Temporal Trends in Patient Characteristics and Clinical Outcomes of TAVR: Over a Decade of Practice
Abstract
1. Introduction
2. Methods
3. Results
3.1. Patient Characteristics
3.2. Procedural Characteristics
3.3. Outcomes
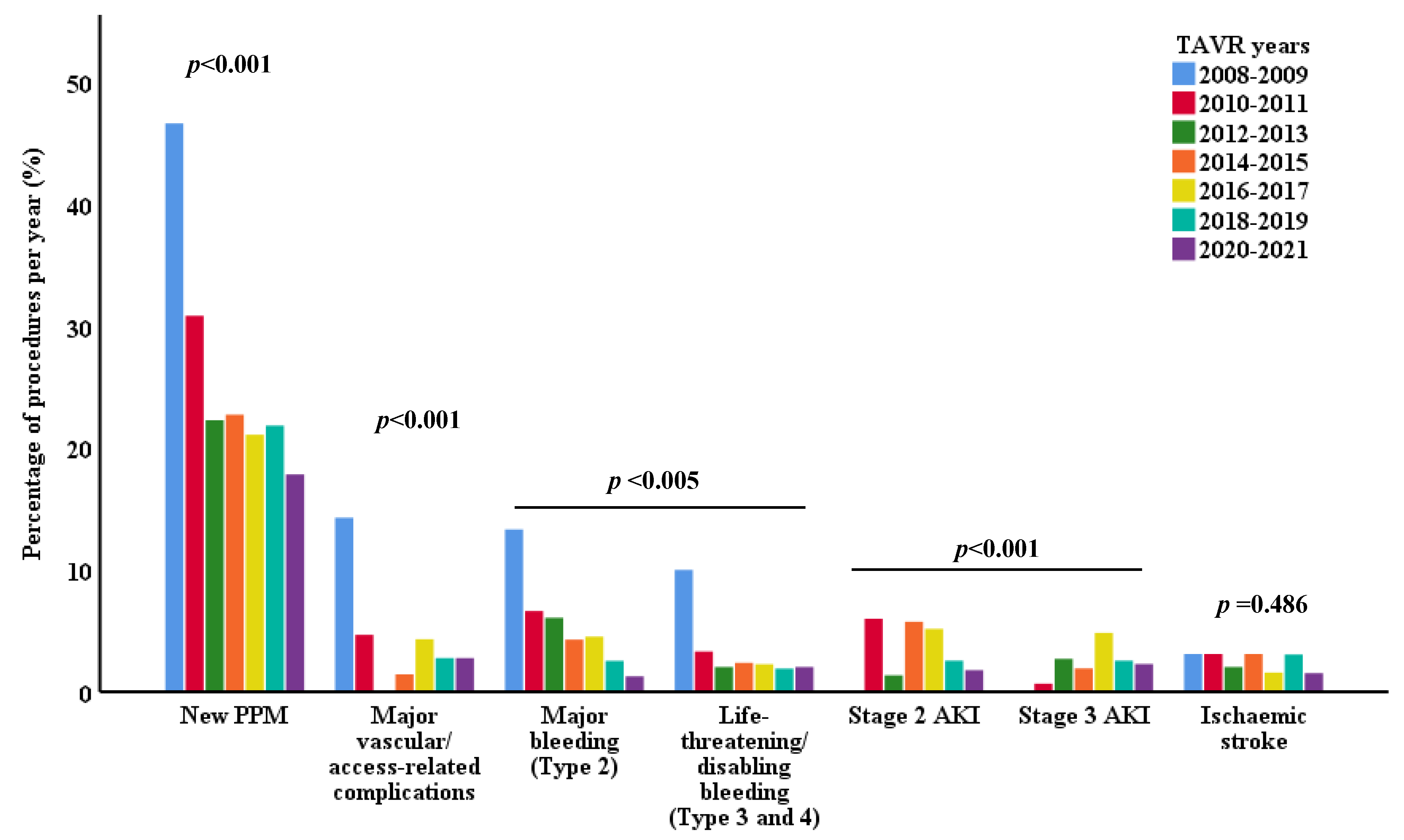
3.4. Procedure Complications
3.5. Mortality
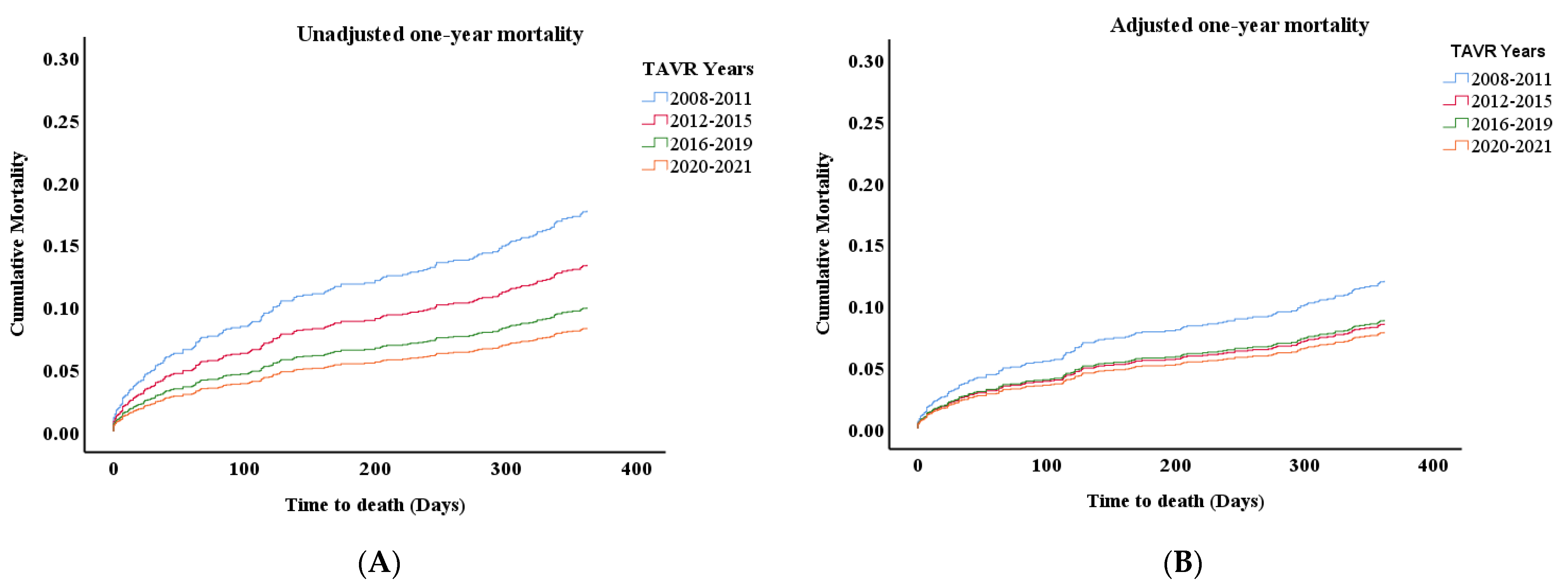
4. Discussion
Study Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Leon, M.B.; Smith, C.R.; Mack, M.; Miller, D.C.; Moses, J.W.; Svensson, L.G.; Tuzcu, E.M.; Webb, J.G.; Fontana, G.P.; Makkar, R.R.; et al. PARTNER Trial Investigators. Transcatheter aortic-valve implantation for aortic stenosis in patients who cannot undergo surgery. N. Engl. J. Med. 2010, 363, 1597–1607. [Google Scholar] [CrossRef] [PubMed]
- Deeb, G.M.; Reardon, M.J.; Chetcuti, S.; Patel, H.J.; Grossman, P.M.; Yakubov, S.J.; Kleiman, N.S.; Coselli, J.S.; Gleason, T.J.; Lee, J.S.; et al. CoreValve USCI. 3-Year outcomes in high-risk patients who underwent surgical or transcatheter aortic valve replacement. J. Am. Coll. Cardiol. 2016, 67, 2565–2574. [Google Scholar] [CrossRef] [PubMed]
- Smith, C.R.; Leon, M.B.; Mack, M.J.; Miller, D.C.; Moses, J.W.; Svensson, L.G.; Tuzcu, E.M.; Webb, J.G.; Fontana, G.P.; Makkar, R.R.; et al. PARTNER Trial Investigators. Transcatheter versus surgical aortic-valve replacement in high-risk patients. N. Engl. J. Med. 2011, 364, 2187–2198. [Google Scholar] [CrossRef]
- Vahanian, A.; Beyersdorf, F. 2021 ESC/EACTS Guidelines for the management of valvular heart disease. Eur. Heart J. 2022, 43, 561–632. [Google Scholar] [CrossRef] [PubMed]
- Leon, M.B.; Smith, C.R.; Mack, M.J.; Makkar, R.R.; Svensson, L.G.; Kodali, S.K.; Thourani, V.H.; Tuzcu, E.M.; Miller, D.C.; Herrmann, H.C.; et al. PARTNER 2 Investigators. Transcatheter or surgical aortic-valve replacement in intermediate-risk patients. N. Engl. J. Med. 2016, 374, 1609–1620. [Google Scholar] [CrossRef] [PubMed]
- Reardon, M.J.; van Mieghem, N.M.; Popma, J.J.; Kleiman, N.S.; Søndergaard, L.; Mumtaz, M.; Adams, D.H.; Deeb, M.; Maini, B.; Gada, H.; et al. Surgical or transcatheter aortic-valve replacement in intermediate-risk patients. N. Engl. J. Med. 2017, 376, 1321–1331. [Google Scholar] [CrossRef]
