Long-Term Follow-Up after Iliosacral Screw Fixation of Unstable Pelvic Ring Fractures
Abstract
1. Introduction
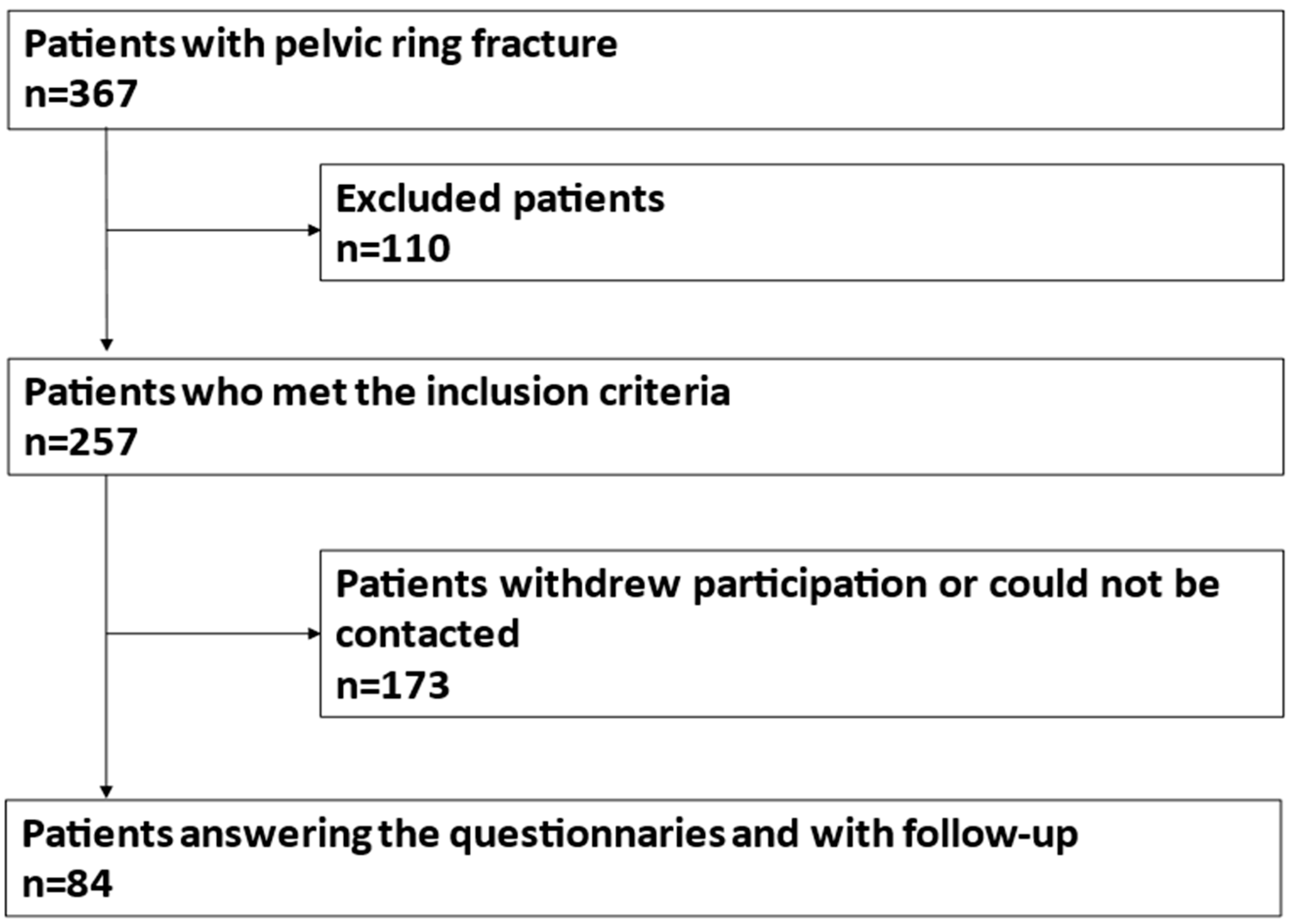
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Balogh, Z.; King, K.L.; Mackay, P.; McDougall, D.; Mackenzie, S.; Evans, J.A.; Lyons, T.; Deane, S.A. The epidemiology of pelvic ring fractures: A population-based study. J. Trauma 2007, 63, 1066–1073; discussion 1072–1073. [Google Scholar] [CrossRef] [PubMed]
- Hsu, S.-D.; Chen, C.-J.; Chou, Y.-C.; Wang, S.-H.; Chan, D.-C. Effect of Early Pelvic Binder Use in the Emergency Management of Suspected Pelvic Trauma: A Retrospective Cohort Study. Int. J. Environ. Res. Public Health 2017, 14, 1217. [Google Scholar] [CrossRef] [PubMed]
- de Ridder, V.A.; Whiting, P.S.; Balogh, Z.J.; Mir, H.R.; Schultz, B.J.; Routt, M.C. Pelvic ring injuries: Recent advances in diagnosis and treatment. OTA Int. 2023, 6, e261. [Google Scholar] [CrossRef] [PubMed]
- Pohlemann, T.; Stengel, D.; Tosounidis, G.; Reilmann, H.; Stuby, F.; Stöckle, U.; Seekamp, A.; Schmal, H.; Thannheimer, A.; Holmenschlager, F.; et al. Survival trends and predictors of mortality in severe pelvic trauma: Estimates from the German Pelvic Trauma Registry Initiative. Injury 2011, 42, 997–1002. [Google Scholar] [CrossRef] [PubMed]
- Meinberg, E.; Agel, J.; Roberts, C.; Karam, M.D.; Kellam, J.F. Fracture and Dislocation Classification Compendium–2018. J. Orthop. Trauma 2018, 32 (Suppl. S1), S1–S170. [Google Scholar] [CrossRef] [PubMed]
- van Loon, P.; Kuhn, S.; Hofmann, A.; Hessmann, M.H.; Rommens, P.M. Radiological analysis, operative management and functional outcome of open book pelvic lesions: A 13-year cohort study. Injury 2011, 42, 1012–1019. [Google Scholar] [CrossRef] [PubMed]
- Matter, P. History of the AO and its global effect on operative fracture treatment. Clin. Orthop. Relat. Res. 1998, 347, 11–18. [Google Scholar] [CrossRef]
- Keating, J.F.; Werier, J.; Blachut, P.; Broekhuyse, H.; Meek, R.N.; O’Brien, P.J. Early fixation of the vertically unstable pelvis: The role of iliosacral screw fixation of the posterior lesion. J. Orthop. Trauma 1999, 13, 107–113. [Google Scholar] [CrossRef]
- Letournel, E. Pelvic fractures. Injury 1978, 10, 145–148. [Google Scholar] [CrossRef]
- Hartensuer, R.; Lodde, M.F.; Keller, J.; Eveslage, M.; Stolberg-Stolberg, J.; Riesenbeck, O.; Raschke, M.J. Safety, Effect and Feasibility of Percutaneous SI-Screw with and without Augmentation-A 15-Year Retrospective Analysis on over 640 Screws. J. Clin. Med. 2020, 9, 2660. [Google Scholar] [CrossRef]
