Vertical Dentofacial Skeletal Divergency Is Not Linked with Oral Health-Related Quality of Life
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
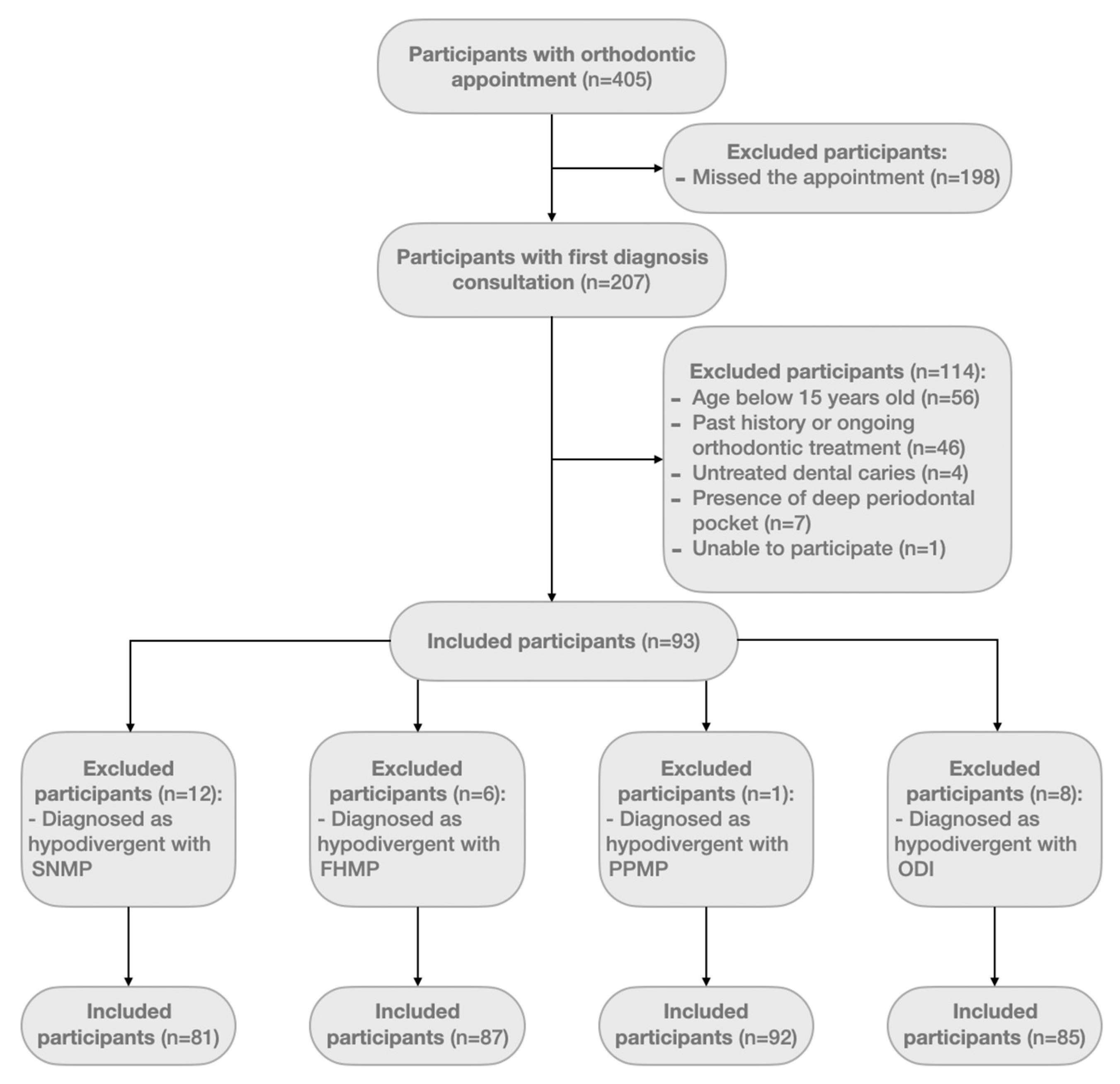
2.2. Participants and Eligibility Criteria
2.3. Sociodemographic and Clinical Orthodontic Questionnaire
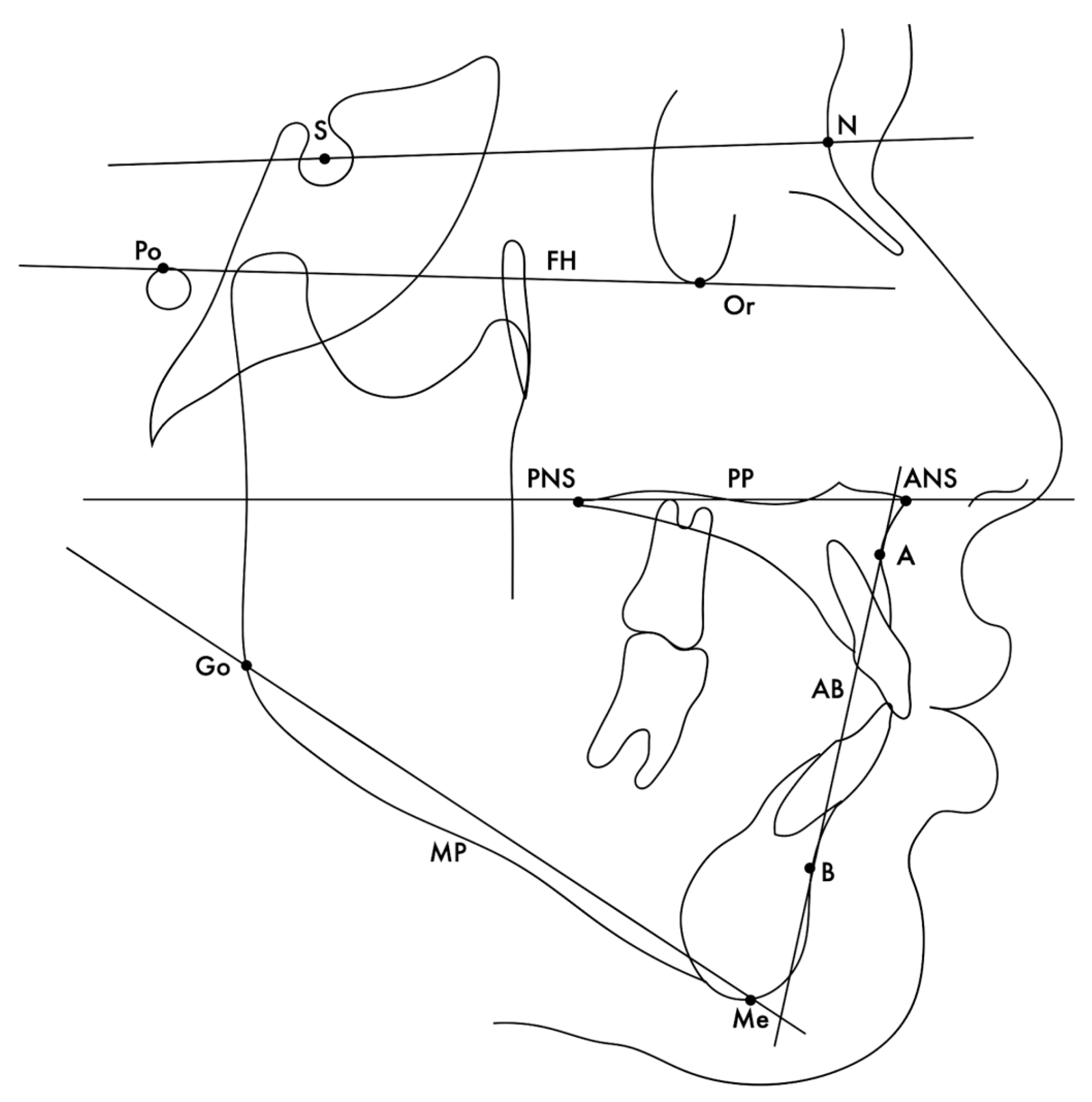
2.4. Measurements on Cephalograms
2.5. Measurement Reliability and Reproducibility
2.6. Statistical Analysis
3. Results
4. Discussion
Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sun, L.; Wong, H.M.; McGrath, C.P. Relationship between the severity of malocclusion and oral health related quality of life: A systematic review and meta-analysis. Oral Health Prev. Dent. 2017, 16, 503. [Google Scholar]
- Bock, J.J.; Odemar, F.; Fuhrmann, R.A.W. Assessment of quality of life in patients undergoing orthognathic surgery. J. Orofac. Orthop. 2009, 70, 407–419. [Google Scholar] [CrossRef] [PubMed]
- Göelzer, J.G.; Becker, O.E.; Junior, O.L.H.; Scolari, N.; Melo, M.F.S.; Heitz, C.; de Oliveira, R.B. Assessing change in quality of life using the Oral Health Impact Profile (OHIP) in patients with different dentofacial deformities undergoing orthognathic surgery: A before and after comparison. Int. J. Oral Maxillofac. Surg. 2014, 43, 1353–1359. [Google Scholar] [CrossRef] [PubMed]
- Rustemeyer, J.; Martin, A.; Gregersen, J. Changes in quality of life and their relation to cephalometric changes in orthognathic surgery patients. Angle Orthod. 2012, 82, 235–241. [Google Scholar] [CrossRef] [PubMed]
- Slade, G.D.; Spencer, A.J. Development and evaluation of the Oral Health Impact Profile. Community Dent. Health 1994, 11, 3–11. [Google Scholar] [PubMed]
- Slade, G.D. Derivation and validation of a short-form oral health impact profile. Community Dent. Oral Epidemiol. 1997, 25, 284–290. [Google Scholar] [CrossRef] [PubMed]
- Locker, D.; Allen, F. What do measures of “oral health-related quality of life” measure? Community Dent. Oral Epidemiol. 2007, 35, 401–411. [Google Scholar] [CrossRef]
- Riva, F.; Seoane, M.; Reichenheim, M.E.; Tsakos, G.; Celeste, R.K. Adult oral health-related quality of life instruments: A systematic review. Community Dent. Oral Epidemiol. 2022, 50, 333–338. [Google Scholar] [CrossRef]
