Current Status of the Management of Idiopathic Condylar Resorption/Progressive Condylar Resorption—A Scoping Review
Abstract
1. Introduction
2. Methods
2.1. Search Strategy
2.2. Study Selection
3. Results
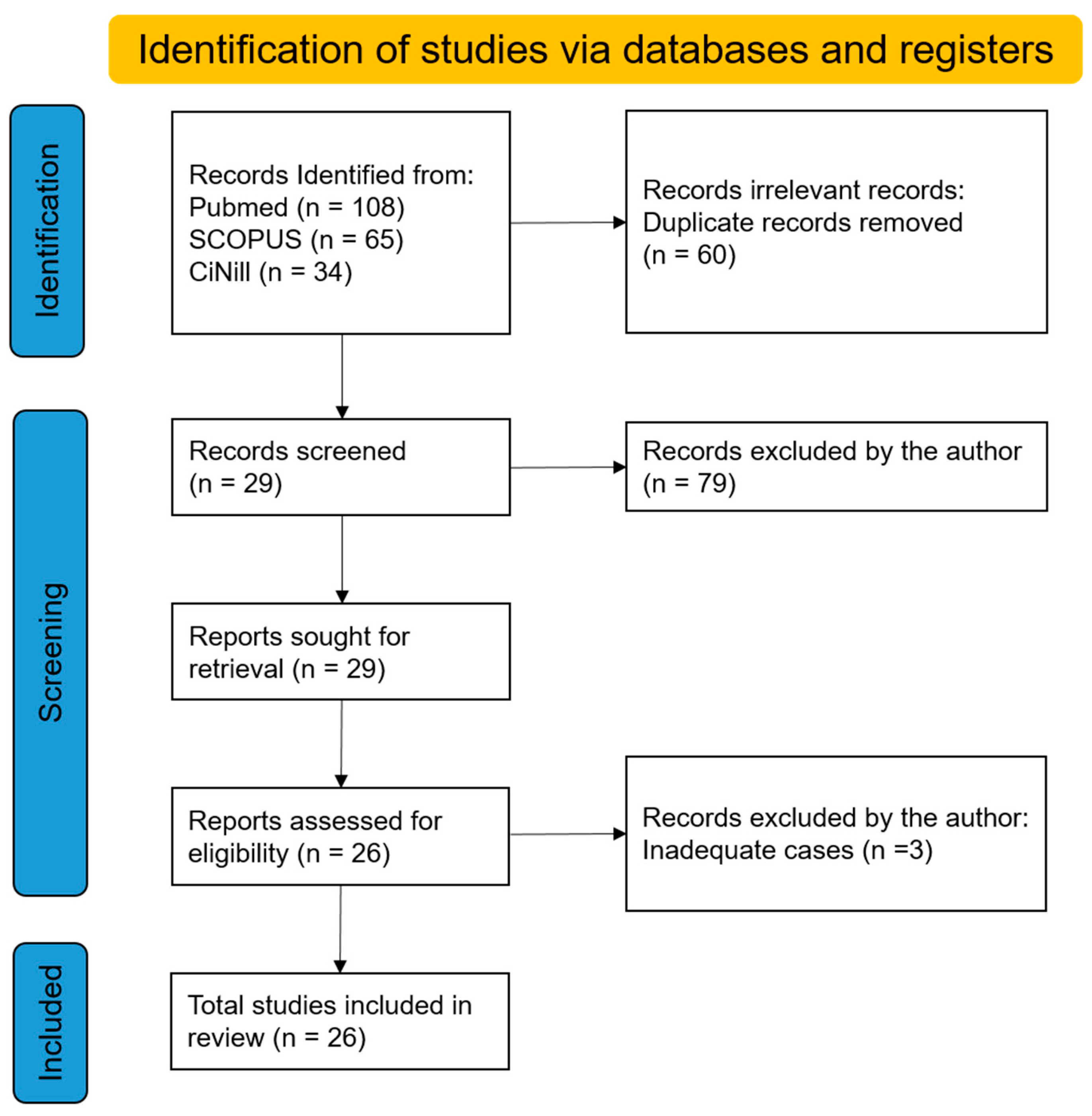
3.1. Search Results
3.2. Confirmation of ICR/PCR Stability
3.3. Management of ICR/PCR
3.4. Non-Surgical Management
3.5. Orthognathic Surgery
3.6. Total Joint Reconstruction
4. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Handelman, C.S.; Greene, C.S. Progressive/Idiopathic condylar resorption: An orthodontic perspective. Semin. Orthod. 2013, 19, 55–70. [Google Scholar] [CrossRef]
- Arnett, G.W.; Gunson, M.J. Risk factors in the initiation of condylar resorption. Semin. Orthod. 2013, 19, 81–88. [Google Scholar] [CrossRef]
- Sarver, D.M.; Janyavula, S.; Cron, R.Q. Condylar degeneration and diseases–Local and systemic etiologies. Semin. Orthod. 2013, 19, 89–96. [Google Scholar] [CrossRef]
- Tanaka, E.; Detamore, M.S.; Mercuri, L. Degenerative disorders of the temporomandibular joint: Etiology, diagnosis, and management. J. Dent. Res. 2008, 87, 296–307. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, E.; Koolstra, J.H. Biomechanics of the temporomandibular joint. J. Dent. Res. 2008, 87, 989–991. [Google Scholar] [CrossRef] [PubMed]
- Hatcher, D.C. Progressive condylar resorption: Pathologic processes and imaging considerations. Semin. Orthod. 2013, 19, 97–105. [Google Scholar] [CrossRef]
- Gallo, L.M.; Chiaravalloti, G.; Iwasaki, L.R.; Nickel, J.C.; Palla, S. Mechanical work during stress-field translation in the human TMJ. J. Dent. Res. 2006, 85, 1006–1010. [Google Scholar] [CrossRef] [PubMed]
- Hashem, G.; Zhang, Q.; Hayami, T.; Chen, J.; Kapila, S. Relaxin and β-estradiol modulate targeted matrix degradation in specific synovial joint fibrocartilages: Progesterone prevents matrix loss. Arthritis Res. Ther. 2006, 8, R98. [Google Scholar] [CrossRef] [PubMed]
- Gunson, M.J.; Arnett, G.W.; Formby, B.; Falzone, C.; Mathur, R.; Alexander, C. Oral contraceptive pill use and abnormal menstrual cycles in women with severe condylar resorption: A case for low serum 17beta-estradiol as a major factor in progressive condylar resorption. Am. J. Orthod. Dentofac. Orthop. 2009, 136, 772–779. [Google Scholar] [CrossRef]
- Ye, T.; Sun, D.; Mu, T.; Chu, Y.; Miao, H.; Zhang, M.; Yang, H.; Liu, Q.; Lu, L.; Xing, X.; et al. Differential effects of high-physiological oestrogen on the degeneration of mandibular condylar cartilage and subchondral bone. Bone 2018, 111, 9–22. [Google Scholar] [CrossRef]
- Park, Y.; Chen, S.; Ahmad, N.; Hayami, T.; Kapila, S. Estrogen selectively enhances TMJ disc but not knee meniscus matrix loss. J. Dent. Res. 2019, 98, 1532–1538. [Google Scholar] [CrossRef]
