Satisfaction with Life and Coping Strategies among Patients with Hidradenitis Suppurativa: A Cross-Sectional Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants and Study Design
2.2. Assessments
2.2.1. HS Severity
2.2.2. Satisfaction with Life
2.2.3. Coping Strategies
2.2.4. Psychopathological Symptoms
2.2.5. Quality of Life
2.3. Statistical Analysis
3. Results
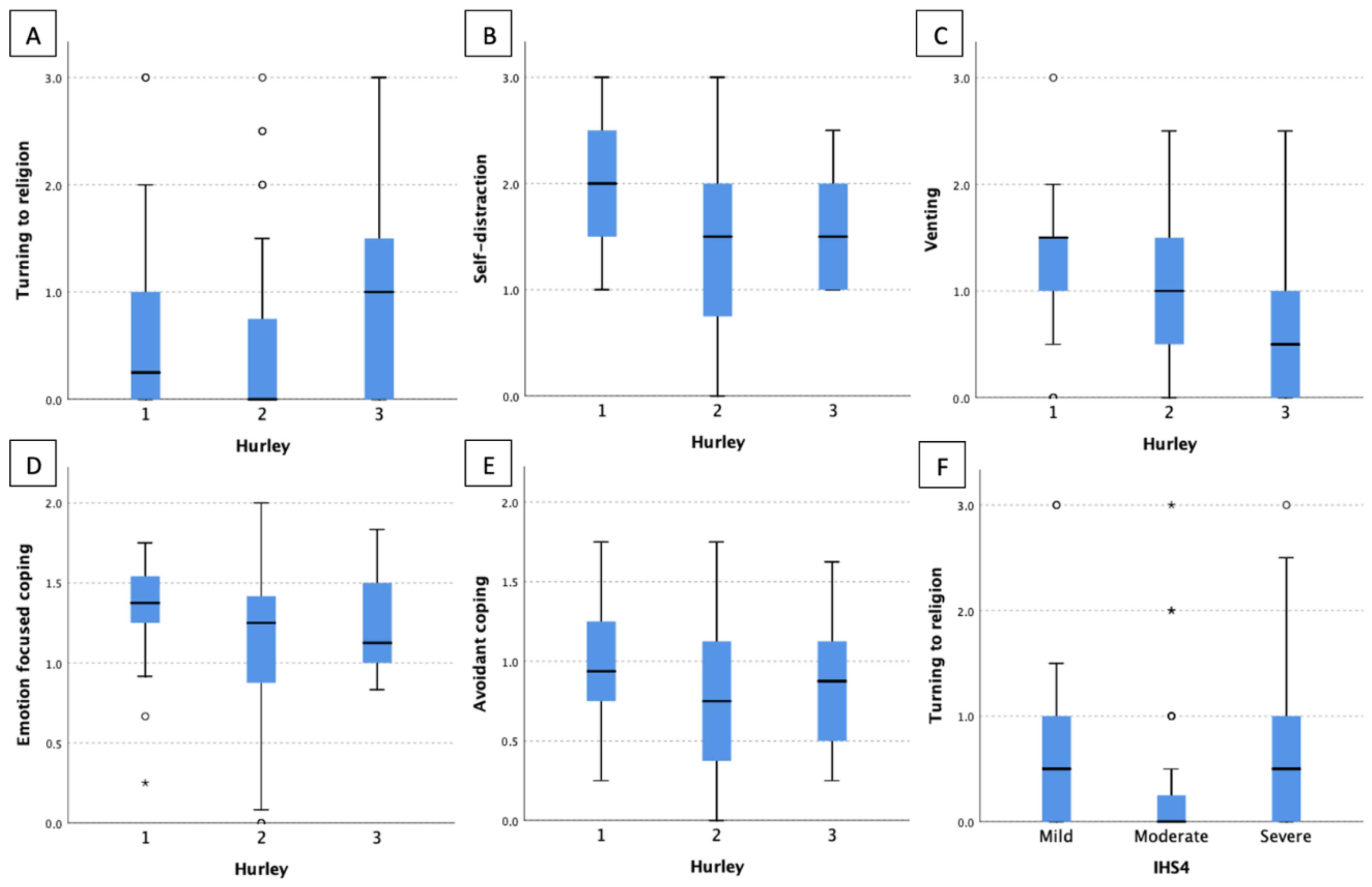
3.1. Clinical HS Severity
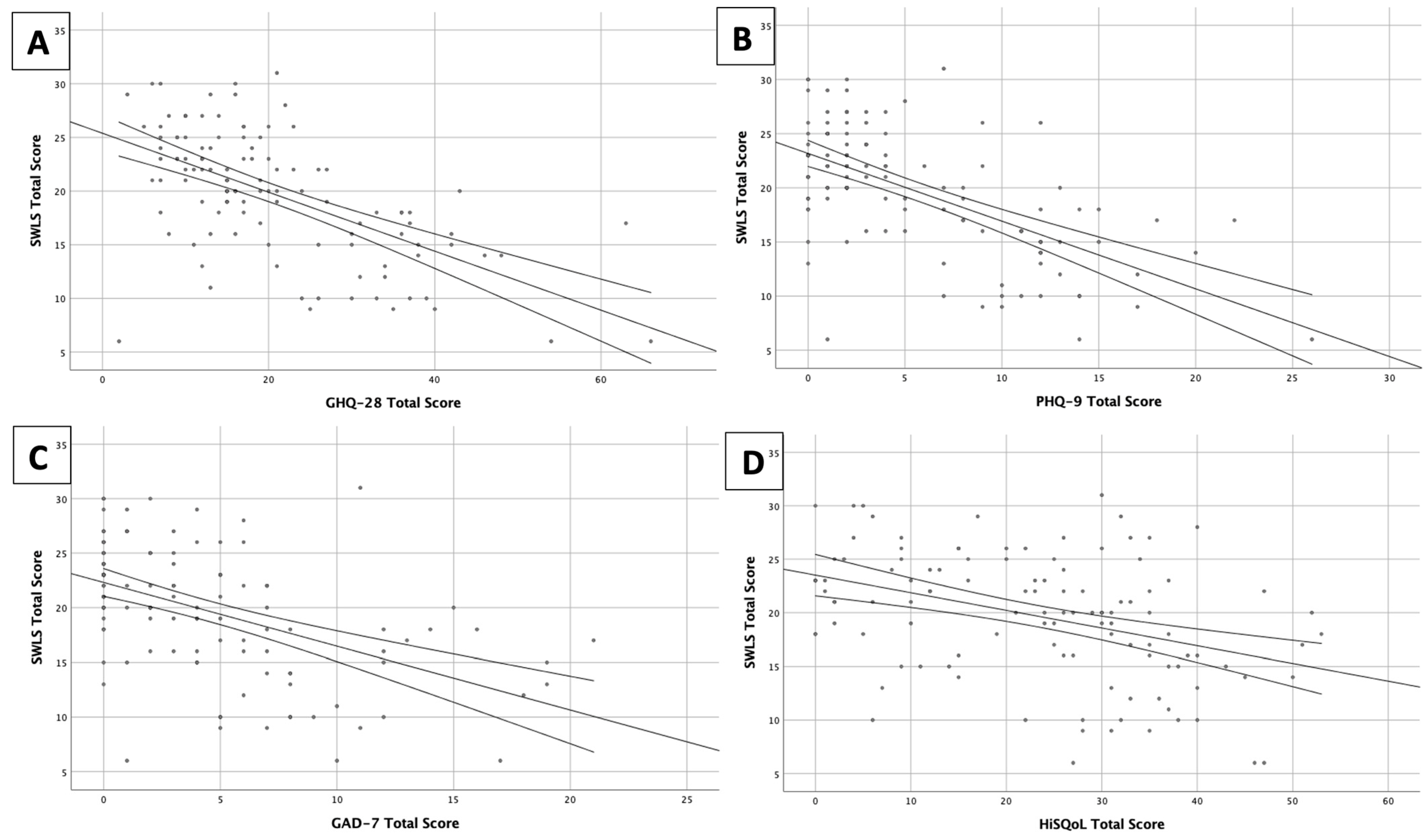
3.2. Satisfaction with Life
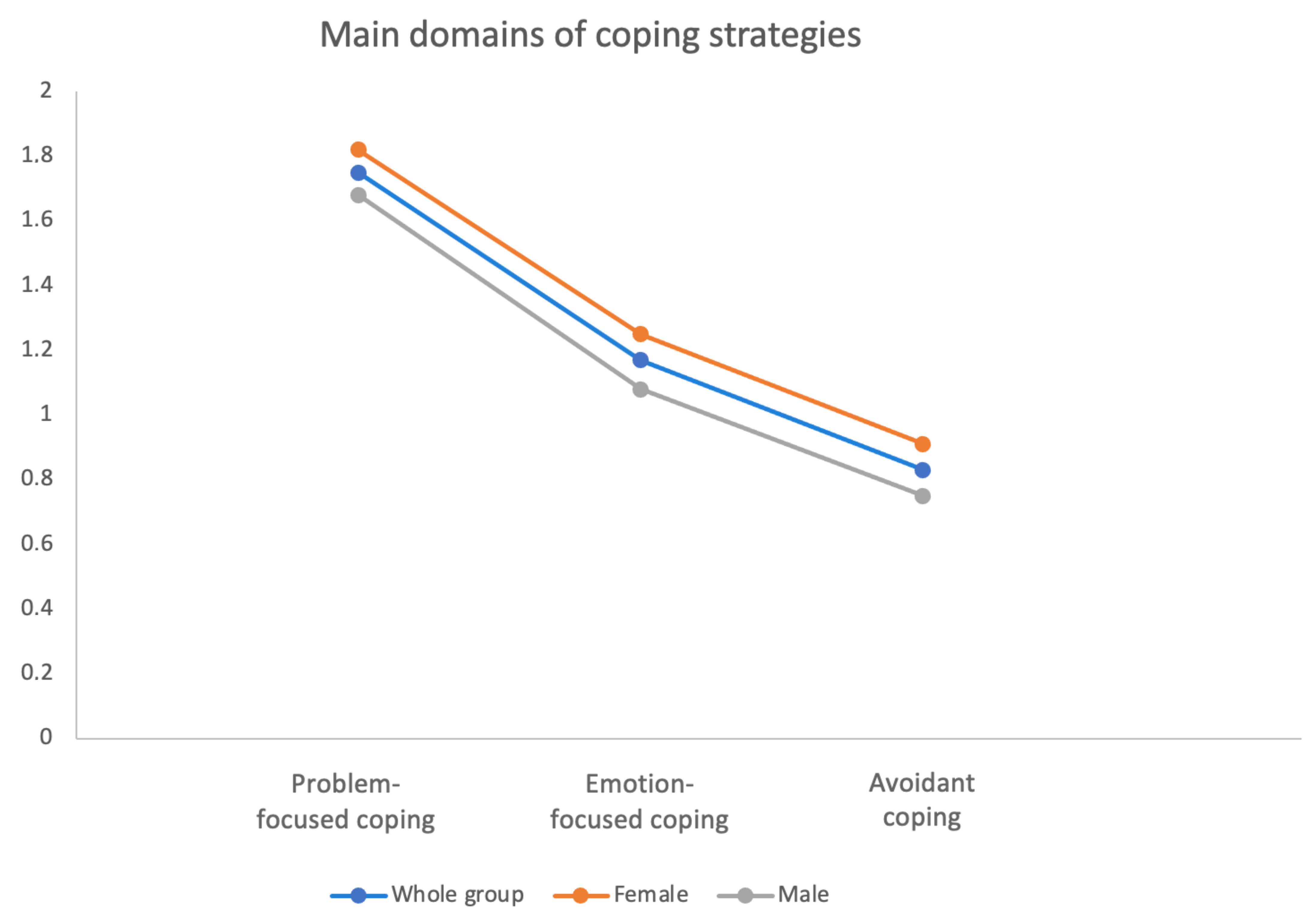
3.3. Coping Strategies
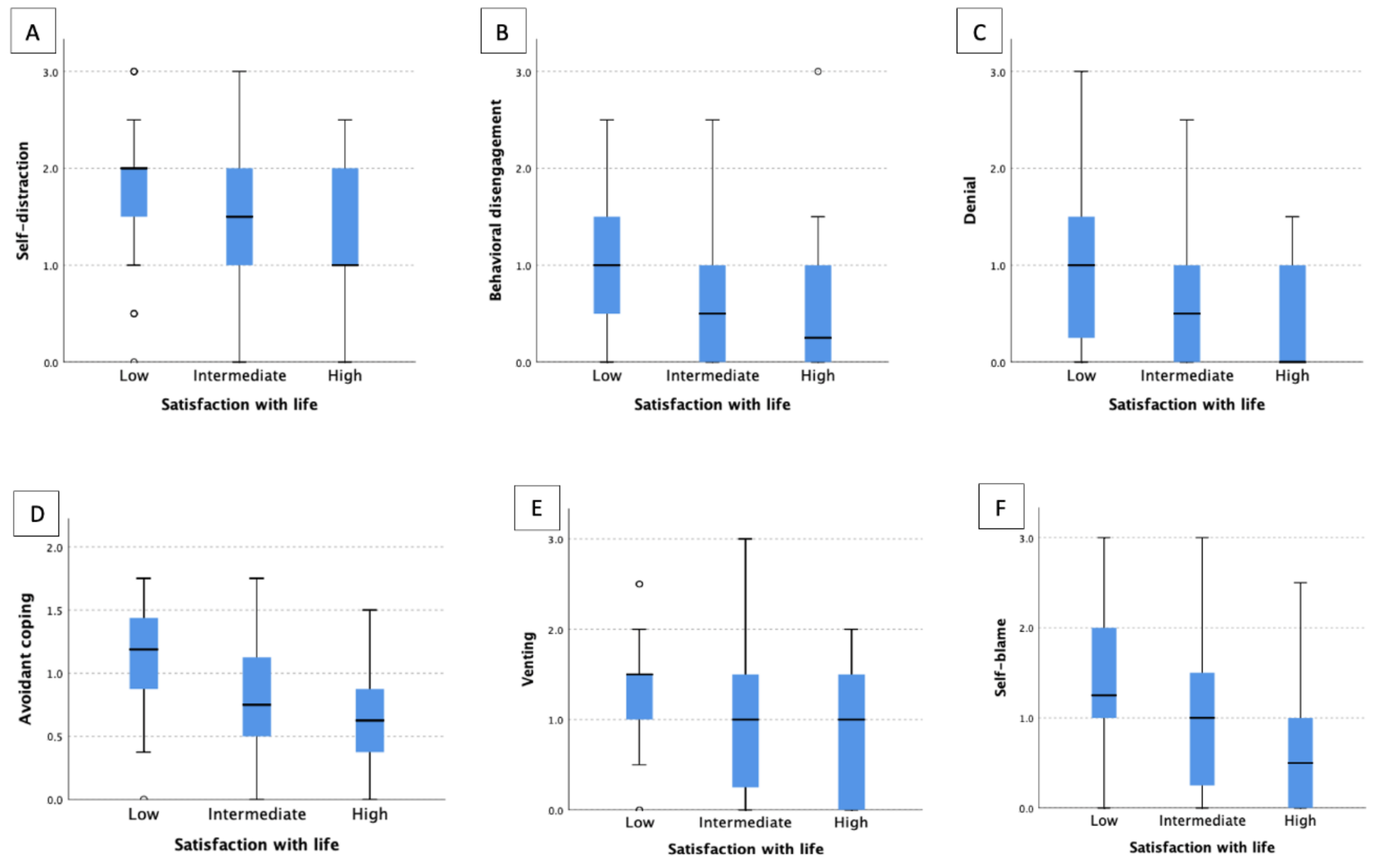
3.4. Relationship between Satisfaction with Life and Coping Strategies
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Zouboulis, C.C.; Benhadou, F.; Byrd, A.S.; Chandran, N.S.; Giamarellos-Bourboulis, E.J.; Fabbrocini, G.; Frew, J.W.; Fujita, H.; González-López, M.A.; Guillem, P.; et al. What Causes Hidradenitis Suppurativa?—15 Years after. Exp. Dermatol. 2020, 29, 1154–1170. [Google Scholar] [CrossRef] [PubMed]
- Sabat, R.; Jemec, G.B.E.; Matusiak, Ł.; Kimball, A.B.; Prens, E.; Wolk, K. Hidradenitis Suppurativa. Nat. Rev. Dis. Prim. 2020, 6, 18. [Google Scholar] [CrossRef] [PubMed]
- Kaaz, K.; Szepietowski, J.C.; Matusiak, Ł. Influence of Itch and Pain on Sleep Quality in Patients with Hidradenitis Suppurativa. Acta Derm.-Venereol. 2018, 98, 757–761. [Google Scholar] [CrossRef] [PubMed]
- Matusiak, Ł.; Szczęch, J.; Kaaz, K.; Lelonek, E.; Szepietowski, J.C. Clinical Characteristics of Pruritus and Pain in Patients with Hidradenitis Suppurativa. Acta Derm.-Venereol. 2018, 98, 191–194. [Google Scholar] [CrossRef]
- Krajewski, P.K.; Matusiak, Ł.; Von Stebut, E.; Schultheis, M.; Kirschner, U.; Nikolakis, G.; Szepietowski, J.C. Pain in Hidradenitis Suppurativa: A Cross-Sectional Study of 1795 Patients. Acta Derm.-Venereol. 2021, 101, 1–4. [Google Scholar] [CrossRef]