- Leite, P.C.C.; Camarini, E.T.; Filho, L.I.; Pavan, Â.J.; Farah, G.J.; da Silva, M.B. Estudo epidemiológico das deformidades dentofaciais de Maringá/PR-1997/2003. Pesqui. Bras. Odontopediatria Clín. Integr. 2004, 4, 217–220. [Google Scholar]
- Ong, M.A.H. Spectrum of dentofacial deformities: A retrospective survey. Ann. Acad. Med. Singap. 2004, 33, 239–242. [Google Scholar]
- Alanko, O.M.E.; Svedstrm-Oristo, A.L.; Tuomisto, M.T. Patients’ perceptions of ortho gnathic treatment, well-being, and psychological or psychiatric status: A systematic review. Acta Odontol. Scand. 2010, 68, 249–260. [Google Scholar] [CrossRef] [PubMed]
- Eslamipour, F.; Najimi, A.; Tadayonfard, A.; Azamian, Z. Impact of Orthognathic Surgery on Quality of Life in Patients with Dentofacial Deformities. Int. J. Dent. 2017, 2017, 4103905. [Google Scholar] [CrossRef] [PubMed]
- Gomes, A.M.P.; Garbin, C.A.S.; Ferraz, F.W.S.; Saliba, T.A.; Garbin, A.J.I. Dentofacial Deformities and Implications on Quality of Life: A Presurgical Multifactorial Analysis in Patients Seeking Orthognathic Surgical Treatment. J. Oral Maxillofac. Surg. 2019, 77, 409.e1–409.e9. [Google Scholar]
- Frejman, M.W.; Vargas, I.A.; Rösing, C.K.; Closs, L.Q. Dentofacial deformities are associated with lower degrees of self-esteem and higher impact on oral health-related quality of life: Results from an observational study involving adults. J. Oral Maxillofac. Surg. 2013, 71, 763–767. [Google Scholar] [CrossRef] [PubMed]
- Feragen, K.B.; Stock, N.M. Psychological adjustment to craniofacial conditions (excluding oral clefts): A review of the literature. Psychol. Health 2017, 32, 253–288. [Google Scholar] [CrossRef] [PubMed]
- Alanko, O.M.E.; Svedström-Oristo, A.L.; Peltomäki, T.; Kauko, T.; Tuomisto, M.T. Psychosocial well-being of prospective orthognathic-surgical patients. Acta Odontol. Scand. 2014, 72, 887–897. [Google Scholar] [CrossRef] [PubMed]
- Rusanen, J.; Lahti, S.; Tolvanen, M.; Pirttiniemi, P. Quality of life in patients with severe malocclusion before treatment. Eur. J. Orthod. 2010, 32, 43–48. [Google Scholar] [CrossRef]
- Schendel, S.A.; Eisenfeld, J.; Bell, W.H.; Epker, B.N.; Mishelevich, D.J. The long face syndrome: Vertical maxillary excess. Am. J. Orthod. 1976, 70, 398–408. [Google Scholar] [CrossRef]
- Bell, W.H.; Creekmore, T.D.; Alexander, R.G. Surgical correction of the long face syndrome. Am. J. Orthod. 1977, 71, 40–67. [Google Scholar] [CrossRef]
