Corrective Osteotomies in Severe Non-Idiopathic Lower Limb Alignment Disorders in the Aspect of Future Joint Endoprosthesis—A Perspective Study
Abstract
1. Introduction
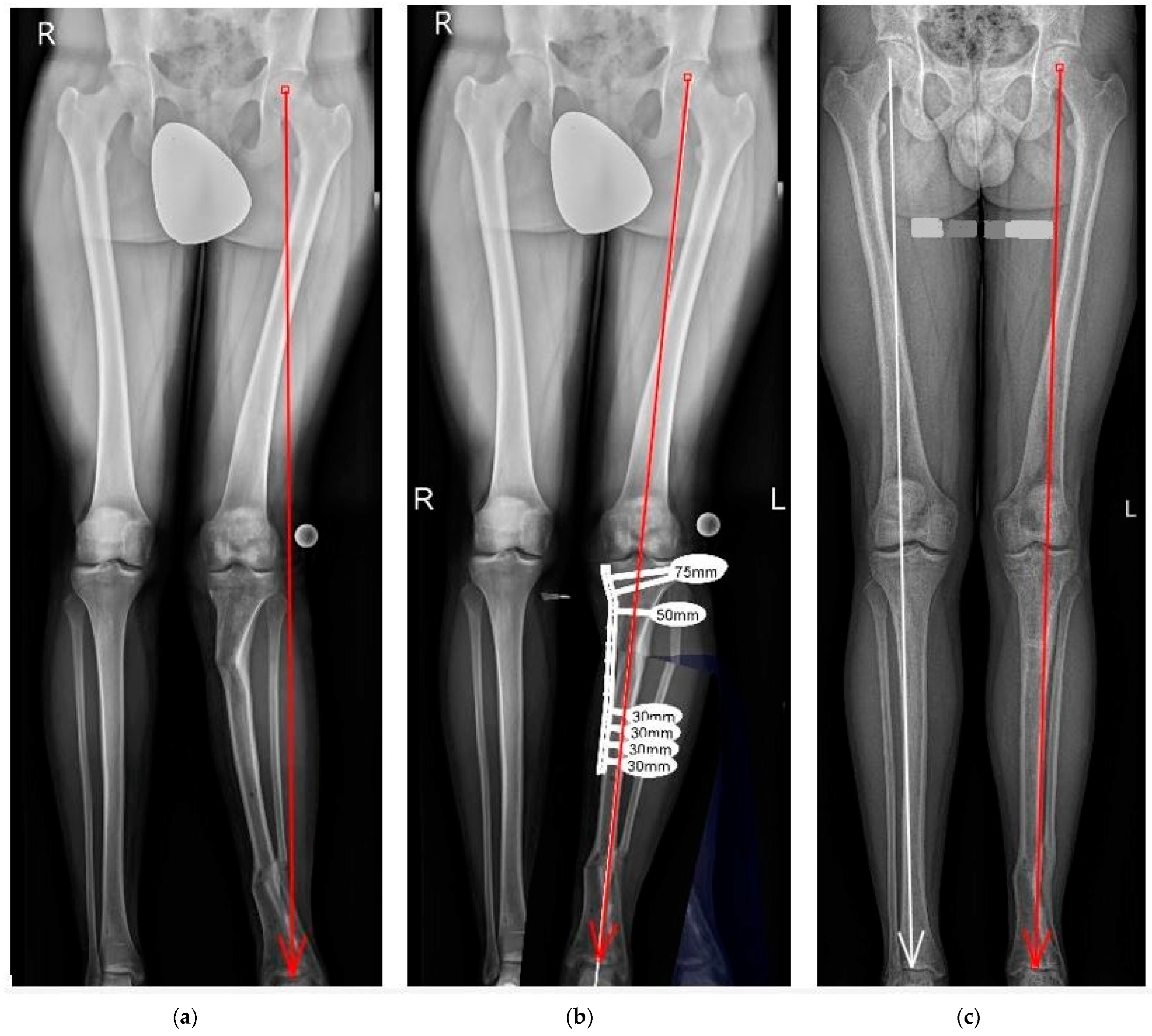
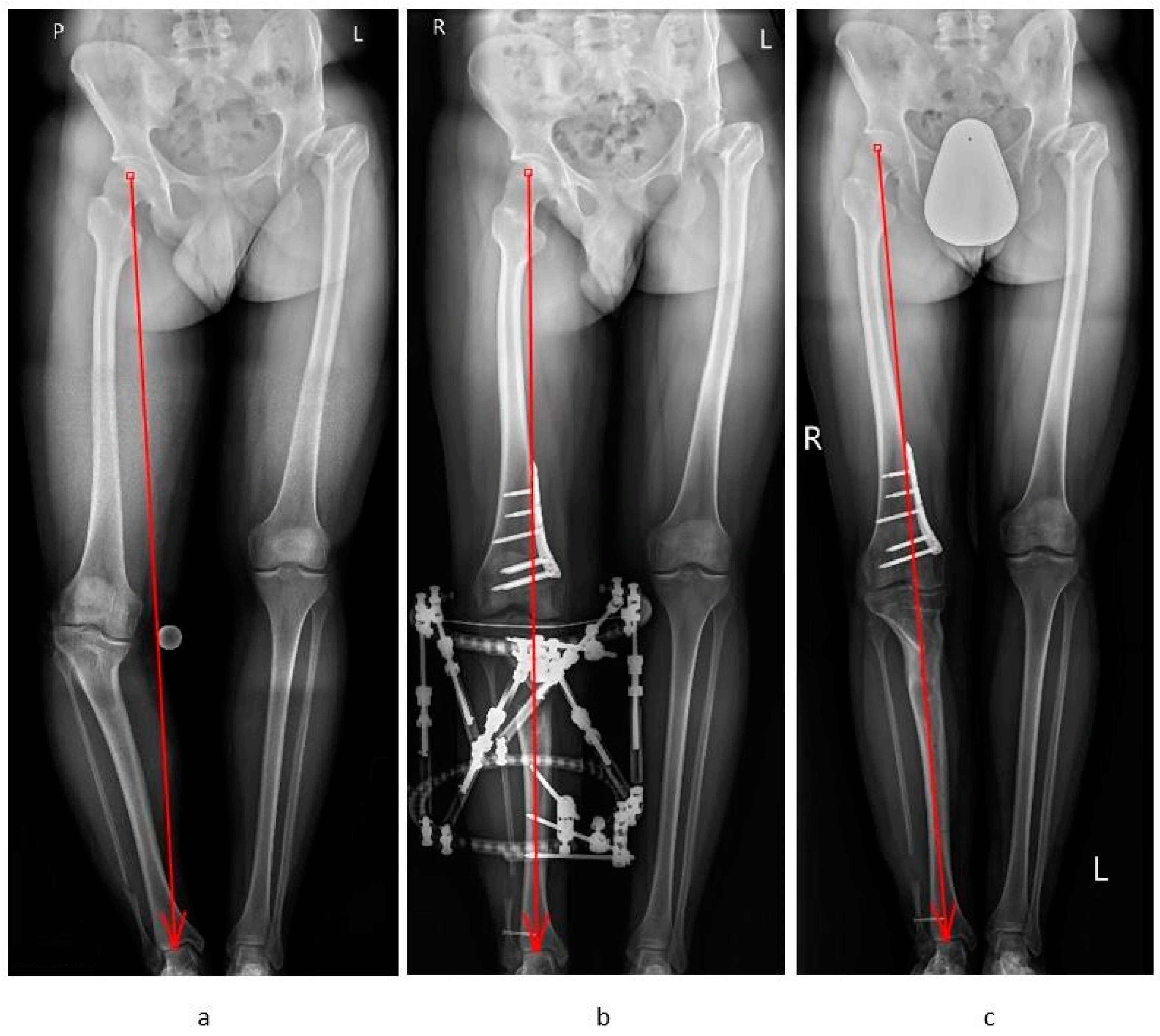
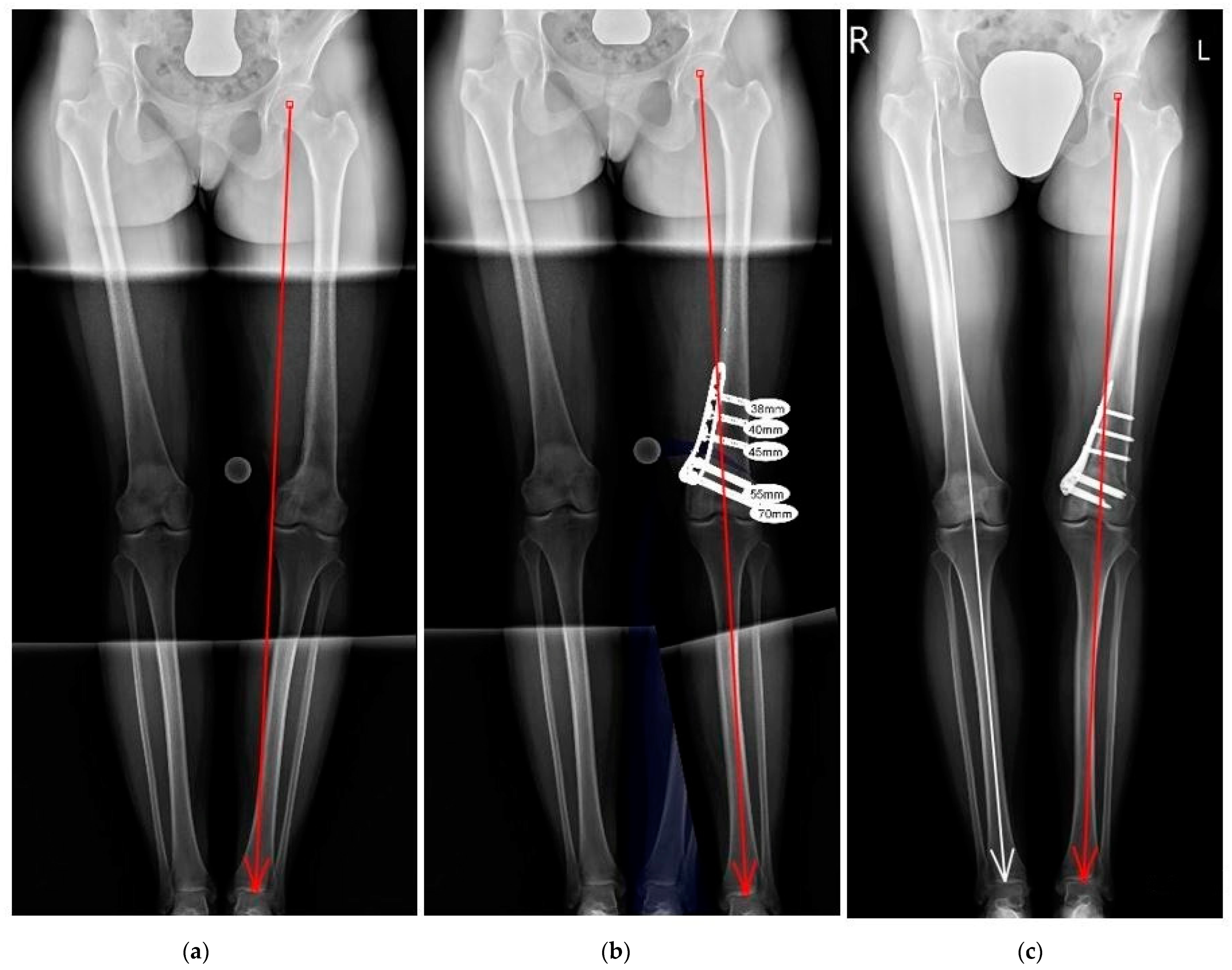
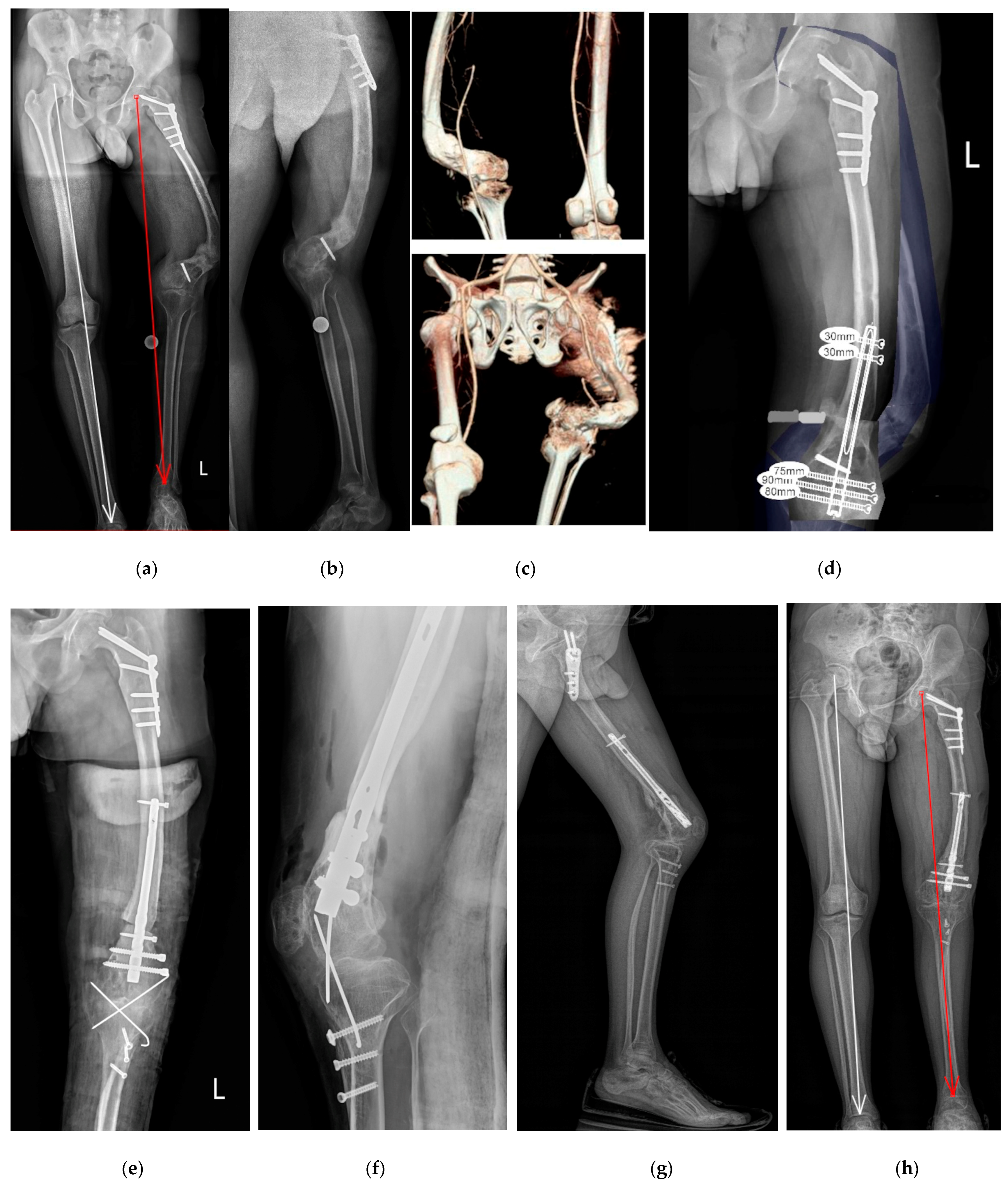
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| DFO | distal femur osteotomy |
| HTO | high tibia osteotomy |
| PTO | proximal tibia osteotomy |
| MOW | medial open wedge |
| LCW | lateral close wedge |
| JLCA | joint line convergence angle |
| CWO | combined wedge osteotomy |
| TSF | Taylor Spatial Frame |
| LCP | locking plate |
| IM | intramedullary nail |
| AP | antero-posterior |
References
- Liu, X.; Chen, Z.; Gao, Y.; Zhang, J.; Jin, Z. High Tibial Osteotomy: Review of Techniques and Biomechanics. J. Healthc. Eng. 2019, 2019, 8363128. [Google Scholar] [CrossRef] [PubMed]
- Lee, B.S.; Kim, T.H.; Bin, S.I.; Kim, J.M.; Kim, H. Clinic radiologic Outcomes of Medial Open-Wedge High-Tibial Osteotomy Are Equivalent in Bone-on-Bone and Non-Bone-on-Bone Medial Osteoarthritis. Arthroscopy 2021, 37, 638–644. [Google Scholar] [CrossRef] [PubMed]
- Cao, Z.; Mai, X.; Wang, J.; Feng, E.; Huang, Y. Unicompartmental Knee Arthroplasty vs High Tibial Osteotomy for Knee Osteoarthritis: A Systematic Review and Meta-Analysis. J. Arthroplast. 2018, 33, 952–959. [Google Scholar] [CrossRef] [PubMed]
- Luis, M.; Varatojo, R. Radiological assessment of lower limb alignment. EFORT Open Rev. 2021, 6, 487–494. [Google Scholar] [CrossRef]
- Paley, D. Normal Lower Limb Alignment and Joint Orientation. In Principles of Deformity Correction; Springer: Berlin/Heidelberg, Germany, 2002; pp. 1–18. [Google Scholar]
- Zak, L.; Tiefenboeck, T.M.; Wozasek, G.E. Computed Tomography in Limb Salvage and Deformity Correction—3D Assessment, Indications, Radiation Exposure, and Safety Considerations. J. Clin. Med. 2021, 10, 3781. [Google Scholar] [CrossRef]