- Zouboulis, C.; Desai, N.; Emtestam, L.; Hunger, R.; Ioannides, D.; Juhász, I.; Lapins, J.; Matusiak, L.; Prens, E.; Revuz, J.; et al. European S1 Guideline for the Treatment of Hidradenitis Suppurativa/Acne Inversa. J. Eur. Acad. Dermatol. Venereol. 2015, 29, 619–644. [Google Scholar] [CrossRef]
- Moltrasio, C.; Tricarico, P.M.; Romagnuolo, M.; Marzano, A.V.; Crovella, S. Hidradenitis Suppurativa: A Perspective on Genetic Factors Involved in the Disease. Biomedicines 2022, 10, 2039. [Google Scholar] [CrossRef]
- Abu Rached, N.; Gambichler, T.; Dietrich, J.W.; Ocker, L.; Seifert, C.; Stockfleth, E.; Bechara, F.G. The Role of Hormones in Hidradenitis Suppurativa: A Systematic Review. Int. J. Mol. Sci. 2022, 23, 15250. [Google Scholar] [CrossRef]
- Krajewski, P.K.; Matusiak, L.S.J. Adipokines as an Important Link between Hidradenitis Suppurativa and Obesity: A Narrative Review. Br. J. Dermatol. 2022, 18, 320–327. [Google Scholar] [CrossRef]
- Ponikowska, M.; Matusiak, L.; Kasztura, M.; Jankowska, E.A.; Szepietowski, J.C. Deranged Iron Status Evidenced by Iron Deficiency Characterizes Patients with Hidradenitis Suppurativa. Dermatology 2020, 236, 52–58. [Google Scholar] [CrossRef]
- Matusiak, Ł.; Bieniek, A.; Szepietowski, J.C. Hidradenitis Suppurativa Markedly Decreases Quality of Life and Professional Activity. J. Am. Acad. Dermatol. 2010, 62, 706–709. [Google Scholar] [CrossRef] [PubMed]
- Głowaczewska, A.; Reszke, R.; Szepietowski, J.C.; Matusiak, Ł. Indirect Self-Destructiveness in Hidradenitis Suppurativa Patients. J. Clin. Med. 2021, 10, 4194. [Google Scholar] [CrossRef] [PubMed]
