A 1RM Strengthening and Exercise Programme for the Treatment of Knee Osteoarthritis: A Quality-Improvement Study
Abstract
1. Introduction
2. Methods
2.1. Context
2.2. Intervention
2.2.1. Participants
2.2.2. Delivery
2.2.3. Exercise Prescription
2.3. Motivation Strategies
2.4. Fidelity
2.5. Adherence
2.6. Study of the Intervention
2.7. Measures
2.7.1. One Repetition Max (1RM) Testing
2.7.2. EQ-5D-5L
2.7.3. The Patient-Specific Function Scale (PSFS)
2.7.4. The Oxford Knee Score
2.8. Analysis
3. Ethical Considerations
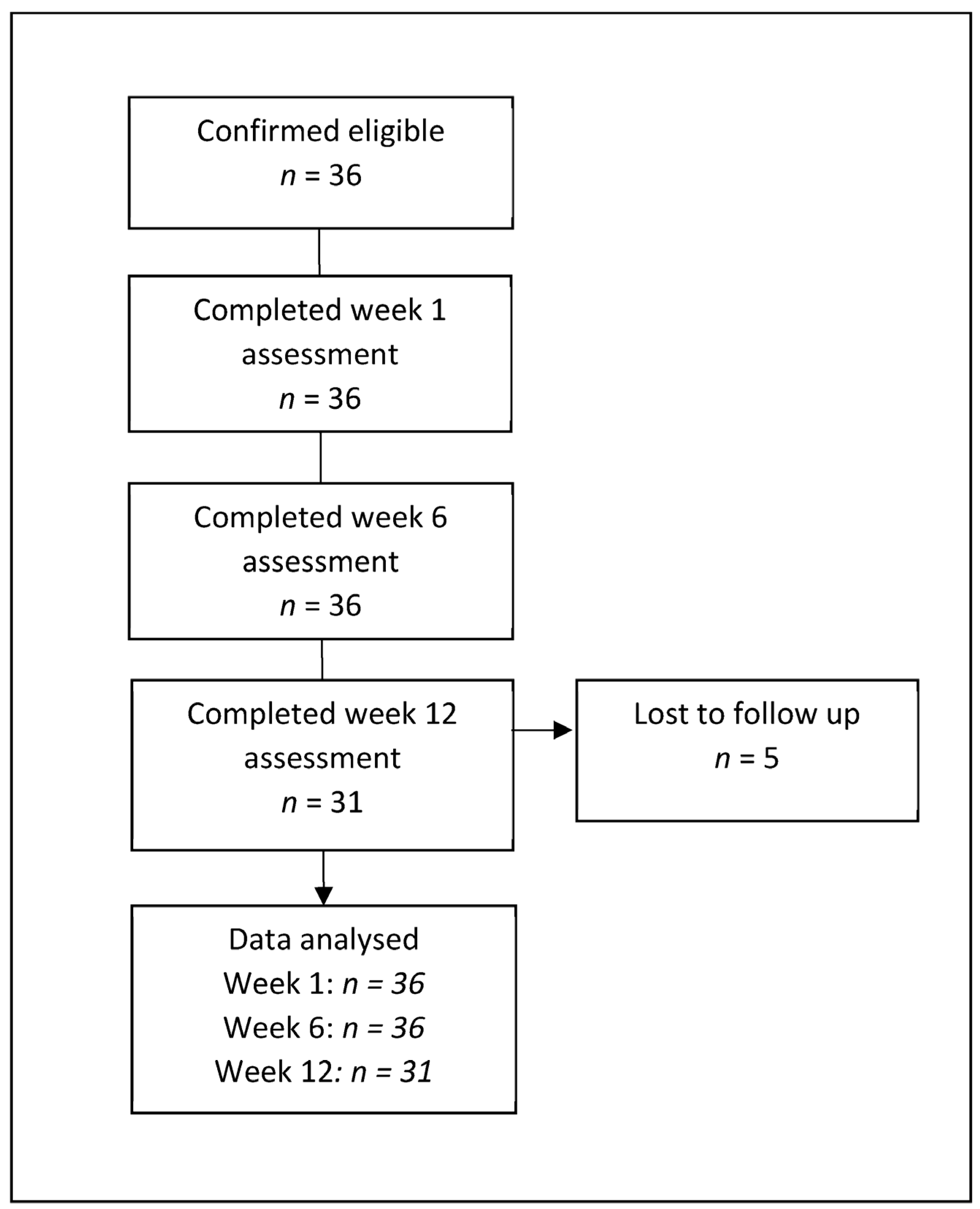
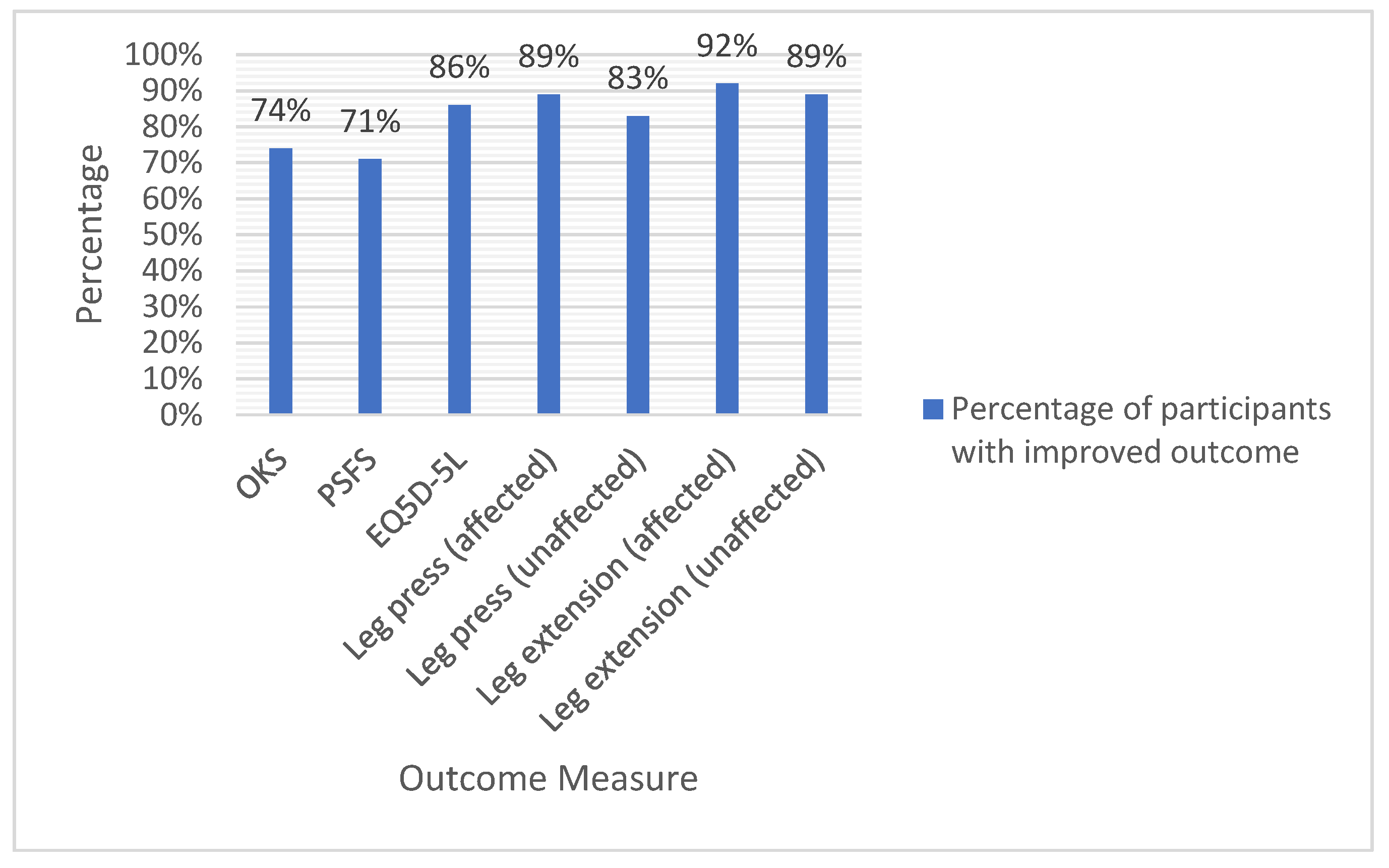
4. Results
5. Discussion
6. Interpretation
7. Limitations
8. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Versus Arthritis. The State of Musculoskeletal Health 2021; Versus Arthritis: Chesterfield, UK, 2021. [Google Scholar]
- Cross, M.; Smith, E.; Hoy, D.; Nolte, S.; Ackerman, I.; Fransen, M.; Bridgett, L.; Wilsliams, S.; Guillemin, F.; Hill, C.L.; et al. The global burden of hip and knee osteoarthritis: Estimates from the Global Burden of Disease 2010 study. Ann. Rheum. Dis. 2014, 73, 1323–1330. [Google Scholar] [CrossRef] [PubMed]
- Office for National Statistics. Population Estimates for the UK, England and Wales, Scotland and Northern Ireland: Mid-2020; Office for National Statistics: Newport, UK, 2021. [Google Scholar]
- National Joint Registry. NJR Surgeon and Hospital Profile; Royal Bournemouth Hospital: Dorset, UK, 2022. [Google Scholar]
- National Institute for Health and Care Excellence. Osteoarthritis: Care and Management Clinical Guideline [CG177]; National Institute for Health and Care Excellence: London, UK, 2014. [Google Scholar]
- American Academy of Orthopaedic Surgeons. Management of Osteoarthritis of the Knee (Non-Arthroplasty): Evidence-Based Clinical Practice Guidelines; American Academy of Orthopaedic Surgeons: Rosemont, IL, USA, 2021. [Google Scholar]
