Classification and Incidence of Heterotopic Ossifications in Relation to NSAID Prophylaxis after Elbow Trauma
Abstract
1. Introduction
2. Materials and Methods
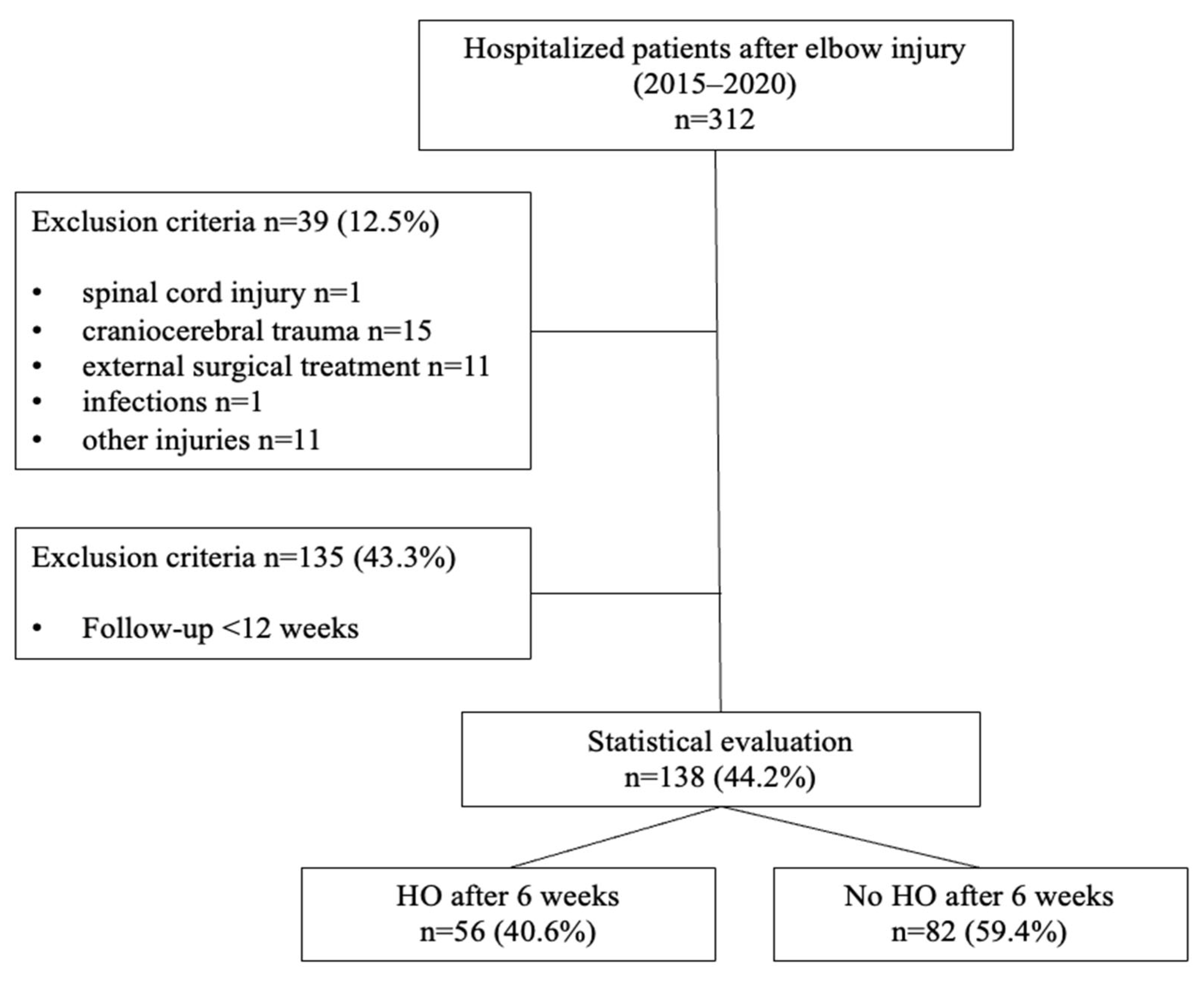