- Głowaczewska, A.; Szepietowski, J.C.; Matusiak, Ł. Prevalence and Associated Factors of Alexithymia in Patients with Hidradenitis Suppurativa: A Cross-Sectional Study. Acta Derm.-Venereol. 2021, 101, 1–2. [Google Scholar] [CrossRef]
- Cuenca-barrales, C.; Montero-vilchez, T.; Krajewski, P.K.; Szepietowski, J.C.; Matusiak, L.; Arias-santiago, S.; Molina-leyva, A. Sexual Dysfunction and Quality of Life in Patients with Hidradenitis Suppurativa and Their Partners. Int. J. Environ. Res. Public Health 2023, 26, 389. [Google Scholar] [CrossRef] [PubMed]
- Matusiak, Ł.; Bieniek, A.; Szepietowski, J.C. Psychophysical Aspects of Hidradenitis Suppurativa. Acta Derm.-Venereol. 2010, 90, 264–268. [Google Scholar] [CrossRef]
- Rymaszewska, J.; Krajewski, P.K.; Szczęch, J.; Szepietowski, J. Depression and Anxiety in Hidradenitis Suppurativa Patients: A Cross-Sectional Study among Polish Patients. Adv. Dermatol. Allergol. 2022, XL, 35–39. [Google Scholar] [CrossRef]
- Kirby, J.S.; Sisic, M.; Tan, J. Exploring Coping Strategies for Patients with Hidradenitis Suppurativa. JAMA Dermatol. 2016, 152, 1166–1167. [Google Scholar] [CrossRef]
- Ovadja, Z.N.; Schuit, M.M.; van der Horst, C.M.A.M.; Lapid, O. Inter- and Intrarater Reliability of Hurley Staging for Hidradenitis Suppurativa. Br. J. Dermatol. 2019, 181, 344–349. [Google Scholar] [CrossRef]
- Zouboulis, C.C.; Tzellos, T.; Kyrgidis, A.; Jemec, G.B.E.; Bechara, F.G.; Giamarellos-Bourboulis, E.J.; Ingram, J.R.; Kanni, T.; Karagiannidis, I.; Martorell, A.; et al. Development and Validation of IHS4, a Novel Dynamic Scoring System to Assess Hidradenitis Suppurativa/Acne Inversa Severity. Br. J. Derm. 2017, 177, 140. [Google Scholar] [CrossRef]
- Juczyński, Z. Polish Adaptation of the Satisfaction with Life Scale SWLS; Diener, E., Emmons, R.A., Larson, R.J., Griffin, S., Eds.; Laboratory of Tests of the Polish Psychological Association: Warsaw, Poland, 2012; pp. 162–166. [Google Scholar]