- Bannuru, R.R.; Osani, M.C.; Vaysbrot, E.E.; Arden, N.K.; Bennell, K.; Bierma-Zeinstra, S.M.A.; Kraus, V.B.; Lohmander, L.S.; Abbott, J.H.; Bhandari, M.; et al. OARSI guidelines for the non-surgical management of knee, hip, and polyarticular osteoarthritis. Osteoarthr. Cartil. 2019, 27, 1578–1589. [Google Scholar] [CrossRef] [PubMed]
- Uthman, O.A.; van der Windt, D.A.; Jordan, J.; Dziedzic, K.S.; Healey, E.L.; Peat, G.M.; Foster, N.E. Exercise for lower limb osteoarthritis: Systematic review incorporating trial sequential analysis and network meta-analysis. Br. J. Sports Med. 2014, 48, 1579. [Google Scholar] [CrossRef] [PubMed]
- Holden, M.A.; Button, K.; Collins, N.J.; Henrotin, Y.; Hinman, R.S.; Larsen, J.B.; Metcalf, B.; Master, H.; Skou, S.T.; Thoma, L.M.; et al. Guidance for Implementing Best Practice Therapeutic Exercise for Patients with Knee and Hip Osteoarthritis: What Does the Current Evidence Base Tell Us? Arthritis Care Res. 2021, 73, 1746–1753. [Google Scholar] [CrossRef] [PubMed]
- Fransen, M.; McConnell, S.; Harmer, A.R.; Van Der Esch, M.; Simic, M.; Bennell, K.L. Exercise for osteoarthritis of the knee: A Cochrane systematic review. Br. J. Sports Med. 2015, 49, 1554–1557. [Google Scholar] [CrossRef] [PubMed]
- Jansen, M.J.; Viechtbauer, W.; Lenssen, A.F.; Hendriks, E.J.; de Bie, R.A. Strength training alone, exercise therapy alone, and exercise therapy with passive manual mobilisation each reduce pain and disability in people with knee osteoarthritis: A systematic review. J. Physiother. 2011, 57, 11–20. [Google Scholar] [CrossRef]
- Ogrinc, G.; Davies, L.; Goodman, D.; Batalden, P.; Davidoff, F.; Stevens, D. Squire 2.0 (Standards for Quality Improvement Reporting Excellence): Revised Publication Guidelines from a Detailed Consensus Process. Am. J. Crit. Care 2015, 24, 466–473. [Google Scholar] [CrossRef]
