Improved Extracorporeal Cardiopulmonary Resuscitation (ECPR) Outcomes are Associated with a Restrictive Patient Selection Algorithm
Abstract
1. Introduction
2. Methods
2.1. Setting
2.2. Study Design
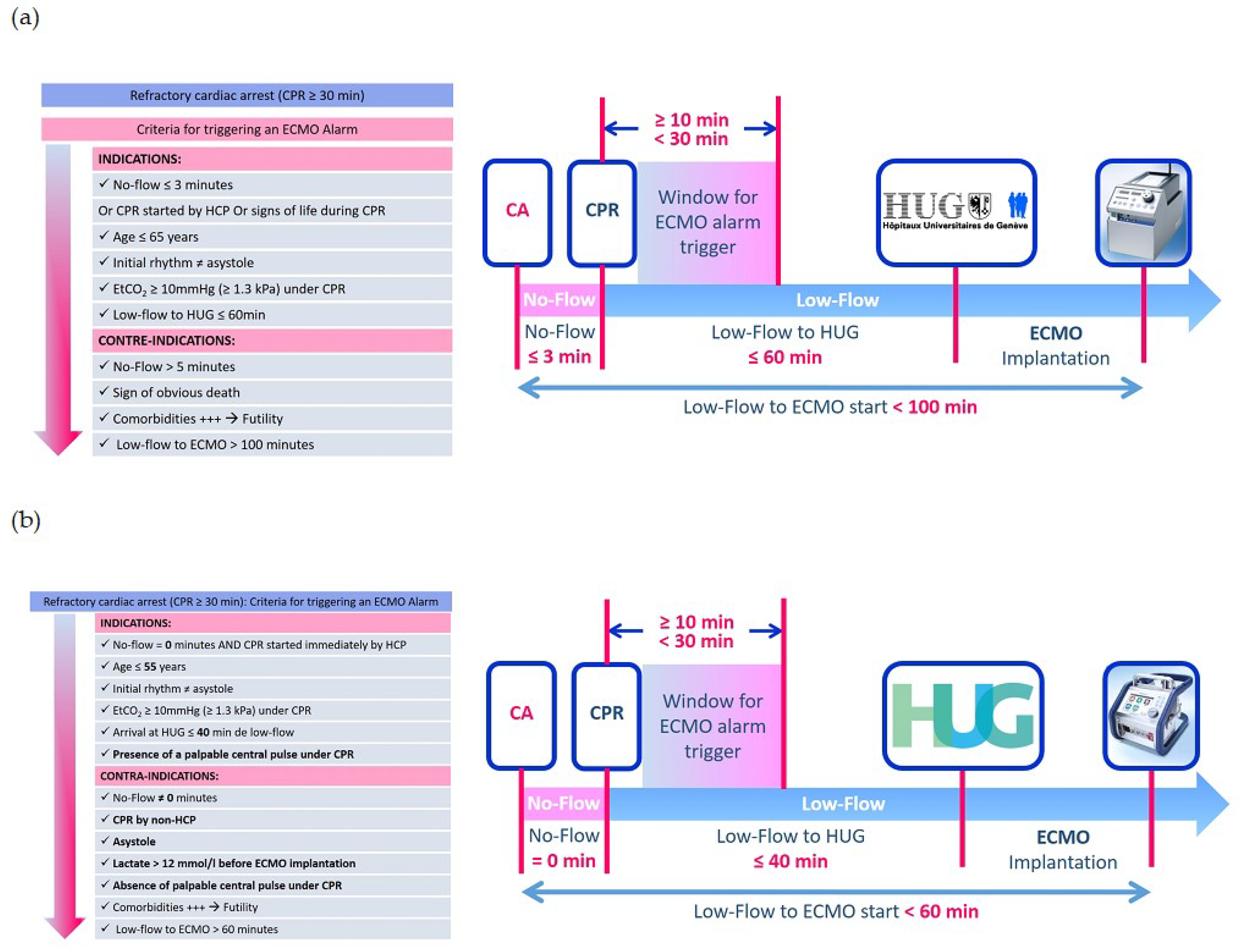
2.3. Study Protocol
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Wong, C.X.; Brown, A.; Lau, D.H.; Chugh, S.S.; Albert, C.M.; Kalman, J.M.; Sanders, P. Epidemiology of Sudden Cardiac Death: Global and Regional Perspectives. Heart Lung Circ. 2019, 28, 6–14. [Google Scholar] [CrossRef] [PubMed]
- Yan, S.; Gan, Y.; Jiang, N.; Wang, R.; Chen, Y.; Luo, Z.; Zong, Q.; Chen, S.; Lv, C. The global survival rate among adult out-of-hospital cardiac arrest patients who received cardiopulmonary resuscitation: A systematic review and meta-analysis. Crit. Care 2020, 24, 61. [Google Scholar] [CrossRef] [PubMed]
- De Charriere, A.; Assouline, B.; Scheen, M.; Mentha, N.; Banfi, C.; Bendjelid, K.; Giraud, R. ECMO in Cardiac Arrest: A Narrative Review of the Literature. J. Clin. Med. 2021, 10, 534. [Google Scholar] [CrossRef] [PubMed]
- Kagawa, E.; Inoue, I.; Kawagoe, T.; Ishihara, M.; Shimatani, Y.; Kurisu, S.; Nakama, Y.; Dai, K.; Takayuki, O.; Ikenaga, H.; et al. Assessment of outcomes and differences between in- and out-of-hospital cardiac arrest patients treated with cardiopulmonary resuscitation using extracorporeal life support. Resuscitation 2010, 81, 968–973. [Google Scholar] [CrossRef]
- Wengenmayer, T.; Rombach, S.; Ramshorn, F.; Biever, P.; Bode, C.; Duerschmied, D.; Staudacher, D.L. Influence of low-flow time on survival after extracorporeal cardiopulmonary resuscitation (eCPR). Crit. Care 2017, 21, 157. [Google Scholar] [CrossRef]
- Link, M.S.; Berkow, L.C.; Kudenchuk, P.J.; Halperin, H.R.; Hess, E.P.; Moitra, V.K.; Neumar, R.W.; O’Neil, B.J.; Paxton, J.H.; Silvers, S.M.; et al. Part 7: Adult Advanced Cardiovascular Life Support: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2015, 132, S444–S464. [Google Scholar] [CrossRef] [PubMed]
- Mancini, M.E.; Diekema, D.S.; Hoadley, T.A.; Kadlec, K.D.; Leveille, M.H.; McGowan, J.E.; Munkwitz, M.M.; Panchal, A.R.; Sayre, M.R.; Sinz, E.H. Part 3: Ethical Issues: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2015, 132, S383–S396. [Google Scholar] [CrossRef]