- Osterhoff, G.; Ossendorf, C.; Wanner, G.A.; Simmen, H.-P.; Werner, C.M.L. Posterior screw fixation in rotationally unstable pelvic ring injuries. Injury 2011, 42, 992–996. [Google Scholar] [CrossRef] [PubMed]
- Klingebiel, F.K.-L.; Hasegawa, M.; Parry, J.; Balogh, Z.J.; Sen, R.K.; Kalbas, Y.; Teuben, M.; Halvachizadeh, S.; Pape, H.-C.; Pfeifer, R. Standard practice in the treatment of unstable pelvic ring injuries: An international survey. Int. Orthop. 2023, 47, 2301–2318. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, T.; Hak, D.J.; Ziran, B.H.; Adams, S.A.; Stahel, P.F.; Morgan, S.J.; Smith, W.R. Outcome and complications of posterior transiliac plating for vertically unstable sacral fractures. Injury 2009, 40, 405–409. [Google Scholar] [CrossRef]
- Boudissa, M.; Saad, M.; Kerschbaumer, G.; Ruatti, S.; Tonetti, J. Posterior transiliac plating in vertically unstable sacral fracture. Orthop. Traumatol. Surg. Res. 2020, 106, 85–88. [Google Scholar] [CrossRef] [PubMed]
- Lodde, M.F.; Katthagen, J.C.; Schopper, C.O.; Zderic, I.; Richards, G.; Gueorguiev, B.; Raschke, M.J.; Hartensuer, R. Biomechanical Comparison of Five Fixation Techniques for Unstable Fragility Fractures of the Pelvic Ring. J. Clin. Med. 2021, 10, 2326. [Google Scholar] [CrossRef]
- Lodde, M.F.; Katthagen, J.C.; Schopper, C.O.; Zderic, I.; Richards, R.G.; Gueorguiev, B.; Raschke, M.J.; Hartensuer, R. Does Cement Augmentation of the Sacroiliac Screw Lead to Superior Biomechanical Results for Fixation of the Posterior Pelvic Ring? A Biomechanical Study. Medicina 2021, 57, 1368. [Google Scholar] [CrossRef]
- Lodde, M.F.; Raschke, M.J.; Riesenbeck, O. FFP: Indication for minimally invasive navigation technique. Trauma Case Rep. 2023, 45, 100829. [Google Scholar] [CrossRef]
- Lindahl, J.; Hirvensalo, E. Outcome of operatively treated type-C injuries of the pelvic ring. Acta Orthop. 2005, 76, 667–678. [Google Scholar] [CrossRef]
- Shetty, A.P.; Bosco, A.; Perumal, R.; Dheenadhayalan, J.; Rajasekaran, S. Midterm radiologic and functional outcomes of minimally-invasive fixation of unstable pelvic fractures using anterior internal fixator(INFIX) and percutaneous iliosacral screws. J. Clin. Orthop. Trauma 2017, 8, 241–248. [Google Scholar] [CrossRef]
- Khaled, S.A.; Soliman, O.; Wahed, M.A. Functional outcome of unstable pelvic ring injuries after iliosacral screw fixation: Single versus two screw fixation. Eur. J. Trauma Emerg. Surg. 2015, 41, 387–392. [Google Scholar] [CrossRef]