- Hoffmann, T.C.; Glasziou, P.P.; Boutron, I.; Milne, R.; Perera, R.; Moher, D.; Altman, D.G.; Barbour, V.; Macdonald, H.; Johnston, M.; et al. Better reporting of interventions: Template for intervention description and replication (TIDieR) checklist and guide. BMJ 2014, 348, g1687. [Google Scholar] [CrossRef]
- Slade, S.C.; Dionne, C.E.; Underwood, M.; Buchbinder, R. Consensus on Exercise Reporting Template (CERT): Explanation and Elaboration Statement. Br. J. Sports Med. 2016, 50, 1428–1437. [Google Scholar] [CrossRef]
- NHS. Plan, Do, Study, Act (PDSA) Cycles and the Model for Improvement; NHS: Leeds, UK, 2022. [Google Scholar]
- ACSM. ACSM’s Guidelines for Exercise Testing and Prescription, 10th ed.; London Wolters Kluwer: London, UK, 2018. [Google Scholar]
- Nam, C.-W.; Kim, K.; Lee, H.-Y. The Influence of Exercise on an Unstable Surface on the Physical Function and Muscle Strength of Patients with Osteoarthritis of the Knee. J. Phys. Ther. Sci. 2014, 26, 1609–1612. [Google Scholar] [CrossRef]
- Jaric, S. Muscle strength testing: Use of normalisation for body size. Sports Med. 2002, 32, 615–631. [Google Scholar] [CrossRef]
- Van Hout, B.; Janssen, M.; Feng, Y.-S.; Kohlmann, T.; Busschbach, J.; Golicki, D.; Lloyd, A.; Scalone, L.; Kind, P.; Pickard, A.S. Interim Scoring for the EQ-5D-5L: Mapping the EQ-5D-5L to EQ-5D-3L Value Sets. Value Health 2012, 15, 708–715. [Google Scholar] [CrossRef]
- Janssen, M.F.; Birnie, E.; Haagsma, J.A.; Bonsel, G.J. Comparing the Standard EQ-5D Three-Level System with a Five-Level Version. Value Health 2008, 11, 275–284. [Google Scholar] [CrossRef]
- Feng, Y.; Devlin, N.; Herdman, M. Assessing the health of the general population in England: How do the three- and five-level versions of EQ-5D compare? Health Qual. Life Outcomes 2015, 13, 171. [Google Scholar] [CrossRef]
- Chatman, A.B.; Hyams, S.P.; Neel, J.M.; Binkley, J.M.; Stratford, P.; Schomberg, A.; Stabler, M. The Patient-Specific Functional Scale: Measurement Properties in Patients with Knee Dysfunction. Phys. Ther. 1997, 77, 820–829. [Google Scholar] [CrossRef]