- Bae, D.K.; Park, C.H.; Kim, E.J.; Song, S.J. Medial cortical fractures in computer-assisted closing-wedge high tibial osteotomy. Knee 2016, 23, 295–299. [Google Scholar] [CrossRef]
- Song, S.J.; Bae, D.K. Computer-Assisted Navigation in High Tibial Osteotomy. Clin. Orthop. Surg. 2016, 8, 349–357. [Google Scholar] [CrossRef]
- Iorio, R.; Pagnottelli, M.; Vadala, A.; Giannetti, S.; Di Sette, P.; Papandrea, P.; Conteduca, F.; Ferretti, A. Open-wedge high tibial osteotomy: Comparison between manual and computer-assisted techniques. Knee Surg. Sports Traumatol. Arthrosc. 2013, 21, 113–119. [Google Scholar] [CrossRef]
- Picardo, N.E.; Khan, W.; Johnstone, D. Computer-assisted navi- gation in high tibial osteotomy: A systematic review of the literature. Open Orthop. J. 2012, 6, 305–312. [Google Scholar] [CrossRef]
- Bakircioglu, S.; Caglar, O.; Yilmaz, G. Multiplanar correction of proximal tibial recurvatum deformity with tibial osteotomy and computer assisted fixator. Knee 2021, 32, 159–165. [Google Scholar] [CrossRef]
- Chung, J.H.; Choi, C.H.; Kim, S.H.; Kim, S.J.; Suk, Y.J.; Jung, M. Effect of the sagittal osteotomy inclination angle on the posterior tibial slope change in high tibial osteotomy: Three-dimensional simulation study. Sci. Rep. 2022, 12, 19254. [Google Scholar] [CrossRef] [PubMed]
- Hoell, S.; Suttmoeller, J.; Stoll, V.; Fuchs, S.; Gosheger, G. The high tibial osteotomy, open versus closed wedge, a comparison of methods in 108 patients. Arch. Orthop. Trauma Surg. 2005, 125, 638–643. [Google Scholar] [CrossRef] [PubMed]
- Nakayama, H.; Schröter, S.; Yamamoto, C.; Iseki, T.; Kanto, R.; Kurosaka, K.; Kam-bara, S.; Yoshiya, S.; Higa, M. Large correction in opening wedge high tibial osteotomy with resultant joint-line obliquity induces excessive shear stress on the articular cartilage. Knee Surg. Sports Traumatol. Arthrosc. 2018, 26, 1873–1878. [Google Scholar] [CrossRef]