- Ghosh, S.; Aggarwal, S.; Kumar, P.; Kumar, V. Functional outcomes in pelvic fractures and the factors affecting them- A short term, prospective observational study at a tertiary care hospital. J. Clin. Orthop. Trauma 2019, 10, 896–899. [Google Scholar] [CrossRef] [PubMed]
- Gruen, G.S.; Leit, M.E.; Gruen, R.J.; Garrison, H.G.; Auble, T.E.; Peitzman, A.B. Functional outcome of patients with unstable pelvic ring fractures stabilized with open reduction and internal fixation. J. Trauma 1995, 39, 838–844; discussion 844–845. [Google Scholar] [CrossRef] [PubMed]
- Chen, P.-H.; Hsu, W.-H.; Li, Y.-Y.; Huang, T.-W.; Huang, T.-J.; Peng, K.-T. Outcome analysis of unstable posterior ring injury of the pelvis: Comparison between percutaneous iliosacral screw fixation and conservative treatment. Biomed. J. 2013, 36, 289–294. [Google Scholar] [CrossRef] [PubMed]
- Abhishek, S.M.; Prashanth; Azhar, A.L.; Vijay, G.B.; Harshal, K. Functional Outcome With Percutaneous Ilio-sacral Screw Fixation For Posterior Pelvic Ring Injuries In Patients Involved In Heavy Manual Laboring. Malays. Orthop. J. 2015, 9, 23–27. [Google Scholar] [CrossRef] [PubMed]
- Schweitzer, D.; Zylberberg, A.; Córdova, M.; Gonzalez, J. Closed reduction and iliosacral percutaneous fixation of unstable pelvic ring fractures. Injury 2008, 39, 869–874. [Google Scholar] [CrossRef] [PubMed]
- Larsen, P.; Goethgen, C.B.; Rasmussen, S.; Iyer, A.B.; Elsoe, R. One-year development of QOL following orthopaedic polytrauma: A prospective observational cohort study of 53 patients. Arch. Orthop. Trauma Surg. 2016, 136, 1539–1546. [Google Scholar] [CrossRef] [PubMed]
- Majeed, S.A. Grading the outcome of pelvic fractures. J. Bone Jt. Surg. Br. 1989, 71, 304–306. [Google Scholar] [CrossRef]
- Martin, J.G.; Marsh, J.L.; Nepola, J.V. The treatment of unstable pelvic injuries with external fixation. Am. Acad. Orthop. Surg. 1994, 18, 1053. [Google Scholar]
- Nepola, J.V.; Trenhaile, S.W.; Miranda, M.A.; Butterfield, S.L.; Fredericks, D.C.; Riemer, B.L. Vertical shear injuries: Is there a relationship between residual displacement and functional outcome? J. Trauma 1999, 46, 1024–1029; discussion 1029–1030. [Google Scholar] [CrossRef]
- de Zwart, B.C.H.; Frings-Dresen, M.H.W.; van Duivenbooden, J.C. Test-retest reliability of the Work Ability Index questionnaire. Occup. Med. 2002, 52, 177–181. [Google Scholar] [CrossRef]
- Ilmarinen, J. The Work Ability Index (WAI). Occup. Med. 2006, 57, 160. [Google Scholar] [CrossRef]
- WAI. Available online: https://www.wainetzwerk.de/uploads/z-neue%20Uploads/WAI-Netzwerk/WAI%20Fragebogen/NEU_WAI-Langversion%20mit%20Auswertung%202021.pdf (accessed on 15 October 2023).