- Mack, M.J.; Leon, M.B.; Thourani, V.H.; Makkar, R.; Kodali, S.K.; Russo, M.; Kapadia, S.R.; Malaisrie, S.C.; Cohen, D.J.; Pibarot, P.; et al. PARTNER 3 Investigators. Transcatheter aortic-valve replacement with a balloon-expandable valve in low-risk patients. N. Engl. J. Med. 2019, 380, 1695–1705. [Google Scholar] [CrossRef]
- Popma, J.J.; Deeb, G.M.; Yakubov, S.J.; Mumtaz, M.; Gada, H.; O’Hair, D.; Bajwa, T.; Heiser, J.C.; Merhi, W.; Kleiman, N.S.; et al. Evolut Low Risk Trial Investigators. Transcatheter aortic-valve replacement with a self-expanding valve in low-risk patients. N. Engl. J. Med. 2019, 380, 1706–1715. [Google Scholar] [CrossRef]
- Leon, M.B.; Mack, M.J.; Hahn, R.T.; Thourani, V.H.; Makkar, R.; Kodali, S.K.; Alu, M.C.; Madhavan, M.V.; Chau, K.H.; Russo, M.; et al. PARTNER 3 Investigators. Outcomes 2 years after transcatheter aortic valve replacement in patients at low surgical risk. J. Am. Coll. Cardiol. 2021, 77, 1149–1161. [Google Scholar] [CrossRef]
- Carroll, J.D.; Mack, M.J.; Vemulapalli, S.; Herrmann, H.C.; Gleason, T.G.; Hanzel, G.; Deeb, G.M.; Thourani, V.H.; Cohen, D.J.; Desai, N.; et al. STS-ACC TVT Registry of Transcatheter Aortic Valve Replacement. J. Am. Coll. Cardiol. 2020, 76, 2492–2516. [Google Scholar] [CrossRef]
- Mauri, V.; Abdel-Wahab, M.; Bleiziffer, S.; Veulemans, V.; Sedaghat, A.; Adam, M.; Nickenig, G.; Kelm, M.; Thiele, H.; Baldus, S.; et al. Temporal trends of TAVI treatment characteristics in high volume centers in Germany 2013–2020. Clin. Res. Cardiol. 2022, 111, 881–888. [Google Scholar] [CrossRef]
- Didier, R.; Le Breton, H.; Eltchaninoff, H.; Cayla, G.; Commeau, P.; Collet, J.-P.; Cuisset, T.; Dumonteil, N.; Verhoye, J.-P.; Beurtheret, S.; et al. Evolution of TAVI patients and techniques over the past decade: The French TAVI registries. Arch. Cardiovasc. Dis. 2022, 115, 206–213. [Google Scholar] [CrossRef]
- Graversen, P.L.; Butt, J.H.; Østergaard, L.; Jensen, A.D.; Warming, P.E.; Strange, J.E.; Møller, C.H.; Schou, M.; De Backer, O.; Køber, L.; et al. Changes in aortic valve replacement procedures in Denmark from 2008 to 2020. Heart 2023, 109, 557–563. [Google Scholar] [CrossRef] [PubMed]
