Antegrade Intramedullary Femoral Lengthening and Distal Temporary Hemiepiphysiodesis for Combined Correction of Leg Length Discrepancy and Coronal Angular Deformity in Skeletally Immature Patients
Abstract
1. Introduction
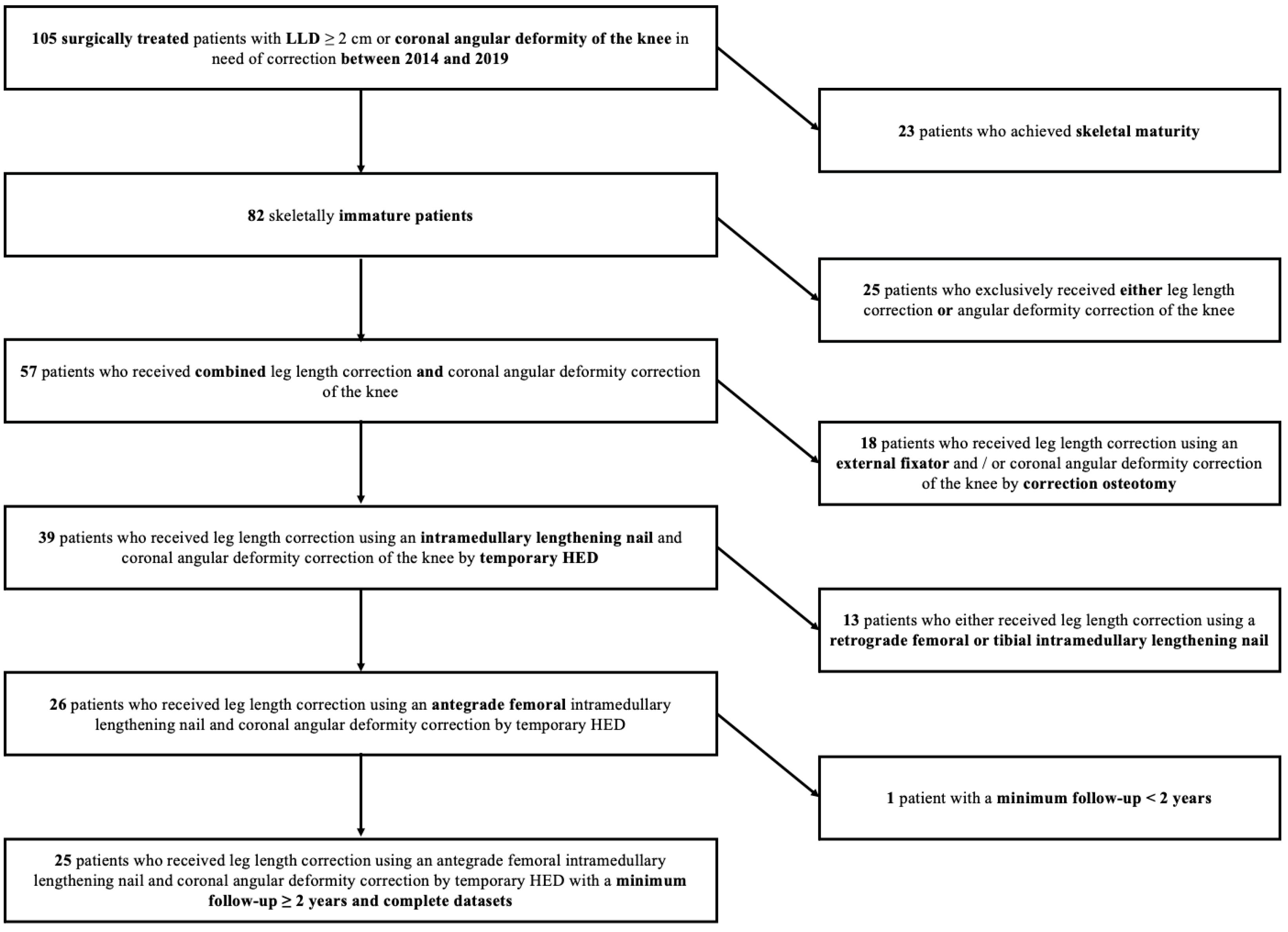
2. Materials and Methods
2.1. Study Design and Setting
2.2. Descriptive Data
2.3. Preoperative and Postoperative Clinical and Radiographic Evaluation
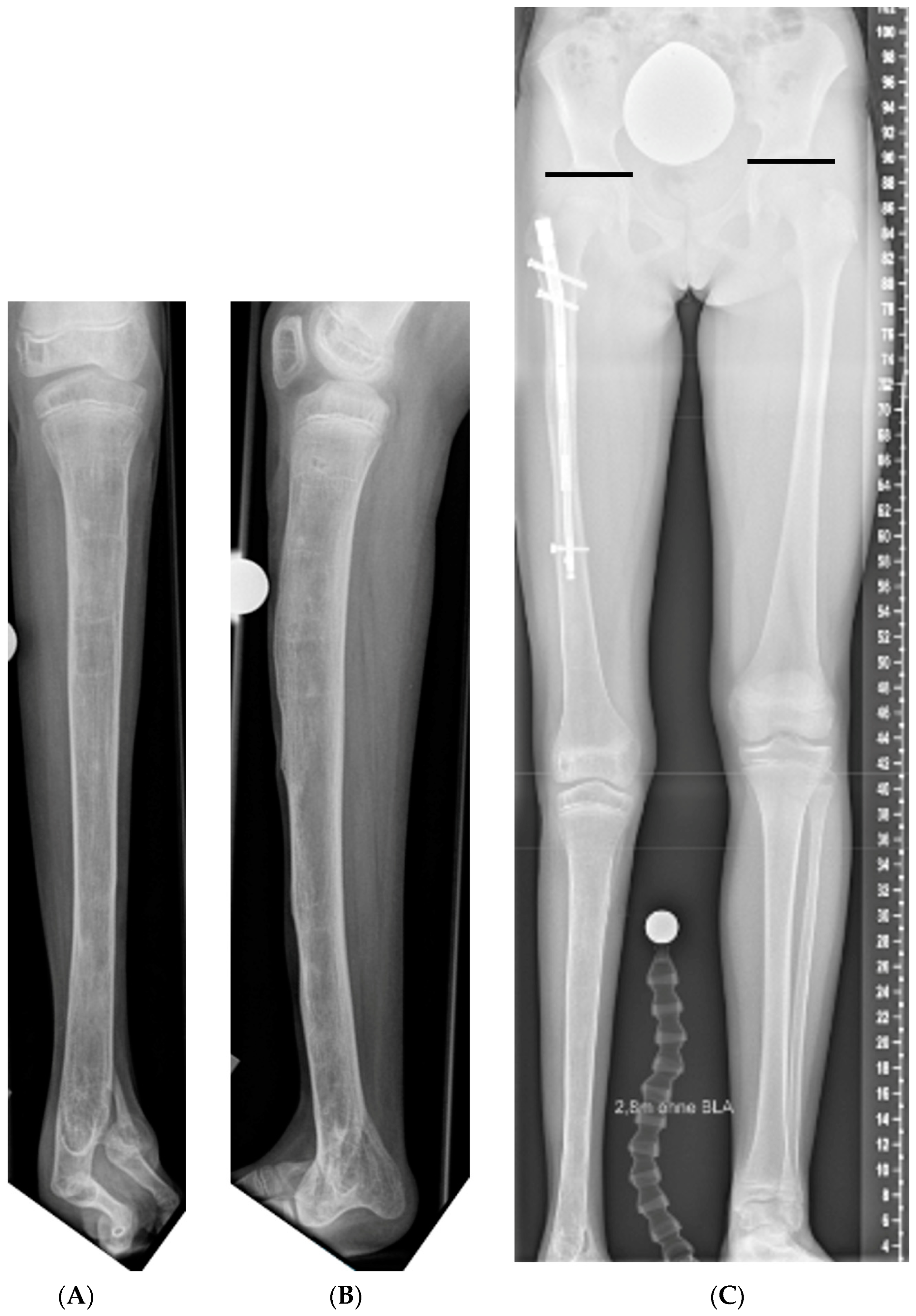
2.4. Surgical Technique and Perioperative Parameters
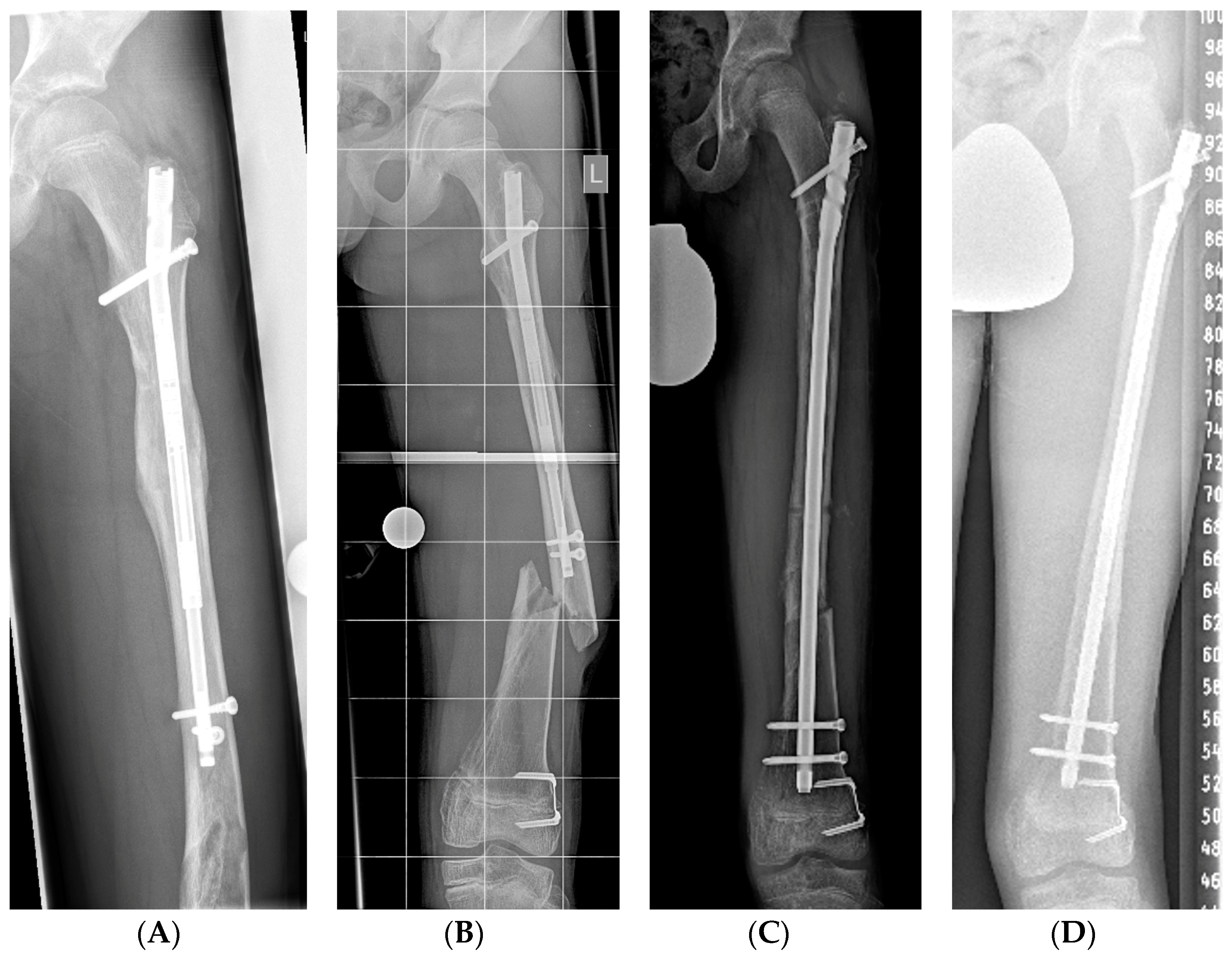
2.4.1. Limb Lengthening
2.4.2. Guided Growth
2.5. Postoperative Lengthening and Follow-Up Protocol
2.6. Complications
2.7. Statistical Analysis
3. Results
3.1. Perioperative Parameters
3.2. Implant Retrieval
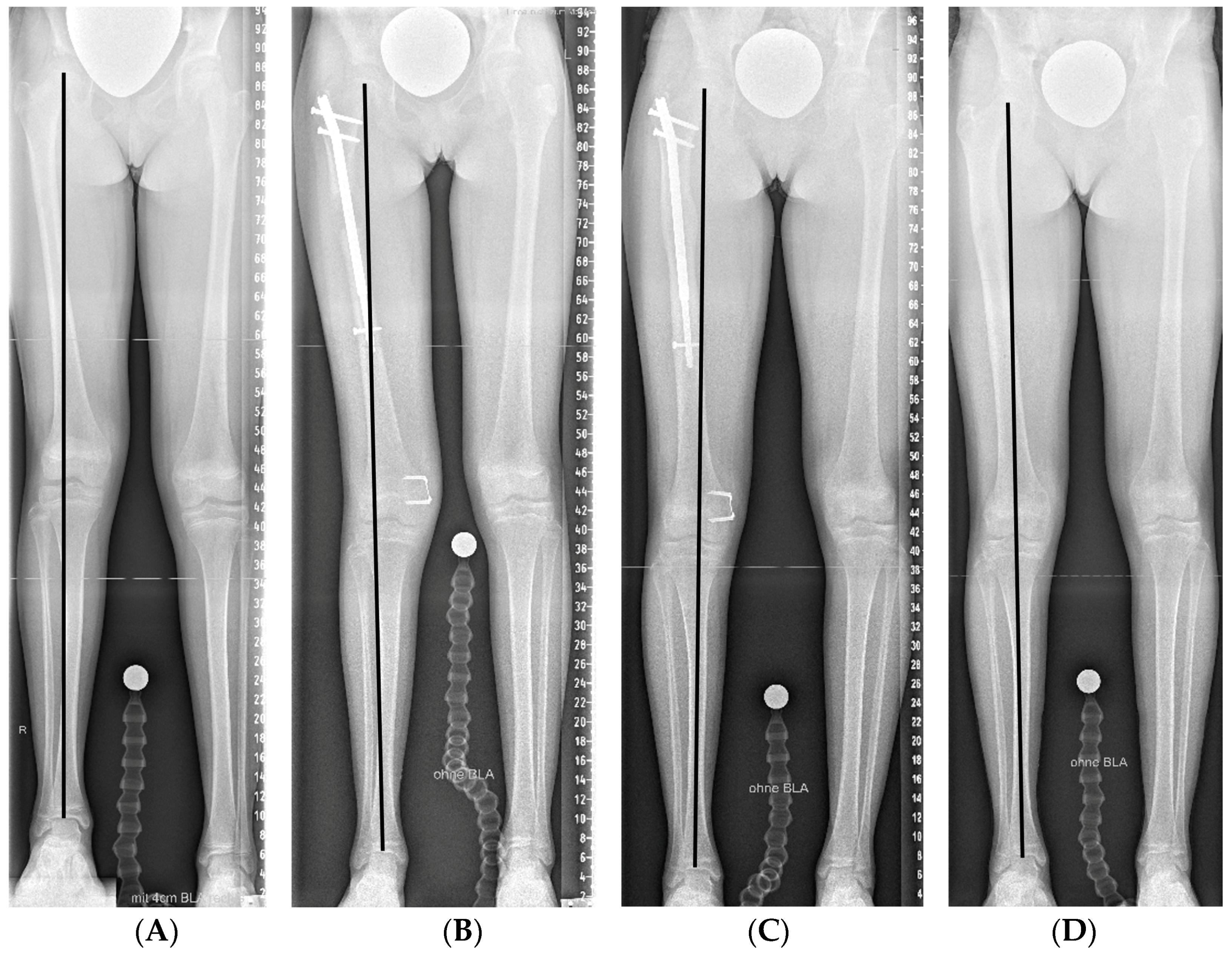
3.3. Radiological Assessment
3.4. Leg Length Equalization
3.5. Axis Realignment
3.6. Complications
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Gross, R.H. Leg length discrepancy: How much is too much? Orthopedics 1978, 1, 307–310. [Google Scholar] [CrossRef] [PubMed]
- Vogt, B.; Gosheger, G.; Wirth, T.; Horn, J.; Rodl, R. Leg Length Discrepancy—Treatment Indications and Strategies. Dtsch. Arztebl. Int. 2020, 117, 405–411. [Google Scholar] [CrossRef] [PubMed]
- Quinones, D.; Liu, R.; Gebhart, J.J. Study Guide—Leg Length Discrepancy (LLD); Pediatric Orthopaedic Society of North America (POSNA): Oakbrook Terrace, IL, USA, 2020. [Google Scholar]
- Vogt, B.; Roedl, R.; Gosheger, G.; Frommer, A.; Laufer, A.; Kleine-Koenig, M.T.; Theil, C.; Toporowski, G. Growth arrest: Leg length correction through temporary epiphysiodesis with a novel rigid staple (RigidTack). Bone Jt. J. 2021, 103-B, 1428–1437. [Google Scholar] [CrossRef] [PubMed]