- Soar, J.; Nolan, J.P.; Bottiger, B.W.; Perkins, G.D.; Lott, C.; Carli, P.; Pellis, T.; Sandroni, C.; Skrifvars, M.B.; Smith, G.B.; et al. European Resuscitation Council Guidelines for Resuscitation 2015: Section 3. Adult advanced life support. Resuscitation 2015, 95, 100–147. [Google Scholar] [CrossRef]
- Yannopoulos, D.; Bartos, J.; Raveendran, G.; Walser, E.; Connett, J.; Murray, T.A.; Collins, G.; Zhang, L.; Kalra, R.; Kosmopoulos, M.; et al. Advanced reperfusion strategies for patients with out-of-hospital cardiac arrest and refractory ventricular fibrillation (ARREST): A phase 2, single centre, open-label, randomised controlled trial. Lancet 2020, 396, 1807–1816. [Google Scholar] [CrossRef]
- Belohlavek, J.; Smalcova, J.; Rob, D.; Franek, O.; Smid, O.; Pokorna, M.; Horak, J.; Mrazek, V.; Kovarnik, T.; Zemanek, D.; et al. Effect of Intra-arrest Transport, Extracorporeal Cardiopulmonary Resuscitation, and Immediate Invasive Assessment and Treatment on Functional Neurologic Outcome in Refractory Out-of-Hospital Cardiac Arrest: A Randomized Clinical Trial. JAMA 2022, 327, 737–747. [Google Scholar] [CrossRef]
- Suverein, M.M.; Delnoij, T.S.R.; Lorusso, R.; Brandon Bravo Bruinsma, G.J.; Otterspoor, L.; Elzo Kraemer, C.V.; Vlaar, A.P.J.; van der Heijden, J.J.; Scholten, E.; den Uil, C.; et al. Early Extracorporeal CPR for Refractory Out-of-Hospital Cardiac Arrest. N. Engl. J. Med. 2023, 388, 299–309. [Google Scholar] [CrossRef]
- Chen, Y.S.; Lin, J.W.; Yu, H.Y.; Ko, W.J.; Jerng, J.S.; Chang, W.T.; Chen, W.J.; Huang, S.C.; Chi, N.H.; Wang, C.H.; et al. Cardiopulmonary resuscitation with assisted extracorporeal life-support versus conventional cardiopulmonary resuscitation in adults with in-hospital cardiac arrest: An observational study and propensity analysis. Lancet 2008, 372, 554–561. [Google Scholar] [CrossRef] [PubMed]