- Ware, J.E.; Sherbourne, C.D. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med. Care 1992, 30, 473–483. [Google Scholar] [CrossRef] [PubMed]
- Available online: https://euroqol.org/publications/user-guides/ (accessed on 20 October 2023).
- Brazier, J.; Jones, N.; Kind, P. Testing the validity of the Euroqol and comparing it with the SF-36 health survey questionnaire. Qual. Life Res. 1993, 2, 169–180. [Google Scholar] [CrossRef] [PubMed]
- van den Bosch, E.W.; van der Kleyn, R.; Hogervorst, M.; van Vugt, A.B. Functional outcome of internal fixation for pelvic ring fractures. J. Trauma 1999, 47, 365–371. [Google Scholar] [CrossRef]
- Suzuki, T.; Shindo, M.; Soma, K.; Minehara, H.; Nakamura, K.; Uchino, M.; Itoman, M. Long-term functional outcome after unstable pelvic ring fracture. J. Trauma 2007, 63, 884–888. [Google Scholar] [CrossRef]
- Oliver, C.W.; Twaddle, B.; Agel, J.; Routt, M.L. Outcome after pelvic ring fractures: Evaluation using the medical outcomes short form SF-36. Injury 1996, 27, 635–641. [Google Scholar] [CrossRef]
- Miranda, M.A.; Riemer, B.L.; Butterfield, S.L.; Burke, C.J. Pelvic ring injuries. A long term functional outcome study. Clin. Orthop. Relat. Res. 1996, 329, 152–159. [Google Scholar] [CrossRef]
- Cole, J.D.; Blum, D.A.; Ansel, L.J. Outcome after fixation of unstable posterior pelvic ring injuries. Clin. Orthop. Relat. Res. 1996, 329, 160–179. [Google Scholar] [CrossRef]
- Gabbe, B.J.; Stewart, I.; Veitch, W.; Beck, B.; Cameron, P.; Russ, M.; Bucknill, A.; de Steiger, R.; Esser, M. Long-term outcomes of major trauma with unstable open pelvic fractures: A population-based cohort study. Trauma 2021, 23, 111–119. [Google Scholar] [CrossRef]
- Brenneman, F.D.; Katyal, D.; Boulanger, B.R.; Tile, M.; Redelmeier, D.A. Long-term outcomes in open pelvic fractures. J. Trauma 1997, 42, 773–777. [Google Scholar] [CrossRef]
- Dujardin, F.H.; Hossenbaccus, M.; Duparc, F.; Biga, N.; Thomine, J.M. Long-term functional prognosis of posterior injuries in high-energy pelvic disruption. J. Orthop. Trauma 1998, 12, 145–150; discussion 150–151. [Google Scholar] [CrossRef]
- Korovessis, P.; Baikousis, A.; Stamatakis, M.; Katonis, P. Medium- and long-term results of open reduction and internal fixation for unstable pelvic ring fractures. Orthopedics 2000, 23, 1165–1171. [Google Scholar] [CrossRef]
- Kabak, S.; Halici, M.; Tuncel, M.; Avsarogullari, L.; Baktir, A.; Basturk, M. Functional outcome of open reduction and internal fixation for completely unstable pelvic ring fractures (type C): A report of 40 cases. J. Orthop. Trauma 2003, 17, 555–562. [Google Scholar] [CrossRef] [PubMed]