- Willegger, M.; Schreiner, M.; Kolb, A.; Windhager, R.; Chiari, C. Epiphysiodesis for the treatment of tall stature and leg length discrepancy. Wien. Med. Wochenschr. 2021, 171, 133–141. [Google Scholar] [CrossRef]
- Hasler, C.C. Leg length inequality. Indications for treatment and importance of shortening procedures. Orthopade 2000, 29, 766–774. [Google Scholar] [CrossRef]
- Vogt, B.; Schiedel, F.; Rodl, R. Guided growth in children and adolescents. Correction of leg length discrepancies and leg axis deformities. Orthopade 2014, 43, 267–284. [Google Scholar] [CrossRef]
- Paley, D.; Bhave, A.; Herzenberg, J.E.; Bowen, J.R. Multiplier method for predicting limb-length discrepancy. J. Bone Jt. Surg. Am. 2000, 82, 1432–1446. [Google Scholar] [CrossRef]
- Hafez, M.; Nicolaou, N.; Offiah, A.; Giles, S.N.; Madan, S.S.; Fernandes, J.A. Femoral Lengthening in Children-A Comparison Between Magnetic Intramedullary Lengthening Nails and External Fixators. J. Pediatr. Orthop. 2022, 42, e290–e294. [Google Scholar] [CrossRef]
- Calder, P.R.; McKay, J.E.; Timms, A.J.; Roskrow, T.; Fugazzotto, S.; Edel, P.; Goodier, W.D. Femoral lengthening using the Precice intramedullary limb-lengthening system: Outcome comparison following antegrade and retrograde nails. Bone Jt. J. 2019, 101-B, 1168–1176. [Google Scholar] [CrossRef]
- Laubscher, M.; Mitchell, C.; Timms, A.; Goodier, D.; Calder, P. Outcomes following femoral lengthening: An initial comparison of the Precice intramedullary lengthening nail and the LRS external fixator monorail system. Bone Jt. J. 2016, 98-B, 1382–1388. [Google Scholar] [CrossRef]
- Landge, V.; Shabtai, L.; Gesheff, M.; Specht, S.C.; Herzenberg, J.E. Patient Satisfaction After Limb Lengthening with Internal and External Devices. J. Surg. Orthop. Adv. 2015, 24, 174–179. [Google Scholar] [PubMed]