- Ali, U.S.; Sukhia, R.H.; Fida, M.; Kamal, A.T.; Abbas, A. Influence of incisor inclination and anterior vertical facial height on facial attractiveness in an adult Asian male. Am. J. Orthod. Dentofac. Orthop. 2022, 161, 381–389. [Google Scholar] [CrossRef]
- Arqoub, S.H.A.; Al-Khateeb, S.N. Perception of facial profile attractiveness of different antero-posterior and vertical proportions. Eur. J. Orthod. 2011, 33, 103–111. [Google Scholar] [CrossRef] [PubMed]
- Morgan, L.K.; Kisley, M.A. The effects of facial attractiveness and perceiver’s mate value on adaptive allocation of central processing resources. Evol. Hum. Behav. 2014, 35, 96–102. [Google Scholar] [CrossRef]
- Lee, S.; McGrath, C.; Samman, N. Quality of life in patients with dentofacial deformity: A comparison of measurement approaches. Int. J. Oral Maxillofac. Surg. 2007, 36, 488–492. [Google Scholar] [CrossRef] [PubMed]
- Elm, E.V.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. PLoS Med. 2007, 4, 1623–1627. [Google Scholar] [CrossRef] [PubMed]
- Pereira, D.; Machado, V.; Botelho, J.; Proença, L.; Rua, J.; Lemos, C.; Mendes, J.J.; Delgado, A.S. Impact of malocclusion, tooth loss and oral hygiene habits on quality of life in orthodontic patients: A cross-sectional study. Int. J. Environ. Res. Public. Health 2021, 18, 7145. [Google Scholar] [CrossRef]
- Andiappan, M.; Gao, W.; Bernabé, E.; Kandala, N.B.; Donaldson, A.N. Malocclusion, orthodontic treatment, and the Oral Health Impact Profile (OHIP-14): Systematic review and meta-analysis. Angle Orthod. 2015, 85, 493–500. [Google Scholar] [CrossRef]
- Afonso, A.; Silva, R.M.I.; Frias-Bulhosa, J. Qualidade de Vida Relacionada Com a Saude Oral: Validaçao Portuguesa de OHIP-14. Soc. Port. Psicol. Saúde 2017, 18, 374–388. [Google Scholar] [CrossRef]
- Riedel, R. The relation of maxillary structures to cranium in malocclusion and in normal occlusion. Angle Orthod. 1952, 22, 142–145. [Google Scholar]
- Sato, S. Alterations of Occlusal Plane due to Posterior Discrepancy related to development of malocclusion—Introduction to denture frame analysis. Bull. Kanagawa Dent. Col. 1987, 15, 115–123. [Google Scholar]
- Bjork, A. The Relationship of the Jaws to the Cranium; Introduction to Orthodontics; Lundstrom, A., Ed.; McGraw-Hill: New York, NY, USA, 1960. [Google Scholar]
