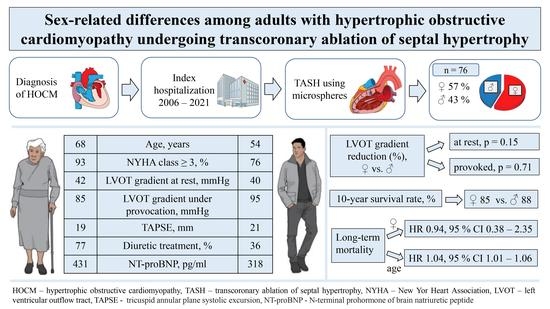
Sex-Related Differences among Adults with Hypertrophic Obstructive Cardiomyopathy Undergoing Transcoronary Ablation of Septal Hypertrophy
Abstract
1. Introduction
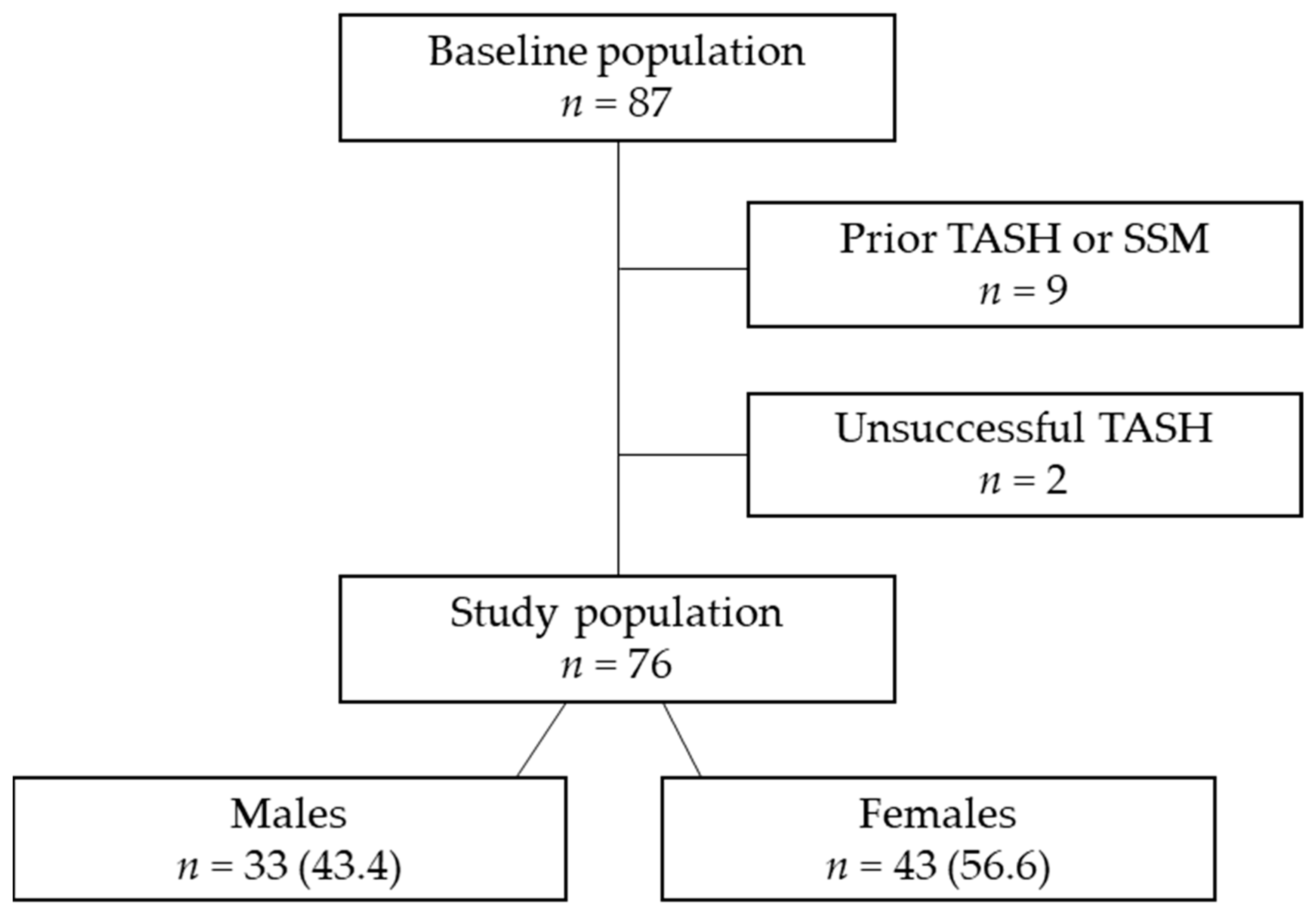
2. Materials and Methods
2.1. Study Population and Design
2.2. TASH Protocol and Non-Invasive Investigations
2.3. Statistical Analysis
3. Results
3.1. Baseline Characteristics
3.2. Periprocedural Outcomes
3.3. Long-Term Follow-up
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Pelliccia, F.; Limongelli, G.; Autore, C.; Gimeno-Blanes, J.R.; Basso, C.; Elliott, P. Sex-related differences in cardiomyopathies. Int. J. Cardiol. 2019, 286, 239–243. [Google Scholar] [CrossRef]
- Geske, J.B.; Ong, K.C.; Siontis, K.C.; Hebl, V.B.; Ackerman, M.J.; Hodge, D.O.; Miller, V.M.; Nishimura, R.A.; Oh, J.K.; Schaff, H.V.; et al. Women with hypertrophic cardiomyopathy have worse survival. Eur. Heart J. 2017, 38, 3434–3440. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.; Kim, B.; Choi, Y.J.; Lee, H.J.; Lee, H.; Park, J.B.; Lee, S.P.; Han, K.D.; Kim, Y.J.; Kim, H.K. Sex differences in the prognosis of patients with hypertrophic cardiomyopathy. Sci. Rep. 2021, 11, 4854. [Google Scholar] [CrossRef]
- Kubo, T.; Kitaoka, H.; Okawa, M.; Hirota, T.; Hayato, K.; Yamasaki, N.; Matsumura, Y.; Yabe, T.; Doi, Y.L. Gender-specific differences in the clinical features of hypertrophic cardiomyopathy in a community-based Japanese population: Results from Kochi RYOMA study. J. Cardiol. 2010, 56, 314–319. [Google Scholar] [CrossRef]
- Preveden, A.; Golubovic, M.; Bjelobrk, M.; Miljkovic, T.; Ilic, A.; Stojsic, S.; Gajic, D.; Glavaski, M.; Maier, L.S.; Okwose, N.; et al. Gender Related Differences in the Clinical Presentation of Hypertrophic Cardiomyopathy-An Analysis from the SILICOFCM Database. Medicina 2022, 58, 314. [Google Scholar] [CrossRef] [PubMed]