- Iobst, C.A.; Rozbruch, S.R.; Nelson, S.; Fragomen, A. Simultaneous Acute Femoral Deformity Correction and Gradual Limb Lengthening Using a Retrograde Femoral Nail: Technique and Clinical Results. J. Am. Acad. Orthop. Surg. 2018, 26, 241–250. [Google Scholar] [CrossRef] [PubMed]
- Hammouda, A.I.; Jauregui, J.J.; Gesheff, M.G.; Standard, S.C.; Herzenberg, J.E. Trochanteric Entry for Femoral Lengthening Nails in Children: Is It Safe? J. Pediatr. Orthop. 2017, 37, 258–264. [Google Scholar] [CrossRef] [PubMed]
- Frommer, A.; Rodl, R.; Gosheger, G.; Vogt, B. Application of motorized intramedullary lengthening nails in skeletally immature patients: Indications and limitations. Unfallchirurg 2018, 121, 860–867. [Google Scholar] [CrossRef]
- Radler, C.; Mindler, G.T.; Stauffer, A.; Weiss, C.; Ganger, R. Limb Lengthening with Precice Intramedullary Lengthening Nails in Children and Adolescents. J. Pediatr. Orthop. 2022, 42, e192–e200. [Google Scholar] [CrossRef]
- Frommer, A.; Roedl, R.; Gosheger, G.; Niemann, M.; Turkowski, D.; Toporowski, G.; Theil, C.; Laufer, A.; Vogt, B. What Are the Potential Benefits and Risks of Using Magnetically Driven Antegrade Intramedullary Lengthening Nails for Femoral Lengthening to Treat Leg Length Discrepancy? Clin. Orthop. Relat. Res. 2021, 1480, 790–803. [Google Scholar]
- Jardaly, A.; Gilbert, S.R. Combined antegrade femur lengthening and distal deformity correction: A case series. J. Orthop. Surg. Res. 2021, 16, 60. [Google Scholar] [CrossRef]
- Steiger, C.N.; Lenze, U.; Krieg, A.H. A new technique for correction of leg length discrepancies in combination with complex axis deformities of the lower limb using a lengthening nail and a locking plate. J. Child. Orthop. 2018, 12, 515–525. [Google Scholar] [CrossRef]
