1. Introduction
The incidence of spinal cord injury (SCI) following high-voltage electrical trauma ranges between 2 and 5%. SCI can occur early or late after trauma. Early SCI occurs in patients within a few hours of the injury and they recover within a few days [
1]. Delayed SCI occurs a few days to a few months after electrical trauma and becomes permanent as incomplete SCI [
1,
2]. Tissue mechanisms caused by electricity include trauma, ischemic injury, heating effect, and electroporation [
3]. The heating effect causes early SCI, and cell membrane rupture due to electroporation causes delayed SCI. Ischemic injury caused by endothelial injury or thrombosis is also a major cause of delayed SCI [
4,
5]. There is a lot of damage to the anterior spinal cord, where many blood vessels are distributed, and motor tracks passing through this area are damaged, causing motor function deterioration [
4]. However, there is no specific imaging test used to diagnose SCI caused by electrical trauma, and imaging tests are often judged to be normal [
6]. When symptoms of SCI occur, imaging test results are usually normal. Thus, the diagnosis of neurological injury is based on progress and clinical findings. Early recognition of SCI could be important to initiating intensive rehabilitation as early as possible. Patients with SCI have varying degrees of muscle weakness, spasticity, and impaired balance. The most challenging complication of SCI is walking impairment [
7]. Additionally, hypertrophic scarring caused by electrical burns causes joint contracture and sensorimotor disturbances, which reduces gait function [
8].
Conventional physical therapy for a patient with SCI focuses on muscle strengthening, stretching, and manually assisted gait training. Manually assisted gait training helps to strengthen lower extremity muscles and improve walking ability. As in normal walking, exercises to move the lower extremities are required to activate the locomotor centers in the spinal cord. However, in reality, manually assisted gait training by therapists requires significant effort from the therapist, and long-term training is not possible. Patients who cannot walk independently need the help of a mechanical system to improve their walking function.
Robot-assisted gait training (RAGT) positively affects lower extremity muscle strength, gait speed, walking performance, and gait pattern in patients with central nervous system damage such as SCI or stroke [
9,
10,
11,
12,
13]. The therapeutic area of robot therapy is expanding to improve the function of musculoskeletal patients who have undergone arthroplasty or burn skin grafting [
14,
15,
16].
However, there is still no research on the application of robot training to improve gait function in patients with combined SCI and hypertrophic scars caused by electrical trauma. It was assumed that RAGT would have a positive effect in terms of improving gait function in patients with SCI caused by high-voltage electricity. The objective of this study was to demonstrate that the RAGT for 12 weeks with conventional physiotherapy can lead to clinically meaningful improvement in patients with SCI caused by electrical trauma.
2. Case Reports
This study was approved by the Ethics Committee of Hangang Sacred Heart Hospital (HG2021-001). This study was registered at
ClinicalTrials.gov (identifier: NCT05883917). The patients provided written informed consent. The inclusion criteria were (1) age between 18 and 75 years old; (2) high-voltage electrical injury at more than 1000 volts; (3) motor incomplete spinal cord injury or upper motor neuron injuries with an NLI of T10 or higher; (4) severity (American Spinal Cord Injury Association Impairment Scale [ASIA]) of B or C or D; (5) no current issues with or history of other neurological conditions; and (6) involvement in standing program or ability to tolerate at least 30 min upright without signs or symptoms of orthostatic hypotension. The exclusion criteria were (1) ASIA A; (2) lower motor neuron injuries, as shown by absent reflexes during bilateral quadriceps and Achilles tendon taps; (3) previous history of spinal cord disease; (4) abnormal lesions in radiologic evaluations taken after development of extremity weakness; (5) orthostatic hypotension that makes training impossible during 30 min; (6) recent lower extremity fracture; (7) fixed contractures that make it impossible to apply the robot; and (8) skin lesions at the contact areas with the exoskeleton. We recruited 2 patients from the Department of Rehabilitation Medicine at Hangang Sacred Heart Hospital in Korea to participate in this study between January 2021 to December 2021.