- Charles, S. Carver You Want to Measure Coping but Your Protocol’s Too Long: Consider the Brief COPE. Int. J. Behav. Med. 1997, 4, 92–100. [Google Scholar]
- Finzi, A.; Colombo, D.; Caputo, A.; Andreassi, L.; Chimenti, S.; Vena, G.; Simoni, L.; Sgarbi, S.; Giannetti, A. Psychological Distress and Coping Strategies in Patients with Psoriasis: The PSYCHAE Study. J. Eur. Acad. Dermatol. Venereol. JEADV 2007, 21, 1161–1169. [Google Scholar] [CrossRef] [PubMed]
- Sterling, M. General Health Questionnaire-28 (GHQ-28). J. Physiother. 2011, 57, 259. [Google Scholar] [CrossRef] [PubMed]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B.W. The PHQ-9: Validity of a Brief Depression Severity Measure. J. Gen. Intern. Med. 2001, 16, 606–613. [Google Scholar] [CrossRef] [PubMed]
- Spitzer, R.L.; Kroenke, K.; Williams, J.W.; Löwe, B. A Brief Measure for Assessing Generalized Anxiety Disorder: The GAD-7. Arch. Intern. Med. 2006, 166, 1092–1097. [Google Scholar] [CrossRef]
- Thorlacius, L.; Esmann, S.; Miller, I.; Vinding, G.; Jemec, G.B.E. Development of HiSQOL: A Hidradenitis Suppurativa-Specific Quality of Life Instrument. Ski. Appendage Disord. 2019, 5, 221–229. [Google Scholar] [CrossRef] [PubMed]
- Krajewski, P.K.; Matusiak, Ł.; Szepietowska, M.; Rymaszewska, J.E.; Jemec, G.B.E.; Kirby, J.S.; Szepietowski, J.C. Hidradenitis Suppurativa Quality of Life (HiSQOL): Creation and Validation of the Polish Language Version. Postep. Dermatol. Alergol. 2021, 38, 967–972. [Google Scholar] [CrossRef]
- Díaz, D.; Rivera, A.; Otero, V.; Rueda, L. Epidemiology of Hidradenitis Suppurativa: Current Status. Curr. Dermatol. Rep. 2022, 11, 336–340. [Google Scholar] [CrossRef]