- Stevens, P.M. Guided growth for angular correction: A preliminary series using a tension band plate. J. Pediatr. Orthop. 2007, 27, 253–259. [Google Scholar] [CrossRef]
- Vogt, B.; Frommer, A.; Gosheger, G.; Toporowski, G.; Tretow, H.; Rodl, R.; Laufer, A. Growth modulation through hemiepiphysiodesis: Novel surgical techniques: Risks and progress. Orthopade 2021, 50, 538–547. [Google Scholar] [CrossRef]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gotzsche, P.C.; Vandenbroucke, J.P.; Initiative, S. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. Epidemiology 2007, 18, 800–804. [Google Scholar] [CrossRef] [PubMed]
- Vogt, B.; Toporowski, G.; Gosheger, G.; Laufer, A.; Frommer, A.; Kleine-Koenig, M.T.; Roedl, R.; Antfang, C. Guided growth: Angular deformity correction through temporary hemiepiphysiodesis with a flexible staple (FlexTack). Bone Jt. J. 2023, 105-B, 331–340. [Google Scholar] [CrossRef] [PubMed]
- Paley, D. Normal Lower Limb Alignment and Joint Orientation. In Principles of Deformity Correction; Springer: Berlin/Heidelberg, Germany, 2002; pp. 1–18. [Google Scholar]
- Veilleux, L.N.; AlOtaibi, M.; Dahan-Oliel, N.; Hamdy, R.C. Incidence of knee height asymmetry in a paediatric population of corrected leg length discrepancy: A retrospective chart review study. Int. Orthop. 2018, 42, 1979–1985. [Google Scholar] [CrossRef] [PubMed]
- Escott, B.G.; Kelley, S.P. Management of traumatic physeal growth arrest. Orthop. Trauma 2012, 26, 200–211. [Google Scholar] [CrossRef]
- Stanitski, D.F. Limb-length inequality: Assessment and treatment options. J. Am. Acad. Orthop. Surg. 1999, 7, 143–153. [Google Scholar] [CrossRef] [PubMed]
