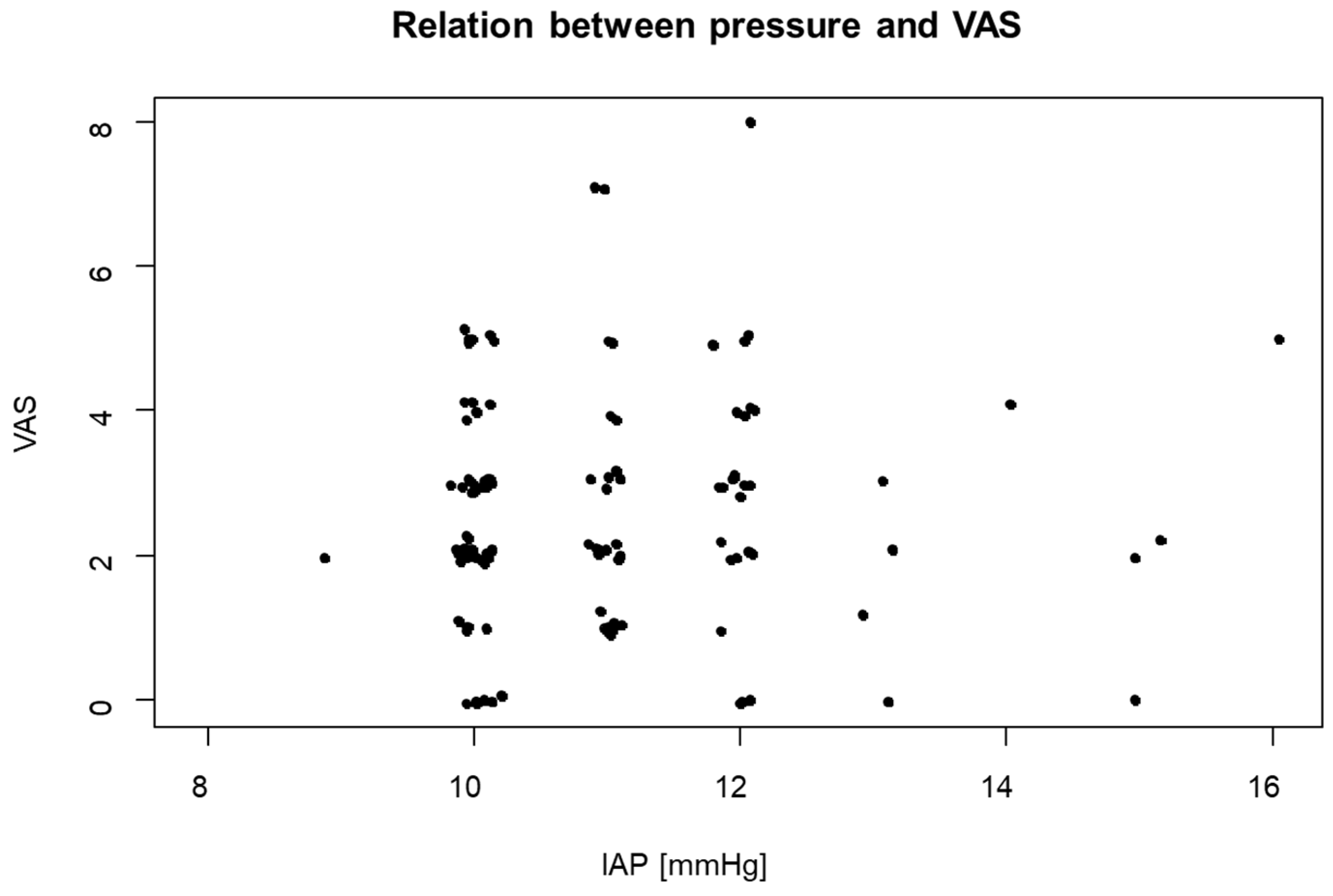
3.4. Effects of Capnoperitoneum on the Clinical Outcome
3.5. Effects of Visceral Fat on the Inflammatory Response
3.6. Effects of Dexamethasone on the Clinical Outcome
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Loscalzo, J.; Fauci, A.S.; Kasper, D.L.; Hauser, S.L.; Longo, D.L.; Jameson, J.L. (Eds.) Harrison’s Principles of Internal Medicine, 21st ed.; McGraw-Hill: New York, NY, USA; Chicago, IL, USA; San Francisco, CA, USA; Athens, Greece; London, UK; Madrid, Spain; Mexico City, Mexico; Milan, Italy; New Delhi, India; Singapore; Sydney, Australia; Toronto, ON, Canada, 2022; ISBN 9781264268504. [Google Scholar]
- Ficarra, V.; Novara, G.; Artibani, W.; Cestari, A.; Galfano, A.; Graefen, M.; Guazzoni, G.; Guillonneau, B.; Menon, M.; Montorsi, F.; et al. Retropubic, laparoscopic, and robot-assisted radical prostatectomy: A systematic review and cumulative analysis of comparative studies. Eur. Urol. 2009, 55, 1037–1063. [Google Scholar] [CrossRef]
- McAninch, J.W.; Lue, T.F. (Eds.) Smith & Tanagho’s General Urology, 19th ed.; McGraw-Hill Education LLC: New York, NY, USA, 2020; ISBN 978-1-259-83433-2. [Google Scholar]
- Neudecker, J.; Sauerland, S.; Neugebauer, E.A.M.; Bergamaschi, R.; Bonjer, H.J.; Cuschieri, A.; Fuchs, K.-H.; Jacobi, C.A.; Jansen, F.W.; Koivusalo, A.-M.; et al. The EAES Clinical Practice Guidelines on the Pneumoperitoneum for Laparoscopic Surgery (2002). In EAES Guidelines for Endoscopic Surgery; Neugebauer, E., Sauerland, S., Fingerhut, A., Millat, B., Buess, G., Eds.; Springer: Berlin/Heidelberg, Germany, 2006. [Google Scholar] [CrossRef]
- Suematsu, T.; Hirabayashi, Y.; Shiraishi, N.; Adachi, Y.; Kitamura, H.; Kitano, S. Morphology of the murine peritoneum after pneumoperitoneum vs laparotomy. Surg. Endosc. 2001, 15, 954–958. [Google Scholar] [CrossRef] [PubMed]
- Albers, K.I.; Polat, F.; Loonen, T.; Graat, L.J.; Mulier, J.P.; Snoeck, M.M.; Panhuizen, I.F.; Vermulst, A.A.; Scheffer, G.-J.; Warlé, M.C. Visualising improved peritoneal perfusion at lower intra-abdominal pressure by fluorescent imaging during laparoscopic surgery: A randomised controlled study. Int. J. Surg. 2020, 77, 8–13. [Google Scholar] [CrossRef] [PubMed]
- Junghans, T.; Böhm, B.; Gründel, K.; Schwenk, W.; Müller, J.M. Does pneumoperitoneum with different gases, body positions, and intraperitoneal pressures influence renal and hepatic blood flow? Surgery 1997, 121, 206–211. [Google Scholar] [CrossRef] [PubMed]
- Papparella, A.; Nino, F.; Coppola, S.; Noviello, C.; Paciello, O.; Papparella, S. Peritoneal morphological changes due to pneumoperitoneum: The effect of intra-abdominal pressure. Eur. J. Pediatr. Surg. 2014, 24, 322–327. [Google Scholar] [CrossRef] [PubMed]