- Kim, Y.H. Overbite depth indicator with particular reference to anterior open-bite. Am. J. Orthod. 1974, 65, 586–611. [Google Scholar] [CrossRef]
- Antoun, J.S.; Thomson, W.M.; Merriman, T.R.; Rongo, R.; Farella, M. Impact of skeletal divergence on oral health-related quality of life and self-reported jaw function. Korean J. Orthod. 2017, 47, 186–194. [Google Scholar] [CrossRef] [PubMed]
- Meger, M.N.; Fatturi, A.L.; Gerber, J.T.; Weiss, S.G.; Rocha, J.S.; Scariot, R.; Wambier, L.M. Impact of orthognathic surgery on quality of life of patients with dentofacial deformity: A systematic review and meta-analysis. Br. J. Oral Maxillofac. Surg. 2021, 59, 265–271. [Google Scholar] [CrossRef] [PubMed]
- de Araujo, C.M.; Schroder, A.G.D.; de Araujo, B.M.M.; Calvacante-Leão, B.L.; Stechman-Neto, J.; Zeigelboim, B.S.; Santos, R.S.; Guariza-Filho, O. Impact of orthodontic-surgical treatment on quality of life: A meta-analysis. Eur. J. Orthod. 2020, 42, 281–289. [Google Scholar] [CrossRef]
- Tuk, J.G.; Lindeboom, J.A.; Tan, M.L.; de Lange, J. Impact of orthognathic surgery on quality of life in patients with different dentofacial deformities: Longitudinal study of the Oral Health Impact Profile (OHIP-14) with at least 1 year of follow-up. Oral Maxillofac. Surg. 2022, 26, 281–289. [Google Scholar] [CrossRef] [PubMed]
- Ryan, F.S.; Barnard, M.; Cunningham, S.J. Impact of dentofacial deformity and motivation for treatment: A qualitative study. Am. J. Orthod. Dentofac. Orthop. 2012, 141, 734–742. [Google Scholar] [CrossRef] [PubMed]
- de Oliveira, E.G.S.; Pinzan-Vercelino, C.R.M. Comparative evaluation of cephalometric and occlusal characteristics between the Long Face pattern and Pattern I. Dent. Press J. Orthod. 2013, 18, 86–93. [Google Scholar] [CrossRef]
- Curto, A.; Albaladejo, A.; Alvarado-Lorenzo, A. Oral-Health-Related Quality of Life (OHRQoL) and Anterior Open Bite in Adult Patients: A Case-Control Study. Healthcare 2022, 10, 129. [Google Scholar] [CrossRef]
- Plaza, S.P.; Reimpell, A.; Silva, J.; Montoya, D. Relationship between skeletal class II and class III malocclusions with vertical skeletal pattern. Dent. Press J. Orthod. 2019, 24, 63–72. [Google Scholar] [CrossRef]
- Cochrane, S.M.; Cunningham, S.J.; Hunt, N.P. A comparison of the perception of facial profile by the general public and 3 groups of clinicians. Int. J. Adult Orthodon. Orthognath. Surg. 1999, 14, 291–295. [Google Scholar]