- Auffret, V.; Lefevre, T.; Van Belle, E.; Eltchaninoff, H.; Iung, B.; Koning, R.; Motreff, P.; Leprince, P.; Verhoye, J.P.; Manigold, T.; et al. Temporal Trends in Transcatheter Aortic Valve Replacement in France. FRANCE 2 to FRANCE TAVI. J. Am. Coll. Cardiol. 2017, 70, 42–55. [Google Scholar] [CrossRef] [PubMed]
- Stortecky, S.; Franzone, A.; Heg, D.; Tueller, D.; Noble, S.; Pilgrim, T.; Jeger, R.; Toggweiler, S.; Ferrari, E.; Nietlispach, F.; et al. Temporal trends in adoption and outcomes of transcatheter aortic valve implantation: A Swiss TAVI Registry analysis. Eur. Heart J.-Qual. Care Clin. Outcomes 2019, 5, 242–251. [Google Scholar] [CrossRef] [PubMed]
- Lundahl, C.; Kragholm, K.; Tayal, B.; Karasoy, D.; Andersen, N.H.; Strange, J.E.; Olesen, J.B.; Østergaard, L.; Fosbøl, E.; Torp-Pedersen, C.; et al. Temporal Trends in Patient Characteristics and Outcomes of Transcatheter Aortic Valve Implantation and Surgical Aortic Valve Replacement: A Nationwide Study. Am. J. Cardiol. 2024, 211, 299–306. [Google Scholar] [CrossRef] [PubMed]
- Landes, U.; Barsheshet, A.; Finkelstein, A.; Guetta, V.; Assali, A.; Halkin, A.; Vaknin-Assa, H.; Segev, A.; Bental, T.; Ben-Shoshan, J.; et al. Temporal trends in transcatheter aortic valve implantation, 2008-2014: Patient characteristics, procedural issues, and clinical outcome. Clin. Cardiol. 2017, 40, 82–88. [Google Scholar] [CrossRef]
- Ben Zadok, O.I.; Kornowski, R.; Finkelstein, A.; Barbash, I.; Danenberg, H.; Segev, A.; Guetta, V.; Halkin, A.; Vaknin, H.; Planer, D.; et al. Temporal Trends in Gender-Related Differences and Outcomes in Patients Who Underwent Transcatheter Aortic Valve Implantation (from the Israeli Transcatheter Aortic Valve Implantation Multicenter Registry). Am. J. Cardiol. 2019, 123, 108–115. [Google Scholar] [CrossRef]
- Frydman, S.; Zahler, D.; Merdler, I.; Freund, O.; Shacham, Y.; Banai, S.; Finkelstein, A.; Steinvil, A. Temporal Trends of Transcatheter Aortic Valve Implantation over 12 Years: A High-Volume Single-Center Experience. J. Clin. Med. 2022, 11, 4962. [Google Scholar] [CrossRef]
- Généreux, P.; Piazza, N.; Alu, M.C.; Nazif, T.; Hahn, R.T.; Pibarot, P.; Bax, J.J.; Leipsic, J.A.; Blanke, P.; Blackstone, E.H.; et al. Valve Academic Research Consortium 3: Updated Endpoint Definitions for Aortic Valve Clinical Research. J. Am. Coll. Cardiol. 2021, 77, 2717–2746. [Google Scholar] [CrossRef]