- Zur Mertens Borg, I.R.A.M.; Lim, A.; Verbrugge, S.J.C.; IJzermans, J.N.M.; Klein, J. Effect of intraabdominal pressure elevation and positioning on hemodynamic responses during carbon dioxide pneumoperitoneum for laparoscopic donor nephrectomy: A prospective controlled clinical study. Surg. Endosc. 2004, 18, 919–923. [Google Scholar] [CrossRef] [PubMed]
- Alhusseinawi, H.; Sander, L.; Rosenvinge, P.M.; Jensen, S.L.; Bruun, N.H.; Kingo, P.S.; Jensen, J.B.; Rasmussen, S. Low- versus standard-pneumoperitoneum in patients undergoing robot-assisted radical prostatectomy: A randomised, triple-blinded study. BJU Int. 2023, 132, 560–567. [Google Scholar] [CrossRef] [PubMed]
- Abaza, R.; Ferroni, M.C. Randomized trial of ultralow vs standard pneumoperitoneum during robotic prostatectomy. J. Urol. 2022, 208, 626–632. [Google Scholar] [CrossRef] [PubMed]
- Fahy, B.G.; Barnas, G.M.; Flowers, J.L.; Nagle, S.E.; Njoku, M.J. The effects of increased abdominal pressure on lung and chest wall mechanics during laparoscopic surgery. Anesth. Analg. 1995, 81, 744–750. [Google Scholar] [CrossRef] [PubMed]
- Liem, T.K.; Krishnamoorthy, M.; Applebaum, H.; Kolata, R.; Rudd, R.G.; Chen, W. A comparison of the hemodynamic and ventilatory effects of abdominal insufflation with helium and carbon dioxide in young swine. J. Pediatr. Surg. 1996, 31, 297–300. [Google Scholar] [CrossRef]
- Brokelman, W.J.A.; Lensvelt, M.; Borel Rinkes, I.H.M.; Klinkenbijl, J.H.G.; Reijnen, M.M.P.J. Peritoneal changes due to laparoscopic surgery. Surg. Endosc. 2011, 25, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Neuhaus, S.J.; Watson, D.I.; Ellis, T.; Lafullarde, T.; Jamieson, G.G.; Russell, W.J. Metabolic and immunologic consequences of laparoscopy with helium or carbon dioxide insufflation: A randomized clinical study. ANZ J. Surg. 2001, 71, 447–452. [Google Scholar] [CrossRef] [PubMed]
- Kuebler, J.F.; Vieten, G.; Shimotakahara, A.; Metzelder, M.L.; Jesch, N.K.; Ure, B.M. Acidification during carbon dioxide pneumoperitoneum is restricted to the gas-exposed peritoneal surface: Effects of pressure, gas flow, and additional intraperitoneal fluids. J. Laparoendosc. Adv. Surg. Technol. A 2006, 16, 654–658. [Google Scholar] [CrossRef]
- Hutley, L.; Prins, J.B. Fat as an endocrine organ: Relationship to the metabolic syndrome. Am. J. Med. Sci. 2005, 330, 280–289. [Google Scholar] [CrossRef]
- Okamura, A.; Watanabe, M.; Fukudome, I.; Yamashita, K.; Yuda, M.; Hayami, M.; Imamura, Y.; Mine, S. Relationship Between Visceral Obesity and Postoperative Inflammatory Response Following Minimally Invasive Esophagectomy. World J. Surg. 2018, 42, 3651–3657. [Google Scholar] [CrossRef] [PubMed]