- Rowin, E.J.; Maron, M.S.; Wells, S.; Patel, P.P.; Koethe, B.C.; Maron, B.J. Impact of Sex on Clinical Course and Survival in the Contemporary Treatment Era for Hypertrophic Cardiomyopathy. J. Am. Heart Assoc. 2019, 8, e012041. [Google Scholar] [CrossRef]
- Ommen, S.R.; Mital, S.; Burke, M.A.; Day, S.M.; Deswal, A.; Elliott, P.; Evanovich, L.L.; Hung, J.; Joglar, J.A.; Kantor, P.; et al. 2020 AHA/ACC Guideline for the Diagnosis and Treatment of Patients With Hypertrophic Cardiomyopathy: Executive Summary: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation 2020, 142, e533–e557. [Google Scholar]
- Elliott, P.M.; Anastasakis, A.; Borger, M.A.; Borggrefe, M.; Cecchi, F.; Charron, P.; Hagege, A.A.; Lafont, A.; Limongelli, G.; Mahrholdt, H.; et al. 2014 ESC Guidelines on diagnosis and management of hypertrophic cardiomyopathy: The Task Force for the Diagnosis and Management of Hypertrophic Cardiomyopathy of the European Society of Cardiology (ESC). Eur. Heart J. 2014, 35, 2733–2779. [Google Scholar]
- Spirito, P.; Rossi, J.; Maron, B.J. Alcohol septal ablation: In which patients and why? Ann. Cardiothorac. Surg. 2017, 6, 369–375. [Google Scholar] [CrossRef] [PubMed]
- Affronti, A.; Pruna-Guillen, R.; Sandoval, E.; Pereda, D.; Alcocer, J.; Castellà, M.; Quintana, E. Surgery for Hypertrophic Obstructive Cardiomyopathy: Comprehensive LVOT Management beyond Septal Myectomy. J. Clin. Med. 2021, 10, 4397. [Google Scholar] [CrossRef]
- Embozene™ Color-Advanced Microspheres. Available online: https://www.bostonscientific.com/content/dam/Manuals/bz/current-rev-pt/50913186-01A_Embozene_eDFU_bz_s.pdf (accessed on 20 February 2023).