- Eliav, R.; Elitzur, Y.; Planer, D.; Beeri, R.; Gilon, D.; Shuvy, M.; Luria, D.; Danenberg, H.; Perlman, G.Y. Predictors for permanent pacemaker implantation following transcatheter aortic valve implantation: Trends over the past decade. J. Interv. Card. Electrophysiol. 2020, 62, 299–307. [Google Scholar] [CrossRef] [PubMed]
- Webb, J.G.; Blanke, P.; Meier, D.; Sathananthan, J.; Lauck, S.; Chatfield, A.G.; Jelisejevas, J.; Wood, D.A.; Akodad, M. TAVI in 2022: Remaining issues and future direction. Arch. Cardiovasc. Dis. 2022, 115, 235–242. [Google Scholar] [CrossRef] [PubMed]
- Head, S.J.; Çelik, M.; Kappetein, A.P. Mechanical versus bioprosthetic aortic valve replacement. Eur. Heart J. 2017, 38, 2183–2191. [Google Scholar] [CrossRef] [PubMed]
- Dunning, J.; Gao, H.; Chambers, J.; Moat, N.; Murphy, G.; Pagano, D.; Ray, S.; Roxburgh, J.; Bridgewater, B. Aortic valve surgery: Marked increases in volume and significant decreases in mechanical valve use–an analysis of 41,227 patients over 5 years from the Society for Cardiothoracic Surgery in Great Britain and Ireland National database. J. Thorac. Cardiovasc. Surg. 2011, 142, 776–782.e3. [Google Scholar] [CrossRef] [PubMed]
- Siregar, S.; de Heer, F.; Groenwold, R.H.; Versteegh, M.I.; Bekkers, J.A.; Brinkman, E.S.; Bots, M.L.; van der Graaf, Y.; van Herwerden, L.A. Trends and outcomes of valve surgery: 16-year results of Netherlands Cardiac Surgery National Database. Eur. J. Cardio-Thorac. Surg. 2014, 46, 386–397. [Google Scholar] [CrossRef] [PubMed]
| Years | 2008–2009 | 2010–2011 | 2012–2013 | 2014–2015 | 2016–2017 | 2018–2019 | 2020–2021 |
|---|---|---|---|---|---|---|---|
| Number of patients | 30 | 151 | 148 | 211 | 327 | 366 | 396 |
| Age (years) | 85.1 ± 4 | 83.4 ± 6.9 | 82.3 ± 7.9 | 82.2 ± 7.4 | 82.6 ± 7.4 | 80.3 ± 8.5 | 80.1 ± 6.8 |
| Male, N (%) | 10 (33%) | 71 (47%) | 68 (45.9%) | 110 (52%) | 148 (45%) | 176 (48%) | 214 (54%) |
| STS score (%) | 5.9 ± 4.4 | 5.7 ± 3.37 | 5.9 ± 4.5 | 4.4 ± 2.4 | 4.2 ± 2.85 | 3.1 ± 2.16 | 2.8 ± 3.16 |
| EuroScore II (%) | 4.5 ± 3.1 | 6.2 ± 6.63 | 5.5 ± 6.2 | 5.4 ± 6.8 | 4.1 ± 4.47 | 4.6 ± 22.54 | 2.7 ± 2.43 |
| LVEF (%) | 59.6 + 7.8 | 53 ± 13.4 | 54.6 ± 13.2 | 53.9 ± 12.7 | 55.9 ± 11.8 | 55 ± 12.1 | 54.8 ± 12 |
| AV peak PG (mmHg) * | 87.3 ± 22.7 | 75.3 ± 25.4 | 70.8 ± 23.3 | 66.7 ± 23.3 | 66.9 ± 23.2 | 70.9 ± 48.3 | 67.5 ± 21 |