- Nejima, S.; Kumagai, K.; Yamada, S.; Sotozawa, M.; Kumagai, D.; Yamane, H.; Inaba, Y. Potential anatomic risk factors resulting oversized postoperative medial proximal tibial angle after double level osteotomy. BMC Musculoskelet. Disord. 2022, 23, 1121. [Google Scholar] [CrossRef]
- Huizinga, M.R.; Brouwer, R.W.; van Raaij, T.M. High tibial osteotomy: Closed wedge versus combined wedge osteotomy. BMC Musculoskelet. Disord. 2014, 15, 124. [Google Scholar] [CrossRef] [PubMed]
- Gaasbeek, R.; Welsing, R.; Barink, M.; Verdonschot, N.; van Kampen, A. The influence of open and closed high tibial osteotomy on dynamic patellar tracking: A biomechanical study. Knee Surg. Sports Traumatol. Arthrosc. 2007, 15, 978–984. [Google Scholar] [CrossRef] [PubMed]
- Hinterwimmer, S.; Beitzel, K.; Paul, J.; Kirchhoff, C.; Sauerschnig, M.; von Eisenhart-Rothe, R.; Imhoff, A.B. Control of pos-terior tibial slope and patellar height in open-wedge valgus high tibial osteotomy. Am. J. Sports Med. 2011, 39, 851–856. [Google Scholar] [CrossRef] [PubMed]
- Kloos, F.; Becher, C.; Fleischer, B.; Feucht, M.J.; Hohloch, L.; Südkamp, N.; Niemeyer, P.; Bode, G. High tibial osteotomy increases patellofemoral pressure if adverted proximal, while open-wedge HTO with distal biplanar osteotomy discharges the patellofemoral joint: Different open-wedge high tibial osteotomies compared to an extra-articular unloading device. Knee Surg. Sports Traumatol. Arthrosc. 2019, 27, 2334–2344. [Google Scholar]
- Wahab, H.; Fahad, S.; Noor-Us-Sabah, T.A.; Mohib, Y.; Ur Rashid, H.; Umer, M. Correction of lower limb deformities with fixator assisted nailing. Ann. Med. Surg. 2019, 45, 40–44. [Google Scholar] [CrossRef]
- Kariksiz, M.; Karakoyun, O. Acute correction of distal femoral deformities by retrograde femoral nail using preoperative planning. J. Orthop. Surg. 2022, 30, 10225536221143552. [Google Scholar] [CrossRef]
- Pietrzak, S.; Grzelecki, D.; Parol, T.; Czubak, J. Comparison of Intramedullaryy Magnetic Nail, Monolateral External Distractor, and Spatial External Fixator in Femur Lengthening in Adolescents with Congenital Diseases. J. Clin. Med. 2021, 10, 5957. [Google Scholar] [CrossRef] [PubMed]