- Dickmann, B.; Baars, T.; Heusch, G.; Erbel, R. Transcoronary septal ablation in hypertrophic obstructive cardiomyopathy by embolizing microspheres. Eur. Heart J. 2013, 34, 2489. [Google Scholar] [CrossRef]
- Bandyopadhyay, D.; Chakraborty, S.; Amgai, B.; Kapadia, S.R.; Braunwald, E.; Naidu, S.S.; Kalra, A. Association of Hypertrophic Obstructive Cardiomyopathy With Outcomes Following Transcatheter Aortic Valve Replacement. JAMA Netw. Open 2020, 3, e1921669. [Google Scholar] [CrossRef]
- Desai, M.Y.; Alashi, A.; Popovic, Z.B.; Wierup, P.; Griffin, B.P.; Thamilarasan, M.; Johnston, D.; Svensson, L.G.; Lever, H.M.; Smedira, N.G. Outcomes in Patients With Obstructive Hypertrophic Cardiomyopathy and Concomitant Aortic Stenosis Undergoing Surgical Myectomy and Aortic Valve Replacement. J. Am. Heart Assoc. 2021, 10, e018435. [Google Scholar] [CrossRef] [PubMed]
- Lakdawala, N.K.; Olivotto, I.; Day, S.M.; Han, L.; Ashley, E.A.; Michels, M.; Ingles, J.; Semsarian, C.; Jacoby, D.; Jefferies, J.L.; et al. Associations Between Female Sex, Sarcomere Variants, and Clinical Outcomes in Hypertrophic Cardiomyopathy. Circ. Genom. Precis. Med. 2021, 14, e003062. [Google Scholar] [CrossRef]
- Gimeno, J.R.; Tomé-Esteban, M.; Lofiego, C.; Hurtado, J.; Pantazis, A.; Mist, B.; Lambiase, P.; McKenna, W.J.; Elliott, P.M. Exercise-induced ventricular arrhythmias and risk of sudden cardiac death in patients with hypertrophic cardiomyopathy. Eur. Heart J. 2009, 30, 2599–2605. [Google Scholar] [CrossRef] [PubMed]
- McLeod, C.J.; Ackerman, M.J.; Nishimura, R.A.; Tajik, A.J.; Gersh, B.J.; Ommen, S.R. Outcome of patients with hypertrophic cardiomyopathy and a normal electrocardiogram. J. Am. Coll. Cardiol. 2009, 54, 229–233. [Google Scholar] [CrossRef]
- Varnava, A.M.; Elliott, P.M.; Sharma, S.; McKenna, W.J.; Davies, M.J. Hypertrophic cardiomyopathy: The interrelation of disarray, fibrosis, and small vessel disease. Heart 2000, 84, 476–482. [Google Scholar] [CrossRef]
- Yang, H.; Woo, A.; Monakier, D.; Jamorski, M.; Fedwick, K.; Wigle, E.D.; Rakowski, H. Enlarged left atrial volume in hypertrophic cardiomyopathy: A marker for disease severity. J. Am. Soc. Echocardiogr. 2005, 18, 1074–1082. [Google Scholar] [CrossRef] [PubMed]
- Mahmod, M.; Raman, B.; Chan, K.; Sivalokanathan, S.; Smillie, R.W.; Samat, A.H.A.; Ariga, R.; Dass, S.; Ormondroyd, E.; Watkins, H.; et al. Right ventricular function declines prior to left ventricular ejection fraction in hypertrophic cardiomyopathy. J. Cardiovasc. Magn. Reson. 2022, 24, 36. [Google Scholar] [CrossRef] [PubMed]
- Butters, A.; Lakdawala, N.K.; Ingles, J. Sex Differences in Hypertrophic Cardiomyopathy: Interaction With Genetics and Environment. Curr. Heart Fail. Rep. 2021, 18, 264–273. [Google Scholar] [CrossRef] [PubMed]