| AV mean PG (mmHg) * | 55.4 ± 15.1 | 46.1 ± 15.6 | 45 ± 18.2 | 42.9 ± 19.4 | 42 ± 15.1 | 42.6 ± 15 | 42.3 ± 13.9 |
| AVA (cm2) * | 0.63 ± 0.16 | 0.69 ± 0.18 | 0.71 ± 0.21 | 0.74 ± 0.23 | 0.71 ± 0.18 | 0.74 ± 0.19 | 0.73 ± 0.2 |
| BMI | 27.2 ± 4.1 | 28.2 ± 12.7 | 27.2 ± 4.4 | 28 ± 5.4 | 27.9 ± 5.3 | 28.3 ± 5.3 | 28.8 ± 12 |
| Hypertension, N (%) | 26 (86.7%) | 128 (84.8%) | 132 (89.2%) | 165 (78.6%) | 254 (78.4%) | 246 (77%) | 283 (71.6%) |
| GFR (ml/min) | 50 ± 15.9 | 50.4 ± 17.1 | 49.7 ± 19.5 | 58 ± 21.1 | 64 ± 23.5 | 66.5 ± 25.4 | 62.7 ± 24.3 |
| Dialysis, N (%) | 0 | 2 (1.3%) | 3 (2.1%) | 5 (2.4%) | 7 (2.2%) | 4 (1.3%) | 13 (3.3%) |
| Diabetes, N (%) | 12 (40%) | 52 (34.7%) | 56 (38%) | 94 (44.8%) | 118 (36.6%) | 121 (38.3%) | 160 (40.5%) |
| COPD, N (%) | 2 (6.7%) | 25 (16.8%) | 27 (18.4%) | 33 (15.7%) | 19 (5.9%) | 19 (6%) | 23 (5.9%) |
| PVD, N (%) | 3 (10%) | 24 (16.2%) | 21 (14.4%) | 26 (12.3%) | 49 (15.2%) | 24 (9.4%) | 27 (6.9%) |
| CAD, N (%) | 15 (50%) | 91 (61%) | 69 (47%) | 103(48.8%) | 193 (59.8%) | 151 (47.8%) | 173 (44.5%) |
| Previous MI, N (%) * | 6 (20%) | 42 (28.6%) | 45 (31.3%) | 40 (19%) | 98 (31%) | 26 (15.4%) | 36 (20.9%) |
| Previous CABG, N (%) * | 8 (26.7%) | 39 (26.2%) | 28 (19.4%) | 42 (20%) | 78 (24.7%) | 79 (45.7%) | 53 (31%) |
| Previous stroke, N (%) | 5 (16.7%) | 20 (13.5%) | 26 (17.7%) | 33 (15.6%) | 52 (16%) | 26 (8.2%) | 56 (14.3%) |
| History of AF, N (%) | 8 (26.7%) | 40 (26.7%) | 40 (27.4%) | 74 (35.2%) | 94 (29%) | 93 (27.8%) | 101(25.5%) |
| Years | 2008–2009 | 2010–2011 | 2012–2013 | 2014–2015 | 2016–2017 | 2018–2019 | 2020–2021 | p Value |
|---|---|---|---|---|---|---|---|---|
| Number of Patients | 30 | 151 | 148 | 211 | 327 | 366 | 396 | |
| Vascular access | ||||||||
| Transfemoral | 29 (96.7%) | 112 (74.2%) | 111 (75%) | 167 (79%) | 301 (92.3%) | 351 (96.4%) | 376(94.5%) | <0.001 |
| Axillary | 1 (3.3%) | 8 (5.3%) | 10 (6.8%) | 8 (3.8%) | 5 (1.5%) | 1 (0.3%) | 1 (0.3%) | |
| Transapical | 0 | 29 (19.2%) | 27 (18.2%) | 36 (17%) | 20 (6.1%) | 5 (1.4%) | 1 (0.3%) | |
| Direct aortic | 0 | 2 (1.3%) | 0 | 0 | 0 | 0 | 0 | |
| Transcaval | 0 | 0 | 0 | 0 | 0 | 7 (1.9%) | 20 (5%) | |
| Anaesthesia method | ||||||||