- Bettoli, V.; Cazzaniga, S.; Scuderi, V.; Zedde, P.; Di Landro, A.; Naldi, L.; Cannavò, S.; Fabbrocini, G.; Marzano, A.V.; Mazzanti, C.; et al. Hidradenitis Suppurativa Epidemiology: From the First Italian Registry in 2009 to the Most Recent Epidemiology Updates—Italian Registry Hidradenitis Suppurativa Project 2. J. Eur. Acad. Dermatol. Venereol. 2019, 33, 4–6. [Google Scholar] [CrossRef]
- Wierenga, K.L.; Lehto, R.H.; Given, B. Emotion Regulation in Chronic Disease Populations: An Integrative Review. Res. Theory Nurs. Pract. 2016, 31, 247–271. [Google Scholar] [CrossRef]
- Machado, M.O.; Stergiopoulos, V.; Maes, M.; Kurdyak, P.A.; Lin, P.Y.; Wang, L.J.; Shyu, Y.C.; Firth, J.; Koyanagi, A.; Solmi, M.; et al. Depression and Anxiety in Adults with Hidradenitis Suppurativa: A Systematic Review and Meta-Analysis. JAMA Dermatol. 2019, 155, 939–945. [Google Scholar] [CrossRef]
- Soliman, M.M. Feeling of Stigmatization and Satisfaction with Life among Arabic Psoriatic Patients. Saudi Pharm. J. 2020, 28, 1868–1873. [Google Scholar] [CrossRef] [PubMed]
- Kowalewska, B.; Jankowiak, B.; Niedżwiecka, B.; Krajewska-Kułak, E.; Niczyporuk, W.; Khvorik, D.F. Relationships between the Acceptance of Illness, Quality of Life and Satisfaction with Life in Psoriasis. Postep. Dermatol. Alergol. 2021, 37, 948–955. [Google Scholar] [CrossRef] [PubMed]
- Kulczycka, L.; Sysa-Jędrzejowska, A.; Robak, E. Quality of Life and Satisfaction with Life in SLE Patients-the Importance of Clinical Manifestations. Clin. Rheumatol. 2010, 29, 991–997. [Google Scholar] [CrossRef]
- Nielsen, M.B.; Knardahl, S. Coping Strategies: A Prospective Study of Patterns, Stability, and Relationships with Psychological Distress. Scand. J. Psychol. 2014, 55, 142–150. [Google Scholar] [CrossRef]