- Ahmad, N.; Chen, S.; Wang, W.; Kapila, S. 17β-estradiol induces MMP-9 and MMP-13 in TMJ fibrochondrocytes via estrogen receptor α. J. Dent. Res. 2019, 97, 1023–1030. [Google Scholar] [CrossRef] [PubMed]
- Milam, S.B. TMJ osteoarthritis. In Temporomandibular Disorders: An Evidence-Based Approach to Diagnosis and Treatment; Laskin, D.M., Greene, C.S., Hylander, W.L., Eds.; Quintessence: Chicago, IL, USA, 2006; pp. 105–123. [Google Scholar]
- Mehra, P.; Nadershah, M.; Chigurupati, R. Is alloplastic temporomandibular joint reconstruction a viable option in the surgical management of adult patients with idiopathic condylar resorption? J. Oral Maxillofac. Surg. 2016, 74, 2044–2054. [Google Scholar] [CrossRef] [PubMed]
- Merkx, M.A.; Van Damme, P.A. Condylar resorption after orthognathic surgery. Evaluation of management in 8 patients. J. Craniomaxillofac. Surg. 1994, 22, 53–58. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.L.; Pogrel, M.A.; Kaban, L.B. Diagnosis and management of condylar resorption. J. Oral Maxillofac. Surg. 1997, 55, 114–119. [Google Scholar] [CrossRef] [PubMed]
- Hoppenreijs, T.J.; Stoelinga, P.J.W.; Grace, K.L.; Robben, C.M.G. Long-term evaluation of patients with progressive condylar resorption following orthognathic surgery. Int. J. Oral Maxillofac. Surg. 1999, 28, 411–418. [Google Scholar] [CrossRef] [PubMed]
- Troulis, M.J.; Williams, W.B.; Kaban, L.B. Endoscopic mandibular condylectomy and reconstruction: Early clinical results. J. Oral Maxillofac. Surg. 2004, 62, 460–465. [Google Scholar] [CrossRef] [PubMed]
- Mercuri, L.G. A rationale for total alloplastic temporomandibular joint reconstruction in the management of idiopathic/progressive condylar resorption. J. Oral Maxillofac. Surg. 2007, 65, 1600–1609. [Google Scholar] [CrossRef] [PubMed]
- Schendel, S.A.; Tulasne, J.F.; Linck, D.W., 3rd. Idiopathic condylar resorption and micrognathia: The case for distraction osteogenesis. J. Oral Maxillofac. Surg 2007, 65, 1610–1616. [Google Scholar] [CrossRef]
- Troulis, M.J.; Tayebaty, F.T.; Papadaki, M.; Williams, W.B.; Kaban, L.B. Condylectomy and costochondral graft reconstruction for management of active idiopathic condylar resorption. J. Oral Maxillofac. Surg. 2008, 66, 65–72. [Google Scholar] [CrossRef]
- Qiu, Y.T.; Yang, C.; Chen, M.J. Endoscopically assisted reconstruction of the mandibular condyle with a costochondral graft through a modified preauricular approach. Br. J. Oral Maxillofac. Surg. 2010, 48, 443–447. [Google Scholar] [CrossRef] [PubMed]
- Chung, C.J.; Choi, Y.J.; Kim, I.S.; Huh, J.K.; Kim, H.G.; Kim, K.H. Total alloplastic temporomandibular joint reconstruction combined with orthodontic management in a patient with idiopathic condylar resorption. Am. J. Orthod. Dentofac. Orthop. 2011, 140, 404–417. [Google Scholar] [CrossRef] [PubMed]