- Horn, K.K.; Jennings, S.; Richardson, G.; van Vliet, D.; Hefford, C.; Abbott, J.H. The Patient-Specific Functional Scale: Psychometrics, Clinimetrics, and Application as a Clinical Outcome Measure. J. Orthop. Sports Phys. Ther. 2012, 42, 30–42. [Google Scholar] [CrossRef]
- Murray, D.W.; Fitzpatrick, R.; Rogers, K.; Pandit, H.; Beard, D.J.; Carr, A.J.; Dawson, J. The use of the Oxford hip and knee scores. J. Bone Jt. Surg. Br. 2007, 89, 1010–1014. [Google Scholar] [CrossRef]
- Xie, F.; Ye, H.; Zhang, Y.; Liu, X.; Lei, T.; Li, S.-C. Extension from inpatients to outpatients: Validity and reliability of the Oxford Knee Score in measuring health outcomes in patients with knee osteoarthritis. Int. J. Rheum. Dis. 2010, 14, 206–210. [Google Scholar] [CrossRef]
- Habibzadeh, F. Statistical Data Editing in Scientific Articles. J. Korean Med. Sci. 2017, 32, 1072–1076. [Google Scholar] [CrossRef]
- World Medical Association. WMA Declaration of Helsinki—Ethical Principles for Medical Research Involving Human Subjects; World Medical Association: Ferney-Voltaire, France, 2018. [Google Scholar]
- Bilbao, A.; García-Pérez, L.; Arenaza, J.C.; García, I.; Ariza-Cardiel, G.; Trujillo-Martín, E.; Forjaz, M.J.; Martín-Fernández, J. Psychometric properties of the EQ-5D-5L in patients with hip or knee osteoarthritis: Reliability, validity and responsiveness. Qual. Life Res. 2018, 27, 2897–2908. [Google Scholar] [CrossRef]
- Oliveira, A.; Rebelo, P.; Paixão, C.; Jácome, C.; Cruz, J.; Martins, V.; Simão, P.; Brooks, D.; Marques, A. Minimal Clinically Important Difference for Quadriceps Muscle Strength in People with COPD following Pulmonary Rehabilitation. COPD J. Chronic Obstr. Pulm. Dis. 2021, 18, 35–44. [Google Scholar] [CrossRef] [PubMed]
- Von Heideken, J.; Chowdhry, S.; Borg, J.; James, K.; Iversen, M.D. Reporting of Harm in Randomized Controlled Trials of Therapeutic Exercise for Knee Osteoarthritis: A Systematic Review. Phys. Ther. 2021, 101, pzab161. [Google Scholar] [CrossRef] [PubMed]