2.1. Therapeutic Intervention
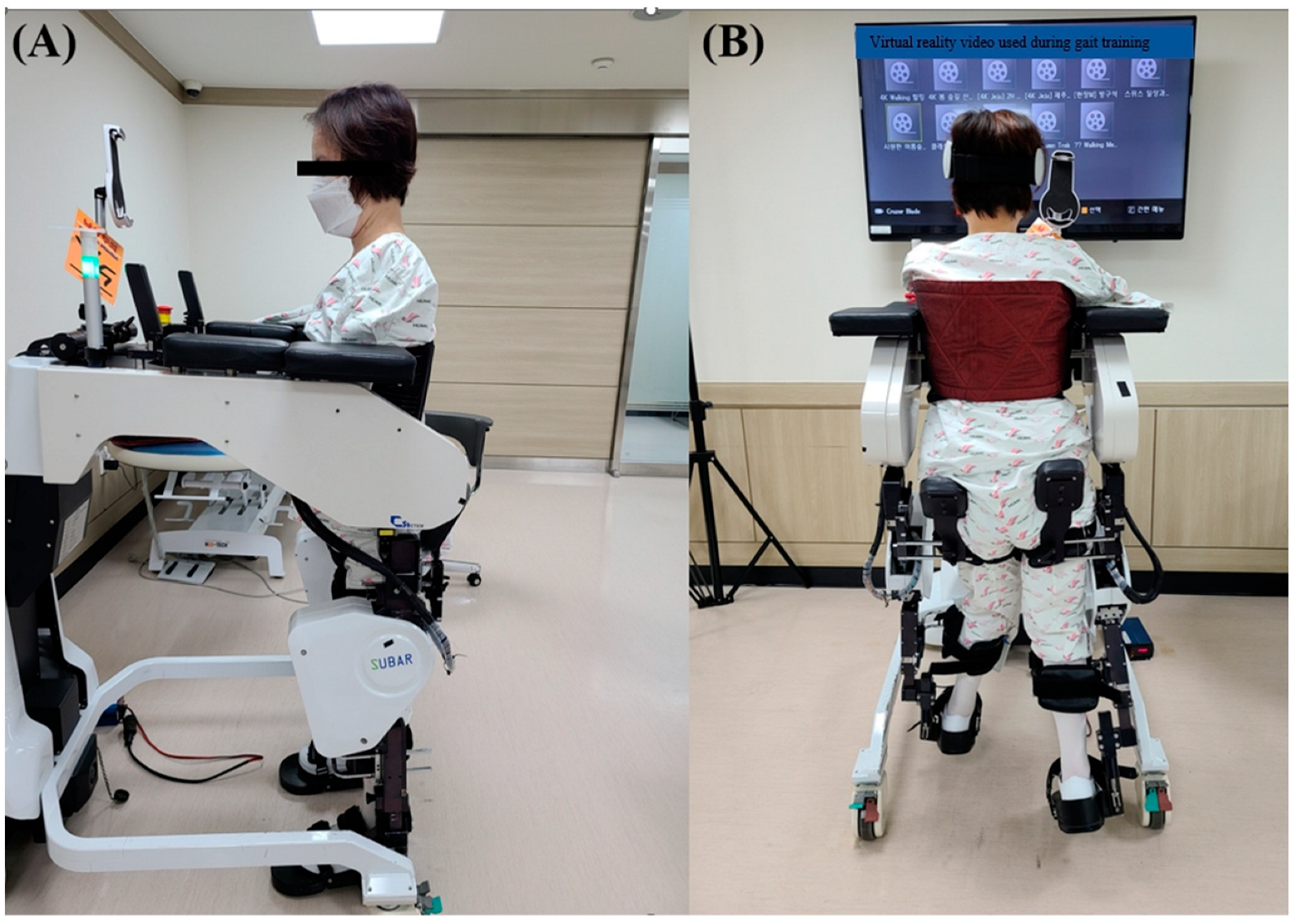
Before robot training, it was recommended to apply scar lubrication and wear a compression garment to prevent complications in the scar area. Gait training was conducted using SUBAR
® (Cretem, Anyang-si, Republic of Korea), which is a wearable robot with a footplate that assists in improving patient gait [
8,
14,
17,
18]. The SUBAR
® is an exoskeleton robot that can adjust step length, gait speed, and knee flexion angle. The SUBAR
® allows voluntary trunk muscles and reciprocal movements of the upper limbs when gait training and allows passive movements of the lower limb according to the adjusted parameters. The patient’s thigh length and lower leg length were measured before training so that the SUBAR
® could be adjusted to the patient’s size in order to ensure accurate training. One physiotherapist, who has experience in SUBAR
®, assisted the patients with wearing exoskeleton robot and setting the training intensity. Periodic movement of the lower extremities during training was simulated at a tolerable and comfortable gait speed, adjusted to the gait speed of each patient.