- Sattelberger, J.; Hillebrand, H.; Gosheger, G.; Laufer, A.; Frommer, A.; Appelbaum, S.; Abood, A.A.; Gottliebsen, M.; Rahbek, O.; Moller-Madsen, B.; et al. Comparison of histomorphometric and radiographic effects of growth guidance with tension-band devices (eight-Plate and FlexTack) in a pig model. Acta Orthop. 2021, 92, 364–370. [Google Scholar] [CrossRef]
- Rolfing, J.D.; Bunger, M.; Petruskevicius, J.; Abood, A.A. Removal of broken precice stryde intramedullary lengthening nails. Orthop. Traumatol. Surg. Res. 2021, 107, 102958. [Google Scholar] [CrossRef]
- Iobst, C.A.; Frost, M.W.; Rolfing, J.D.; Rahbek, O.; Bafor, A.; Duncan, M.; Kold, S. Radiographs of 366 removed limb-lengthening nails reveal differences in bone abnormalities between different nail types. Bone Jt. J. 2021, 103-B, 1731–1735. [Google Scholar] [CrossRef]
- Jellesen, M.S.; Lomholt, T.N.; Hansen, R.Q.; Mathiesen, T.; Gundlach, C.; Kold, S.; Nygaard, T.; Mikuzis, M.; Olesen, U.K.; Rolfing, J.D. The STRYDE limb lengthening nail is susceptible to mechanically assisted crevice corrosion: An analysis of 23 retrieved implants. Acta Orthop. 2021, 92, 621–627. [Google Scholar] [CrossRef]
- Paley, D. Surgical reconstruction for fibular hemimelia. J. Child. Orthop. 2016, 10, 557–583. [Google Scholar] [CrossRef]
- Horn, J.; Steen, H.; Huhnstock, S.; Hvid, I.; Gunderson, R.B. Limb lengthening and deformity correction of congenital and acquired deformities in children using the Taylor Spatial Frame. Acta Orthop. 2017, 88, 334–340. [Google Scholar] [CrossRef] [PubMed]
- Tsuchiya, H.; Uehara, K.; Abdel-Wanis, M.E.; Sakurakichi, K.; Kabata, T.; Tomita, K. Deformity correction followed by lengthening with the Ilizarov method. Clin. Orthop. Relat. Res. 2002, 402, 176–183. [Google Scholar] [CrossRef] [PubMed]
