Evaluation of Isokinetic Knee Strengths after ACL Reconstruction with Quadrupled Semitendinosus Suspensory Femoral and Tibial Fixation versus Four-Strand Semitendinosus and Gracilis Suspensory Femoral and Tibial Screw Fixation
Abstract
:1. Introduction
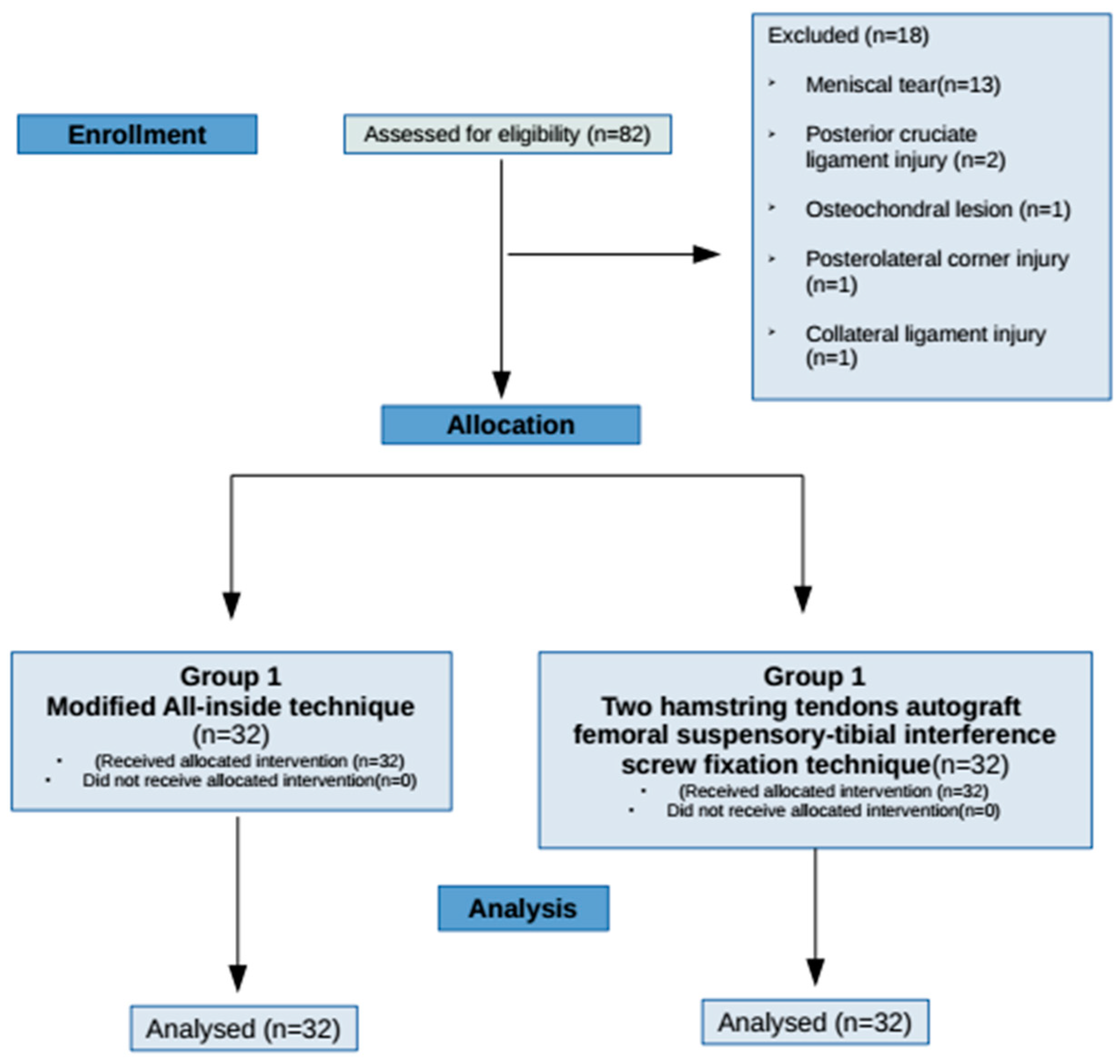
2. Material and Methods
2.1. Surgical Technique
2.1.1. Group 1: Only the Semitendinosus Tendon Autograft Tibial-Femoral Suspensory Fixation Technique (Modified All-Inside Technique)
2.1.2. Group 2: Semitendinosus and Gracilis Tendons Autograft Femoral Suspensory-Tibial Interference Screw Fixation Technique
2.2. Rehabilitation Protocol
2.3. Experimental Design
2.4. Isokinetic Knee Strength Measurements
3. Statistical Analysis
4. Results
5. Discussions
6. Limitations
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Risberg, M.A.; Lewek, M.; Snyder-Mackler, L. A systematic review of the evidence for anterior cruciate ligament rehabilitation: How much and what type? Phys. Ther. Sport 2004, 5, 125–145. [Google Scholar] [CrossRef]
- Sanders, T.L.; Maradit Kremers, H.; Bryan, A.J.; Larson, D.R.; Dahm, D.L.; Levy, B.A.; Stuart, M.J.; Krych, A.J. Incidence of Anterior Cruciate Ligament Tears and Reconstruction: A 21-Year Population-Based Study. Am. J. Sports Med. 2016, 44, 1502–1507. [Google Scholar] [CrossRef] [PubMed]
- Aglietti, P.; Giron, F.; Buzzi, R.; Biddau, F.; Sasso, F. Anterior cruciate ligament reconstruction: Bone-patellar tendon-bone compared with double semitendinosus and gracilis tendon grafts. J. Bone Jt. Surg. Am. 2004, 86, 2143–2155. [Google Scholar] [CrossRef]
- Bhimani, R.; Shahriarirad, R.; Ranjbar, K.; Erfani, A.; Ashkani-Esfahani, S. Transportal versus all-inside techniques of anterior cruciate ligament reconstruction: A systematic review. J. Orthop. Surg. Res. 2021, 16, 734. [Google Scholar] [CrossRef]
- Bosco, F.; Giustra, F.; Crivellaro, M.; Giai Via, R.; Lavia, A.D.; Capella, M.; Sabatini, L.; Risitano, S.; Rovere, G.; Massè, A.; et al. Is augmentation the best solution in partial anterior cruciate ligament tears? A literature systematic review and meta-analysis. J. Orthop. 2022, 36, 11–17. [Google Scholar] [CrossRef]
- Sarraj, M.; de Sa, D.; Shanmugaraj, A.; Musahl, V.; Lesniak, B.P. Over-the-top ACL reconstruction yields comparable outcomes to traditional ACL reconstruction in primary and revision settings: A systematic review. Knee Surg. Sports Traumatol. Arthrosc. 2019, 27, 427–444. [Google Scholar] [CrossRef]