- Sørensen, J.; Davidsen, M.; Gudex, C.; Pedersen, K.M.; Brønnum-Hansen, H. Danish EQ-5D population norms. Scand. J. Public Health 2009, 37, 467–474. [Google Scholar] [CrossRef] [PubMed]
- Ellert, U.; Kurth, B.M. Gesundheitsbezogene Lebensqualität bei Erwachsenen in Deutschland: Ergebnisse der Studie zur Gesundheit Erwachsener in Deutschland (DEGS1). Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz 2013, 56, 643–649. [Google Scholar] [CrossRef]
- Grochtdreis, T.; Dams, J.; König, H.-H.; Konnopka, A. Health-related quality of life measured with the EQ-5D-5L: Estimation of normative index values based on a representative German population sample and value set. Eur. J. Health Econ. 2019, 20, 933–944. [Google Scholar] [CrossRef] [PubMed]
- Lodde, M.F.; Fischer, T.M.; Riesenbeck, O.; Roßlenbroich, S.; Katthagen, J.C.; Rometsch, D.; Günes, D.; Schneider, M.; Raschke, M.J.; Liljenqvist, U. Analysis of the Spinopelvic Parameters in Patients with Fragility Fractures of the Pelvis. J. Clin. Med. 2023, 12, 4445. [Google Scholar] [CrossRef] [PubMed]
- Reilly, M.C.; Zinar, D.M.; Matta, J.M. Neurologic injuries in pelvic ring fractures. Clin. Orthop. Relat. Res. 1996, 329, 28–36. [Google Scholar] [CrossRef] [PubMed]
- Schmid, F.A.; Held, U.; Eberli, D.; Pape, H.-C.; Halvachizadeh, S. Erectile dysfunction and penile rehabilitation after pelvic fracture: A systematic review and meta-analysis. BMJ Open 2021, 11, e045117. [Google Scholar] [CrossRef] [PubMed]
- Ter-Grigorian, A.A.; Kasyan, G.R.; Pushkar, D.Y. Urogenital disorders after pelvic ring injuries. Cent. Eur. J. Urol. 2013, 66, 352–356. [Google Scholar] [CrossRef]
- Lefaivre, K.A.; Slobogean, G.P.; Valeriote, J.; O’Brien, P.J.; Macadam, S.A. Reporting and interpretation of the functional outcomes after the surgical treatment of disruptions of the pelvic ring: A systematic review. J. Bone Jt. Surg. Br. 2012, 94, 549–555. [Google Scholar] [CrossRef] [PubMed]
- Kane, R.L. (Ed.) Understanding Health Care Outcomes Research, 2nd.; Jones and Bartlett: Sudbury, MA, USA, 2006; ISBN 0763734411. [Google Scholar]
- Kreder, H.J.; Wright, J.G.; McLeod, R. Outcome studies in surgical research. Surgery 1997, 121, 223–225. [Google Scholar] [CrossRef] [PubMed]
- Tornetta, P.; Dickson, K.; Matta, J.M. Outcome of rotationally unstable pelvic ring injuries treated operatively. Clin. Orthop. Relat. Res. 1996, 329, 147–151. [Google Scholar] [CrossRef] [PubMed]