- Lamhaut, L.; Hutin, A.; Puymirat, E.; Jouan, J.; Raphalen, J.H.; Jouffroy, R.; Jaffry, M.; Dagron, C.; An, K.; Dumas, F.; et al. A Pre-Hospital Extracorporeal Cardio Pulmonary Resuscitation (ECPR) strategy for treatment of refractory out hospital cardiac arrest: An observational study and propensity analysis. Resuscitation 2017, 117, 109–117. [Google Scholar] [CrossRef] [PubMed]
- Yannopoulos, D.; Bartos, J.A.; Martin, C.; Raveendran, G.; Missov, E.; Conterato, M.; Frascone, R.J.; Trembley, A.; Sipprell, K.; John, R.; et al. Minnesota Resuscitation Consortium’s Advanced Perfusion and Reperfusion Cardiac Life Support Strategy for Out-of-Hospital Refractory Ventricular Fibrillation. J. Am. Heart Assoc. 2016, 5, e003732. [Google Scholar] [CrossRef] [PubMed]
- Guy, A.; Kawano, T.; Besserer, F.; Scheuermeyer, F.; Kanji, H.D.; Christenson, J.; Grunau, B. The relationship between no-flow interval and survival with favourable neurological outcome in out-of-hospital cardiac arrest: Implications for outcomes and ECPR eligibility. Resuscitation 2020, 155, 219–225. [Google Scholar] [CrossRef]
- Giraud, R.; Siegenthaler, N.; Schussler, O.; Kalangos, A.; Muller, H.; Bendjelid, K.; Banfi, C. The LUCAS 2 chest compression device is not always efficient: An echographic confirmation. Ann. Emerg. Med. 2015, 65, 23–26. [Google Scholar] [CrossRef]
- Ohbe, H.; Tagami, T.; Ogura, T.; Matsui, H.; Yasunaga, H. Low-Flow Duration and Outcomes of Extracorporeal Cardiopulmonary Resuscitation in Adults with In-Hospital Cardiac Arrest: A Nationwide Inpatient Database Study. Crit. Care Med. 2022, 50, 1768–1777. [Google Scholar] [CrossRef]
- Ralston, S.H.; Voorhees, W.D.; Showen, L.; Schmitz, P.; Kougias, C.; Tacker, W.A. Venous and arterial blood gases during and after cardiopulmonary resuscitation in dogs. Am. J. Emerg. Med. 1985, 3, 132–136. [Google Scholar] [CrossRef]
- Adrie, C.; Cariou, A.; Mourvillier, B.; Laurent, I.; Dabbane, H.; Hantala, F.; Rhaoui, A.; Thuong, M.; Monchi, M. Predicting survival with good neurological recovery at hospital admission after successful resuscitation of out-of-hospital cardiac arrest: The OHCA score. Eur. Heart J. 2006, 27, 2840–2845. [Google Scholar] [CrossRef]