- Pisitsak, C.; Lee, J.G.H.; Boyd, J.H.; Coxson, H.O.; Russell, J.A.; Walley, K.R. Increased Ratio of Visceral to Subcutaneous Adipose Tissue in Septic Patients Is Associated With Adverse Outcome. Crit. Care Med. 2016, 44, 1966–1973. [Google Scholar] [CrossRef]
- Ferroni, M.C.; Abaza, R. Feasibility of robot-assisted prostatectomy performed at ultra-low pneumoperitoneum pressure of 6 mmHg and comparison of clinical outcomes vs standard pressure of 15 mmHg. BJU Int. 2019, 124, 308–313. [Google Scholar] [CrossRef] [PubMed]
- Koninckx, P.R.; Corona, R.; Timmerman, D.; Verguts, J.; Adamyan, L. Peritoneal full-conditioning reduces postoperative ad-hesions and pain: A randomised controlled trial in deep endometriosis surgery. J. Ovarian Res. 2013, 6, 90. [Google Scholar] [CrossRef]
- Gadekar, T.; Dudeja, P.; Basu, I.; Vashisht, S.; Mukherji, S. Correlation of visceral body fat with waist-hip ratio, waist cir-cum-ference and body mass index in healthy adults: A cross sectional study. Med. J. Armed Forces India 2020, 76, 41–46. [Google Scholar] [CrossRef]
- Mishra, P.; Pandey, C.M.; Singh, U.; Gupta, A.; Sahu, C.; Keshri, A. Descriptive statistics and normality tests for statistical data. Ann. Card. Anaesth. 2019, 22, 67–72. [Google Scholar] [CrossRef]
- Mishra, P.; Pandey, C.M.; Singh, U.; Keshri, A.; Sabaretnam, M. Selection of appropriate statistical methods for data analysis. Ann. Card. Anaesth. 2019, 22, 297–301. [Google Scholar] [CrossRef]
- Christensen, C.R.; Maatman, T.K.; Maatman, T.J.; Tran, T.T. Examining clinical outcomes utilizing low-pressure pneu-mope-ri-toneum during robotic-assisted radical prostatectomy. J. Robot. Surg. 2016, 10, 215–219. [Google Scholar] [CrossRef]
- Ortenzi, M.; Montori, G.; Sartori, A.; Balla, A.; Botteri, E.; Piatto, G.; Gallo, G.; Vigna, S.; Guerrieri, M.; Williams, S.; et al. Low-pressure versus standard-pressure pneumoperitoneum in laparoscopic cholecystectomy: A systematic review and me-ta-analysis of randomized controlled trials. Surg. Endosc. 2022, 36, 7092–7113. [Google Scholar] [CrossRef] [PubMed]
- Rohloff, M.; Peifer, G.; Shakuri-Rad, J.; Maatman, T.J. The impact of low pressure pneumoperitoneum in robotic assisted radical prostatectomy: A prospective, randomized, double blinded trial. World J. Urol. 2021, 39, 2469–2474. [Google Scholar] [CrossRef] [PubMed]
- Martinschek, A.; Stumm, L.; Ritter, M.; Heinrich, E.; Bolenz, C.; Trojan, L. Prospective, Controlled Study of Invasiveness and Post-Aggression Metabolism in Patients Undergoing Robotic-Assisted Radical Prostatectomy. Urol. Int. 2017, 99, 201–206. [Google Scholar] [CrossRef] [PubMed]
- Roh, G.U.; Song, Y.; Park, J.; Ki, Y.M.; Han, D.W. Effects of propofol on the inflammatory response during robot-assisted lap-aroscopic radical prostatectomy: A prospective randomized controlled study. Sci. Rep. 2019, 9, 5242. [Google Scholar] [CrossRef]