Conventional physiotherapy comprised 30 min of traditional gait training (extremity mobilization, strengthening and stretching exercises for the lower limbs, and gait re-education when participants can stand or walk). The total duration of each session was about 1 h 30 min, which included 10 min to put on the exoskeleton, 30 min of robot-assisted training using SUBAR®, 10 min to remove the exoskeleton, 10 min to observe whether complications occur in the scar area after RAGT, and 30 min of conventional physiotherapy, at a rate of 5 days a week for 12 weeks.
2.2. Outcome Measure
All measurements were assessed before training (0 week) and after training (12 weeks). Using the standards for Neurological Classification of Spinal Cord Injury (ISNCSCI) [
19], 28 dermatomes on the bilateral side of SCI patients were evaluated for sensory sensitivity to light touch and pin prick testing. The sensitivities were determined on the three-point scale of absent (0), impaired (1), or normal (2). Each ASIA sensory score for light tough and pin prick is a summation, falling within a 0–112 range of the scores for all 28 dermatomes. The manual muscles tests (MMTs) of ten key muscles were evaluated and graded on a six-point scale between 0 (complete paralysis) and 5 (normal active movements, full range of motion against full resistance). These scores were aggregated to generate an ASIA motor score within the 0–100 range. The ASIA lower extremity motor subscale score (LEMS; range 0–50) was used to evaluate the motor function. LEMS is the sum of bilateral lower extremity key muscle power, ranging from total paralysis (0) to normal active movement with a full range of motion against gravity and maximum resistance (5), with a total possible score of 50 [
20]. The passive range of motions (ROMs) of different joints (hip, knee, and ankle) were measured using a goniometer [
21]. The ambulatory motor index (AMI; range 0–30), which predicts ambulatory capability, was measured by evaluating muscles of hip flexion, hip abduction, hip extension, knee extension, and knee flexion on both sides [
22]. Functional ambulation categories (FAC) were evaluated based on a 6-point scale, ranging from unable to walk (0), dependency in gait (1 or 2), gait on even and level surfaces without manual contact with another person except for safety (3), and independent gait over 15 m irrespective of aids used (4 or 5). Walking distances of 6 min (6 MWT) were in accordance with the standardized guidelines, and the walking course was 20 m. The patients were instructed to walk as far as possible in 6 min [
23].