- You, M.S.; Yang, H.J.; Hwang, S.J. Postoperative functional remodeling of preoperative idiopathic condylar resorption: A case report. J. Oral Maxillofac. Surg. 2011, 69, 1056–1063. [Google Scholar] [CrossRef]
- Alexander, R. Idiopathic condylar resorption. N. Y. State. Dent. J. 2012, 78, 22–25. [Google Scholar]
- Kau, C.H.; Bejemir, M.P. Application of virtual three-dimensional surgery planning in management of open bite with idiopathic condylar resorption. Ann. Maxillofac. Surg. 2015, 5, 249–254. [Google Scholar] [CrossRef] [PubMed]
- Nakamura, M.; Yanagita, T.; Matsumura, T.; Yamashiro, T.; Ida, S.; Kamioka, H. A case of severe mandibular retrognathism with bilateral condylar deformities treated with Le Fort I osteotomy and two advancement genioplasty procedures. Korean J. Orthod. 2016, 46, 395–408. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Alsabban, L.; Amarista, F.J.; Mercuri, L.G.; Perez, D. Idiopathic condylar resorption: A survey and review of the literature. J. Oral Maxillofac. Surg. 2018, 76, 2316.e1–2316.e13. [Google Scholar] [CrossRef] [PubMed]
- Rahman, F.; Celebi, A.A.; Loius, P.J.; Kau, C.H. A comprehensive management approach for idiopathic condylar resorption and anterior open bite with 3D virtual surgical planning and self-ligated customized lingual appliance. Am. J. Orthod. Dentofac. Orthop. 2019, 155, 560–571. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Veiszenbacher, E.; Waite, P.D.; Kau, C.H. Comprehensive management approach for bilateral idiopathic condylar resorption and anterior open bite with customized lingual braces and total joint prostheses. Am. J. Orthod. Dentofac. Orthop. 2019, 156, 125–136. [Google Scholar] [CrossRef]
- Lee, G.H.; Park, J.H.; Lee, S.M.; Moon, D.N. Orthodontic management protocols for patients with idiopathic condylar resorption. J. Clin. Pediatr. Dent. 2019, 43, 292–303. [Google Scholar] [CrossRef]
- Peacock, Z.S.; Lee, C.C.Y.; Troulis, M.J.; Kaban, L.B. Long-term stability of condylectomy and costochondral graft reconstruction for management of idiopathic condylar resorption. J. Oral Maxollofac. Surg. 2019, 77, 792–802. [Google Scholar] [CrossRef] [PubMed]
- Chamberland, S. Progressive idiopathic condylar resorption: Three case reports. Am. J. Orthod. Dentofac. Orthop. 2019, 156, 531–544. [Google Scholar] [CrossRef] [PubMed]
- Galiano, A.; Wolford, L.; Goncalves, D.J.; Goncalves, D. Adolescent internal condylar resorption (AICR) of the temporomandibular joint can be successfully treated by disk repositioning and orthognathic surgery, part 2: Management outcomes. Cranio. J. Craniomandib. Pract. 2019, 37, 111–120. [Google Scholar]
- Mercuri, L.G.; Handelman, C.S. Idiopathic Condylar Resorption: What Should We Do? Oral Maxillofac. Surg. Clin. N. Am. 2020, 32, 105–116. [Google Scholar] [CrossRef] [PubMed]