- Laufer, A.; Frommer, A.; Gosheger, G.; Toporowski, G.; Duedal Rölfing, J.; Antfang, C.; Roedl, R.; Vogt, B. Antegrade Intramedullaryy Femoral Lengthening and Distal Temporary Hemiepiphysiodesis for Combined Correction of Leg Length Discrepancy and Coronal Angular Deformity in Skeletally Immature Patients. J. Clin. Med. 2023, 12, 3022. [Google Scholar] [CrossRef] [PubMed]
- Dessyn, E.; Sharma, A.; Donnez, M.; Chabrand, P.; Ehlinger, M.; Argenson, J.N.; Parratte, S.; Ollivier, M. Adding a protective K-wire during opening high tibial osteotomy increases lateral hinge resistance to fracture. Knee Surg. Sports Traumatol. Arthrosc. 2020, 28, 751–758. [Google Scholar] [CrossRef]
- Zak, L.; Tiefenboeck, T.M.; Wozasek, G.E. Traumatic periimplant fracture after nail arthrodesis of the knee in a limb reconstruction case. Trauma Case Rep. 2019, 20, 100173. [Google Scholar] [CrossRef] [PubMed]
- Powel, K.; Hammound, A.; Hlukha, L.; Rivera, J.; Patel, M.; Rozbruch, S.; Conway, J.; Herzenberg, J. Motorized Intramedullaryy Nail Lengthening in the Older Population. J. Clin. Med. 2022, 11, 5242. [Google Scholar] [CrossRef]
- Bei, T.; Yang, L.; Huang, Q.; Wu, J.; Liu, J. Effectiveness of bone substitute materials in opening wedge high tibial osteotomy: A systematic review and meta-analysis. Ann. Med. 2022, 54, 565–577. [Google Scholar] [CrossRef]
- Seagrave, R.A.; Sojka, J.; Goodyear, A.; Munns, S.W. Utilizing reamer irrigator aspirator (RIA) autograft for opening wedge high tibial osteotomy: A new surgical technique and report of three cases. Int. J. Surg. Case Rep. 2014, 5, 37–42. [Google Scholar] [CrossRef][Green Version]
- Jones, G.G.; Clarke, S.; Jaere, M.; Cobb, J.P. Failed high tibial osteotomy: A joint preserving alternative to total knee arthroplasty. Orthop. Traumatol. Surg. Res. 2019, 105, 85–88. [Google Scholar] [CrossRef]