- Richards, H.L.; Ling, T.C.; Evangelou, G.; Brooke, R.C.C.; Fortune, D.G.; Rhodes, L.E. Evidence of High Levels of Anxiety and Depression in Polymorphic Light Eruption and Their Association with Clinical and Demographic Variables. Br. J. Dermatol. 2008, 159, 439–444. [Google Scholar] [CrossRef]
- Iglesias-Rey, M.; Barreiro-de Acosta, M.; Caamaño-Isorna, F.; Rodríguez, I.V.; González, A.L.; Lindkvist, B.; Domínguez-Muñoz, E. How Do Psychological Variables Influence Coping Strategies in Inflammatory Bowel Disease? J. Crohn’s Colitis 2013, 7, e219–e226. [Google Scholar] [CrossRef]
- Schoenmakers, E.C.; van Tilburg, T.G.; Fokkema, T. Problem-Focused and Emotion-Focused Coping Options and Loneliness: How Are They Related? Eur. J. Ageing 2015, 12, 153–161. [Google Scholar] [CrossRef] [PubMed]
- Ziarko, M.; Mojs, E.; Sikorska, D.; Samborski, W. Coping and Life Satisfaction: Mediating Role of Ego-Resiliency in Patients with Rheumatoid Arthritis. Med. Princ. Pract. 2020, 29, 160–165. [Google Scholar] [CrossRef]
- Pokryszko-Dragan, A.; Chojdak-Łukasiewicz, J.; Gruszka, E.; Pawłowski, M.; Pawłowski, T.; Rudkowska-Mytych, A.; Rymaszewska, J.; Budrewicz, S. Burden of COVID-19 Pandemic Perceived by Polish Patients with Multiple Sclerosis. J. Clin. Med. 2021, 10, 4215. [Google Scholar] [CrossRef]
- Blaževi, S.; Rubeša, G.; Brajac, I.; Vu, M.; Pavlovi, E. Satisfaction with Life and Coping Skills in the Acute and Chronic Urticaria. Psychiatr. Danub. 2016, 28, 34–38. [Google Scholar]
- Lazarus, R.S. From Psychological Stress to the Emotions: A History of Changing Outlooks. Annu. Rev. Psychol. 1993, 44, 1–21. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | Whole Group (n = 114) | Females (n = 61) | Males (n = 53) | p |
|---|---|---|---|---|
| Sex, number of participants (%) | NA | NA | NA | |
| Males | 53 (46.5) | |||
| Females | 61 (53.5) | |||
| Age Mean ± SD (years) | 36.56 ± 13.10 | 37.47 ± 13.63 | 39.92 ± 12.5 | NS |