- Zhou, J.; Fu, Y.; Yu, L.; Li, Z.; Chen, S. A novel three-dimensional morphological analysis of idiopathic condylar resorption following stabilization splint management. J. Oral Rehabil. 2021, 48, 560–567. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Xue, C.; Dai, W.; Shu, R. Three-dimensional surgical guide approach to correcting skeletal Class II malocclusion with idiopathic condylar resorption. Angle Orthod. 2021, 91, 399–415. [Google Scholar] [CrossRef] [PubMed]
- Noh, H.K.; Park, H.S. Considerations for vertical control with microimplants in an idiopathic condylar resorption patient: A case report. J. Orthod. 2021, 48, 172–182. [Google Scholar] [CrossRef] [PubMed]
- Mao, B.; Tian, Y.; Li, J.; Zhou, Y.; Wang, X. A quantitative analysis of facial changes after orthodontic management with vertical control in patients with idiopathic condylar resorption. Orthod. Craniofac. Res. 2023, 26, 402–444. [Google Scholar] [CrossRef]
- Fahey, F.H.; Abramson, Z.R.; Padwa, B.L.; Zimmerman, R.E.; Zurakowski, D.; Nissenbaum, M.; Kaban, L.B.; Treves, S.T. Use of (99m)Tc-MDP SPECT for assessment of mandibular growth: Development of normal values. Eur. J. Nucl. Med. Mol. Imaging. 2010, 37, 1002–1010. [Google Scholar] [CrossRef]
- Munakata, K.; Miyashita, H.; Nakahara, T.; Shiba, H.; Sugahara, K.; Katakura, A.; Nakagawa, T. The use of SPECT/CT to access resorptive activity in mandibular condyles. Int. J. Oral Maxillofac. Surg. 2022, 51, 942–948. [Google Scholar] [CrossRef]
- Riechmann, M.; Schmidt, C.; Ahlers, M.O.; Feurer, I.; Kleinheinz, J.; Kolk, A.; Pautke, C.; Schon, A.; Teschke, M.; Toferer, A.; et al. Controversial Aspect of Diagnostics and Therapy of Idiopathic Condylar Resorption: An Analysis of Evidence- and Consensus-Based Recommendations Based on an Interdisciplinary Guideline Project. J. Clin. Med. 2023, 12, 4946. [Google Scholar] [CrossRef] [PubMed]
- Valladares-Neto, J.; Acioli, G.M.R.; Teodoro, A.B.; Evangelista, K.; Furquim, B.D.; Silva, M.A.G. Conservative and minimally invasive approaches to control idiopathic condylar resorption: A scoping review. Int. J. Oral Maxillofac. Surg. 2023, 52, 1188–1196. [Google Scholar] [CrossRef]
- Cevidanes, L.H.; Hajati, A.K.; Paniagua, B.; Lim, P.F.; Walker, D.G.; Palconet, G.; Nackley, A.G.; Styner, M.; Ludlow, J.B.; Zhu, H.; et al. Quantification of condylar resorption in temporomandibular joint osteoarthritis. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2010, 110, 110–117. [Google Scholar] [CrossRef] [PubMed]
- Bremke, M.; Luers, J.C.; Stenner, M.; Bovenschulte, H.; Dorn, F.; Unkel, C.; Hollering, J.; Beutner, D. Radiologic examinations in human temporal bone specimens using digital volume tomography and high-resolution computed tomography after implantation of middle ear prosthesis and cochlear implant electrode array. Otol. Neurotol. 2013, 34, 1321–1328. [Google Scholar] [CrossRef] [PubMed]