- Kulinski, K.; Trams, E.; Pomianowski St Kaminski, R. Osteotomies and Total Knee Arthroplasty: Systematic Review and Meta-Analysis. Life 2022, 12, 1120. [Google Scholar] [CrossRef]
- Iseki, T.; Onishi, S.; Kanto, M.; Kanto, R.; Kambara, S.; Yoshiya, S.; Tachibana, T.; Nakayama, H. Double-level osteotomy for severe varus osteoarthritic knees can prevent change in leg length and restore physiological joint geometry. Knee 2021, 31, 136–143. [Google Scholar] [CrossRef]
| GROUP A—Femur Segment Alignment Disorder | GROUP B—Tibia Segment Alignment Disorder | GROUP C—Femur and Tibia Segment Alignment Disorder | TOTAL | |
|---|---|---|---|---|
| Mean age (year) | 47 (18–86) | 44 (18–72) | 38 (18–52) | 45 (18–86) |
| Sex | 5 Female 19 Male | 4 Female 14 Male | 4 Female 4 Male | 13 Female 37 Male |
| Patient number | 24 | 18 | 8 | 50 |
| Operation side | 13 Right 11 Left | 12 Right 6 Left | 4 Right 4 Left | 29 Right 21 Left |
| Etiology | Post-traumatic 15; Other 9: Fibrous dysplasia 3, Congenital femur diseases 2, Fibular hemimelia 2, Post septic 2 | Post-traumatic 14; Other 4: Fibular hemimelia 3, Ollier disease 1 | Other 8: Blount diseases 6, Fibular hemimelia 1, Post septic 2 | Post-traumatic: 29; Other: 21 |
| Deformity | Varus: 20 Valgus: 3 Torsion: 11 Shortening: 1 Sagittal: 7 | Varus: 8 Valgus: 8 Torsion: 9 Shortening: 3 Sagittal: 6 | Varus: 7 Valgus: 8 Shortening: 1 | Varus: 35 Valgus: 19 Torsion: 20 Shortening: 5 Sagittal: 13 |
| Osteotomy level | PFO: 9 Femur shaft: 6 DFO: 9 | PTO: 6 Tibia shaft: 3 DTO: 9 | DFO: 7 PTO: 8 Femur shaft: 1 | PFO: 9 Shaft f: 7 DFO: 16 PTO: 14 Shaft t: 3 DTO: 9 |
| Osteosynthesis | LCP: 10 Intramedullary nail: 15 | LCP: 6 Intramedullary nail: 11 TSF: 2 | LCP: 10 Intramedullary nail: 1 TSF: 3 | LCP: 26 Intramedullary nail: 27 TSF: 5 |
| Deformation duration (mean months) | 150.7 (±103.5) | 184.5 (±76.4) | 200.6 (±60.3) | 170.7 (±89.5) |
| Operative time (mean minutes) | 162 (±61.9) | 156.3 (±52.9) | 158.7 (±16.4) | 159.4 (±53.2) |