- Jessep, S.A.; Walsh, N.E.; Ratcliffe, J.; Hurley, M.V. Long-term clinical benefits and costs of an integrated rehabilitation programme compared with outpatient physiotherapy for chronic knee pain. Physiotherapy 2009, 95, 94–102. [Google Scholar] [CrossRef] [PubMed]
- Roos, E.; Grønne, D.; Skou, S.; Zywiel, M.; McGlasson, R.; Barton, C.; Kemp, J.; Crossley, K.; Davis, A. Immediate outcomes following the GLA:D® program in Denmark, Canada and Australia. A longitudinal analysis including 28,370 patients with symptomatic knee or hip osteoarthritis. Osteoarthr. Cartil. 2021, 29, 502–506. [Google Scholar] [CrossRef]

| PDSA Element | Description |
|---|---|
| Plan |
|
| Do |
|
| Study |
|
| Act |
|
| Outcome Measure | n | Week 1 Median (IQR) | n | Week 6 Median (IQR) | n | Week 12 Median (IQR) |
|---|---|---|---|---|---|---|
| Oxford Knee Score | 36 | 28.0 (24 to 35.75) | 35 | 35.0 (26.0 to 40.0) | 31 | 37.0 (26.0 to 42.0) |
| EQ5D-5L | 31 | 0.64 (0.49 to 0.72) | 31 | 0.73 (0.60 to 0.80) | 29 | 0.71 (0.65 to 0.78) |
| PSFS | 36 | 4.2 (2.7 to 5.5) | 35 | 5.3 (4 to 6.6) | 31 | 6.3 (5 to 7.6) |
| Leg press—affected (1RM normalised to bodyweight (kg)) | 34 | 59.3 (40.2 to 71.9) | 35 | 71.7 (57.6 to 84.2) | 29 | 73.3 (65.1 to 97.6) |
| Leg press—unaffected (1RM normalised to bodyweight (kg)) | 35 | 73.3 (54.9 to 86.8) | 35 | 78.30 (65.6 to 98.3) | 30 | 81.8 (75.4 to 107.0) |
| Leg extension—affected (1RM normalised to bodyweight (kg)) | 30 | 11.2 (3.2 to 23.6) | 34 | 14.0 (6.5 to 29.1) | 28 | 18.1 (10.3 to 28.7) |
| Leg extension—unaffected (1RM normalised to bodyweight (kg)) | 35 | 20.3 (12.1 to 32.1) | 36 | 22.0 (11.5 to 31.1) | 29 | 25.8 (17.7 to 25.2) |
| Outcome | n | Change from Week 1 to Week 6 Median (IQR) | p | n | Change from Week 1 to Week 12 Median (IQR) | p |
|---|---|---|---|---|---|---|
| Oxford Knee Score | 35 | 4.0 (4.0 to 9.0) | <0.001 | 31 | 4.0 (4 to 8.0) | <0.001 |