- Iobst, C.; Liu, R. A systematic review of incidence of pin track infections associated with external fixation. J. Limb Lengthening Reconstr. 2016, 2, 6–16. [Google Scholar] [CrossRef]
- Bue, M.; Bjarnason, A.O.; Rolfing, J.D.; Larsen, K.; Petruskevicius, J. Prospective evaluation of pin site infections in 39 patients treated with external ring fixation. J. Bone Jt. Infect. 2021, 6, 135–140. [Google Scholar] [CrossRef] [PubMed]
- Hafez, M.; Nicolaou, N.; Offiah, A.; Offorha, B.; Giles, S.; Madan, S.; Fernandes, J.A. Quality of life of children during distraction osteogenesis: A comparison between intramedullary magnetic lengthening nails and external fixators. Int. Orthop. 2022, 46, 1367–1373. [Google Scholar] [CrossRef] [PubMed]
- Stevens, P.M. The role of guided growth as it relates to limb lengthening. J. Child. Orthop. 2016, 10, 479–486. [Google Scholar] [CrossRef]
- Burghardt, R.D.; Paley, D.; Specht, S.C.; Herzenberg, J.E. The effect on mechanical axis deviation of femoral lengthening with an intramedullary telescopic nail. J. Bone Jt. Surg. Br. 2012, 94, 1241–1245. [Google Scholar] [CrossRef]
- Wagner, P.; Burghardt, R.D.; Green, S.A.; Specht, S.C.; Standard, S.C.; Herzenberg, J.E. PRECICE((R)) magnetically-driven, telescopic, intramedullary lengthening nail: Pre-clinical testing and first 30 patients. SICOT J. 2017, 3, 19. [Google Scholar] [CrossRef]
- Baumgart, R. The reverse planning method for lengthening of the lower limb using a straight intramedullary nail with or without deformity correction. A new method. Oper. Orthop. Traumatol. 2009, 21, 221–233. [Google Scholar] [CrossRef]
| Etiology | n |
|---|---|
| Fibular hemimelia | 9 |
| Congenital femoral deficiency | 6 |
| Idiopathic | 2 |
| Posttraumatic | 2 |
| Hereditary multiple exostoses | 2 |
| Enchondromatosis | 1 |
| Idiopathic hemihypertrophy | 1 |
