Non-Surgical Management of Upper Cervical Instability via Improved Cervical Lordosis: A Case Series of Adult Patients
Abstract
1. Introduction
2. Materials and Methods
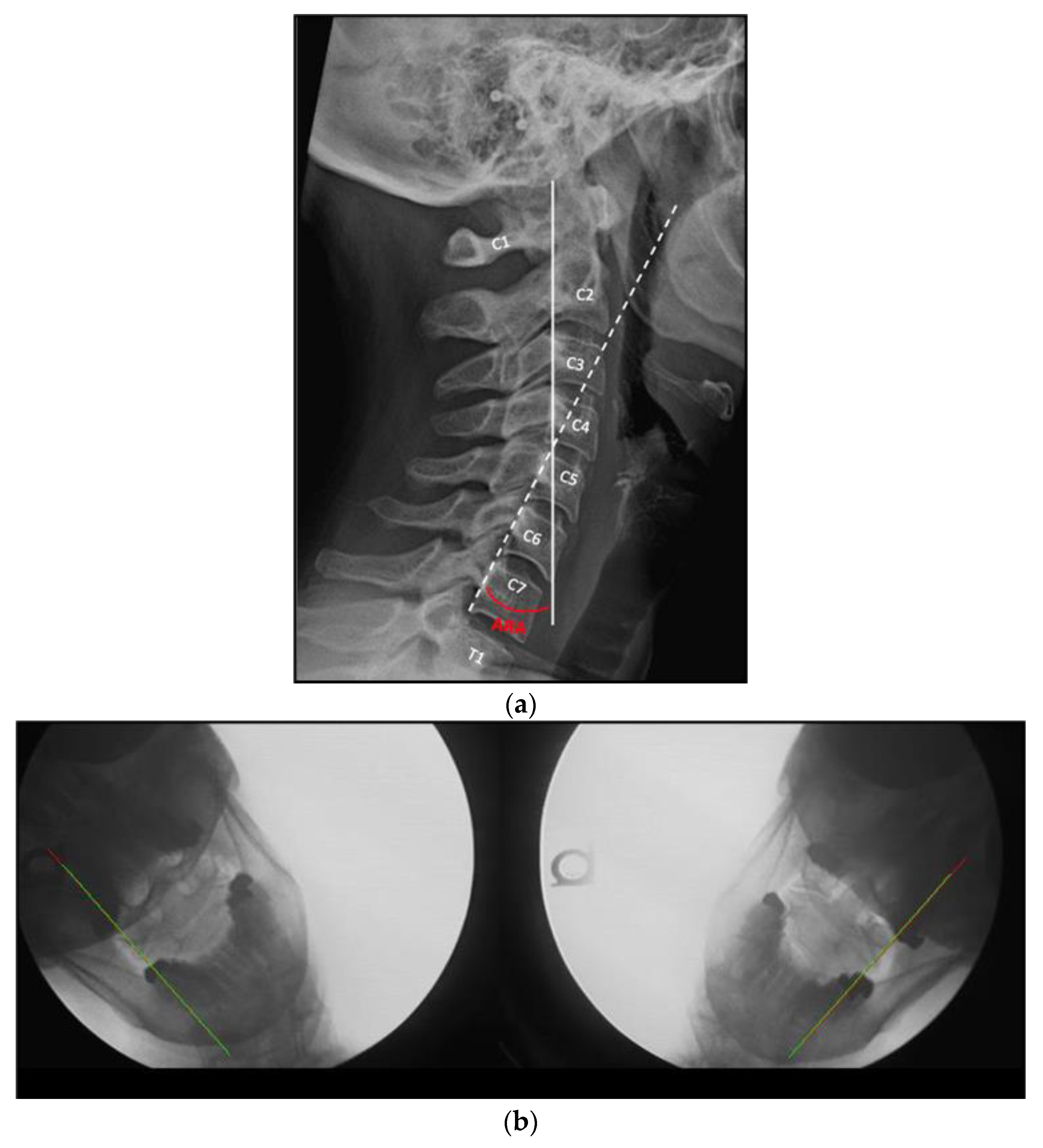
2.1. Radiographic Analysis
2.2. Intervention