2.3. Case Presentation
2.3.1. Patient 1
The first patient (male, 48 years old) was admitted to the hospital after suffering an electrical trauma (22,900 V) without loss of consciousness. On admission, the patient was alert and oriented. No neurological deficits were present. A 28% burn of the total body surface area (TBSA) was identified on the frank, bilateral thighs, and bilateral legs. After 14 days of hospitalization, signs of SCI, such as exacerbated knee reflex, Babinski’s sign, abnormal sensation, and loss of leg strength, were observed. Owing to a developing lower extremity weakness, contrast-enhanced CT and MRI using T1- and T2-weighted sequences of the spine were performed, the results of which were normal. The patient had difficulty walking because of weakness in the lower extremities and complained of paresthesia. A split-thickness skin graft (STSG) was performed on the left flank and both thighs a month after the injury. One week after the STSG, balance training and lower extremity muscle strengthening exercises were started in bed by a physical therapist. After the completion of epithelialization of the burn scar, the patient was admitted to the Department of Rehabilitation Medicine. He started a RAGT on the 56th day of the injury for lower extremity weakness and gait dysfunction. Before training, the patient’s physical condition showed a neurological level of injury (NLI) of T 10, an ASIA impairment scale grade C (
Table 1), an LEMS of 22 points, and an AMI of 12 points, and he was able to sit independently.
However, he was unable to stand or walk independently. In an MMT, the flexor (right/left), extensor (right/left), abductor (right/left), and adductor (right/left) of the hip joint improved from 2/2, 2/2, 2/2, and 1/1 before training to 3/3, 2/2, 3/3, and 2/2 after training. No differences were observed in knee flexor (right/left) and knee extensor (right/left), with scores of 2/2 and 3/3 before training and 2/2 and 3/3 after training. The ankle dorsiflexor (right/left) and ankle plantarflexor (right/left) improved from 2/2 and 2/2 before training to 3/3 and 3/3 after training. The long toe extensor (right/left) improved from 2/2 before training to 3/3 after training (
Table 2). In passive ROM evaluation, hip flexion (right/left) ROMs improved from 60°/60° before training to 100°/100° after training. And there were no differences in the hip extension (right/left) ROMs, moving from 5°/5° before training to 5°/5° after training. The knee flexion (right/left) ROMs improved from 100°/105° before training to 105°/105° after training. There was no difference in the knee extension (right/left) ROMs, moving from 0°/0° before training to 0°/0° after training. The ankle dorsiflexion (right/left) ROMs improved from 5°/5° before training to 10°/10° after training. There was no difference in the ankle plantarflexion (right/left) ROMs, moving from 40°/40° before training to 40°/40° after training (
Table 2).
Patient 1, who was unable to walk before training, was able to walk indoors after 12 weeks training. After 12 weeks of RAGT, he could walk 92.16 m in the 6 MWT. LEMS improved from 22 before training to 30 after training, and AMI scores improved from 12 before training to 16 after training (
Table 3).
2.3.2. Patient 2
The second patient (female, 45 years old) was admitted to the hospital after an electrical trauma (22,900 V). A 29% burn of TBSA was identified on the abdomen, right inguinal, bilateral arms, bilateral forearms, and bilateral hands. On the day of hospitalization, escharectomy and fasciotomy were performed on the upper extremity scars, and 12 days after injury, bilateral transhumeral amputation was performed owing to the inflammatory reaction and decay of the upper limb scars on both sides. Motor weakness and paresthesia of both lower extremities occurred 5 weeks after the injury. She was referred to the Department of Rehabilitation Medicine. Signs of SCI appeared, such as bilaterally exacerbated knee reflexes, bilateral Babinski’s sign, and decreased sensation. Contrast-enhanced CT and MRI using T1- and T2-weighted sequences of the spine at this time revealed normal results. After the epithelialization of the burn scar was completed, she was admitted to the Department of Rehabilitation Medicine. She could not sit independently due to muscle weakness in her trunk; therefore, sitting training, and trunk strengthening exercises were performed when she was first admitted. Notably, 110 days after the injury, the trunk muscles became strong enough to allow her to sit independently for 5 min, and RAGT was started. RAGT was performed for 30 min using a trunk support harness because of trunk muscle weakness (
Figure 1).