- Gregers, E.; Mork, S.R.; Linde, L.; Andreasen, J.B.; Smerup, M.; Kjaergaard, J.; Moller-Sorensen, P.H.; Holmvang, L.; Christensen, S.; Terkelsen, C.J.; et al. Extracorporeal cardiopulmonary resuscitation: A national study on the association between favourable neurological status and biomarkers of hypoperfusion, inflammation, and organ injury. Eur. Heart J. Acute Cardiovasc. Care 2022, 11, 808–817. [Google Scholar] [CrossRef]
- Wang, C.H.; Huang, C.H.; Chang, W.T.; Tsai, M.S.; Yu, P.H.; Wu, Y.W.; Hung, K.Y.; Chen, W.J. Monitoring of serum lactate level during cardiopulmonary resuscitation in adult in-hospital cardiac arrest. Crit. Care 2015, 19, 344. [Google Scholar] [CrossRef] [PubMed]
- Pozzi, M.; Armoiry, X.; Achana, F.; Koffel, C.; Pavlakovic, I.; Lavigne, F.; Fellahi, J.L.; Obadia, J.F. Extracorporeal Life Support for Refractory Cardiac Arrest: A 10-Year Comparative Analysis. Ann. Thorac. Surg. 2019, 107, 809–816. [Google Scholar] [CrossRef] [PubMed]
- Debaty, G.; Babaz, V.; Durand, M.; Gaide-Chevronnay, L.; Fournel, E.; Blancher, M.; Bouvaist, H.; Chavanon, O.; Maignan, M.; Bouzat, P.; et al. Prognostic factors for extracorporeal cardiopulmonary resuscitation recipients following out-of-hospital refractory cardiac arrest. A systematic review and meta-analysis. Resuscitation 2017, 112, 1–10. [Google Scholar] [CrossRef] [PubMed]
| Permissive Algorithm (1) (n = 23) | Restrictive Algorithm (2) (n = 25) | p | |
|---|---|---|---|
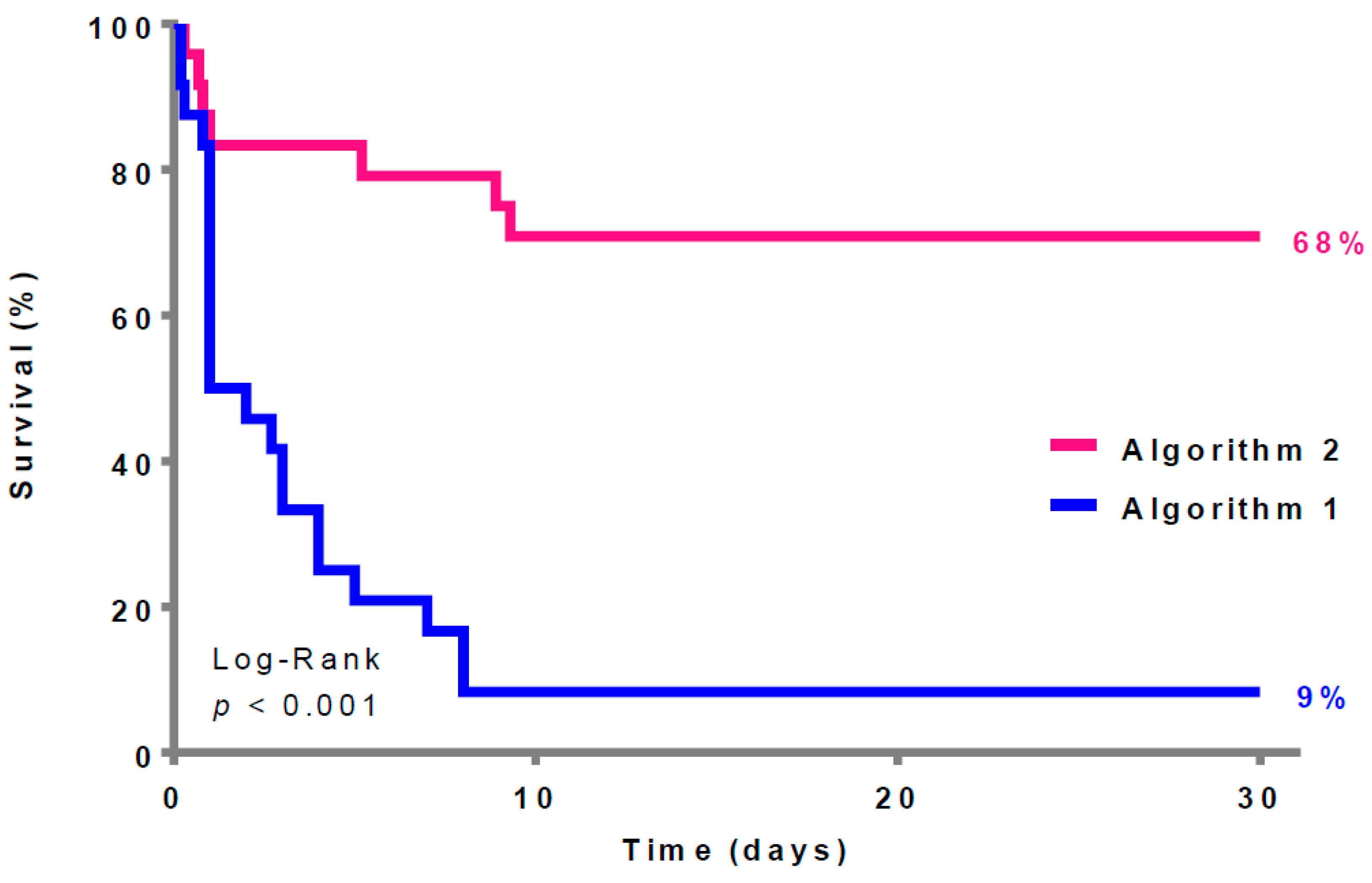
| Survival, n (%) | 2 (9%) | 17 (68%) | <0.01 |
| First rhythm, n (%) | 0.43 | ||
| PEA | 5 (21.7) | 10 (40) | 0.2 |
| VF | 15 (65.2) | 12 (48) | 0.3 |
| VT | 0 | 2 (8) | 0.5 |
| Asystole | 3 (13) | 1 (4) | 0.4 |
| Cause of cardiac arrest, n (%) | 0.8 | ||
| Coronary artery disease | 13 (56.5) | 14 (56) | 0.6 |
| Pulmonary embolism | 3 (13) | 4 (16) | 1 |
| Rhythm disorder | 4 (17.4) | 2 (8) | 0.4 |
| Other | 3 (13) | 5 (20) | 0.7 |
| No-flow time (minutes), median (IQR) | 0 (0–5) | 0 (0–0) | <0.01 |
| Low-flow time (minutes), median (IQR) | 50 (35–90) | 48 (40–60) | 0.4 |
| Cardiac massage providers, n (%) | 0.03 | ||
| Non-HCP * | 11 (47.8) | 6 (24) | 0.1 |
| Paramedics | 9 (39.1) | 6 (24) | 0.3 |
| Nurse | 0 | 4 (16) | 0.1 |