- Kyriakou, Y.; Kolditz, D.; Langner, O.; Krause, J.; Kalender, W. Digital volume tomography (DVT) and multislice spiral CT (MSCT): An objective examination of dose and image quality. Rofo 2011, 183, 144–153. [Google Scholar] [CrossRef] [PubMed]
- Hilgenberg-Sydney, P.B.; Bonotto, D.V.; Stechman-Neto, J.; Zwir, L.F.; Pachêco-Pereira, C.; Canto, G.L.; Porporatti, A.L. Diagnostic validity of CT to access degenerative temporomandibular joint disease: A systematic review. Dentomaxillofac. Radiol. 2018, 47, 20170389. [Google Scholar] [CrossRef] [PubMed]
- Ibald, L.C.; Witte, V.; Klawonn, F.; Conrad, R.; Mucke, M.; Sellin, J.; Techke, M. Suggestion of a new standard in measuring the mandible via MRI and an overview of reference values in young women. Oral Maxillofac. Surg. 2024, 28, 373–383. [Google Scholar] [CrossRef] [PubMed]
- He, Z.; Ji, H.; Du, W.; Xu, C.; Luo, E. Management of condylar resorption before or after orthognathic surgery: A systematic review. J. Craniomaxillofac. Surg. 2019, 47, 1007–1014. [Google Scholar] [CrossRef] [PubMed]
- Gunson, M.J.; Arnett, G.W.; Milam, S.B. Pathophysiology and pharmacologic control of osseous mandibular condylar resorption. J. Oral Maxillofac. Surg. 2012, 70, 1918–1934. [Google Scholar] [CrossRef]
- Wolford, L.M.; Cardenas, L. Idiopathic condylar resorption: Diagnosis, management protocol, and outcomes. Am. J. Orthod. Dentofac. Orthop. 1999, 116, 667–677. [Google Scholar] [CrossRef]
- Matsuki, Y.; Hiasa, M.; Hanawa, S.; Nakagawa, M.; Horiuchi, S.; Tanaka, E. A case of anterior open bite associated with idiopathic condylar resorption treated with miniscrew-assisted orthodontics. AJO-DO Clin. Comp. 2024, 4, 211–228. [Google Scholar] [CrossRef]
- Hylander, W.L. The human mandible: Lever or link? Am. J. Phys. Anthropol. 1975, 43, 227–242. [Google Scholar] [CrossRef] [PubMed]
- Taylor, R.M. Nonlever action of the mandible. Am. J. Phys. Anthropol. 1986, 70, 417–421. [Google Scholar] [CrossRef] [PubMed]
- Al-Rezami, K.F.; Abotaleb, B.M.; Alkebsi, K.; Wang, R.; Al-Nasri, A.; Sakran, K.; Aladimi, M.; Yang, P. Long-term three-dimensional condylar remodeling during presurgical orthodontics and after orthognathic surgery of mandibular retrognathia with high mandibular plane angle. Clin. Oral Investig. 2022, 26, 7253–7263. [Google Scholar] [CrossRef] [PubMed]
- Fields, R.T., Jr.; Cardenas, L.E.; Wolford, L.M. The pullout force for Mitek mini and micro suture anchor systems in human mandibular condyles. J. Oral Maxillofac. Surg. 1997, 55, 483–487. [Google Scholar] [CrossRef] [PubMed]
- Fields, R.T., Jr.; Wolford, L.M. The osseointegration of Mitek mini anchors in the mandibular condyle. J. Oral Maxillofac. Surg. 2001, 59, 1402–1406. [Google Scholar] [CrossRef] [PubMed]
- Mehra, P.; Wolford, L.M. The Mitek mini anchor for TMJ disc repositioning: Surgical technique and results. Int. J. Oral Maxillofac. Surg. 2001, 30, 497–503. [Google Scholar] [CrossRef] [PubMed]