The patient’s physical condition showed an NLI C4, ASIA impairment scale grade C (
Table 1), LEMS of 10 points, and AMI of 10 points. Independent sitting was possible for 5 min; however, independent standing and walking were impossible before training (
Table 3). In an MMT, the flexor (right/left), extensor (right/left), abductor (right/left), and adductor (right/left) of the hip joint improved from 1/1, 1/1, 1/1, and 1/1 before training to 2/2, 2/2, 2/2, and 2/2 after training. The knee flexor (right/left) and knee extensor (right/left) improved from 1/1 and 1/1 before training to 2/2 and 2/2 after training. The ankle dorsiflexor (right/left) and ankle plantarflexor (right/left) improved from 1/1 and 1/1 before training to 3/3 and 3/3 after training. The long toe extensor (right/left) improved from 1/1 before training to 3/3 after training (
Table 2). In passive ROM evaluation, hip flexion (right/left) ROMs improved from 90°/90° before training to 95°/95° after training. And there were no differences in the hip extension (right/left) ROMs from 5°/5° before training to 5°/5° after training. The knee flexion (right/left) ROMs improved from 120°/120° before training to 130°/130° after training. There was no difference in the knee extension (right/left) ROMs from 0°/0° before training to 0°/0° after training. The ankle plantarflexion (right/left) ROMs improved from 35°/35° before training to 45°/45° after training. There was no difference in the ankle dorsiflexion (right/left) ROMs, with 10°/10° before training and 10°/10° after training (
Table 2). She could not walk independently. LEMS improved from 10 before training to 26 after training. AMI scores were the same at 10 points before and after training (
Table 3).
The patients could physically tolerate the RAGT, all sessions were completed, and no adverse events occurred.
3. Discussion
After 12 weeks of RAGT and conventional physiotherapy in patients with delayed SCI due to high-voltage electrical burns, the first patient’s lower limb strength and joint ROMs improved, and the walking function recovered to the point where indoor walking was possible. In the second patient, walking function was not recovered, but lower limb strength and ROMs were confirmed to be improved.
Joint contractures and movement restrictions in the lower extremities interfere with normal walking and act as factors that decrease gait speed and reduce the step length [
14]. We used 6 MWT to quantitatively evaluate gait ability in patients with incomplete SCI [
23]. LEMS is the most important factor in predicting gait ability with incomplete SCI. A previous study indicated that the prospects for gait improvement are poor if LEMS is less than 20, but that the prognosis is good if LEMS is more than 30 [
24]. Efforts are made to improve these parameters that affect gait function [
25].
The clinical effect of applying robot therapy to burn patients is described as the influence of task-specific training on walking performance or hand function [
8,
14]. It was confirmed that joint ROM, muscle strength, and gait speed improved when robot training was applied to patients with decreased lower extremity function due to thermal trauma [
8,
14]. The reduced arthrogenic muscle inhibition during robot treatment for patients is also considered a mechanism for improving performance. Sensory deficits, muscle weakness, abnormal muscle activities, proprioception impairments, and soft tissue tightness in patients with SCI can impair walking ability [
26,
27]. RAGT can increase the repetition of training while maintaining a physiological gait pattern [
28]. The mechanism underlying gait function restoration after SCI involves enhancing the sensory and proprioception input to the spinal cord [
29] and activating the central gait pattern generator [
22]. Plastic changes can be induced at the spinal cord level and in the sensory–motor cortex. This means that robot training changes the gait center of the spine and supraspinal area [
10]. RAGT in the acute phase improves muscle strength and gait speed through muscle activation patterns and gait pattern relearning [
30]. Improvement in cardiopulmonary capacity via robot training improves gait speed and endurance. Trunk control during robot training is an important factor that affects gait [
9]. One case report demonstrated how robot gait training engages trunk muscles and can elicit training effects on balance control in patients with SCI [
31]. RAGT is a promising technique for restoring functional walking and improving the gait ability of SCI patients [
9,
28].