- Johnston, D.J.; Hunt, O.; Johnston, C.D.; Burden, D.J.; Stevenson, M.; Hepper, P. The influence of lower face vertical proportion on facial attractiveness. Eur. J. Orthod. 2005, 27, 349–354. [Google Scholar] [CrossRef]
- Pabari, S.; Moles, D.R.; Cunningham, S.J. Assessment of motivation and psychological characteristics of adult orthodontic patients. Am. J. Orthod. Dentofac. Orthop. 2011, 140, 263–272. [Google Scholar] [CrossRef] [PubMed]
- Goulart, M.S.; Filho, L.C.; Conti, A.C.C.F.; Pedrin, R.R.A.; Ladewig, V.M.; Cardoso, M.A. Evaluation of facial esthetics in long-faced white Brazilian middle school students. Am. J. Orthod. Dentofac. Orthop. 2019, 155, 812–818. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, M.; Shaikh, A.; Fida, M. Diagnostic performance of various cephalometric parameters for the assessment of vertical growth pattern. Dent. Press J. Orthod. 2016, 21, 41–49. [Google Scholar] [CrossRef] [PubMed]
- Esperão, P.T.G.; de Oliveira, B.H.; Almeida, M.A.O.; Kiyak, H.A.; Miguele, J.A.M. Oral health-related quality of life in orthognathic surgery patients. Am. J. Orthod. Dentofac. Orthop. 2010, 137, 790–795. [Google Scholar] [CrossRef]
- Cohen, L.K.; Jago, J.D. Toward the formulation of sociodental indicators. Int. J. Health Serv. 1976, 6, 681–698. [Google Scholar] [CrossRef]
| Variable | SN-MP | Total (n = 81) | FH-MP | Total (n = 87) | PP-MP | Total (n = 92) | ODI | Total (n = 85) | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Hyper (n = 27) | Normo (n = 54) | Hyper (n = 45) | Normo (n = 42) | Hyper (n = 39) | Normo (n = 53) | Hyper (n = 28) | Normo (n = 57) | |||||
| Female, n (%) | 21 (77.8) | 31 (57.4) | 52 (64.2) | 27 (60.0) | 30 (71.4) | 57 (65.5) | 25 (64.1) | 34 (64.2) | 59 (64.1) | 15 (53.6) | 41 (71.9) | 56 (65.9) |
| Male, n (%) | 6 (22.2) | 23 (42.6) | 29 (35.8) | 18 (40.0) | 12 (28.6) | 30 (34.5) | 14 (35.9) | 19 (35.8) | 33 (35.9) | 13 (46.4) | 16 (28.1) | 29 (34.1) |
| Age, mean (SD) | 30.7 (14.2) | 30.0 (15.2) | 30.3 (14.9) | 30.1 (14.4) | 29.1 (13.3) | 30.1 (14.4) | 30.4 (15.2) | 29.8 (13.8) | 30.1(14.3) | 29.5 (16.4) | 30.1(13.4) | 29.9 (14.4) |
| OHIP-14, Mean (SD) | SN-MP | SN-MP | p-Value * | Total (n = 81) | Adjusted Model for Sex and Age [SE] (p-Value) |
|---|---|---|---|---|---|
