A Pilot Multisensory Approach for Emotional Eating: Pivoting from Virtual Reality to a 2-D Telemedicine Intervention during the COVID-19 Pandemic
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Study Design
2.3. Treatment as Usual (TAU)
2.4. Non-Immersive Multisensory Virtual Experience for Emotional Regulation Intervention (VE-ER)
2.5. Measures
2.5.1. Descriptive Variables
2.5.2. Feasibility
2.5.3. Acceptability
2.5.4. Exploratory Outcomes of Effectiveness
- -
- Difficulties in Emotion Regulation (DERS) [48]. This self-report scale asks respondents to rate how they manage their emotions on a 5-point Likert scale ranging from never to always. Six subscales emerge from the questionnaires: (1) “The inability to accept emotional responses”, (2) “Impulse control difficulties”, (3) “Difficulty engaging in goal-directed behavior”, (4) “A lack of emotional awareness”, (5) “Lack of emotional clarity”, and (6) “Limited access to emotion regulation strategies”. Higher scores indicate greater problems with emotion regulation. In this study, we considered only the Total Scores that ranged from 36 to 180. There are no standardized clinical cutoffs for this measure; however, prior research suggests that the clinical range based on the DERS total score varies from averages of approximately 80 to 127 [49]. This measure has good internal consistency, good test-retest reliability, and predictive validity [50].
- -
- The Dutch Eating Behavior Questionnaire (DEBQ) [51]. The DEBQ is a 33-item self-report questionnaire that assesses three distinct eating behaviors in adults: (1) emotional eating, (2) external eating, and (3) restrained eating. Items on the DEBQ range from 1 (never) to 5 (very often), with higher scores indicating greater endorsement of the eating behavior. Similar to the DERS, there are no standardized clinical cutoffs. Research community samples suggest a score > 3.25 as the 80% percentile. The DEBQ’s subscales have good internal consistency, test-retest reliability over a 4-week period, and criterion validity [51]. For reliability, De Cavalho and colleagues identified an acceptable Spearman correlation coefficient (rho > 0.30 and p < 0.05) and Cronbach’s alpha (α ≥ 0.70) for all DEBQ items of the online format [52].
- -
- Frequency of disordered eating. At the beginning of each session in both conditions, therapists assessed the participant’s frequency of disordered eating. This information was entered into a Therapist Note on Qualtrics. Preliminary signals of effectiveness were determined by changes in the frequency of disordered eating behaviors over the previous 7 days (e.g., number of EE episodes, evaluation of the trend of EE, number of objective binge episodes (OBEs), subjective binge episodes (SBEs), purging episodes). EE episode frequency was assessed using a 5-point Likert scale: Never (1), Seldom (2), Sometimes (3), Often (4), Always (5). Binge episodes were distinguished as objective or subjective as defined by the Eating Disorder Examination Questionnaire (EDE-Q). OBE and SBE episodes were assessed asking for a specific number of episodes over the prior week.
- -
- The Acceptance and Action Questionnaire (AAQ-II) [53]. This seven-item measure assesses psychological inflexibility and experiential avoidance. Items range from 1 (never true) to 7 (always true). The scale is scored by summing the seven items. Higher total scores indicate less flexibility, while lower total scores mean more flexibility (total range: 7–49). This measure has good internal consistency (α = 0.88) and good test retest reliability over 3 and 12 months at 0.81 and 0.79, respectively.
- -
- Weight Efficacy Life-Style Questionnaire (WELSQ) [54]. The Weight Efficacy Lifestyle Questionnaire (WELSQ) is a commonly used measure of eating self-efficacy consisting of 20 items and five situational factors (negative emotions, availability, social pressure, physical discomfort, positive activities). Respondents rate their confidence to resist eating in certain situations on a 10-point Likert scale ranging from 0 (not confident) to 9 (very confident). The WELSQ yields five subscale scores ranging from 0 to 36. High WELSQ scores indicate a higher self-efficacy to resist eating.