- Rommens, P.M.; Hessmann, M.H. Staged reconstruction of pelvic ring disruption: Differences in morbidity, mortality, radiologic results, and functional outcomes between B1, B2/B3, and C-type lesions. J. Orthop. Trauma 2002, 16, 92–98. [Google Scholar] [CrossRef] [PubMed]
- Neufeld, M.E.; Broekhuyse, H.M.; OʼBrien, P.J.; Guy, P.; Lefaivre, K.A. The Longitudinal Short-, Medium-, and Long-Term Functional Recovery After Unstable Pelvic Ring Injuries. J. Orthop. Trauma 2019, 33, 608–613. [Google Scholar] [CrossRef]
- Pohlemann, T.; Gänsslen, A.; Schellwald, O.; Culemann, U.; Tscherne, H. Outcome after pelvic ring injuries. Injury 1996, 27 (Suppl. 2), 31–38. [Google Scholar] [CrossRef]
- Henderson, R.C. The long-term results of nonoperatively treated major pelvic disruptions. J. Orthop. Trauma 1989, 3, 41–47. [Google Scholar] [CrossRef]
- McLaren, A.C.; Rorabeck, C.H.; Halpenny, J. Long-term pain and disability in relation to residual deformity after displaced pelvic ring fractures. Can. J. Surg. 1990, 33, 492–494. [Google Scholar]
- Cen, X.; Song, Y.; Yu, P.; Sun, D.; Simon, J.; Bíró, I.; Gu, Y. Effects of plantar fascia stiffness on the internal mechanics of idiopathic pes cavus by finite element analysis: Implications for metatarsalgia. Comput. Methods Biomech. Biomed. Engin. 2023, 1–9. [Google Scholar] [CrossRef]
| EQ5D-5L | SF-36 | MPS | IPS | WAI |
|---|---|---|---|---|
| Standardized and widely accepted tool to measure health outcome after orthopedic polytrauma injuries. Based on 5 dimensions each with 5 levels. | General health assessment. Based on 36 questions and divided into 8 subscales. | Pelvic-specific assessment of function after major pelvic injury including five categories: Sitting, pain, work, sexual intercourse, mobility. | Instrument to assess functional pelvic specific outcome consisting of six categories: activity of daily living, work history, pain, limp, visual pain line, and cosmesis. | Tool of clinical and occupational research to examine work ability including general health questions and subjective assessment of the ability to work. |
| SF-36 General Health (GH) | Mean 63.06 (SD 22.87) |
| SF-36 Physical Functioning (PF) | Mean 71.25 (SD 29.61) |
| SF-36 Bodily pain (BP) | Mean 71.49 (SD 29.50) |
| SF-36 Vitality (VT) | Mean 57.44 (SD 22.38) |
| SF-36 Mental Health (MH) | Mean 72.34 (SD 20.73) |
| SF-36 Social functioning (SF) | Mean 81.48 (SD 23.78) |
| SF-36 Role-functioning physical (RP) | Mean 66.98 (SD 44.34) |
| SF-36 Role-functioning emotional (RE) | Mean 80.25 (SD 34.47) |