| General sedation | 6 (37.5%) | 69 (46.3%) | 44 (29.7%) | 53 (25%) | 29 (8.9%) | 9 (2.5%) | 10 (2.5%) | <0.001 |
| Conscious sedation | 10 (62.5%) | 80 (53.7%) | 104 (70.3%) | 152 (72%) | 290 (88.7%) | 229 (62.7%) | 191(48%) | |
| Conscious converted to general sedation | 0 | 0 | 0 | 6 (2.8%) | 7 (2.1%) | 4 (1.1%) | 5 (1.3%) | |
| No sedation (local only) | 0 | 0 | 0 | 0 | 1 (0.3%) | 123 (33.7%) | 191 (48%) | |
| Balloon pre-dilatation | 25 (83.3%) | 141 (93.4%) | 125 (85%) | 83 (41.3%) | 142 (43.7%) | 158 (43.4%) | 242 (61%) | <0.001 |
| Balloon post-dilatation | 2 (6.7%) | 29 (19.6%) | 26 (17.9%) | 45 (22.6%) | 96 (29.4%) | 104 (28.5%) | 82 (20.8%) | <0.005 |
| Valve-in-valve (VIV) | 0 | 5 (3.3%) | 7 (4.7%) | 9 (4.3%) | 21 (6.5%) | 22 (6%) | 27 (6.8%) | 0.442 |
| Valve type | ||||||||
| CoreValve/Evolute | 30 (100%) | 92 (61.3%) | 74 (50.3%) | 96 (45.9%) | 195 (59.8%) | 186 (51%) | 151 (41.6%) | <0.001 |
| SAPIEN | 0 | 58 (38.7%) | 73 (49.7%) | 112 (53.6%) | 120 (36.8%) | 128 (35%) | 165(45.5%) | |
| ACURATE Neo | 0 | 0 | 0 | 0 | 0 | 44 (12%) | 38 (10.5%) | |
| Portico/Navitor | 0 | 0 | 0 | 1 (0.5%) | 11 (3.4%) | 7 (1.9%) | 9 (2.5%) | |
| Years | 2008–2009 | 2010–2011 | 2012–2013 | 2014–2015 | 2016–2017 | 2018–2019 | 2020–2021 | p Value |
|---|---|---|---|---|---|---|---|---|
| Number of Patients | 30 | 151 | 148 | 211 | 327 | 366 | 396 | |
| TAVR device success rate % (VARC-3) | 100% | 98% | 97.3% | 96.6% | 97.5% | 95% | 95% | 0.261 |
| Need for a second valve | 1 (3.3%) | 7 (4.6%) | 9 (6.2%) | 12 (5.9%) | 8 (2.5%) | 13 (3.5%) | 9 (2.3%) | 0.150 |
| Final perivalvular leak (PVL) (per angiography) | ||||||||
| None | 4 (13.3%) | 44 (29.3%) | 60(42.3%) | 88(45.6%) | 96 (29.9%) | 143 (39.2%) | 195(49.2%) | <0.001 |
| Minimal | 16(53.3%) | 67 (44.7%) | 62 (43.7%) | 67 (34.7%) | 109(34%) | 127 (34.8%) | 123 (31%) | |
| Mild | 10 (33.3%) | 38 (25.3%) | 17 (12%) | 33 (17%) | 103 (32%) | 82 (22.5%) | 76 (19.2%) | |
| Moderate | 0 | 1 (0.7%) | 1 (0.7%) | 4 (2.1%) | 11 (3.4%) | 13 (3.6%) | 2 (0.5%) | |
| Severe | 0 | 0 | 2 (1.4%) | 1 (0.5%) | 2 (0.6%) | 0 | 0 | |
| Vascular or access related non-vascular complication (VARC-3) | ||||||||
| Major | 4 (14.3%) | 7 (4.7%) | 0 | 3 (1.4%) | 14 (4.3%) | 10 (2.8%) | 11 (2.8%) | <0.001 |
| Minor | 8 (28.6%) | 22 (14.7%) | 37 (25.2%) | 51 (24.3%) | 67 (20.6%) | 85 (23.5%) | 69 (17.3%) | |