- (1)
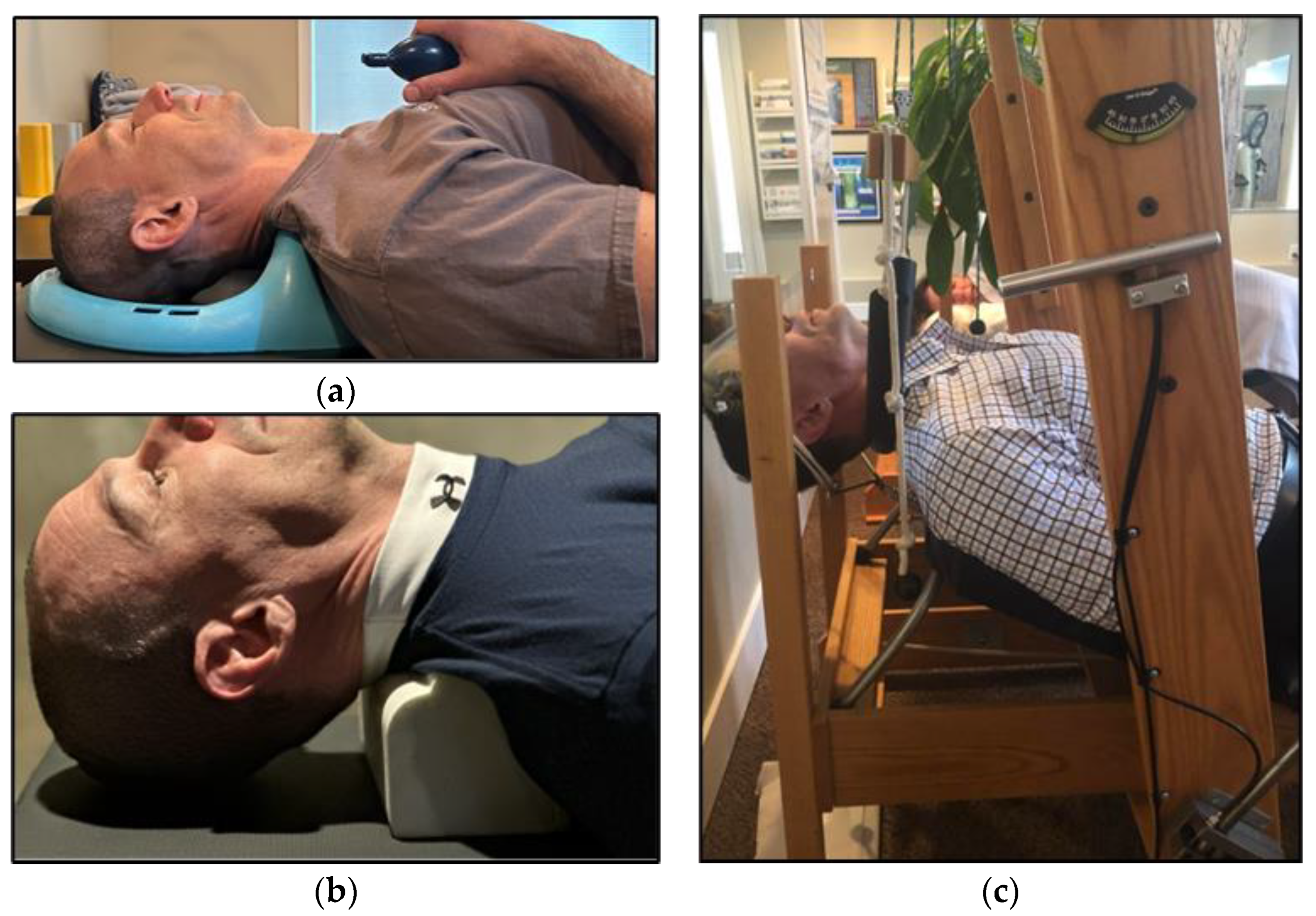
- Use of a Cervical posture pump® (Posture Pro, Inc., Huntington Beach, CA, USA), a self-controlled device with an inflatable airbladder that is applied to the supine mid-cervical spine. See Figure 2a.