- Lawrenz, T.; Lieder, F.; Bartelsmeier, M.; Leuner, C.; Borchert, B.; Meyer zu Vilsendorf, D.; Strunk-Mueller, C.; Reinhardt, J.; Feuchtl, A.; Stellbrink, C.; et al. Predictors of complete heart block after transcoronary ablation of septal hypertrophy: Results of a prospective electrophysiological investigation in 172 patients with hypertrophic obstructive cardiomyopathy. J. Am. Coll. Cardiol. 2007, 49, 2356–2363. [Google Scholar] [CrossRef]
- Vriesendorp, P.A.; Van Mieghem, N.M.; Vletter, W.B.; Ten Cate, F.J.; de Jong, P.L.; Schinkel, A.F.; Michels, M. Microsphere embolisation as an alternative for alcohol in percutaneous transluminal septal myocardial ablation. Neth. Heart J. 2013, 21, 245–248. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, A.; Schaff, H.V.; Hang, D.; Nishimura, R.A.; Geske, J.B.; Dearani, J.A.; Lahr, B.D.; Ommen, S.R. Surgical myectomy versus alcohol septal ablation for obstructive hypertrophic cardiomyopathy: A propensity score-matched cohort. J. Thorac. Cardiovasc. Surg. 2019, 157, 306–315.e3. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, A.; Schaff, H.V.; Hang, D.; Nishimura, R.A.; Geske, J.B.; Dearani, J.A.; Lahr, B.D.; Ommen, S.R. Long-term clinical outcome after alcohol septal ablation for obstructive hypertrophic cardiomyopathy: Results from the Euro-ASA registry. Eur. Heart J. 2016, 37, 1517–1523. [Google Scholar]
- Sawaya, F.J.; Louvard, Y.; Spaziano, M.; Morice, M.C.; Hage, F.; El-Khoury, C.; Roy, A.; Garot, P.; Hovasse, T.; Benamer, H. Short and long-term outcomes of alcohol septal ablation with the trans-radial versus the trans-femoral approach: A single center-experience. Int. J. Cardiol. 2016, 220, 7–13. [Google Scholar] [CrossRef]
- Saberi, S.; Cardim, N.; Yamani, M.; Schulz-Menger, J.; Li, W.; Florea, V.; Sehnert, A.J.; Kwong, R.Y.; Jerosch-Herold, M.; Masri, A. Mavacamten Favorably Impacts Cardiac Structure in Obstructive Hypertrophic Cardiomyopathy: EXPLORER-HCM Cardiac Magnetic Resonance Substudy Analysis. Circulation 2021, 143, 606–608. [Google Scholar] [CrossRef]
- Marian, A.J.; Braunwald, E. Hypertrophic cardiomyopathy: Genetics, pathogenesis, clinical manifestations, diagnosis, and therapy. Circ. Res. 2017, 121, 749–770. [Google Scholar] [CrossRef] [PubMed]
- Yang, H.; Yang, Y.; Xue, Y.; Luo, S. Efficacy and safety of radiofrequency ablation for hypertrophic obstructive cardiomyopathy: A systematic review and meta-analysis. Clin. Cardiol. 2020, 43, 450–458. [Google Scholar] [CrossRef] [PubMed]
| Patient Characteristics | Overall Population n = 76 | Male n = 33 (43.4) | Female n = 43 (56.6) | p Value |
|---|---|---|---|---|
| 1. Demographics | ||||
| Age, years | 60.5 [26.0] | 54.0 [22.0] | 68.0 [21.0] | <0.001 |
| BMI, kg/m2 | 28.2 ± 4.8 | 28.6 ± 4.8 | 27.9 ± 4.9 | 0.509 |
| BSA, m2 | 1.9 ± 0.3 | 2.0 ± 0.3 | 1.8 ± 0.2 | <0.001 |
| NYHA ≥ 3, n (%) | 65 (85.5) | 25 (75.8) | 40 (93.0) | 0.049 |