2.1. Patient Collective and Study Design
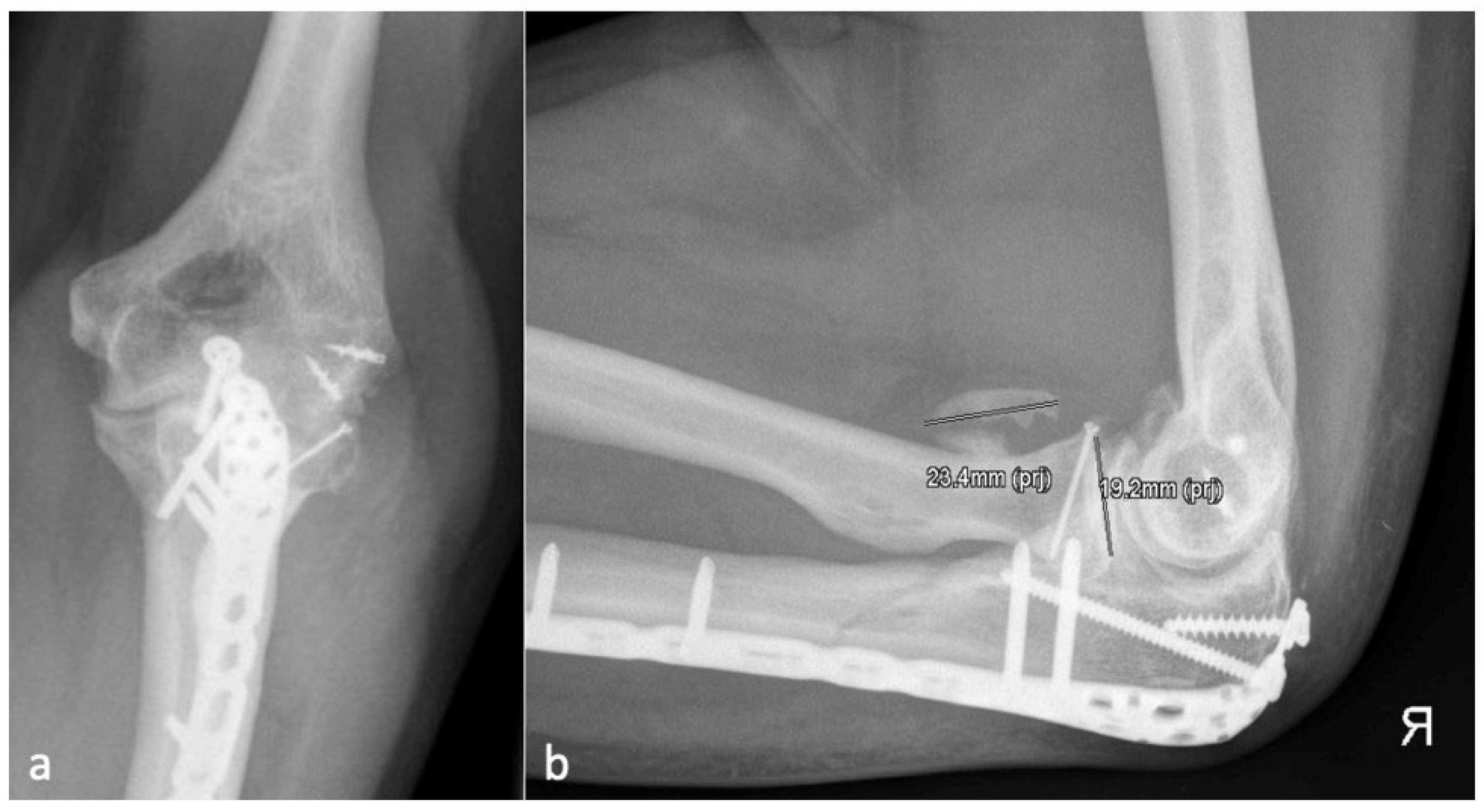
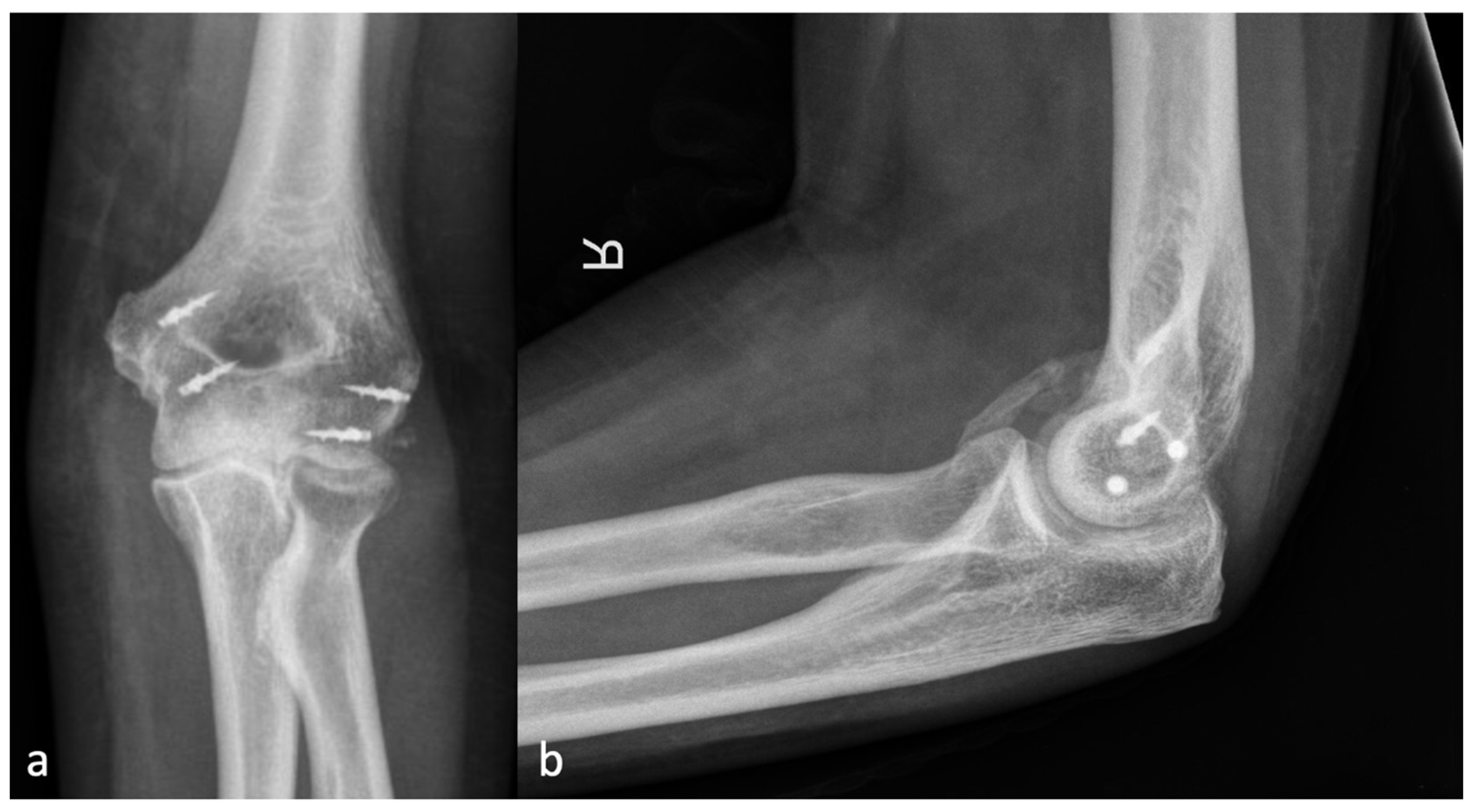
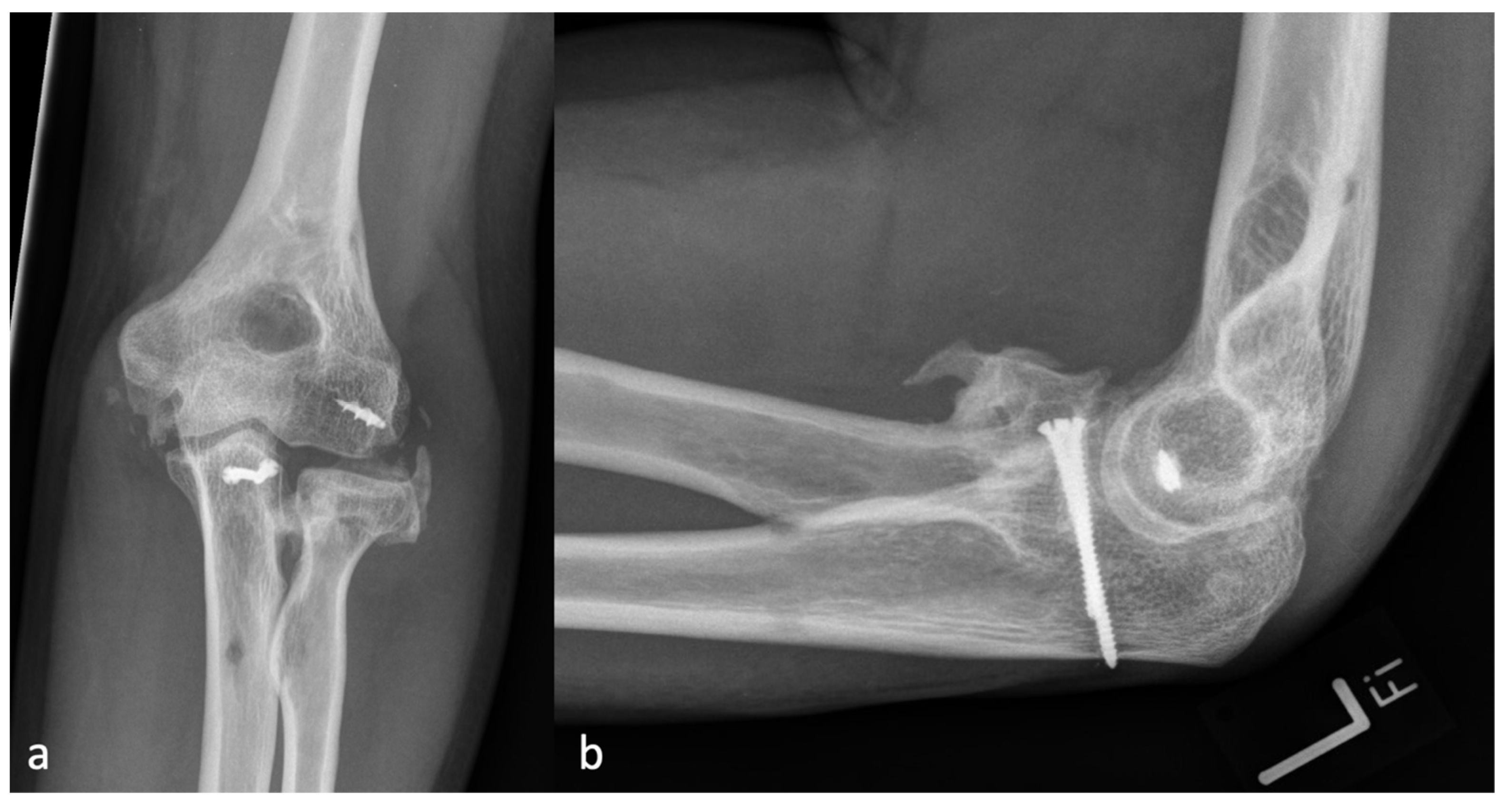
2.2. Radiographic Assessment
2.3. Classification
2.4. Further Parameters
- -
- Lateral: radial head fracture, LCL tear, lateral condyle fractures of the humerus.
- -
- Ventral: Coronoid fractures.
- -
- Medial: MCL tear, medial condyle fractures of the humerus.
- -
- Dorsal: Olecranon fractures.
- -
- Multilateral: Distal humerus fractures (AO C 1–3), Monteggia fractures, Monteggia-like-lesions, LCL, and MCL rupture at the same time.