| EQ5D-5L | 31 | 0.078 (0.03 to 0.20) | <0.001 | 29 | 0.071 (0.02 to 0.25) | <0.001 |
| PSFS | 35 | 1.3 (0 to 2.6) | 0.005 | 31 | 2.3 (−0.3 to 3.3) | 0.016 |
| Leg press—affected (1RM normalised to bodyweight (kg)) | 33 | 17.8 (5.8 to 27.7) | <0.001 | 28 | 24.2 (9.6 to 35.9) | <0.001 |
| Leg press—unaffected (1RM normalised to bodyweight (kg)) | 34 | 10.1 (0.6 to 19.1) | <0.001 | 29 | 13.5 (1.0 to 24.4) | <0.001 |
| Leg extension—affected (1RM normalised to bodyweight (kg)) | 30 | 3.8 (0.1 to 9.4) | <0.001 | 24 | 7.8 (3.9 to 14.0) | <0.001 |
| Leg extension—unaffected (1RM normalised to bodyweight (kg)) | 35 | 0.6 (−1.9 to 6.1) | 0.153 | 38 | 5.4 (1.7 to 7.4) | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Creasey, J.; Masterman, J.; Turpin, G.; Stanley, R.; Immins, T.; Burgess, L.; Wainwright, T.W. A 1RM Strengthening and Exercise Programme for the Treatment of Knee Osteoarthritis: A Quality-Improvement Study. J. Clin. Med. 2023, 12, 3156. https://doi.org/10.3390/jcm12093156
Creasey J, Masterman J, Turpin G, Stanley R, Immins T, Burgess L, Wainwright TW. A 1RM Strengthening and Exercise Programme for the Treatment of Knee Osteoarthritis: A Quality-Improvement Study. Journal of Clinical Medicine. 2023; 12(9):3156. https://doi.org/10.3390/jcm12093156
Chicago/Turabian StyleCreasey, James, Jo Masterman, Gregory Turpin, Richard Stanley, Tikki Immins, Louise Burgess, and Thomas W. Wainwright. 2023. "A 1RM Strengthening and Exercise Programme for the Treatment of Knee Osteoarthritis: A Quality-Improvement Study" Journal of Clinical Medicine 12, no. 9: 3156. https://doi.org/10.3390/jcm12093156
APA StyleCreasey, J., Masterman, J., Turpin, G., Stanley, R., Immins, T., Burgess, L., & Wainwright, T. W. (2023). A 1RM Strengthening and Exercise Programme for the Treatment of Knee Osteoarthritis: A Quality-Improvement Study. Journal of Clinical Medicine, 12(9), 3156. https://doi.org/10.3390/jcm12093156