| Time to bone union (mean months) | 7.44 (±3.5) | 7.05 (±2.5) | 4.1 (±0.84) | 6.7 (±3.11) |
| Complication: | 2 (Destabilization, non-union) | 2 (Infection) | 0 | 4 |
| Follow-up (mean months) | 53.5 (±18.7) | 57.8 (±15.7) | 58 (±19.8) | 55.8 (±17.6) |
| Femur Varus Alignment Disorders (Mean) n = 22 | Pre-Operation SD (95% CI) | Post-Operation SD (95% CI) | Diff. | p-Value |
|---|---|---|---|---|
| mLPFA (80–90 deg) | 102.5 ± 11.5 (90–127.5) | 91.5 ± 5.3 (80–102) | −11.0 | <0.005 |
| mLDFA (85–90 deg) | 94.5 ± 8.7 (81.5–117) | 90.0 ± 1.7 (87–93) | −4.5 | 0.01 |
| CORA coronal | 29.5 ± 19.7 (11.5–80.5) | 5.0 ± 9.0 (0–36.0) | −24.5 | <0.005 |
| CORA sagittal | 8.0 ± 16.5 (0–64.0) | 1.0 ± 4.0 (0–20.0) | −7.0 | 0.03 |
| MAD (10–15 mm) | 26.5 ± 17.0 (5.0–65.0) | 7.0 ± 8.0 (0–28.0) | −19.5 | <0.005 |
| Femur Valgus Alignment Disorders (Mean) n = 10 | Pre-Operation SD (95% CI) | Post-Operation SD (95% CI) | Diff. | p-Value |
|---|---|---|---|---|
| mLPFA (85–90 deg) | 81.0 ± 7.62 (64.0–89.0) | 84.0 ± 8.0 (67.5–89) | 3.0 | 0.18 |
| mLDFA (85–90 deg) | 75.5 ± 4.6 (67.0–81.0) | 87.5 ± 2.63 (83.5–91.5) | 12.0 | <0.005 |
| CORA coronal | −12.5 ± 4.5 (−7.5–−20.0) | 0.05 ± 1.82 (−2.5–2.5) | 12.55 | <0.005 |
| CORA sagittal | 0.0 | 0.0 | 0 | 1 |
| MAD (10–15 mm) | −26.5 ± 8.1 (−16.0–−40.0) | 4.5 ± 7.3 (−6.0–15.0) | 31.0 | <0.005 |
| Tibia Varus Alignment Disorders (Mean) n = 14 | Pre-Operation SD (95% CI) | Post-Operation SD (95% CI) | Diff. | p-Value |
|---|---|---|---|---|
| mMPTA (85–90 deg) | 78.5 ± 9.1 (63.0–89.5) | 88.0 ± 2.5 (82.5–90.0) | 9.5 | <0.005 |
| mLDTA (86–92 deg) | 100.5 ± 14.1 (76.0–124.0) | 92.0 ± 4.2 (89.0–99.0) | −8.5 | 0.02 |
| CORA coronal | 22.5 ± 7.7 (10.0–33.0) | 2.0 ± 2.8 (0–6.5) | −20.5 | <0.005 |
| CORA sagittal | 9.5 ± 13.3 (0–40) | 1.5 ± 4.6 (0–15.5) | −8.0 | 0.02 |
| MAD (10–15 mm) | 40.5 ± 20.7 (22.0–95.0) | 9.5 ± 6.24 (2.0–20.0) | −31.0 | <0.005 |
| Tibia Valgus Alignment Disorders (Mean) n = 10 | Pre-Operation SD (95% CI) | Post-Operation SD (95% CI) | Diff. | p-Value |