- (2)
- Home use of a cervical Denneroll™ (Denneroll Industries International Pty Ltd., Sydney, Australia), used like a pillow while the patient is supine, and positioned at the mid to lower cervical spine. See Figure 2b.
- (3)
- Once tolerance to the previous two devices was established, the patient was progressed into a form of 2-way extension traction performed in office [33]. This therapy is applied while the patient lies supine on a specially designed chair, that employs a forehead harness to fix the head in a slightly extended position. A second strap is used to apply anterior tension to the mid to lower cervical spine, along the plane of the mid cervical spinal disks. See Figure 2c.
2.3. Statistical Analysis
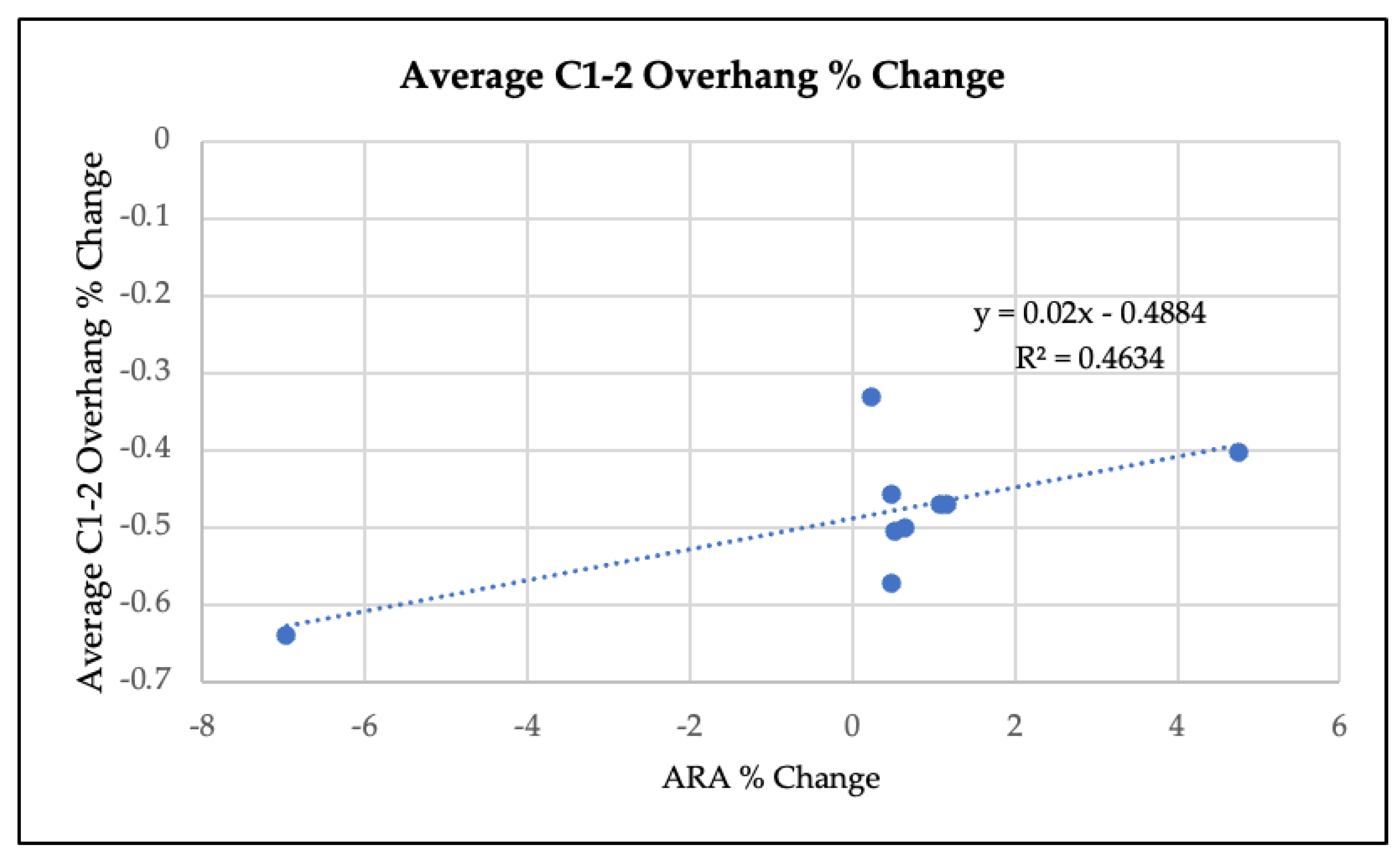
3. Results
4. Discussion
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Yadla, S.; Ratliff, J.K.; Harrop, J.S. Whiplash: Diagnosis, Treatment, and Associated Injuries. Curr. Rev. Musculoskelet. Med. 2008, 1, 65–68. [Google Scholar] [CrossRef] [PubMed]
- Freeman, M.D.; Croft, A.C.; Rossignol, A.M.; Weaver, D.S.; Reiser, M. A Review and Methodologic Critique of the Literature Refuting Whiplash Syndrome. Spine 1999, 24, 86–96. [Google Scholar] [CrossRef] [PubMed]
- Pastakia, K.; Kumar, S. Acute Whiplash Associated Disorders (WAD). Open Access Emerg. Med. 2011, 3, 29–32. [Google Scholar] [CrossRef] [PubMed]
- Berglund, A.; Alfredsson, L.; Cassidy, J.D.; Jensen, I.; Nygren, A. The Association between Exposure to a Rear-End Collision and Future Neck or Shoulder Pain: A Cohort Study. J. Clin. Epidemiol. 2000, 53, 1089–1094. [Google Scholar] [CrossRef] [PubMed]
- Freeman, M.D.; Centeno, C.J.; Katz, E. Magnetic Resonance Imaging of Whiplash Injury in the Upper Cervical Spine: Controversy or Confounding? Spine J. 2009, 9, 789–790. [Google Scholar] [CrossRef]
- Derrick, L.J.; Chesworth, B.M. Post-Motor Vehicle Accident Alar Ligament Laxity. J. Orthop. Sports Phys. Ther. 1992, 16, 6–11. [Google Scholar] [CrossRef]
- Grauer, J.N.; Panjabi, M.M.; Cholewicki, J.; Nibu, K.; Dvorak, J. Whiplash Produces an S-Shaped Curvature of the Neck with Hyperextension at Lower Levels. Spine 1997, 22, 2489–2494. [Google Scholar] [CrossRef]
- Yang, S.Y.; Boniello, A.J.; Poorman, C.E.; Chang, A.L.; Wang, S.; Passias, P.G. A Review of the Diagnosis and Treatment of Atlantoaxial Dislocations. Glob. Spine J. 2014, 4, 197–210. [Google Scholar] [CrossRef]