| Previous syncope, n (%) | 14 (18.4) | 8 (24.2) | 6 (14.0) | 0.371 |
| Family history of SCD, n (%) | 11 (14.5) | 6 (18.2) | 5 (11.6) | 0.517 |
| Previous cardiac arrest or sustained VT, n (%) | 3 (3.9) | 2 (6.1) | 1 (2.3) | 0.576 |
| ICD, n (%) | 13 (17.1) | 8 (24.2) | 5 (11.6) | 0.219 |
| Pacemaker, n (%) | 2 (2.6) | 1 (3.0) | 1 (2.3) | 1.000 |
| CRT, n (%) | 1 (1.3) | 0 (0.0) | 1 (2.3) | 1.000 |
| 2. Comorbidities | ||||
| HTN, n (%) | 65 (85.5) | 28 (84.8) | 37 (86.0) | 1.000 |
| Diabetes mellitus, n (%) | 13 (17.1) | 5 (15.2) | 8 (18.6) | 0.766 |
| Atrial fibrillation, n (%) | 13 (17.1) | 6 (18.2) | 7 (16.3) | 1.000 |
| CAD, n (%) | 22 (28.9) | 7 (21.2) | 15 (34.9) | 0.214 |
| COPD, n (%) | 6 (7.9) | 3 (9.1) | 3 (7.0) | 1.000 |
| AV block, n (%) | 5 (6.7) | 1 (3.0) | 4 (9.3) | 0.381 |
| LAFB, n (%) | 5 (6.6) | 3 (9.1) | 2 (4.7) | 0.647 |
| LBBB, n (%) | 6 (7.9) | 2 (6.1) | 4 (9.3) | 0.692 |
| RBBB, n (%) | 6 (7.9) | 5 (15.2) | 1 (2.3) | 0.080 |
| nsVT, n (%) | 8 (10.5) | 3 (9.1) | 5 (11.6) | 1.000 |
| 3. Echocardiography | ||||
| LVEF, % | 61 [11.0] | 63 [14.0] | 60 [8.0] | 0.113 |
| LVOT gradient at rest, mmHg | 41.0 [27.0] | 40.0 [28.0] | 42.0 [32.0] | 0.560 |
| LVOT gradient (Valsalva), mmHg | 95.0 [71.0] | 95.0 [75.0] | 85.0 [60.0] | 0.208 |
| SAM, n (%) | 62 (81.6) | 29 (87.9) | 33 (76.7) | 0.248 |
| MR ≥ 2 grade, n (%) | 35 (46.1) | 16 (48.5) | 19 (44.2) | 0.817 |
| LA diameter/m2, mm | 22.0 [4.6] | 21.5 [4.7] | 23.7 [5.3] | 0.040 |
| LAVI/m2, mL | 38.9 [20.0] | 34.8 [4.7] | 40.1 [20.5] | 0.283 |
| TAPSE, mm | 19 [4.0] | 21 [5.0] | 19 [3.0] | 0.009 |
| sPAP > 35 mmHg, n (%) | 22 (28.9) | 9 (27.3) | 13 (30.2) | 0.805 |
| 4. Laboratory results | ||||
| NTproBNP, pg/mL | 388.0 [737.0] | 318.0 [562.0] | 430.7 [1142.0] | 0.099 |
| Creatinine, mg/dL | 1.1 [0.2] | 1.1 [0.3] | 1.1 [0.2] | 0.146 |
| CK, U/L | 75.0 [53.5] | 77.0 [33.0] | 69.0 [67.0] | 0.052 |
| TroponinI, ng/L | 20.0 [30.0] | 20.0 [48.5] | 20.0 [30.0] | 0.577 |
| Medical treatment | ||||
| Betablockers, n (%) | 62 (81.6) | 29 (87.9) | 33 (76.7) | 0.248 |
| Verapamil, n (%) | 16 (21.1) | 6 (18.2) | 10 (23.3) | 0.778 |
| Diltiazem, n (%) | 1 (1.3) | 1 (3.1) | 0 (0.0) | 0.427 |
| Diuretics, n (%) | 45 (59.2) | 12 (36.4) | 33 (76.7) | <0.001 |
| NOACs, n (%) | 4 (5.3) | 2 (6.1) | 2 (4.7) | 1.000 |
| Vitamin K antagonists, n (%) | 8 (10.5) | 4 (12.1) | 4 (9.3) | 0.721 |
| Antiplatelet agents, n (%) | 42 (55.3) | 17 (51.5) | 25 (58.1) | 0.644 |
| Peri- and Postprocedural Outcomes | Overall Population n = 76 | Male n = 33 | Female n = 43 | p Value |
|---|---|---|---|---|
| Volume of microspheres, mL | 2.0 [2.0] | 3.0 [3.0] | 2.0 [2.0] | 0.306 |
| ICU stay, days | 1.0 [0.0] | 1.0 [0.0] | 1.0 [1.0] | 0.133 |
| Hospitalisation, days | 12.5 [10.0] | 12.0 [8.0] | 13.0 [11.0] | 0.449 |
| CK max, U/L | 926.0 [949.0] | 1018.0 [1537.0] | 897 [947.0] | 0.234 |