- Lautamies, R.; Harilainen, A.; Kettunen, J.; Sandelin, J.; Kujala, U.M. Isokinetic quadriceps and hamstring muscle strength and knee function 5 years after anterior cruciate ligament reconstruction: Comparison between bone-patellar tendon-bone and hamstring tendon autografts. Knee Surg. Sports Traumatol. Arthrosc. 2008, 16, 1009–1016. [Google Scholar] [CrossRef]
- Makihara, Y.; Nishino, A.; Fukubayashi, T.; Kanamori, A. Decrease of knee flexion torque in patients with ACL recon- struction: Combined analysis of the architecture and function of the knee flexor muscles. Knee Surg. Sports Traumatol. Arthrosc. 2006, 14, 310–317. [Google Scholar] [CrossRef]
- Nakamura, N.; Horibe, S.; Sasaki, S.; Kitaguchi, T.; Tagami, M.; Mitsuoka, T.; Toritsuka, Y.; Hamada, M.; Shino, K. Evaluation of active knee flexion and hamstring strength after anterior cruciate ligament reconstruction using hamstring tendons. Arthroscopy 2002, 18, 598–602. [Google Scholar] [CrossRef]
- Lepley, L.K. Deficits in Quadriceps Strength and Patient-Oriented Outcomes at Return to Activity after ACL Reconstruction: A Review of the Current Literature. Sports Health 2015, 7, 231–238. [Google Scholar] [CrossRef]
- Zwolski, C.; Schmitt, L.C.; Quatman-Yates, C.; Thomas, S.; Hewett, T.E.; Paterno, M.V. The influence of quadriceps strength asymmetry on patient-reported function at time of return to sport after anterior cruciate ligament reconstruction. Am. J. Sports Med. 2015, 43, 2242–2249. [Google Scholar] [CrossRef] [PubMed]
- Danneskiold-Samsøe, B.; Bartels, E.M.; Bülow, P.M.; Lund, H.; Stockmarr, A.; Holm, C.C.; Wätjen, I.; Appleyard, M.; Bliddal, H. Isokinetic and isometric muscle strength in a healthy population with special reference to age and gender. Acta Physiol. 2009, 197 (Suppl. S673), 1–68. [Google Scholar] [CrossRef] [PubMed]
- Neeter, C.; Gustavsson, A.; Thomeé, P.; Augustsson, J.; Thomeé, R.; Karlsson, J. Development of a strength test battery for evaluating leg muscle power after anterior cruciate ligament injury and reconstruction. Knee Surg. Sports Traumatol. Arthrosc. 2006, 14, 571–580. [Google Scholar] [CrossRef] [PubMed]
- Undheim, M.B.; Cosgrave, C.; King, E.; Strike, S.; Marshall, B.; Falvey, É.; Franklyn-Miller, A. Isokinetic muscle strength and readiness to return to sport following anterior cruciate ligament reconstruction: Is there an association? A systematic review and a protocol recommendation. Br. J. Sports Med. 2015, 49, 1305–1310. [Google Scholar] [CrossRef] [PubMed]