- Freeman, M.D.; Katz, E.A.; Rosa, S.L.; Gatterman, B.G.; Strömmer, E.M.F.; Leith, W.M. Diagnostic Accuracy of Videofluoroscopy for Symptomatic Cervical Spine Injury Following Whiplash Trauma. Int. J. Environ. Res. Public Health 2020, 17, 1693. [Google Scholar] [CrossRef]
- Evaniew, N.; Yarascavitch, B.; Madden, K.; Ghert, M.; Drew, B.; Bhandari, M.; Kwok, D. Atlantoaxial Instability in Acute Odontoid Fractures Is Associated with Nonunion and Mortality. Spine J. 2015, 15, 910–917. [Google Scholar] [CrossRef]
- Maiman, D.J.; Yoganandan, N.; Pintar, F.A. Preinjury Cervical Alignment Affecting Spinal Trauma. J. Neurosurg. 2002, 97, 57–62. [Google Scholar] [CrossRef] [PubMed]
- Cook, C.; Brismée, J.-M.; Fleming, R.; Sizer, P.S.J. Identifiers Suggestive of Clinical Cervical Spine Instability: A Delphi Study of Physical Therapists. Phys. Ther. 2005, 85, 895–906. [Google Scholar] [CrossRef] [PubMed]
- Olson, K.A.; Joder, D. Diagnosis and Treatment of Cervical Spine Clinical Instability. J. Orthop. Sports Phys. Ther. 2001, 31, 194–206. [Google Scholar] [CrossRef] [PubMed]
- Jacobson, M.E.; Khan, S.N.; An, H.S. C1-C2 Posterior Fixation: Indications, Technique, and Results. Orthop. Clin. N. Am. 2012, 43, 11–18, vii. [Google Scholar] [CrossRef]
- Smith, M.D.; Phillips, W.A.; Hensinger, R.N. Complications of Fusion to the Upper Cervical Spine. Spine 1991, 16, 702–705. [Google Scholar] [CrossRef]
- Griffiths, H.J.; Olson, P.N.; Everson, L.I.; Winemiller, M. Hyperextension Strain or “Whiplash” Injuries to the Cervical Spine. Skeletal. Radiol. 1995, 24, 263–266. [Google Scholar] [CrossRef]
- Marshall, D.L.; Tuchin, P.J. Correlation of Cervical Lordosis Measurement with Incidence of Motor Vehicle Accidents. Australas. Chiropr. Osteopat. 1996, 5, 79–85. [Google Scholar]
- Lippa, L.; Lippa, L.; Cacciola, F. Loss of Cervical Lordosis: What Is the Prognosis? J. Craniovertebral Junction Spine 2017, 8, 9–14. [Google Scholar] [CrossRef]
- Kristjansson, E.; Jónsson, H.J. Is the Sagittal Configuration of the Cervical Spine Changed in Women with Chronic Whiplash Syndrome? A Comparative Computer-Assisted Radiographic Assessment. J. Manip. Physiol. Ther. 2002, 25, 550–555. [Google Scholar] [CrossRef]
- Matsumoto, M.; Fujimura, Y.; Suzuki, N.; Toyama, Y.; Shiga, H. Cervical Curvature in Acute Whiplash Injuries: Prospective Comparative Study with Asymptomatic Subjects. Injury 1998, 29, 775–778. [Google Scholar] [CrossRef]