| Duration of the disease Mean ± SD (years) | 9.76 ± 8.20 | 10.9 ± 7.99 | 8.57 ± 8.38 | 0.028 |
| Number of hospitalizations, Mean ± SD (years) | 1.7 ± 2.63 | 1.86 ± 3.23 | 1.51 ± 1.66 | NS |
| Hurley stages, n (%) | ||||
| I | 28 (24.6) | 17 (27.9) | 11 (20.8) | NS |
| II | 76 (66.7) | 41 (67.2) | 35 (66.0) | NS |
| III | 10 (8.8) | 3 (4.9) | 7 (13.2) | NS |
| IHS4 severity stage, n (%) | ||||
| Mild | 26 (22.8) | 15 (24.6) | 11 (20.8) | NS |
| Moderate | 40 (35.1) | 21 (34.4) | 19 (35.8) | NS |
| Severe | 48 (42.1) | 25 (41.0) | 23 (43.4) | NS |
| SWLS | Whole Group (n = 114) | Females (n = 61) | Males (n = 53) | p |
|---|---|---|---|---|
| Total score, mean ± SD | 19.8 ± 5.7 | 19.53 ± 5.94 | 19.7 ± 5.7 | NS |
| SWL, n (%) | ||||
| 36 (31.6) 48 (42.1) 30 (26.3) | 21 (34.4) 24 (39.4) 16 (26.2) | 15 (28.3) 24 (45.3) 14 (26.4) | NS |
| SWLS Total Score | GHQ-28 | PHQ-9 | GAD-7 | HiSQoL Total Score | HiSQoL Activities–Adaptations | HiSQoL Symptoms | HiSQoL Psychosocial |
|---|---|---|---|---|---|---|---|
| Whole group (n = 114) | r = −0.579 p < 0.001 | r = −0.603 p < 0.001 | r = −0.579 p < 0.001 | r = −0.449 p < 0.001 | r = −0.366 p < 0.001 | r = −0.331 p = 0.011 | r = −0.478 p < 0.001 |
| Females (n = 61) | r = −0.533 p < 0.001 | r = −0.699 p < 0.001 | r = −0.624 p < 0.001 | r = −0.455 p < 0.001 | r = −0.364 p = 0.005 | r = −0.455 p < 0.001 | r = −0.458 p < 0.001 |
| Males (n = 53) | r = −0.636 p < 0.001 | r = −0.507 p < 0.001 | r = −0.549 p < 0.001 | r = −0.483 p < 0.001 | r = −0.406 p = 0.003 | r = −0.305 p = 0.026 | r = −0.497 p < 0.001 |
| Coping Strategies Mean ± SD | Whole Group (n = 114) | Females (n = 61) | Males (n = 53) | p |
|---|---|---|---|---|
Problem-focused coping
| 1.75 ± 0.65 1.96 ± 0.85 1.93 ± 0.88 1.52 ± 0.76 1.61 ± 0.84 | 1.82 ± 0.63 1.98 ± 0.85 1.95 ± 0.87 1.58 ± 0.74 1.76 ± 0.83 | 1.68 ± 0.68 1.92 ± 0.87 1.92 ± 0.9 1.44 ± 0.79 1.6 ± 0.87 | NS NS NS NS 0.039 |