- Gokeler, A.; Welling, W.; Zaffagnini, S.; Seil, R.; Padua, D. Development of a test battery to enhance safe return to sports after anterior cruciate ligament reconstruction. Knee Surg. Sports Traumatol. Arthrosc. 2017, 25, 192–199. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Xergia, S.A.; McClelland, J.A.; Kvist, J.; Vasiliadis, H.S.; Georgoulis, A.D. The influence of graft choice on isokinetic muscle strength 4–24 months after anterior cruciate ligament reconstruction. Knee Surg. Sports Traumatol. Arthrosc. 2011, 19, 768–780. [Google Scholar] [CrossRef] [Green Version]
- Baumgart, C.; Schubert, M.; Hoppe, M.W.; Gokeler, A.; Freiwald, J. Do ground reaction forces during unilateral and bilateral movements exhibit compensation strategies following ACL reconstruction? Knee Surg. Sports Traumatol. Arthrosc. 2017, 25, 1385–1394. [Google Scholar] [CrossRef]
- Gokeler, A.; Bisschop, M.; Benjaminse, A.; Myer, G.D.; Eppinga, P.; Otten, E. Quadriceps function following ACL reconstruction and rehabilitation: Implications for optimisation of current practices. Knee Surg. Sports Traumatol. Arthrosc. 2014, 22, 1163–1174. [Google Scholar] [CrossRef]
- Mahirogullari, M.; Kehribar, L.; Surucu, S.; Kayaalp, M.E.; Yilmaz, A.K.; Aydin, M. Comparative Results of Anterior Cruciate Ligament Reconstruction with Full Tibial Tunnel: Quadrupled Semitendinosus Suspensory Femoral and Tibial Fixation versus Quadrupled Semitendinosus and Gracilis Suspensory Femoral and Tibial Screw and Staple Fixation. J. Knee Surg. 2022. [Google Scholar] [CrossRef]
- van Grinsven, S.; van Cingel, R.E.; Holla, C.J.; van Loon, C.J. Evidence-based rehabilitation following anterior cruciate ligament reconstruction. Knee Surg. Sports Traumatol. Arthrosc. 2010, 18, 1128–1144. [Google Scholar] [CrossRef]
- Kruse, L.M.; Gray, B.; Wright, R.W. Rehabilitation after anterior cruciate ligament reconstruction: A systematic review. J. Bone Jt. Surg. Am. 2012, 94, 1737–1748. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kambič, T.; Lainščak, M.; Hadžić, V. Reproducibility of isokinetic knee testing using the novel isokinetic SMM iMoment dynamometer. PLoS ONE 2020, 15, e0237842. [Google Scholar] [CrossRef]
- Faul, F.; Erdfelder, E.; Lang, A.G.; Buchner, A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef]