|---|---|---|---|---|
| mMPTA (85–90 deg) | 92.0 ± 5.4 (81.5–101.0) | 89.5 ± 3.1 (86.0–96.5) | −2.5 | 0.11 |
| mLDTA (86–92 deg) | 82.0 ± 8.2 (65.5–93.0) | 86.0 ± 4.8 (78.0–93.0) | 4.0 | 0.103 |
| CORA coronal | −14.0 ± 4.9 (−8.0–−21.0) | −0.5 ± 1.9 (−4.2–3.0) | 13.5 | <0.005 |
| CORA sagittal | 5.0 ± 14.5 (−12.0–36.5) | 1.5 ± 5.2 (−8.0–12.0) | −3.5 | 0.26 |
| MAD (10–15 mm) | −25.0 ± 6.7 (−34.0–−17.0) | 3.0 ± 5.4 (−5.0–10.0) | 28.0 | <0.005 |
| Patient Group Comparison | Deformation Duration (mth) (p-Value) | Operative Time (min) (p-Value) | Time to Bone Union (mth) (p-Value) | Follow-Up (mth) (p-Value) |
|---|---|---|---|---|
| Group A/B | 150.7 ± 103.5/184.5 ± 76.4 (p = 0.110) | 162 ± 61.9/156.3 ± 52.9 (p = 0.372) | 7.44 ± 3.5/7.05 ± 2.5 (p = 0.337) | 53.5 ± 18.7/57.8 ± 15.7 (p = 0.202) |
| Group B/C | 184.5 ± 76.4/200.6 ± 60.3 (p = 0.283) | 156.3 ± 52.9/158.7 ± 16.4 (p = 0.429) | 7.05 ± 2.5/4.1 ± 0.84 (p < 0.005) | 57.8 ± 15.7/58 ± 19.8 (p = 0.494) |
| Group A/C | 150.7 ± 103.5/200.6 ± 60.3 (p = 0.054) | 162 ± 61.9/158.7 ±16.4 (p = 0.406) | 7.44 ± 3.5/4.1 ± 0.84 (p < 0.005) | 53.5 ± 18.7/58 ± 19.8 (p = 0.292) |
| LLFI (Mean) | Pre-Operation SD (95% CI) | Post-Operation SD (95% CI) | Diff. | p-Value |
|---|---|---|---|---|
| Group A | 31.8 ± 4.8 (24.0–42.0) | 72.3 ± 5.8 (55.0–80.0) | 40.5 | <0.005 |
| Group B | 39.4 ± 9.5 (25.0–58.0) | 70.1 ± 6.8 (59.0–79.0) | 30.67 | <0.005 |
| Group C | 36.7 ± 5.4 (30.0–45.0) | 74 ± 3.6 (69.0–79.0) | 37.25 | <0.005 |
| LLFI (Mean) | Varus Femur n = 22 | Valgus Femur n = 10 | Diff. | p-Value |
|---|---|---|---|---|
| Pre-operation SD (95% CI) | 32.0 ± 5.5 (24.0–45.0) | 35.8 ± 4.6 (30.0–42.0) | 3.8 | 0.02 |
| Post-operation SD (95% CI) | 72.5 ± 6.0 (55.0–80.0) | 73.8 ± 3.99 (68.0–79.0) | 1.3 | 0.28 |
| Varus Tibia n = 14 | Valgus Tibia n = 10 | |||
| Pre-operation SD (95% CI) | 35.3 ± 5.8 (25.0–46.0) | 42.0 ± 10.3 (25.0–45.0) | 6.7 | 0.04 |