| Hyperdivergent (n = 27) | Normodivergent (n = 54) | ||||
| Total | 15 (11.0) | 13.2 (11.3) | 0.4046 | 13.8 (11.2) | −0.15 [0.06] (0.010) |
| Domains | |||||
| Functional limitation | 0.7 (1.1) | 0.5 (1.0) | 0.5783 | 0.6 (1.0) | 0.04 [0.21] (0.851) |
| Physical pain | 1.6 (1.3) | 1.4 (1.3) | 0.8716 | 1.4 (1.3) | −0.01 [0.13] (0.966) |
| Psychological discomfort | 1.9 (1.5) | 1.7 (1.5) | 0.2634 | 1.8 (1.5) | −0.30 [0.12] (0.010) |
| Physical disability | 0.8 (1.1) | 0.7 (1.1) | 0.7395 | 0.8 (1.1) | 0.02 [0.17] (0.930) |
| Psychological disability | 1.5 (1.3) | 1.3 (1.4) | 0.7308 | 1.4 (1.4) | −0.24 [0.13] (0.079) |
| Social disability | 0.5 (1.0) | 0.5 (0.9) | 0.2452 | 0.5 (1.0) | −0.31 [0.23] (0.165) |
| Handicap | 0.6 (1.0) | 0.6 (1.0) | 0.5520 | 0.6 (1.0) | 0.06 [0.20] (0.752) |
| OHIP-14, Mean (SD) | FH-MP | FH-MP | p-Value * | Total (n = 87) | Adjusted Model for Sex and Age [SE] (p-Value) |
|---|---|---|---|---|---|
| Hyperdivergent (n = 45) | Normodivergent (n = 42) | ||||
| Total | 14.8 (11.1) | 13.0 (11.2) | 0.4458 | 13.9 (11.2) | 0.04 [0.06] (0.562) |
| Domains | |||||
| Functional limitation | 0.6 (1.1) | 0.6 (1.0) | 0.9131 | 0.6 (1.1) | 0.13 [0.22] (0.548) |
| Physical pain | 1.5 (1.3) | 1.5 (1.3) | 0.3854 | 1.5 (1.3) | 0.08 [0.14] (0.578) |
| Psychological discomfort | 1.97 (1.5) | 1.5 (1.4) | 0.6862 | 1.7 (1.5) | −0.03 [0.13] (0.798) |
| Physical disability | 0.8 (1.1) | 0.8 (1.1) | 0.3385 | 0.8 (1.1) | −0.02 [0.19] (0.933) |
| Psychological disability | 1.5 (1.4) | 1.2 (1.3) | 0.8935 | 1.3 (1.4) | −0.07 [0.14] (0.600) |
| Social disability | 0.5 (1.0) | 0.4 (0.9) | 0.4068 | 0.5 (1.0) | 0.10 [0.24] (0.682) |
| Handicap | 0.6 (1.0) | 0.6 (1.0) | 0.3949 | 0.6 (1.0) | 0.07 [0.23] (0.762) |
| OHIP-14, Mean (SD) | PP-MP | PP-MP | p-Value * | Total (n = 92) | Adjusted Model for Sex and Age, [SE] (p-Value) |
|---|---|---|---|---|---|
| Hyperdivergent (n = 39) | Normodivergent (n = 53) | ||||
| Total | 13.4 (11.0) | 14.7 (11.4) | 0.5472 | 14.1 (11.3) | 0.10 [0.06] (0.092) |
| Domains | |||||
| Functional limitation | 0.5 (1.0) | 0.6 (1.1) | 0.7363 | 0.6 (1.1) | 0.16 [0.20] (0.414) |
| Physical pain | 1.3 (1.2) | 1.6 (1.3) | 0.3716 | 1.5 (1.3) | 0.22 [0.13] (0.079) |
| Psychological discomfort | 1.7 (1.4) | 1.8 (1.5) | 0.2970 | 1.8 (1.5) | 0.01 [0.11] (0.937) |
| Physical disability | 0.8 (1.1) | 0.8 (1.1) | 0.2376 | 0.8 (1.1) | −0.02 [0.17] (0.898) |