- Fischer, F.; Fink, C.; Herbst, E.; Hoser, C.; Hepperger, C.; Blank, C.; Gföller, P. Higher hamstring-to-quadriceps isokinetic strength ratio during the first post-operative months in patients with quadriceps tendon compared to hamstring tendon graft following ACL reconstruction. Knee Surg. Sports Traumatol. Arthrosc. 2018, 26, 418–425. [Google Scholar] [CrossRef] [PubMed]
- Herrington, L.; Wrapson, C.; Matthews, M.; Matthews, H. Anterior cruciate ligament reconstruction, hamstring versus bone-patella tendon-bone grafts: A systematic literature review of outcome from surgery. Knee 2005, 12, 41–50. [Google Scholar] [CrossRef]
- Kim, J.G.; Yang, S.J.; Lee, Y.S.; Shim, J.C.; Ra, H.J.; Choi, J.Y. The effects of hamstring harvesting on outcomes in anterior cruciate ligament-reconstructed patients: A comparative study between hamstring-harvested and -unharvested patients. Arthroscopy 2011, 27, 1226–1234. [Google Scholar] [CrossRef]
- Yosmaoglu, H.B.; Baltaci, G.; Ozer, H.; Atay, A. Effects of additional gracilis tendon harvest on muscle torque, motor coordination, and knee laxity in ACL reconstruction. Knee Surg. Sports Traumatol. Arthrosc. 2011, 19, 1287–1292. [Google Scholar] [CrossRef]
- Tashiro, T.; Kurosawa, H.; Kawakami, A.; Hikita, A.; Fukui, N. Influence of medial hamstring tendon harvest on knee flexor strength after anterior cruciate ligament reconstruction. A detailed evaluation with comparison of single- and double-tendon harvest. Am. J. Sports Med. 2003, 31, 522–529. [Google Scholar] [CrossRef] [PubMed]
- Blackman, A.J.; Stuart, M.J. All-inside anterior cruciate ligament reconstruction. J. Knee Surg. 2014, 27, 347–352. [Google Scholar] [CrossRef] [PubMed]
- Simonian, P.T.; Harrison, S.D.; Cooley, V.J.; Escabedo, E.M.; Deneka, D.A.; Larson, R.V. Assessment of morbidity of semitendinosus and gracilis tendon harvest for ACL reconstruction. Am. J. Knee Surg. 1997, 10, 54–59. [Google Scholar] [PubMed]
- Baron, J.E.; Parker, E.A.; Duchman, K.R.; Westermann, R.W. Perioperative and Postoperative Factors Influence Quadriceps Atrophy and Strength After ACL Reconstruction: A Systematic Review. Orthop. J. Sports Med. 2020, 8, 2325967120930296. [Google Scholar] [CrossRef] [PubMed]
- Hernández-Vaquero, D.; Fernández-Fairen, M.; Torres-Perez, A.; Santamaría, A. Cirugía de mínima invasión frente a cirugía convencional. Una aproximación desde la evidencia científica [Minimally invasive surgery versus conventional surgery. A review of the scientific evidence]. Rev. Esp. Cir. Ortop. Traumatol. 2012, 56, 444–458. (In Spanish) [Google Scholar] [CrossRef] [PubMed]