Emotion-focused coping
| 1.17 ± 0.65 1.84 ± 0.8 0.89 ± 0.63 0.54 ± 0.79 1.76 ± 0.8 1.01 ± 0.75 0.98 ± 0.82 | 1.25 ± 0.38 1.97 ± 0.73 0.87 ± 0.64 0.59 ± 0.85 1.89 ± 0.72 1.12 ± 0.71 1.07 ± 0.92 | 1.08 ± 0.47 1.7 ± 0.86 0.91 ± 0.62 0.47 ± 0.7 1.61 ± 0.87 0.88 ± 0.77 0.89 ± 0.68 | NS NS NS NS NS NS NS |
Avoidant coping
| 0.83 ± 0.46 1.53 ± 0.85 0.66 ± 0.7 0.46 ± 0.74 0.68 ± 0.7 | 0.91 ± 0.45 1.71 ± 0.8 0.68 ± 0.8 0.52 ± 0.83 0.73 ± 0.71 | 0.75 ± 0.47 1.33 ± 0.88 0.64 ± 0.57 0.39 ± 0.63 0.63 ± 0.7 | NS 0.028 NS NS NS |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rymaszewska, J.E.; Krajewski, P.K.; Matusiak, Ł.; Maj, J.; Szepietowski, J.C. Satisfaction with Life and Coping Strategies among Patients with Hidradenitis Suppurativa: A Cross-Sectional Study. J. Clin. Med. 2023, 12, 2755. https://doi.org/10.3390/jcm12082755
Rymaszewska JE, Krajewski PK, Matusiak Ł, Maj J, Szepietowski JC. Satisfaction with Life and Coping Strategies among Patients with Hidradenitis Suppurativa: A Cross-Sectional Study. Journal of Clinical Medicine. 2023; 12(8):2755. https://doi.org/10.3390/jcm12082755
Chicago/Turabian StyleRymaszewska, Julia E., Piotr K. Krajewski, Łukasz Matusiak, Joanna Maj, and Jacek C. Szepietowski. 2023. "Satisfaction with Life and Coping Strategies among Patients with Hidradenitis Suppurativa: A Cross-Sectional Study" Journal of Clinical Medicine 12, no. 8: 2755. https://doi.org/10.3390/jcm12082755
APA StyleRymaszewska, J. E., Krajewski, P. K., Matusiak, Ł., Maj, J., & Szepietowski, J. C. (2023). Satisfaction with Life and Coping Strategies among Patients with Hidradenitis Suppurativa: A Cross-Sectional Study. Journal of Clinical Medicine, 12(8), 2755. https://doi.org/10.3390/jcm12082755