| Bleeding | ||||||||
| Bleeding minor (Type 1) | 3 (10%) | 16 (10.6%) | 16 (10.8%) | 29 (13.8%) | 37 (12%) | 54 (17%) | 45 (11.4%) | <0.005 |
| Bleeding major (Type 2) | 4 (13.3%) | 10 (6.6%) | 9 (6%) | 9 (4.3%) | 14 (4.5%) | 8 (2.5%) | 5 (1.3%) | |
| Life-threatening/disabling (Type 3–4) | 3 (10%) | 5 (3.3%) | 3 (2%) | 5 (2.4%) | 7 (2.3%) | 6 (1.9%) | 8 (2%) | |
| Stroke | ||||||||
| Ischaemic stroke/TIA | 1 (3.3%) | 6 (4%) | 4 (2.7%) | 9 (4.3%) | 5 (1.6%) | 13 (4%) | 7 (1.8%) | 0.314 |
| Haemorrhagic stroke | 0 | 0 | 0 | 1 (0.5%) | 0 | 0 | 0 | |
| New AVB | ||||||||
| First-degree AVB * | 1 (10%) | 0 | 1 (3%) | 1 (1.5%) | 1 (0.6%) | 21 (6.7%) | 46 (11.7%) | <0.001 |
| Second-degree AVB * | 0 | 0 | 0 | 0 | 3 (1.8%) | 3 (1%) | 8 (2%) | |
| CAVB * | 8 (80%) | 26 (57.8%) | 17 (51.5%) | 33 (49.3%) | 50 (29.6%) | 50 (15.9%) | 47 (11.9%) | |
| New permanent PPM | 14 (46.7%) | 46(30.9%) | 33 (22.3%) | 48 (22.7%) | 69 (21%) | 80 (21.9%) | 71 (17.8%) | <0.001 |
| New LBBB | 8 (27.6%) | 34 (23%) | 36 (24.3%) | 54 (25.7%) | 83 (25.5%) | 78 (21.8%) | 101(25.6%) | 0.883 |
| AKI (VARC-3) | ||||||||
| Stage 1 | 7 (24%) | 28 (18.7%) | 25 (16.9%) | 28 (13.4%) | 22 (7%) | 34 (10.8%) | 30 (7.6%) | <0.001 |
| Stage 2 | 0 | 9 (6%) | 2 (1.4%) | 12 (5.7%) | 16 (5.2%) | 8 (2.5%) | 7 (1.8%) | |
| Stage 3 | 0 | 1 (0.7%) | 4 (2.7%) | 4 (1.9%) | 15 (4.8%) | 8 (2.5%) | 9 (2.3%) | |
| Cardiac tamponade | 3 (10%) | 5 (3.3%) | 3 (2%) | 3 (1.4%) | 5 (1.5%) | 4 (1.1%) | 6 (1.5%) | <0.05 |
| Conversion to open surgery | 0 | 3 (2%) | 0 | 2 (0.9%) | 3 (0.9%) | 2 (0.5%) | 1 (0.3%) | 0.338 |
| Valve mal-position | 1 (3.3%) | 9 (6%) | 6 (4.1%) | 7 (3.3%) | 2 (0.6%) | 2 (0.5%) | 4 (1%) | <0.001 |
| Valve migration/embolisation | 1 (3.3%) | 5 (3.3%) | 5 (3.4%) | 6 (2.8%) | 3 (0.9%) | 1 (0.3%) | 3 (0.8%) | <0.05 |
| Peri-procedure MI (till 72 h) | 0 | 3 (2%) | 7 (4.7%) | 1 (0.5%) | 4 (1.2%) | 1 (0.3%) | 8 (2%) | <0.01 |
| In-hospital HF | 10 (34.5%) | 21 (14.8%) | 12 (8.2%) | 32 (15.6%) | 16 (5.2%) | 22 (7%) | 16 (4%) | <0.001 |
| Days from TAVR till discharge | 5.99 [4.9–6.2] | 5.99 [4.9–9.9] | 5.9 [3.9–7.9] | 4.9 [3.9–7.9] | 3.9 [2.9–5.9] | 3.9 [2.9–5.9] | 3.9 [2.9–5.9] | - |
| Mortality | ||||||||