- Wolford, L.M.; Reiche-Fischel, O.; Mehra, P. Changes in temporomandibular joint dysfunction after orthognathic surgery. J. Oral Maxillofac. Surg. 2003, 61, 655–660. [Google Scholar] [CrossRef] [PubMed]
- Gonçalves, J.R.; Cassano, D.S.; Wolford, L.M.; Santos-Pinto, A.; Marquez, I.M. Postsurgical stability of counterclockwise maxillomandibular advancement surgery: Affect of articular disc repositioning. J. Oral Maxillofac. Surg. 2008, 66, 724–738. [Google Scholar] [CrossRef]
- Abrahamsson, C.; Ekberg, E.; Henrikson, T.; Nilner, M.; Sunzel, B.; Bondemark, L. TMD in consecutive patients referred for orthognathic surgery. Angle Orthod. 2009, 79, 621–627. [Google Scholar] [CrossRef]
- Kaban, L.B.; Perrott, D.H.; Fisher, K. A protocol for management of temporomandibular joint ankyloses. J. Oral Maxillofac. Surg. 1990, 48, 1145–1151. [Google Scholar] [CrossRef] [PubMed]
- Guyuron, B.; Lasa, C.I., Jr. Unpredictable growth pattern of costochondral graft. Plast. Reconstr. Surg. 1992, 90, 880–886. [Google Scholar] [CrossRef] [PubMed]
- Siavosh, S.; Ali, M. Overgrowth of a costochondral graft in a case of temporomandibular joint ankyloses. J. Craniofac. Surg. 2007, 18, 1488–1491. [Google Scholar] [CrossRef] [PubMed]
- Medra, A.M.M. Follow up of mandibular costochondral grafts after release of ankylosis of the temporomandibular joints. Br. J. Oral Maxillofac. Surg. 2005, 43, 118–122. [Google Scholar] [CrossRef]
- Mercuri, L.G.; Swift, J.Q. Considerations for the use of alloplastic temporomandibular joint replacement in the growing patient. J. Oral Maxillofac. Surg. 2009, 67, 1979–1990. [Google Scholar] [CrossRef]
| Authors | Year | Country | Number | Management Method | Follow-Up | Major Results of Patients |
|---|---|---|---|---|---|---|
| Merkx et al. [15] | 1994 | The Netherlands | 8 | Orthognathic surgery | 3.5 mo.–3 yr. | Revision surgery for treatment of ICR was unsatisfactory with poor esthetics and poor occlusal stability. |
| Huang et al. [16] | 1997 | USA | 22 | Condylectomy and CCG (5) or orthognathic surgery (18) | 2 yr. | Condylectomy and CCG appeared to produce stable and functional results, during a short-term period, while orthognathic surgery might be associated with complication rate. |
| Hoppenreijs et al. [17] | 1999 | The Netherlands | 26 | Non-surgical therapies (13) or orthognathic surgery (13) | 94 mo. for non-surgery; 58 mo. for surgery | 13 patients treated with non-surgery showed satisfactory results, while 7 out of 13 patients treated with second surgery exhibited good results but the remaining 6 showed a considerable relapse. |
| Troulis et al. [18] | 2004 | USA | 7 | Endoscopic condylectomy and CCG | 17 mo. (8–38 mo.) | Endoscopic condylectomy and CCG produce satisfactory clinical outcomes without significant morbidity in a short term period. |