| Troponin I, ng/L | 2485.0 [2874.0] | 2311.0 [2908.0] | 2659.0 [2889.0] | 0.506 |
| Complications | ||||
| AV block, n (%) | 5 (6.6) | 2 (6.1) | 3 (7.0) | 1.000 |
| New LBBB, n (<%) | 1 (1.3) | 0 (0.0) | 1 (2.3) | 1.000 |
| New RBBB, n (%) | 3 (3.9) | 1 (3.0) | 2 (4.7) | 1.000 |
| Access site complications, n (%) | 4 (5.3) | 2 (6.1) | 2 (4.7) | 1.000 |
| Postprocedural death, n (%) | 1 (1.3) | 1 (3.0) | 0 (0.0) | 0.434 |
| Characteristics | Males (n = 33) | Females (n = 43) | Males vs. Females | ||||
|---|---|---|---|---|---|---|---|
| Pre-TASH | Post-TASH | p Value | Pre-TASH | Post-TASH | p Value | p Value for Δ | |
| LVOT gradient at rest, mmHg | 40 [22.0] | 16.0 [14.0] | <0.001 | 42.0 [32.0] | 15.0 [17.0] | <0.001 | 0.147 |
| Provoked LVOT gradient, mmHg | 95.0 [75.0] | 25.0 [41.0] | <0.001 | 85.0 [60.0] | 24.0 [42.0] | <0.001 | 0.709 |
| NT-proBNP, pg/mL | 318.0 [562.0] | 189.0 [367.0] | 0.073 | 430.7 [1142.0] | 281.0 [408.0] | 0.009 | 0.338 |
| NYHA ≥ 3, n (%) | 25 (75.8) | 1 (3.0) | <0.001 | 40 (93.0) | 2 (4.7) | <0.001 | 0.636 |
| IVSd > 20 mm, n (%) | 16 (48.5) | 4 (12.1) | <0.001 | 21 (48.8) | 3 (7.0) | <0.001 | 0.583 |
| Characteristics | HR | 95% CI | p Value |
|---|---|---|---|
| Age at TASH, years | 1.035 | 1.007–1.063 | 0.015 |
| NYHA ≥ 3 | 1.256 | 0.359–4.395 | 0.722 |
| Female sex | 0.940 | 0.376–2.350 | 0.895 |
| TAPSE, mm | 1.921 | 0.802–1.057 | 0.240 |
| Diuretics | 1.703 | 0.707–4.101 | 0.235 |
| LA diameter, mm | 1.007 | 0.974–1.040 | 0.697 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alyaydin, E.; Vogel, J.K.; Luedike, P.; Rassaf, T.; Jánosi, R.A.; Papathanasiou, M. Sex-Related Differences among Adults with Hypertrophic Obstructive Cardiomyopathy Undergoing Transcoronary Ablation of Septal Hypertrophy. J. Clin. Med. 2023, 12, 3024. https://doi.org/10.3390/jcm12083024
Alyaydin E, Vogel JK, Luedike P, Rassaf T, Jánosi RA, Papathanasiou M. Sex-Related Differences among Adults with Hypertrophic Obstructive Cardiomyopathy Undergoing Transcoronary Ablation of Septal Hypertrophy. Journal of Clinical Medicine. 2023; 12(8):3024. https://doi.org/10.3390/jcm12083024
Chicago/Turabian StyleAlyaydin, Emyal, Julia Kirsten Vogel, Peter Luedike, Tienush Rassaf, Rolf Alexander Jánosi, and Maria Papathanasiou. 2023. "Sex-Related Differences among Adults with Hypertrophic Obstructive Cardiomyopathy Undergoing Transcoronary Ablation of Septal Hypertrophy" Journal of Clinical Medicine 12, no. 8: 3024. https://doi.org/10.3390/jcm12083024
APA StyleAlyaydin, E., Vogel, J. K., Luedike, P., Rassaf, T., Jánosi, R. A., & Papathanasiou, M. (2023). Sex-Related Differences among Adults with Hypertrophic Obstructive Cardiomyopathy Undergoing Transcoronary Ablation of Septal Hypertrophy. Journal of Clinical Medicine, 12(8), 3024. https://doi.org/10.3390/jcm12083024