- Scheer, J.K.; Tang, J.A.; Smith, J.S.; Acosta, F.L.J.; Protopsaltis, T.S.; Blondel, B.; Bess, S.; Shaffrey, C.I.; Deviren, V.; Lafage, V.; et al. Cervical Spine Alignment, Sagittal Deformity, and Clinical Implications: A Review. J. Neurosurg. Spine 2013, 19, 141–159. [Google Scholar] [CrossRef] [PubMed]
- Gao, K.; Zhang, J.; Lai, J.; Liu, W.; Lyu, H.; Wu, Y.; Lin, Z.; Cao, Y. Correlation between Cervical Lordosis and Cervical Disc Herniation in Young Patients with Neck Pain. Medicine 2019, 98, e16545. [Google Scholar] [CrossRef] [PubMed]
- Oakley, P.A.; Ehsani, N.N.; Moustafa, I.M.; Harrison, D.E. Restoring Cervical Lordosis by Cervical Extension Traction Methods in the Treatment of Cervical Spine Disorders: A Systematic Review of Controlled Trials. J. Phys. Ther. Sci. 2021, 33, 784–794. [Google Scholar] [CrossRef]
- Oakley, P.A.; Harrison, D.D.; Harrison, D.E.; Haas, J.W. Evidence-Based Protocol for Structural Rehabilitation of the Spine and Posture: Review of Clinical Biomechanics of Posture (CBP) Publications. J. Can. Chiropr. Assoc. 2005, 49, 270–296. [Google Scholar] [PubMed]
- Moustafa, I.M.; Diab, A.A.; Harrison, D.E. The Effect of Normalizing the Sagittal Cervical Configuration on Dizziness, Neck Pain, and Cervicocephalic Kinesthetic Sensibility: A 1-Year Randomized Controlled Study. Eur. J. Phys. Rehabil. Med. 2017, 53, 57–71. [Google Scholar] [CrossRef] [PubMed]
- Patwardhan, A.G.; Havey, R.M.; Khayatzadeh, S.; Muriuki, M.G.; Voronov, L.I.; Carandang, G.; Nguyen, N.-L.; Ghanayem, A.J.; Schuit, D.; Patel, A.A.; et al. Postural Consequences of Cervical Sagittal Imbalance: A Novel Laboratory Model. Spine 2015, 40, 783–792. [Google Scholar] [CrossRef]
- Paholpak, P.; Vega, A.; Formanek, B.; Tamai, K.; Wang, J.C.; Buser, Z. Impact of Cervical Sagittal Balance and Cervical Spine Alignment on Craniocervical Junction Motion: An Analysis Using Upright Multi-Positional MRI. Eur. Spine J. 2021, 30, 444–453. [Google Scholar] [CrossRef]
- Buonocore, E.; Hartman, J.T.; Nelson, C.L. Cineradiograms of Cervical Spine in Diagnosis of Soft-Tissue Injuries. JAMA 1966, 198, 143–147. [Google Scholar] [CrossRef]
- Hino, H.; Abumi, K.; Kanayama, M.; Kaneda, K. Dynamic Motion Analysis of Normal and Unstable Cervical Spines Using Cineradiography. An in Vivo Study. Spine 1999, 24, 163–168. [Google Scholar] [CrossRef]
- Harrison, D.D.; Janik, T.J.; Troyanovich, S.J.; Holland, B. Comparisons of Lordotic Cervical Spine Curvatures to a Theoretical Ideal Model of the Static Sagittal Cervical Spine. Spine 1996, 21, 667–675. [Google Scholar] [CrossRef]