| Thirty-day mortality | 3 (10%) | 7 (4.6%) | 8 (5.4%) | 5 (2.4%) | 11 (3.4%) | 8 (2.2%) | 7 (1.8%) | <0.05 |
| One-year mortality | 3 (10%) | 29 (19.2%) | 20 (13.5%) | 28 (13.3%) | 36 (11%) | 33 (9%) | 33 (8.3%) | <0.01 |
| Two-year mortality | 6 (20%) | 43 (28.5%) | 29 (19.6%) | 50 (23.7%) | 61 (18.7%) | 66 (18%) | 72 (18.1%) | 0.095 |
| (A) | HR | 95% CI | p Value |
| 2008–2011 | Reference | Reference | Reference |
| 2012–2015 | 0.736 | [0.47–1.15] | 0.178 |
| 2016–2019 | 0.537 | [0.35–0.81] | 0.004 |
| 2020–2021 | 0.444 | [0.27–0.72] | 0.001 |
| (B) | HR | 95% CI | p Value |
| 2008–2011 | Reference | Reference | Reference |
| 2012–2015 | 0.68 | [0.41–1.12] | 0.126 |
| 2016–2019 | 0.68 | [0.44–1.07] | 0.093 |
| 2020–2021 | 0.61 | [0.37–1.01] | 0.056 |
| STS score | 1.09 | [1.07–1.11] | <0.001 |
| Stage 2–3 AKI | 3.42 | [2.18–5.38] | <0.001 |
| Major bleeding | 2.26 | [1.41–3.63] | 0.001 |
| Stroke | 3.51 | [1.93–6.39] | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Karra, N.; Sharon, A.; Massalha, E.; Fefer, P.; Maor, E.; Guetta, V.; Ben-Zekry, S.; Kuperstein, R.; Matetzky, S.; Beigel, R.; et al. Temporal Trends in Patient Characteristics and Clinical Outcomes of TAVR: Over a Decade of Practice. J. Clin. Med. 2024, 13, 5027. https://doi.org/10.3390/jcm13175027
Karra N, Sharon A, Massalha E, Fefer P, Maor E, Guetta V, Ben-Zekry S, Kuperstein R, Matetzky S, Beigel R, et al. Temporal Trends in Patient Characteristics and Clinical Outcomes of TAVR: Over a Decade of Practice. Journal of Clinical Medicine. 2024; 13(17):5027. https://doi.org/10.3390/jcm13175027
Chicago/Turabian StyleKarra, Nour, Amir Sharon, Eias Massalha, Paul Fefer, Elad Maor, Victor Guetta, Sagit Ben-Zekry, Rafael Kuperstein, Shlomi Matetzky, Roy Beigel, and et al. 2024. "Temporal Trends in Patient Characteristics and Clinical Outcomes of TAVR: Over a Decade of Practice" Journal of Clinical Medicine 13, no. 17: 5027. https://doi.org/10.3390/jcm13175027
APA StyleKarra, N., Sharon, A., Massalha, E., Fefer, P., Maor, E., Guetta, V., Ben-Zekry, S., Kuperstein, R., Matetzky, S., Beigel, R., Segev, A., & Barbash, I. M. (2024). Temporal Trends in Patient Characteristics and Clinical Outcomes of TAVR: Over a Decade of Practice. Journal of Clinical Medicine, 13(17), 5027. https://doi.org/10.3390/jcm13175027