| Mercuri [19] | 2007 | USA | 8 | Alloplastic TMJ reconstruction | Over 4 yr. | Total 5 of 8 ICR patients received TMJ reconstruction with a long term stability. |
| Schendel et al. [20] | 2007 | USA | 1 | Mandibular distraction osteogenesis | 4 yr. | Mandibular osseodistraction produces stable results and no reactivation of ICR with a long-term stability. |
| Troulis et al. [21] | 2008 | USA | 15 | Condylectomy and CCG | Min. 12 mo. | A stable and satisfactory outcome is achievable in patients with active ICR treated by condylectomy and CCG reconstruction. |
| Qiu et al. [22] | 2010 | China | 12 | Reconstruction of the mandible with CCG | Min. 6 mo. | Patients with ICR had successful reconstruction of the condyle with endoscopic CCG. |
| Chung et al. [23] | 2011 | Republic of Korea | 1 | Alloplastic TMJ reconstruction | 1 yr. | Total alloplastic joint reconstruction and counterclockwise rotation of maxillomandibular complex provided a satisfying outcome. |
| You et al. [24] | 2011 | Republic of Korea | 1 | Orthognathic surgery (Two-jaw surgery) | 3 yr. | The case showed functional remodelling of the condyle in preoperative ICR. |
| Alexander [25] | 2012 | USA | 1 | Alloplastic joint reconstruction | 16 yr. | The case treated with a single-stage surgery with alloplast with a 16-year follow-up. |
| Kau and Bejemir [26] | 2015 | USA | 1 | Orthognathic surgery (iliac bone graft with inverted L-osteotomy) | 1 yr. | A segmental Le-Fort I osteotomy and inverted L-osteotomy with iliac bone grafting led to resolve functional, esthetic, and pain concerns to a satisfactory level. |
| Mehra et al. [14] | 2016 | USA | 21 | Alloplastic joint reconstruction | 6.2 yr. (5–12 yr.) | Use of alloplastic joint prostheses allows for the execution of large mandibular advancements in a predictable and accurate manner with a meaningful decrease in symptoms of TMJ dysfunction. |
| Nakamura et al. [27] | 2016 | Japan | 1 | Maxillary osteotomy alone | 30 mo. | Mild ICR patient can be effectively treated without surgical mandibular advancement. |
| Alsabban et al. [28] | 2018 | USA | 1 | Alloplastic joint reconstruction | 17 mo. | As a single surgery, treatment with total joint reconstruction showed stable result. |
| Rahman et al. [29] | 2019 | USA | 1 | Alloplastic joint reconstruction | 0 mo. | A patient with bilateral ICR was treated with total joint replacement and orthodontic-orthognathic surgery. |
| Wang et al. [30] | 2019 | USA | 1 | Alloplastic joint reconstruction | 0 mo. | A patient with bilateral ICR was treated with total joint replacement and orthodontic-orthognathic surgery. |
| Lee et al. [31] | 2019 | Republic of Korea | 1 | Orthodontic treatment after stabilization splint | 2 yr. | After stabilization splint therapy, orthodontic treatment with TADs achieved an acceptable occlusion and facial esthetics. |