- Krakenes, J.; Kaale, B.; Moen, G.; Nordli, H.; Gilhus, N.; Rorvik, J. MRI Assessment of the Alar Ligaments in the Late Stage of Whiplash Injury—A Study of Structural Abnormalities and Observer Agreement. Neuroradiology 2002, 44, 617–624. [Google Scholar] [CrossRef] [PubMed]
- Harrison, D.D.; Janik, T.J.; Harrison, G.R.; Troyanovich, S.; Harrison, D.E.; Harrison, S.O. Chiropractic Biophysics Technique: A Linear Algebra Approach to Posture in Chiropractic. J. Manip. Physiol. Ther. 1996, 19, 525–535. [Google Scholar]
- Harrison, D.E.; Cailliet, R.; Harrison, D.D.; Janik, T.J.; Holland, B. A New 3-Point Bending Traction Method for Restoring Cervical Lordosis and Cervical Manipulation: A Nonrandomized Clinical Controlled Trial. Arch. Phys. Med. Rehabil. 2002, 83, 447–453. [Google Scholar] [CrossRef] [PubMed]
- Mesfar, W.; Moglo, K. Effect of the Transverse Ligament Rupture on the Biomechanics of the Cervical Spine under a Compressive Loading. Clin. Biomech. 2013, 28, 846–852. [Google Scholar] [CrossRef]
- Miyamoto, H.; Hashimoto, K.; Ikeda, T.; Akagi, M. Effect of Correction Surgery for Cervical Kyphosis on Compensatory Mechanisms in Overall Spinopelvic Sagittal Alignment. Eur. Spine J. 2017, 26, 2380–2385. [Google Scholar] [CrossRef]
| Patient Number | Gender (M/F) | Age | Duration a (Weeks) | Symptoms b |
|---|---|---|---|---|
| 1 | F | 46 | 7 | Neck pain and weakness, dizziness. |
| 2 | F | 36 | 10 | Neck pain, headaches. |
| 3 | M | 37 | 12 | Pain at the base of the skull, clicking sensation dizziness. |
| 4 | F | 52 | 16 | Head and neck pain, blurred vision. |
| 5 | F | 34 | 16 | Head and neck pain, blurred vision, arm tingling, clicking sensation, sleep disruption. |
| 6 | M | 28 | 19 | Head and neck pain, occipital spasms, blurred vision, dizziness. |
| 7 | F | 35 | 44 | Head and neck pain, arm tingling. |
| 8 | F | 53 | 52 | Head and neck pain, head pressure, pain behind left eye, sleep disruption |
| 9 | F | 30 | 68 | Debilitating Headaches, neck pain. |
| Time of X-ray, Relative to Intervention a | ARA b C2–C7 | C1–2 Lateral Overhang Margin c | ||
|---|---|---|---|---|
| Left | Right | |||
| Patient 1 | Baseline | −14.1° | 8.8 mm | 6.1 mm |
| Post intervention | −30.4° | 6.3 mm | 2.1 mm | |
| Patient 2 | Baseline | −4.1° | 7.5 mm | 1.8 mm |
| Post intervention | −23.6° | 2.3 mm | 1.6 mm | |