This study was performed on the results of RAGT and conventional physiotherapy in only two patients with delayed SCI due to electrical trauma. Although the results were confirmed, there were limitations in that the clinical effect could not be confirmed when applied to all patients with SCI caused by electrical trauma. In addition, the improvement in the patient’s lower extremity function could not be entirely explained by robot training as RAGT and conventional physiotherapy were performed simultaneously. Further research should seek to confirm that improvement in gait parameters after robot training exceeds that achieved after conventional training to validate the effectiveness of RAGT. Studies employing multiple patients and control groups are necessary to demonstrate the effectiveness and treatment mechanisms of RAGT in patients with SCI after an electrical burn.
4. Conclusions
This study is the first to report the feasibility, safety, and efficacy of RAGT for patients with SCI after electrical burns. The robot training was easily performed in patients with SCI caused by electrical burns without any undesirable side effects. The results suggested the possibility of achieving clinical effects in terms of improving lower extremity muscle strength, joint ROMs, and gait performance in patients with SCI caused by electrical trauma.
Author Contributions
S.-Y.J. contributed as corresponding authors of this work. S.-Y.L. and C.-H.S. performed data analysis and interpreted the results. Y.-S.C. revised the article critically for important intellectual content. All authors have read and agreed to the published version of the manuscript.
Funding
This research was supported by the Basic Science Research Program of the National Research Foundation of Korea (2021R1I1A3051338), and the Soonchunhyang University Research Fund.
Institutional Review Board Statement
The study was conducted in accordance with the guidelines of the Declaration of Helsinki and was approved by the Ethics Committee of Hangang Sacred Heart Hospital (approval no.: HG2021-001). This study was registered at
ClinicalTrials.gov (identifier: NCT05883917). The patients provided written informed consent.
Informed Consent Statement
The patients provided written informed consent.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Levine, N.S.; Atkins, A.; McKeel, D.W., Jr.; Peck, S.D.; Pruitt, B.A., Jr. Spinal cord injury following electrical accidents: Case reports. J. Trauma 1975, 15, 459–463. [Google Scholar] [CrossRef]
- Arévalo, J.M.; Lorente, J.A.; Balseiro-Gómez, J. Spinal cord injury after electrical trauma treated in a burn unit. Burns 1999, 25, 449–452. [Google Scholar] [CrossRef]
- Hunt, J.L.; Mason, A.D., Jr.; Masterson, T.S.; Pruitt, B.A., Jr. The pathophysiology of acute electric injuries. J. Trauma 1976, 16, 335–340. [Google Scholar] [CrossRef]
- Ohn, S.H.; Kim, D.Y.; Shin, J.C.; Kim, S.M.; Yoo, W.K.; Lee, S.K.; Park, C.H.; Jung, K.I.; Jang, K.U.; Seo, C.H.; et al. Analysis of high-voltage electrical spinal cord injury using diffusion tensor imaging. J. Neurol. 2013, 260, 2876–2883. [Google Scholar] [CrossRef]
- Ko, S.H.; Chun, W.; Kim, H.C. Delayed spinal cord injury following electrical burns: A 7-year experience. Burns 2004, 30, 691–695. [Google Scholar] [CrossRef]