| Post-operation SD (95% CI) | 71.7 ± 5.6 (63.0–79.0) | 71 ± 7.8 (59.0–79.0) | 0.7 | 0.37 |
| LLFI (Mean) | Varus Femur n = 22 | Varus Tibia n = 14 | Diff. | p-Value |
|---|---|---|---|---|
| Pre-operation SD (95% CI) | 32.0 ± 5.5 (24.0–45.0) | 35.3 ± 5.8 (25.0–46.0) | 3.3 | 0.04 |
| Post-operation SD (95% CI) | 72.5 ± 6.0 (55.0–80.0) | 71.7 ± 5.6 (63.0–79.0) | 0.8 | 0.3 |
| Valgus Femur n = 10 | Valgus Tibia n = 10 | |||
| Pre-operation SD (95% CI) | 35.8 ± 4.6 (30.0–42.0) | 42.0 ± 10.3 (25.0–45.0) | 6.2 | 0.052 |
| Post-operation SD (95% CI) | 73.8 ± 3.99 (68.0–79.0) | 71 ± 7.8 (59.0–79.0) | 2.8 | 0.14 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kołodziejczyk, K.; Saganek, M.; Czwojdziński, A.; Garlewicz, R.; Złotorowicz, M.; Czubak, J. Corrective Osteotomies in Severe Non-Idiopathic Lower Limb Alignment Disorders in the Aspect of Future Joint Endoprosthesis—A Perspective Study. J. Clin. Med. 2023, 12, 6380. https://doi.org/10.3390/jcm12196380
Kołodziejczyk K, Saganek M, Czwojdziński A, Garlewicz R, Złotorowicz M, Czubak J. Corrective Osteotomies in Severe Non-Idiopathic Lower Limb Alignment Disorders in the Aspect of Future Joint Endoprosthesis—A Perspective Study. Journal of Clinical Medicine. 2023; 12(19):6380. https://doi.org/10.3390/jcm12196380
Chicago/Turabian StyleKołodziejczyk, Kamil, Michał Saganek, Adam Czwojdziński, Rafał Garlewicz, Marcin Złotorowicz, and Jarosław Czubak. 2023. "Corrective Osteotomies in Severe Non-Idiopathic Lower Limb Alignment Disorders in the Aspect of Future Joint Endoprosthesis—A Perspective Study" Journal of Clinical Medicine 12, no. 19: 6380. https://doi.org/10.3390/jcm12196380
APA StyleKołodziejczyk, K., Saganek, M., Czwojdziński, A., Garlewicz, R., Złotorowicz, M., & Czubak, J. (2023). Corrective Osteotomies in Severe Non-Idiopathic Lower Limb Alignment Disorders in the Aspect of Future Joint Endoprosthesis—A Perspective Study. Journal of Clinical Medicine, 12(19), 6380. https://doi.org/10.3390/jcm12196380