| Variables | Technique | N | Mean ± SD | t | p |
|---|---|---|---|---|---|
| Age | Group 1 | 32 | 26.15 ± 8.48 | 1.898 | 0.062 |
| Group 2 | 32 | 22.65 ± 6.17 | |||
| Height (cm) | Group 1 | 32 | 79.00 ± 10.63 | 0.540 | 0.591 |
| Group 2 | 32 | 77.65 ± 9.22 | |||
| Weight (kg) | Group 1 | 32 | 179.37 ± 6.19 | −0.167 | 0.868 |
| Group 2 | 32 | 179.62 ± 5.80 | |||
| BMI (kg/m2) | Group 1 | 32 | 24.45 ± 2.23 | 0.695 | 0.490 |
| Group 2 | 32 | 24.05 ± 2.35 |
| Group 1 | Operated Side | Non-Operated Side | t | p | ES | %95 CI | |
|---|---|---|---|---|---|---|---|
| Mean ± SD | Mean ± SD | LB | UB | ||||
| 60 Ex (Nm) | 164.78 ± 42.99 | 196.65 ± 38.75 | −5.16 | 0.000 | 0.77 | −44.32 | −19.23 |
| 180 Ex (Nm) | 109.81 ± 26.73 | 129.50 ± 22.01 | −4.69 | 0.000 | 0.80 | −28.23 | −11.13 |
| 240 Ex (Nm) | 96.53 ± 24.97 | 109.09 ± 22.68 | −3.40 | 0.002 | 0.53 | −20.08 | −5.03 |
| 60 Flx (Nm) | 114 ± 29.85 | 116.19 ± 25.87 | −0.311 | 0.758 | 0.07 | −13.24 | 9.74 |
| 180 Flx (Nm) | 74.96 ± 15.51 | 85.62 ± 16.81 | −3.28 | 0.003 | 0.65 | −17.26 | −4.04 |
| 240 Flx (Nm) | 70.43 ± 19.34 | 79.40 ± 16.16 | −3.34 | 0.002 | 0.50 | −14.44 | −3.49 |
| Group 2 | Operated side | Non-Operated side | t | p | ES | %95 CI | |
| Mean ± SD | Mean ± SD | LB | UB | ||||
| 60 Ex (Nm) | 146.12 ± 23.77 | 165.90 ± 25.49 | −6.62 | 0.000 | 0.80 | −25.86 | −13.69 |
| 180 Ex (Nm) | 89.53 ± 19.21 | 95.40 ± 19.22 | −1.94 | 0.061 | 0.30 | −12.04 | 0.29 |
| 240 Ex (Nm) | 72.12 ± 15.79 | 79.87 ± 20.89 | −3.153 | 0.004 | 0.41 | −12.76 | −2.73 |
| 60 Flx (Nm) | 96.81 ± 18.29 | 99.75 ± 20.75 | −1.04 | 0.304 | 0.15 | −8.67 | 2.79 |
| 180 Flx (Nm) | 63.34 ± 16.63 | 64.75 ± 16.88 | −0.544 | 0.590 | 0.08 | −6.67 | 3.86 |
| 240 Flx (Nm) | 52.65 ± 13.03 | 59.19 ± 19.22 | −2.581 | 0.015 | 0.39 | −11.69 | −1.37 |
| Variables | Group 1 Non-Operated Side | Group 2 Non-Operated Side | t | p | ES | %95 CI | |
|---|---|---|---|---|---|---|---|
| Mean ± SD | Mean ± SD | LB | UB | ||||
| 60 Ex (Nm) | 196.65 ± 38.75 | 165.90 ± 25.49 | 3.75 | 0.000 | 0.93 | 14.35 | 47.14 |
| 180 Ex (Nm) | 129.50 ± 22.00 | 95.40 ± 19.22 | 6.60 | 0.000 | 1.65 | 23.76 | 44.41 |
| 240 Ex (Nm) | 109.09 ± 22.68 | 79.87 ± 20.89 | 5.36 | 0.000 | 1.39 | 18.32 | 40.11 |