| Patient 3 | Baseline | −2.8° | 5.2 mm | 2.4 mm |
| Post Intervention | −4.6° | 1.3 mm | 1.8 mm | |
| Patient 4 | Baseline | 3.0° | 3.6 mm | 1.2 mm |
| Post intervention | −17.9° | 1.1 mm | 0.5 mm | |
| Patient 5 | Baseline | −8.8° | 8.8 mm | 6.1 mm |
| Post intervention | −18.2° | 6.3 mm | 2.1 mm | |
| Patient 6 | Baseline | −19.9° | 3.2 mm | 3.0 mm |
| Post intervention | −29.6° | 2.2 mm | 0.5 mm | |
| Patient 7 | Baseline | −11.2° | 7.0 mm | 1.9 mm |
| Post intervention | −17.0° | 2.5 mm | 1.2 mm | |
| Patient 8 | Baseline | −12.0° | 5.5 mm | 3.5 mm |
| Post intervention | −14.8° | 2.8 mm | 2.9 mm | |
| Patient 9 | Baseline | −19.7° | 4.6 mm | 2.0 mm |
| Post intervention | −29.0° | 2.0 mm | 1.3 mm | |
| Patient | ARA | Left Overhang | Right Overhang |
|---|---|---|---|
| 1 | −16.3 | −2.5 | −4.0 |
| 2 | −19.5 | −5.2 | −0.2 |
| 3 | −1.8 | −3.9 | −0.6 |
| 4 | −20.9 | −2.5 | −0.7 |
| 5 | −9.4 | −2.5 | −4.0 |
| 6 | −9.7 | −1.0 | −2.5 |
| 7 | −5.8 | −4.5 | −0.7 |
| 8 | −2.8 | −2.7 | −0.6 |
| 9 | −9.3 | −2.6 | −0.7 |
| Shapiro-Wilk test of normality p-value a | 0.4 | 0.29 | 0.004 |
| Mean difference (standard deviation) | −10.6 (6.9) | −3.0 (1.27) | −1.6 (1.5) |
| Mean difference 95% CI | [−15.9, −5.3] | [−4.0, −2.1] | [−2.7, −0.4] |
| Test statistic b | −4.6 | −7.2 | −22.5 |
| Degrees of freedom (df) | 8 | 8 | NA |
| p-value | 0.0018 | <0.0001 | 0.0039 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Katz, E.A.; Katz, S.B.; Freeman, M.D. Non-Surgical Management of Upper Cervical Instability via Improved Cervical Lordosis: A Case Series of Adult Patients. J. Clin. Med. 2023, 12, 1797. https://doi.org/10.3390/jcm12051797
Katz EA, Katz SB, Freeman MD. Non-Surgical Management of Upper Cervical Instability via Improved Cervical Lordosis: A Case Series of Adult Patients. Journal of Clinical Medicine. 2023; 12(5):1797. https://doi.org/10.3390/jcm12051797
Chicago/Turabian StyleKatz, Evan A., Seana B. Katz, and Michael D. Freeman. 2023. "Non-Surgical Management of Upper Cervical Instability via Improved Cervical Lordosis: A Case Series of Adult Patients" Journal of Clinical Medicine 12, no. 5: 1797. https://doi.org/10.3390/jcm12051797
APA StyleKatz, E. A., Katz, S. B., & Freeman, M. D. (2023). Non-Surgical Management of Upper Cervical Instability via Improved Cervical Lordosis: A Case Series of Adult Patients. Journal of Clinical Medicine, 12(5), 1797. https://doi.org/10.3390/jcm12051797