| Klippel–Trenaunay syndrome | 1 |
| Congenital hip dislocation | 1 |
| Initial MAD (mm) | MAD after HED (mm) | MAD at Skeletal Maturity (mm) | Initial mLDFA (°) | mLDFA after HED (°) | mLDFA at Skeletal Maturity (°) | Initial MPTA (°) | MPTA after HED (°) | MPTA at Skeletal Maturity (°) | |
|---|---|---|---|---|---|---|---|---|---|
| Valgus deformity | |||||||||
| n = 21 | −26.5 (±11.8) | +2.3 (±13.1) | 81.8 (±5.3) | 89.3 (±4.7) | 91.4 (±4.9) | 88.6 (±3.2) | |||
| n = 17 | −7.2 (±15.3) | 86.8 (±5.0) | 88.9 (±3.0) | ||||||
| Varus deformity | |||||||||
| n = 4 | +30.0 (±16.1) | +2.3 (±14.2) | +15.5 (±11.3) | 94.0 (±7.6) | 85.0 (±3.4) | 88.8 (±2.6) | 84.3 (±4.2) | 84.8 (±3.4) | 84.3 (±3.1) |
| Lengthening Nail Implantation | Flexible Staple Implantation | Combined Implantation | |
|---|---|---|---|
| Incision-suture time (minutes) | 101.6 (±35.9) | 28.5 (26.3–37.5) | 156.5 (±62.5) |
| Hospitalization time (days) | 8.1 (±3.8) | 2.9 (±1.0) | 8.9 (±4.1) |
| LLD at Surgery (mm) | Predicted LLD at Skeletal Maturity (mm) | LLD after Implant Retrieval (mm) | LLD after Skeletal Maturity (mm) | |
|---|---|---|---|---|
| n = 25 | 39.0 (35.0–45.0) | 44.5 (37.5–58.3) | 4.0 (0.0–8.3) | |
| n = 21 | 10.0 (0.0–12.3) |
| Number | Type of Complication | Resolved by | Permanent Sequalae | |
|---|---|---|---|---|
| Major complications (n = 6 in 5 patients) | 2 | Premature consolidation | Reosteotomy | None |
| 2 | Fracture of the femur | Exchange nailing | None | |
| 1 | Deep infection | Retrieval of the lengthening nail, external fixation | Pain, restricted range of movement | |
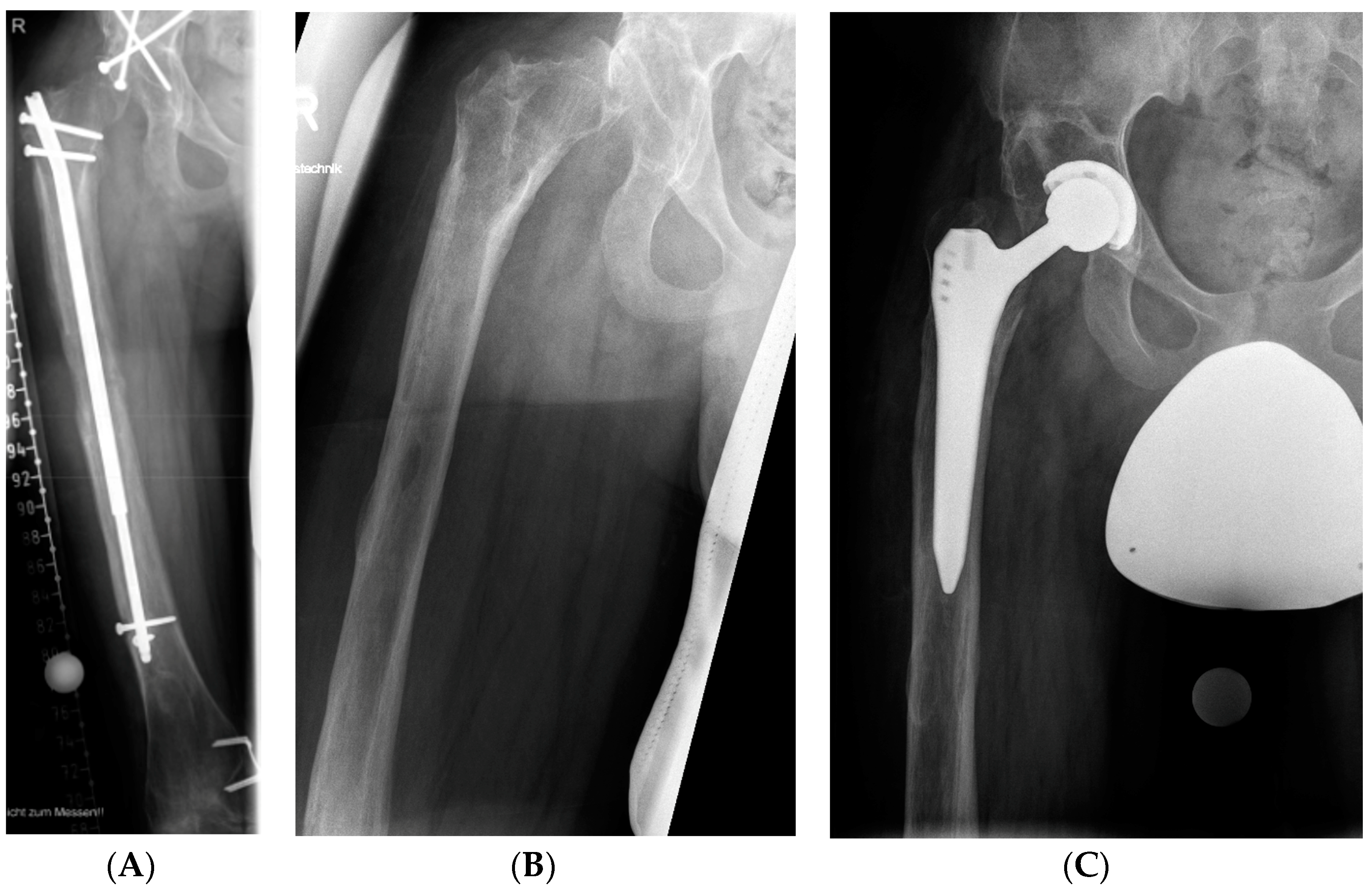
| 1 | Hip subluxation | Total hip arthroplasty | ||
| Minor complications (n = 3 in 3 patients) | 2 | Knee flexion contracture | Reduction of distraction rate Temporary retraction of the lengthening nail | None |