| 60 Flx (Nm) | 116.18 ± 25.87 | 99.75 ± 20.75 | 2.80 | 0.007 | 0.75 | 4.71 | 28.16 |
| 180 Flx (Nm) | 85.62 ± 16.81 | 64.75 ± 16.88 | 4.95 | 0.000 | 1.31 | 12.45 | 29.29 |
| 240 Flx (Nm) | 79.40 ± 16.16 | 59.18 ± 19.22 | 4.55 | 0.000 | 1.13 | 4.43 | 29.09 |
| Variables | Group 1 Operated Side | Group 2 Operated Side | t | p |
|---|---|---|---|---|
| Mean ± SD | Mean ± SD | |||
| 60 Ex (Nm) | 164.87 ± 42.99 | 146.12 ± 23.77 | 0.004 | 0.947 |
| 180 Ex (Nm) | 109.81 ± 26.73 | 89.53 ± 19.21 | 0.070 | 0.792 |
| 240 Ex (Nm) | 96.53 ± 24.97 | 72.12 ± 15.79 | 0.077 | 0.783 |
| 60 Flx (Nm) | 114.43 ± 29.85 | 96.03 ± 18.33 | 1.178 | 0.282 |
| 180 Flx (Nm) | 74.96 ± 15.51 | 63.34 ± 16.63 | 1.923 | 0.171 |
| 240 Flx (Nm) | 70.43 ± 19.34 | 52.65 ± 13.03 | 1.569 | 0.215 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cerci, M.H.; Yilmaz, A.K.; Kehribar, L.; Surucu, S.; Aydin, M.; Mahirogullari, M. Evaluation of Isokinetic Knee Strengths after ACL Reconstruction with Quadrupled Semitendinosus Suspensory Femoral and Tibial Fixation versus Four-Strand Semitendinosus and Gracilis Suspensory Femoral and Tibial Screw Fixation. J. Clin. Med. 2023, 12, 4004. https://doi.org/10.3390/jcm12124004
Cerci MH, Yilmaz AK, Kehribar L, Surucu S, Aydin M, Mahirogullari M. Evaluation of Isokinetic Knee Strengths after ACL Reconstruction with Quadrupled Semitendinosus Suspensory Femoral and Tibial Fixation versus Four-Strand Semitendinosus and Gracilis Suspensory Femoral and Tibial Screw Fixation. Journal of Clinical Medicine. 2023; 12(12):4004. https://doi.org/10.3390/jcm12124004
Chicago/Turabian StyleCerci, Mehmet Halis, Ali Kerim Yilmaz, Lokman Kehribar, Serkan Surucu, Mahmud Aydin, and Mahir Mahirogullari. 2023. "Evaluation of Isokinetic Knee Strengths after ACL Reconstruction with Quadrupled Semitendinosus Suspensory Femoral and Tibial Fixation versus Four-Strand Semitendinosus and Gracilis Suspensory Femoral and Tibial Screw Fixation" Journal of Clinical Medicine 12, no. 12: 4004. https://doi.org/10.3390/jcm12124004
APA StyleCerci, M. H., Yilmaz, A. K., Kehribar, L., Surucu, S., Aydin, M., & Mahirogullari, M. (2023). Evaluation of Isokinetic Knee Strengths after ACL Reconstruction with Quadrupled Semitendinosus Suspensory Femoral and Tibial Fixation versus Four-Strand Semitendinosus and Gracilis Suspensory Femoral and Tibial Screw Fixation. Journal of Clinical Medicine, 12(12), 4004. https://doi.org/10.3390/jcm12124004