| Peacock et al. [32] | 2019 | USA | 25 | Endoscopic condylectomy and CCG | At least 3 yr. | Stable and predictable long-term outcomes can be achieved using endoscopic condylectomy and CCG for treatment of active ICR. |
| Chamberland [33] | 2019 | Canada | 3 | Alloplastic joint reconstruction | 0.5–1 mo. | Two ICR patients after orthodontic treatment was managed by total joint replacement. |
| Galiano et al. [34] | 2019 | Brazil | 24 | Orthognathic surgery with disc repositioning | 30.3 mo. | Adolescent condylar resorption can be successfully treated with disc repositioning and orthognathic surgery. |
| Mercuri and Handelman [35] | 2020 | USA | 15 | Total joint replacement | 6 yr. | Among 15 patients with ICR/PCR, 12 patients underwent alloplastic TMJ replacement, and 11 out of 12 patients showed stable result. Among the remaining three, two patients refused treatment, and one showed PCR after occlusal appliance therapy. |
| Zhou et al. [36] | 2021 | China | 42 | Splint therapy | Min. 6 mo. | The anabolic modelling tendency of the condylar surface p was greater in the stabilization splint group than in the control group. The stabilization splint therapy effectively reduced further bone destruction and promoted condylar modeling. |
| Wang et al. [37] | 2021 | China | 1 | Orthognathic surgery (BSRO and genioplasty) | 1 yr. | Facial appearance and occlusion improved significantly, and a stable result was obtained with a 1-year follow-up. |
| Noh and Park [38] | 2021 | Republic of Korea | 1 | Orthodontic treatment with TADs | 2 yr. | Counterclockwise mechanics not only improved facial esthetics but were also suitable for condylar unloading. |
| Mao et al. [39] | 2022 | China | 19 | Orthodontic treatment with TADs | 0 | Orthodontic treatment with TADs resulted 2.27° counterclockwise mandibular rotation. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tanaka, E.; Mercuri, L.G. Current Status of the Management of Idiopathic Condylar Resorption/Progressive Condylar Resorption—A Scoping Review. J. Clin. Med. 2024, 13, 3951. https://doi.org/10.3390/jcm13133951
Tanaka E, Mercuri LG. Current Status of the Management of Idiopathic Condylar Resorption/Progressive Condylar Resorption—A Scoping Review. Journal of Clinical Medicine. 2024; 13(13):3951. https://doi.org/10.3390/jcm13133951
Chicago/Turabian StyleTanaka, Eiji, and Louis G. Mercuri. 2024. "Current Status of the Management of Idiopathic Condylar Resorption/Progressive Condylar Resorption—A Scoping Review" Journal of Clinical Medicine 13, no. 13: 3951. https://doi.org/10.3390/jcm13133951
APA StyleTanaka, E., & Mercuri, L. G. (2024). Current Status of the Management of Idiopathic Condylar Resorption/Progressive Condylar Resorption—A Scoping Review. Journal of Clinical Medicine, 13(13), 3951. https://doi.org/10.3390/jcm13133951