| Doctor | 3 (13%) | 9 (36) | 0.1 |
| Place of ECMO implantation, n (%) | 0.06 | ||
| Operating room | 9 (39.1) | 1 (4) | <0.01 |
| Cath Lab | 7 (30.4) | 9 (36) | 0.8 |
| Emergency room | 4 (17.4) | 13 (52) | 0.02 |
| ICU | 3 (13) | 2 (8) | 0.7 |
| EtCO2 before ECMO (mmHg), median (IQR) | 30 (14–46) | 25 (19.5–35) | 0.4 |
| pH before ECMO, median (IQR) | 7.0 (6.9–7.04) | 7.07 (6.9–7.2) | 0.09 |
| Lactate (mmol/L) before ECMO, median (IQR) | 13.9 (12–15) | 9.3 (7–13.3) | 0.02 |
| Time on ECMO (hours), median (IQR) | 48 (24–96) | 72 (39–213) | 0.2 |
| Age (years), median (IQR) | 51 (47–60) | 56 (51–62) | 0.5 |
| Gender, male, n (%) | 17 (73.9) | 17 (68) | 0.2 |
| Cardiovascular risk factor overall, n (%) | 18 (78.3) | 19 (76) | 0.6 |
| Overweight, n (%) | 13 (56.) | 14 (56) | 1 |
| Hypertension, n (%) | 10 (43.5) | 7 (28) | 0.3 |
| Hypercholesterolemia, n (%) | 8 (34.8) | 9 (36) | 0.4 |
| Diabetes, n (%) | 5 (21.7) | 5 (20) | 1 |
| Smoker, n (%) | 8 (34.8) | 7 (28) | 0.8 |
| Survivor (n = 19) | Non Survivor (n = 29) | p | |
|---|---|---|---|
| Restrictive algorithm, n (%) | 17 (89.5) | 8 (27.6) | <0.01 |
| First rhythm, n (%) | 0.4 | ||
| PEA | 7 (36.8) | 8 (27.6) | 0.5 |
| VF | 11 (57.9) | 16 (55.2) | 1 |
| VT | 1 (5.3) | 1 (3.5) | 1 |
| Asystole | 0 | 4 (13.8) | 0.1 |
| Cause of cardiac arrest, n (%) | 0.6 | ||
| Coronary artery disease | 10 (52.6) | 17 (58.6) | 0.8 |
| Pulmonary embolism | 4 (21.1) | 3 (10.3) | 0.4 |
| Rhythm disorder | 3 (15.8) | 3 (10.3) | 0.4 |
| Other | 2 (10.5) | 6 (20.7) | 0.5 |
| No-flow time (minutes), median (IQR) | 0 (0–0) | 0 (0–3) | <0.01 |
| Low-flow time (minutes), median (IQR) | 40 (31–53) | 60 (45–80) | 0.02 |
| Cardiac massage providers, n (%) | 0.6 | ||
| Non-HCP | 7 (36.8) | 10 (34.5) | 1 |
| Paramedics | 4 (21.1) | 11 (37.9) | 0.3 |
| Nurse | 2 (10.5) | 2 (7) | 1 |
| Doctor | 6 (31.6) | 6 (20.7) | 0.5 |
| Place of ECMO implantation, n (%) | 0.2 | ||
| Operating room | 3 (15.8) | 7 (24.1) | 0.7 |
| Cath Lab | 7 (36.8) | 9 (31) | 0.8 |
| Emergency room | 9 (47.4) | 8 (27.6) | 0.2 |
| ICU | 0 | 5 (17.2) | 0.1 |
| EtCO2(mmHg), median (IQR) | 25 (22–35) | 25 (13–37) | 0.9 |