- Davidson, G.S.; Deck, J.H. Delayed myelopathy following lightning strike: A demyelinating process. Acta Neuropathol. 1988, 77, 104–108. [Google Scholar] [CrossRef]
- Dietz, V.; Colombo, G.; Jensen, L.; Baumgartner, L. Locomotor capacity of spinal cord in paraplegic patients. Ann. Neurol. 1995, 37, 574–582. [Google Scholar] [CrossRef]
- Joo, S.Y.; Lee, S.Y.; Cho, Y.S.; Lee, K.J.; Kim, S.H.; Seo, C.H. Effectiveness of robot-assisted gait training on patients with burns: A preliminary study. Comput. Methods Biomech. Biomed. Eng. 2020, 23, 888–893. [Google Scholar] [CrossRef]
- Hwang, S.; Kim, H.R.; Han, Z.A.; Lee, B.S.; Kim, S.; Shin, H.; Moon, J.G.; Yang, S.P.; Lim, M.H.; Cho, D.Y.; et al. Improved Gait Speed After Robot-Assisted Gait Training in Patients with Motor Incomplete Spinal Cord Injury: A Preliminary Study. Ann. Rehabil. Med. 2017, 41, 34–41. [Google Scholar] [CrossRef]
- Cheung, E.Y.Y.; Ng, T.K.W.; Yu, K.K.K.; Kwan, R.L.C.; Cheing, G.L.Y. Robot-Assisted Training for People with Spinal Cord Injury: A Meta-Analysis. Arch. Phys. Med. Rehabil. 2017, 98, 2320–2331.e2312. [Google Scholar] [CrossRef]
- de Miguel-Fernández, J.; Lobo-Prat, J.; Prinsen, E.; Font-Llagunes, J.M.; Marchal-Crespo, L. Control strategies used in lower limb exoskeletons for gait rehabilitation after brain injury: A systematic review and analysis of clinical effectiveness. J. Neuroeng. Rehabil. 2023, 20, 23. [Google Scholar] [CrossRef]
- Warutkar, V.; Dadgal, R.; Mangulkar, U.R. Use of Robotics in Gait Rehabilitation Following Stroke: A Review. Cureus 2022, 14, e31075. [Google Scholar] [CrossRef]
- Calafiore, D.; Negrini, F.; Tottoli, N.; Ferraro, F.; Ozyemisci-Taskiran, O.; de Sire, A. Efficacy of robotic exoskeleton for gait rehabilitation in patients with subacute stroke: A systematic review. Eur. J. Phys. Rehabil. Med. 2022, 58, 1–8. [Google Scholar] [CrossRef]
- Joo, S.Y.; Lee, S.Y.; Cho, Y.S.; Lee, K.J.; Seo, C.H. Effects of Robot-Assisted Gait Training in Patients with Burn Injury on Lower Extremity: A Single-Blind, Randomized Controlled Trial. J. Clin. Med. 2020, 9, 2813. [Google Scholar] [CrossRef]
- Samhan, A.F.; Abdelhalim, N.M.; Elnaggar, R.K. Effects of interactive robot-enhanced hand rehabilitation in treatment of paediatric hand-burns: A randomized, controlled trial with 3-months follow-up. Burns 2020, 46, 1347–1355. [Google Scholar] [CrossRef]
- Yoshioka, T.; Kubota, S.; Sugaya, H.; Hyodo, K.; Ogawa, K.; Taniguchi, Y.; Kanamori, A.; Sankai, Y.; Yamazaki, M. Robotic device-assisted knee extension training during the early postoperative period after opening wedge high tibial osteotomy: A case report. J. Med. Case Rep. 2017, 11, 213. [Google Scholar] [CrossRef]
- Cho, Y.S.; Joo, S.Y.; Seo, C.H. Effect of robot-assisted gait training on the biomechanical properties of burn scars: A single-blind, randomized controlled trial. Burns Trauma 2022, 10, tkac026. [Google Scholar] [CrossRef]
- Lee, S.Y.; Cha, J.Y.; Yoo, J.W.; Nazareno, M.; Cho, Y.S.; Joo, S.Y.; Seo, C.H. Effect of the Application of Virtual Reality on Pain Reduction and Cerebral Blood Flow in Robot-Assisted Gait Training in Burn Patients. J. Clin. Med. 2022, 11, 3762. [Google Scholar] [CrossRef]