2.5. Statistical Analysis
3. Results
3.1. Descriptive Statistics
3.2. Relationship between Injury Localization and the Localization of HO
3.3. Correlation between the Application of Ossification Prophylaxis and the Severity of HO
3.4. Intra- and Interobserver Reliability
4. Discussion
4.1. Classification
4.2. Incidences of HO
4.3. Prophylaxis of HO
4.4. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Matsuo, K.; Chavez, R.D.; Barruet, E.; Hsiao, E.C. Inflammation in Fibrodysplasia Ossificans Progressiva and Other Forms of Heterotopic Ossification. Curr. Osteoporos. Rep. 2019, 17, 387–394. [Google Scholar] [CrossRef]
- Ramirez, D.M.; Ramirez, M.R.; Reginato, A.M.; Medici, D. Molecular and cellular mechanisms of heterotopic ossification. Histol. Histopathol. 2014, 29, 1281–1285. [Google Scholar] [CrossRef] [PubMed]
- Evans, K.N.; Forsberg, J.A.; Potter, B.K.; Hawksworth, J.S.; Brown, T.S.; Andersen, R.; Dunne, J.R.; Tadaki, D.; Elster, E.A. Inflammatory cytokine and chemokine expression is associated with heterotopic ossification in high-energy penetrating war injuries. J. Orthop. Trauma 2012, 26, e204–e213. [Google Scholar] [CrossRef] [PubMed]
- Vasileiadis, G.I.; Ramazanian, T.; Kamaci, S.; Bachman, D.R.; Park, S.E.; Thaveepunsan, S.; Fitzsimmons, J.S.; O’Driscoll, S.W. Loss of pronation-supination in patients with heterotopic ossification around the elbow. J. Shoulder Elb. Surg. 2019, 28, 1406–1410. [Google Scholar] [CrossRef] [PubMed]
- Wiggers, J.K.; Helmerhorst, G.T.; Brouwer, K.M.; Niekel, M.C.; Nunez, F.; Ring, D. Injury complexity factors predict heterotopic ossification restricting motion after elbow trauma. Clin. Orthop. Relat. Res. 2014, 472, 2162–2167. [Google Scholar] [CrossRef] [PubMed]
- Veltman, E.S.; Lindenhovius, A.L.; Kloen, P. Improvements in elbow motion after resection of heterotopic bone: A systematic review. Strateg. Trauma Limb Reconstr. 2014, 9, 65–71. [Google Scholar] [CrossRef][Green Version]
- Dey, D.; Wheatley, B.M.; Cholok, D.; Agarwal, S.; Yu, P.B.; Levi, B.; Davis, T.A. The traumatic bone: Trauma-induced heterotopic ossification. Transl. Res. 2017, 186, 95–111. [Google Scholar] [CrossRef] [PubMed]
- Lin, L.; Shen, Q.; Leng, H.; Duan, X.; Fu, X.; Yu, C. Synergistic inhibition of endochondral bone formation by silencing Hif1α and Runx2 in trauma-induced heterotopic ossification. Mol. Ther. 2011, 19, 1426–1432. [Google Scholar] [CrossRef]
- Douglas, K.; Cannada, L.K.; Archer, K.R.; Dean, D.B.; Lee, S.; Obremskey, W. Incidence and risk factors of heterotopic ossification following major elbow trauma. Orthopedics 2012, 35, e815–e822. [Google Scholar] [CrossRef]
- Liu, E.Y.; Hildebrand, A.; Horner, N.S.; Athwal, G.S.; Khan, M.; Alolabi, B. Heterotopic ossification after total elbow arthroplasty: A systematic review. J. Shoulder Elb. Surg. 2019, 28, 587–595. [Google Scholar] [CrossRef]
- Wahl, E.P.; Casey, P.M.; Risoli, T.; Green, C.L.; Richard, M.J.; Ruch, D.S. Heterotopic ossification formation after fractures about the elbow. Eur. J. Orthop. Surg. Traumatol. 2021, 31, 1061–1067. [Google Scholar] [CrossRef]
- Morrey, B.F. The posttraumatic stiff elbow. Clin. Orthop. Relat. Res. 2005, 431, 26–35. [Google Scholar]