| Psychological disability | 1.3 (1.3) | 1.4 (1.4) | 0.8987 | 1.3 (1.4) | 0.10 [0.13] (0.449) |
| Social disability | 0.5 (1.0) | 0.5 (1.0) | 0.4350 | 0.5 (1.0) | 0.06 [0.21] (0.788) |
| Handicap | 0.6 (1.0) | 0.7 (1.0) | 0.5280 | 0.6 (1.0) | 0.15 [0.19] (0.433) |
| OHIP-14, Mean (SD) | ODI | ODI | p-Value * | Total (n = 85) | Adjusted Model for Sex and Age, [SE] (p-Value) |
|---|---|---|---|---|---|
| Hyperdivergent (n = 28) | Normodivergent (n = 57) | ||||
| Total | 13.1 (11.3) | 14.6 (8.8) | 0.7516 | 14.2 (11.1) | 0.04 [0.06] (0.493) |
| Domains | |||||
| Functional limitation | 0.5 (1.0) | 0.6 (1.1) | 0.6035 | 0.6 (1.1) | 0.04 [0.22] (0.846) |
| Physical pain | 1.2 (1.2) | 1.6 (1.3) | 0.4698 | 1.5 (1.3) | 0.18 [0.14] (0.204) |
| Psychological discomfort | 1.7 (1.4) | 1.8 (1.5) | 0.6392 | 1.8 (1.4) | −0.00 [0.12] (0.977) |
| Physical disability | 0.7 (1.1) | 0.8 (1.2) | 0.7971 | 0.8 (1.1) | 0.04 [0.19] (0.802) |
| Psychological disability | 1.3 (1.3) | 1.4 (1.4) | 0.9279 | 1.4 (1.4) | 0.07 [0.15] (0.628) |
| Social disability | 0.6 (1.2) | 0.4 (0.9) | 0.4175 | 0.5 (1.0) | −0.36 [0.23] (0.128) |
| Handicap | 0.6 (1.1) | 0.7 (1.0) | 0.7007 | 0.7 (1.0) | 0.15 [0.21] (0.484) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pereira, D.; Machado, V.; Botelho, J.; Lemos, C.; Mendes, J.J.; Delgado, A.S. Vertical Dentofacial Skeletal Divergency Is Not Linked with Oral Health-Related Quality of Life. J. Clin. Med. 2024, 13, 665. https://doi.org/10.3390/jcm13030665
Pereira D, Machado V, Botelho J, Lemos C, Mendes JJ, Delgado AS. Vertical Dentofacial Skeletal Divergency Is Not Linked with Oral Health-Related Quality of Life. Journal of Clinical Medicine. 2024; 13(3):665. https://doi.org/10.3390/jcm13030665
Chicago/Turabian StylePereira, Dinis, Vanessa Machado, João Botelho, Carolina Lemos, José João Mendes, and Ana Sintra Delgado. 2024. "Vertical Dentofacial Skeletal Divergency Is Not Linked with Oral Health-Related Quality of Life" Journal of Clinical Medicine 13, no. 3: 665. https://doi.org/10.3390/jcm13030665
APA StylePereira, D., Machado, V., Botelho, J., Lemos, C., Mendes, J. J., & Delgado, A. S. (2024). Vertical Dentofacial Skeletal Divergency Is Not Linked with Oral Health-Related Quality of Life. Journal of Clinical Medicine, 13(3), 665. https://doi.org/10.3390/jcm13030665