| 1 | Premature consolidation | Acute lengthening of 5 mm under sedation | None |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Laufer, A.; Frommer, A.; Gosheger, G.; Toporowski, G.; Rölfing, J.D.; Antfang, C.; Roedl, R.; Vogt, B. Antegrade Intramedullary Femoral Lengthening and Distal Temporary Hemiepiphysiodesis for Combined Correction of Leg Length Discrepancy and Coronal Angular Deformity in Skeletally Immature Patients. J. Clin. Med. 2023, 12, 3022. https://doi.org/10.3390/jcm12083022
Laufer A, Frommer A, Gosheger G, Toporowski G, Rölfing JD, Antfang C, Roedl R, Vogt B. Antegrade Intramedullary Femoral Lengthening and Distal Temporary Hemiepiphysiodesis for Combined Correction of Leg Length Discrepancy and Coronal Angular Deformity in Skeletally Immature Patients. Journal of Clinical Medicine. 2023; 12(8):3022. https://doi.org/10.3390/jcm12083022
Chicago/Turabian StyleLaufer, Andrea, Adrien Frommer, Georg Gosheger, Gregor Toporowski, Jan Duedal Rölfing, Carina Antfang, Robert Roedl, and Bjoern Vogt. 2023. "Antegrade Intramedullary Femoral Lengthening and Distal Temporary Hemiepiphysiodesis for Combined Correction of Leg Length Discrepancy and Coronal Angular Deformity in Skeletally Immature Patients" Journal of Clinical Medicine 12, no. 8: 3022. https://doi.org/10.3390/jcm12083022
APA StyleLaufer, A., Frommer, A., Gosheger, G., Toporowski, G., Rölfing, J. D., Antfang, C., Roedl, R., & Vogt, B. (2023). Antegrade Intramedullary Femoral Lengthening and Distal Temporary Hemiepiphysiodesis for Combined Correction of Leg Length Discrepancy and Coronal Angular Deformity in Skeletally Immature Patients. Journal of Clinical Medicine, 12(8), 3022. https://doi.org/10.3390/jcm12083022