| pH before ECMO, median (IQR) | 7.1 (6.9–7.2) | 7 (6.9–7.1) | 0.09 |
| Lactate (mmol/L) before ECMO, median (IQR) | 8.6 (6.7–12.1) | 13.9 (10.8–15) | <0.01 |
| Time on ECMO (hours), median (IQR) | 96 (48–288) | 24 (20–96) | <0.01 |
| Age (years), median (IQR) | 55 (43–62) | 52 (48–60) | 0.8 |
| Gender, male, n (%) | 11 (57.9) | 23 (79.3) | 0.2 |
| Cardiovascular risk factor overall, n (%) | 11 (57.9) | 26 (89.7) | 0.01 |
| Overweight, n (%) | 9 (47.4) | 18 (62.1) | 0.4 |
| Hypertension, n (%) | 4 (21.1) | 13 (44.8) | 0.08 |
| Hypercholesterolemia, n (%) | 7 (36.8) | 10 (34.5) | 0.6 |
| Diabetes, n (%) | 2 (10.5) | 8 (27.6) | 0.3 |
| Smoker, n (%) | 3 (15.8) | 12 (41.4) | 0.06 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Assouline, B.; Mentha, N.; Wozniak, H.; Donner, V.; Looyens, C.; Suppan, L.; Larribau, R.; Banfi, C.; Bendjelid, K.; Giraud, R. Improved Extracorporeal Cardiopulmonary Resuscitation (ECPR) Outcomes are Associated with a Restrictive Patient Selection Algorithm. J. Clin. Med. 2024, 13, 497. https://doi.org/10.3390/jcm13020497
Assouline B, Mentha N, Wozniak H, Donner V, Looyens C, Suppan L, Larribau R, Banfi C, Bendjelid K, Giraud R. Improved Extracorporeal Cardiopulmonary Resuscitation (ECPR) Outcomes are Associated with a Restrictive Patient Selection Algorithm. Journal of Clinical Medicine. 2024; 13(2):497. https://doi.org/10.3390/jcm13020497
Chicago/Turabian StyleAssouline, Benjamin, Nathalie Mentha, Hannah Wozniak, Viviane Donner, Carole Looyens, Laurent Suppan, Robert Larribau, Carlo Banfi, Karim Bendjelid, and Raphaël Giraud. 2024. "Improved Extracorporeal Cardiopulmonary Resuscitation (ECPR) Outcomes are Associated with a Restrictive Patient Selection Algorithm" Journal of Clinical Medicine 13, no. 2: 497. https://doi.org/10.3390/jcm13020497
APA StyleAssouline, B., Mentha, N., Wozniak, H., Donner, V., Looyens, C., Suppan, L., Larribau, R., Banfi, C., Bendjelid, K., & Giraud, R. (2024). Improved Extracorporeal Cardiopulmonary Resuscitation (ECPR) Outcomes are Associated with a Restrictive Patient Selection Algorithm. Journal of Clinical Medicine, 13(2), 497. https://doi.org/10.3390/jcm13020497