| Score | Mean of Subgroup Fracture Classification | p Value (Man-Whitney-U-Test) | Mean of Subgroup Uni- vs. Bilateral Fractures | p Value (Man-Whitney-U-Test) * Indicates a Significant Value (p < 0.05) | Correlation (Spearman’s-Rank Correlation) | ||
|---|---|---|---|---|---|---|---|
| AO 61B | AO 61C | Unilateral | Bilateral | ISS Correlation Coefficient (p-Value) | |||
| EQ5D-5L | 0.82 | 0.83 | 0.476 | 0.85 | 0.79 | 0.431 | −0.061 (0.584) |
| SF 36 Physical functioning | 69.67 | 72.13 | 0.600 | 72.42 | 67.95 | 0.662 | −0.105 (0.340) |
| SF 36 Role emotional | 81.61 | 79.49 | 0.741 | 80.00 | 80.95 | 0.644 | 0.072 (0.520) |
| SF 36 Role physical | 69.64 | 65.57 | 0.878 | 70.00 | 58.33 | 0.258 | 0.013 (0.908) |
| SF 36 Vitality | 55.50 | 58.52 | 0.512 | 56.77 | 59.32 | 0.725 | 0.061 (0.579) |
| SF 36 Mental Health | 73.20 | 71.85 | 0.703 | 72.13 | 72.91 | 0.756 | −0.014 (0.903) |
| SF 36 Social functioning | 77.92 | 83.49 | 0.119 | 82.17 | 79.55 | 0.771 | −0.037 (0.737) |
| SF 36 Bodily pain | 74.58 | 69.77 | 0.467 | 73.43 | 66.02 | 0.354 | −0.127 (0.251) |
| SF 36 General Health | 62.93 | 63.14 | 0.960 | 63.10 | 62.95 | 0.957 | −0.116 (0.304) |
| WAI | 31.97 | 33.08 | 0.399 | 32.79 | 32.45 | 0.874 | −0.116 (0.448) |
| MPS | 86.52 | 81.69 | 0.533 | 84.88 | 78.25 | 0.193 | −0.230 (0.060) |
| IPS | 78.88 | 77.32 | 0.822 | 79.56 | 73.11 | 0.033 | −0.237 * (0.043) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Stolberg-Stolberg, J.; Lodde, M.F.; Seiß, D.; Köppe, J.; Hartensuer, R.; Raschke, M.J.; Riesenbeck, O. Long-Term Follow-Up after Iliosacral Screw Fixation of Unstable Pelvic Ring Fractures. J. Clin. Med. 2024, 13, 1070. https://doi.org/10.3390/jcm13041070
Stolberg-Stolberg J, Lodde MF, Seiß D, Köppe J, Hartensuer R, Raschke MJ, Riesenbeck O. Long-Term Follow-Up after Iliosacral Screw Fixation of Unstable Pelvic Ring Fractures. Journal of Clinical Medicine. 2024; 13(4):1070. https://doi.org/10.3390/jcm13041070
Chicago/Turabian StyleStolberg-Stolberg, Josef, Moritz F. Lodde, Dominik Seiß, Jeanette Köppe, René Hartensuer, Michael J. Raschke, and Oliver Riesenbeck. 2024. "Long-Term Follow-Up after Iliosacral Screw Fixation of Unstable Pelvic Ring Fractures" Journal of Clinical Medicine 13, no. 4: 1070. https://doi.org/10.3390/jcm13041070
APA StyleStolberg-Stolberg, J., Lodde, M. F., Seiß, D., Köppe, J., Hartensuer, R., Raschke, M. J., & Riesenbeck, O. (2024). Long-Term Follow-Up after Iliosacral Screw Fixation of Unstable Pelvic Ring Fractures. Journal of Clinical Medicine, 13(4), 1070. https://doi.org/10.3390/jcm13041070