- Kim, H.Y.; Lee, S.Y.; Lee, H.S.; Jun, B.K.; Choi, J.B.; Kim, J.E. Beneficial Effects of Intravenous Magnesium Administration during Robotic Radical Prostatectomy: A Randomized Controlled Trial. Adv. Ther. 2021, 38, 1701–1712. [Google Scholar] [CrossRef]
- Zargar-Shoshtari, K.; Sammour, T.; Kahokehr, A.; Connolly, A.B.; Hill, A.G. Randomized clinical trial of the effect of glucocor-ticoids on peritoneal inflammation and postoperative recovery after colectomy. Br. J. Surg. 2009, 96, 1253–1261. [Google Scholar] [CrossRef]
| Parameter | |
|---|---|
| Age in years, median | 67 (IQR 10; range 39–79) |
| Weight in kg, median | 85 (IQR 18; range 61–125) |
| Height in m, mean ± SD | 1.78 ± 0.06 m (range 1.60–1.96) |
| BMI in g/m2, median | 26.87 (IQR 5.31; range 19.88–40.96) |
| Waist circumference in cm, median | 97 (IQR 17.3; range 78–131) |
| Waist–hip ratio | 0.55 (IQR 0.09; range 0.44–0.78) |
| Property of PP | Median |
|---|---|
| Duration | 143 min (IQR 46; range 94–265) |
| Insufflation pressure at start | 10 mmHg (IQR 1; range 7–17) |
| Insufflation volume at start | 4.35 L (IQR 2.3, range 1.5–50.6) |
| Average IAP | 10 mmHg (IQR 2; range 8–16) |
| Maximum IAP | 15 mmHg (IQR 1; range 10–22) |
| Duration × average IAP | 1529 mmHg min (IQR 570; range 972–3180) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ippolito, A.; Mulier, J.; Hahn, M.; Wenzel, M.; Mandel, P.; Flinspach, A.N.; Wenger, K.J. Moderate Intra-Abdominal Pressure Levels in Robot-Assisted Radical Prostatectomy Seem to Have No Negative Impact on Clinical Outcomes. J. Clin. Med. 2024, 13, 1202. https://doi.org/10.3390/jcm13051202
Ippolito A, Mulier J, Hahn M, Wenzel M, Mandel P, Flinspach AN, Wenger KJ. Moderate Intra-Abdominal Pressure Levels in Robot-Assisted Radical Prostatectomy Seem to Have No Negative Impact on Clinical Outcomes. Journal of Clinical Medicine. 2024; 13(5):1202. https://doi.org/10.3390/jcm13051202
Chicago/Turabian StyleIppolito, Angelo, Jan Mulier, Marta Hahn, Mike Wenzel, Philipp Mandel, Armin N. Flinspach, and Katharina J. Wenger. 2024. "Moderate Intra-Abdominal Pressure Levels in Robot-Assisted Radical Prostatectomy Seem to Have No Negative Impact on Clinical Outcomes" Journal of Clinical Medicine 13, no. 5: 1202. https://doi.org/10.3390/jcm13051202
APA StyleIppolito, A., Mulier, J., Hahn, M., Wenzel, M., Mandel, P., Flinspach, A. N., & Wenger, K. J. (2024). Moderate Intra-Abdominal Pressure Levels in Robot-Assisted Radical Prostatectomy Seem to Have No Negative Impact on Clinical Outcomes. Journal of Clinical Medicine, 13(5), 1202. https://doi.org/10.3390/jcm13051202