- Masci, G.; Cazzato, G.; Milano, G.; Ciolli, G.; Malerba, G.; Perisano, C.; Greco, T.; Osvaldo, P.; Maccauro, G.; Liuzza, F. The stiff elbow: Current concepts. Orthop. Rev. 2020, 12 (Suppl. 1), 8661. [Google Scholar] [CrossRef] [PubMed]
- Brooker, A.F.; Bowerman, J.W.; Robinson, R.A.; Riley, L.H. Ectopic ossification following total hip replacement. Incidence and a method of classification. J. Bone Jt. Surg. Am. 1973, 55, 1629–1632. [Google Scholar] [CrossRef]
- Hastings, H.; Graham, T.J. The classification and treatment of heterotopic ossification about the elbow and forearm. Hand Clin. 1994, 10, 417–437. [Google Scholar] [CrossRef] [PubMed]
- Koh, K.H.; Lim, T.K.; Lee, H.I.; Park, M.J. Surgical treatment of elbow stiffness caused by post-traumatic heterotopic ossification. J. Shoulder Elb. Surg. 2013, 22 (Suppl. 1), 1128–1134. [Google Scholar] [CrossRef] [PubMed]
- Salazar, D.; Golz, A.; Israel, H.; Marra, G. Heterotopic ossification of the elbow treated with surgical resection: Risk factors, bony ankylosis, and complications. Clin. Orthop. Relat. Res. 2014, 472, 2269–2275. [Google Scholar] [CrossRef] [PubMed]
- Sun, Y.; Cai, J.; Li, F.; Liu, S.; Ruan, H.; Fan, C. The efficacy of celecoxib in preventing heterotopic ossification recurrence after open arthrolysis for post-traumatic elbow stiffness in adults. J. Shoulder Elb. Surg. 2015, 24, 1735–1740. [Google Scholar] [CrossRef]
- Joice, M.; Vasileiadis, G.I.; Amanatullah, D.F. Non-steroidal anti-inflammatory drugs for heterotopic ossification prophylaxis after total hip arthroplasty: A systematic review and meta-analysis. Bone Jt. J. 2018, 100, 915–922. [Google Scholar] [CrossRef]
- Kan, S.L.; Yang, B.; Ning, G.Z.; Chen, L.X.; Li, Y.L.; Gao, S.J.; Chen, X.Y.; Sun, J.C.; Feng, S.Q. Nonsteroidal Anti-inflammatory Drugs as Prophylaxis for Heterotopic Ossification after Total Hip Arthroplasty: A Systematic Review and Meta-Analysis. Medicine 2015, 94, e828. [Google Scholar] [CrossRef]
- Ma, R.; Chen, G.H.; Zhao, L.J.; Zhai, X.C. Efficacy of naproxen prophylaxis for the prevention of heterotopic ossification after hip surgery: A meta-analysis. J. Orthop. Surg. Res. 2018, 13, 48. [Google Scholar] [CrossRef] [PubMed]
- Bochat, K.; Mattin, A.C.; Ricciardo, B.J. The efficacy of nonsteroidal anti-inflammatories in the prevention of heterotopic ossification following elbow trauma surgery. JSES Int. 2021, 5, 793–796. [Google Scholar] [CrossRef] [PubMed]
- Atwan, Y.; Abdulla, I.; Grewal, R.; Faber, K.J.; King, G.J.W.; Athwal, G.S. Indomethacin for heterotopic ossification prophylaxis following surgical treatment of elbow trauma: A randomized controlled trial. J. Shoulder Elb. Surg. 2023, 32, 1242–1248. [Google Scholar] [CrossRef] [PubMed]
- Li, F.; Mao, D.; Pan, X.; Zhang, X.; Mi, J.; Rui, Y. Celecoxib cannot inhibit the progression of initiated traumatic heterotopic ossification. J. Shoulder Elb. Surg. 2019, 28, 2379–2385. [Google Scholar] [CrossRef] [PubMed]
- Landis, J.R.; Koch, G.G. The measurement of observer agreement for categorical data. Biometrics 1977, 33, 159–174. [Google Scholar] [CrossRef]
- Herman, Z.J.; Edelman, D.G.; Ilyas, A.M. Heterotopic Ossification After Elbow Fractures. Orthopedics 2021, 44, 10–16. [Google Scholar] [CrossRef]