- Snider, B.A.; Eren, F.; Reeves, R.K.; Rupp, R.; Kirshblum, S.C. The International Standards for Neurological Classification of Spinal Cord Injury: Classification Accuracy and Challenges. Top Spinal Cord. Inj. Rehabil. 2023, 29, 1–15. [Google Scholar] [CrossRef]
- Kirshblum, S.; Snider, B.; Rupp, R.; Read, M.S. Updates of the International Standards for Neurologic Classification of Spinal Cord Injury: 2015 and 2019. Phys. Med. Rehabil. Clin. N. Am. 2020, 31, 319–330. [Google Scholar] [CrossRef]
- Maggioni, S.; Melendez-Calderon, A.; van Asseldonk, E.; Klamroth-Marganska, V.; Lünenburger, L.; Riener, R.; van der Kooij, H. Robot-aided assessment of lower extremity functions: A review. J. Neuroeng. Rehabil. 2016, 13, 72. [Google Scholar] [CrossRef]
- Shin, J.C.; Kim, J.Y.; Park, H.K.; Kim, N.Y. Effect of robotic-assisted gait training in patients with incomplete spinal cord injury. Ann. Rehabil. Med. 2014, 38, 719–725. [Google Scholar] [CrossRef]
- Van Hedel, H.J.; Wirz, M.; Dietz, V. Assessing walking ability in subjects with spinal cord injury: Validity and reliability of 3 walking tests. Arch. Phys. Med. Rehabil. 2005, 86, 190–196. [Google Scholar] [CrossRef]
- Waters, R.L.; Adkins, R.; Yakura, J.; Vigil, D. Prediction of ambulatory performance based on motor scores derived from standards of the American Spinal Injury Association. Arch. Phys. Med. Rehabil. 1994, 75, 756–760. [Google Scholar] [CrossRef]
- Tarnacka, B.; Korczyński, B.; Frasuńska, J. Impact of Robotic-Assisted Gait Training in Subacute Spinal Cord Injury Patients on Outcome Measure. Diagnostics 2023, 13, 1966. [Google Scholar] [CrossRef]
- Lin, P.Y.; Yang, Y.R.; Cheng, S.J.; Wang, R.Y. The relation between ankle impairments and gait velocity and symmetry in people with stroke. Arch. Phys. Med. Rehabil. 2006, 87, 562–568. [Google Scholar] [CrossRef]
- Soma, Y.; Kubota, S.; Kadone, H.; Shimizu, Y.; Hada, Y.; Koda, M.; Sankai, Y.; Yamazaki, M. Postoperative Acute-Phase Gait Training Using Hybrid Assistive Limb Improves Gait Ataxia in a Patient with Intradural Spinal Cord Compression Due to Spinal Tumors. Medicina 2022, 58, 1825. [Google Scholar] [CrossRef]
- Nam, K.Y.; Kim, H.J.; Kwon, B.S.; Park, J.W.; Lee, H.J.; Yoo, A. Robot-assisted gait training (Lokomat) improves walking function and activity in people with spinal cord injury: A systematic review. J. Neuroeng. Rehabil. 2017, 14, 24. [Google Scholar] [CrossRef]
- Lam, T.; Pauhl, K.; Ferguson, A.; Malik, R.N.; Krassioukov, A.; Eng, J.J. Training with robot-applied resistance in people with motor-incomplete spinal cord injury: Pilot study. J. Rehabil. Res. Dev. 2015, 52, 113–129. [Google Scholar] [CrossRef]
- Ziegler, M.D.; Zhong, H.; Roy, R.R.; Edgerton, V.R. Why variability facilitates spinal learning. J. Neurosci. 2010, 30, 10720–10726. [Google Scholar] [CrossRef]
- Chisholm, A.E.; Alamro, R.A.; Williams, A.M.; Lam, T. Overground vs. treadmill-based robotic gait training to improve seated balance in people with motor-complete spinal cord injury: A case report. J. Neuroeng. Rehabil. 2017, 14, 27. [Google Scholar] [CrossRef]
| Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).