- Foruria, A.M.; Lawrence, T.M.; Augustin, S.; Morrey, B.F.; Sanchez-Sotelo, J. Heterotopic ossification after surgery for distal humeral fractures. Bone Jt. J. 2014, 96, 1681–1687. [Google Scholar] [CrossRef]
- Hong, C.C.; Nashi, N.; Hey, H.W.; Chee, Y.H.; Murphy, D. Clinically relevant heterotopic ossification after elbow fracture surgery: A risk factors study. Orthop. Traumatol. Surg. Res. 2015, 101, 209–213. [Google Scholar] [CrossRef]
- Costopoulos, C.L.; Abboud, J.A.; Ramsey, M.L.; Getz, C.L.; Sholder, D.S.; Taras, J.P.; Huttman, D.; Lazarus, M.D. The use of indomethacin in the prevention of postoperative radioulnar synostosis after distal biceps repair. J. Shoulder Elb. Surg. 2017, 26, 295–298. [Google Scholar] [CrossRef]
- Winkler, S.; Wagner, F.; Weber, M.; Matussek, J.; Craiovan, B.; Heers, G.; Springorum, H.R.; Grifka, J.; Renkawitz, T. Current therapeutic strategies of heterotopic ossification—A survey amongst orthopaedic and trauma departments in Germany. BMC Musculoskelet. Disord. 2015, 16, 313. [Google Scholar] [CrossRef][Green Version]
- O’Driscoll, S.W.; Morrey, B.F.; Korinek, S.; An, K.N. Elbow subluxation and dislocation. A spectrum of instability. Clin. Orthop. Relat. Res. 1992, 280, 186–197. [Google Scholar]

| Severity | Localization | |
|---|---|---|
| Absence of HO | 0 | |
| <∅ radial head | 1 | r, p, u, a |
| >∅ radial head | 2 | r, p, u, a |
| Brace formation | 3 | r, p, u, a |
| Synostosis radio-ulnar | 4 |
| HO Incidence (%) | Severity Incidence of HO (%) | Location Incidence of HO (%) | |||
|---|---|---|---|---|---|
| HO Grade | HO Localization | ||||
| 6 weeks | 56 (40.6) | 0 | 82 (59.4) | r | 18 (32.1) |
| 1 | 49 (35.5) | p | 6 (10.7) | ||
| 2 | 6 (4.3) | u | 11 (19.6) | ||
| 3 | 1 (0.7) | a | 21 (37.5) | ||
| 12 weeks | 70 (50.7) | 0 | 68 (49.3) | r | 15 (26.8) |
| 1 | 57 (41.3) | p | 5 (8.9) | ||
| 2 | 9 (6.5) | u | 12 (21.4) | ||
| 3 | 4 (2.9) | a | 23 (41.1) | ||
| 6 months | 45 (60.0) | 0 | 30 (40.0) | r | 10 (31.3) |
| 1 | 30 (40.0) | p | 1 (3.1) | ||
| 2 | 9 (12.0) | u | 5 (15.6) | ||
| 3 | 2 (2.7) | a | 16 (50.0) | ||
| 4 | 4 (5.3) | ||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Leyder, D.; Döbele, S.; Konrads, C.; Histing, T.; Fischer, C.S.; Ahrend, M.-D.; Ziegler, P. Classification and Incidence of Heterotopic Ossifications in Relation to NSAID Prophylaxis after Elbow Trauma. J. Clin. Med. 2024, 13, 667. https://doi.org/10.3390/jcm13030667
Leyder D, Döbele S, Konrads C, Histing T, Fischer CS, Ahrend M-D, Ziegler P. Classification and Incidence of Heterotopic Ossifications in Relation to NSAID Prophylaxis after Elbow Trauma. Journal of Clinical Medicine. 2024; 13(3):667. https://doi.org/10.3390/jcm13030667
Chicago/Turabian StyleLeyder, Diane, Stefan Döbele, Christian Konrads, Tina Histing, Cornelius S. Fischer, Marc-Daniel Ahrend, and Patrick Ziegler. 2024. "Classification and Incidence of Heterotopic Ossifications in Relation to NSAID Prophylaxis after Elbow Trauma" Journal of Clinical Medicine 13, no. 3: 667. https://doi.org/10.3390/jcm13030667
APA StyleLeyder, D., Döbele, S., Konrads, C., Histing, T., Fischer, C. S., Ahrend, M.-D., & Ziegler, P. (2024). Classification and Incidence of Heterotopic Ossifications in Relation to NSAID Prophylaxis after Elbow Trauma. Journal of Clinical Medicine, 13(3), 667. https://doi.org/10.3390/jcm13030667