2.6. Data Analysis
3. Results
3.1. Descriptive Analysis
3.2. Feasibility
3.2.1. Therapists
3.2.2. Patients
3.3. Acceptability
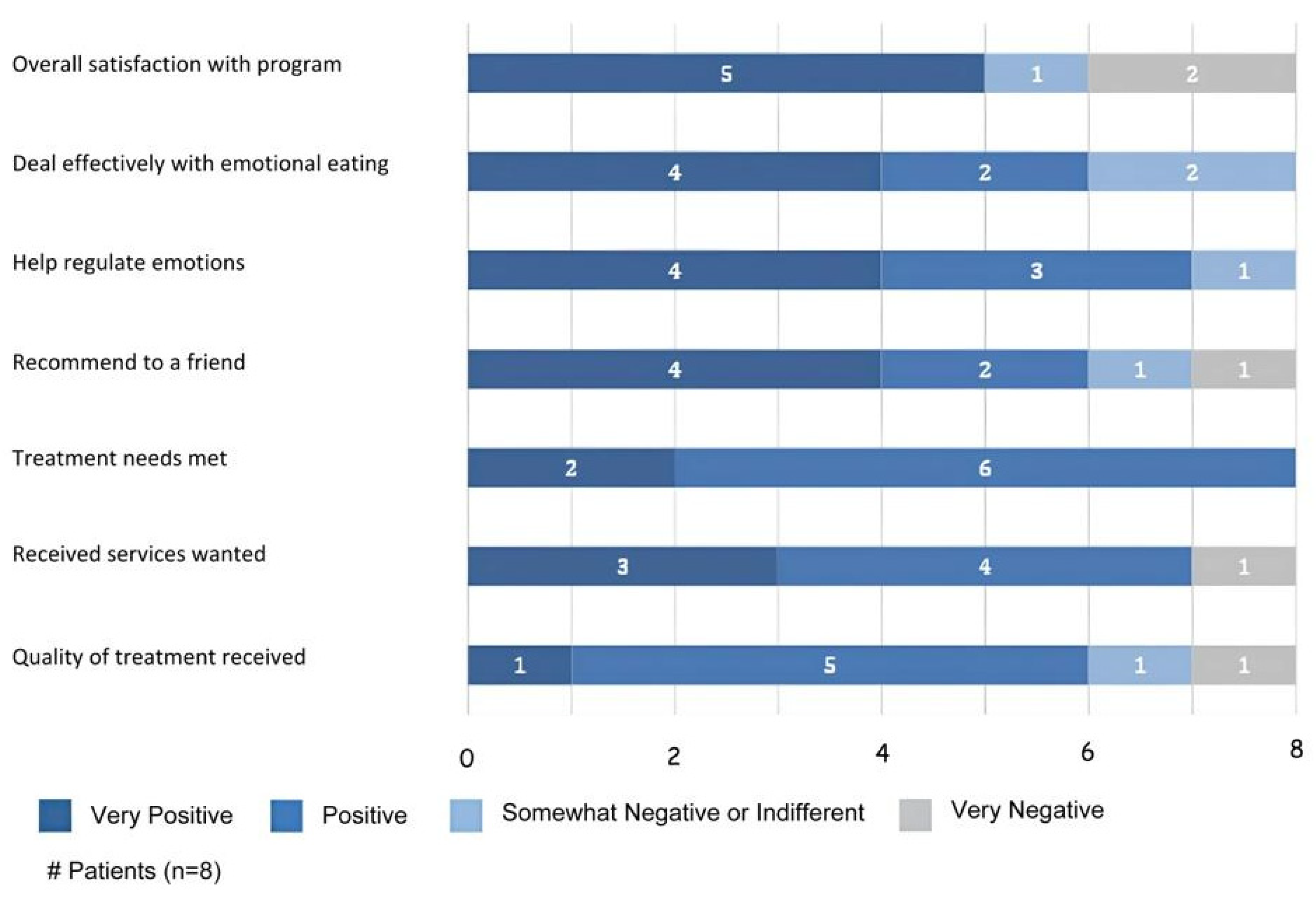
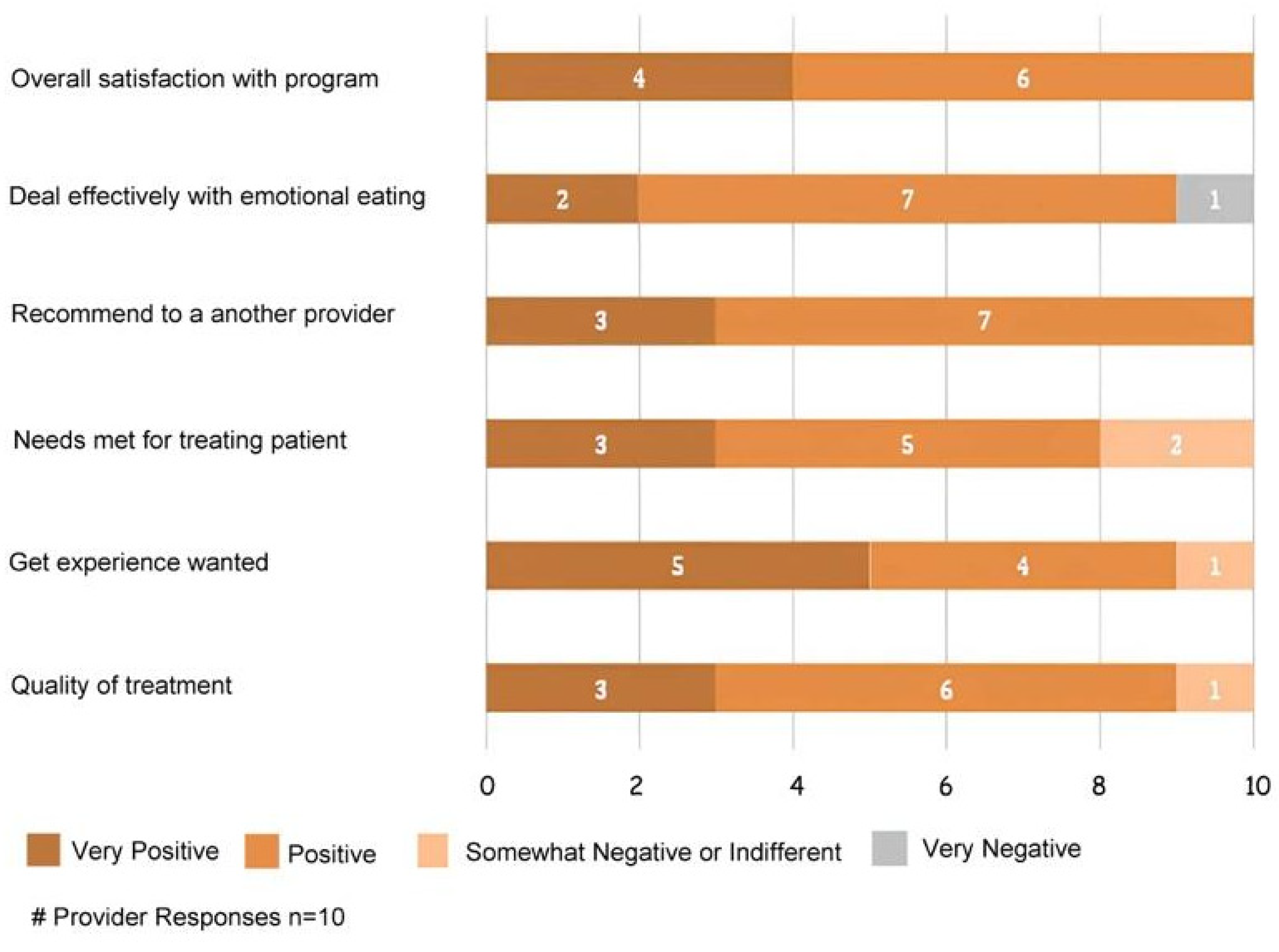
3.3.1. VE-ER Intervention
3.3.2. TAU Treatment
3.3.3. Therapists’ Satisfaction with Virtual Intervention
3.4. Exploratory Outcomes of Effectiveness
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- McRae, K.; Gross, J.J. Emotion regulation. Emotion 2020, 20, 1–9. [Google Scholar] [CrossRef]
- Vintró-Alcaraz, C.; Munguía, L.; Granero, R.; Gaspar-Pérez, A.; Solé-Morata, N.; Sánchez, I.; Sánchez-González, J.; Menchón, J.M.; Jiménez-Murcia, S.; Fernández-Aranda, F. Emotion regulation as a transdiagnostic factor in eating disorders and gambling disorder: Treatment outcome implications. J. Behav. Addict. 2022, 11, 140–146. [Google Scholar] [CrossRef] [PubMed]
- Reichenberger, J.; Schnepper, R.; Arend, A.-K.; Blechert, J. Emotional eating in healthy individuals and patients with an eating disorder: Evidence from psychometric, experimental and naturalistic studies. Proc. Nutr. Soc. 2020, 79, 290–299. [Google Scholar] [CrossRef]
- Ricca, V.; Castellini, G.; Lo Sauro, C.; Ravaldi, C.; Lapi, F.; Mannucci, E.; Rotella, C.M.; Faravelli, C. Correlations between binge eating and emotional eating in a sample of overweight subjects. Appetite 2009, 53, 418–421. [Google Scholar] [CrossRef] [PubMed]
- Barak, R.; Shuval, K.; Li, Q.; Oetjen, R.; Drope, J.; Yaroch, A.L.; Fennis, B.M.; Harding, M. Emotional eating in adults: The role of sociodemographics, lifestyle behaviors, and self-regulation—Findings from a U.S. national study. Int. J. Environ. Res. Public Health 2021, 18, 1744. [Google Scholar] [CrossRef] [PubMed]
- Bemanian, M.; Mæland, S.; Blomhoff, R.; Rabben, Å.K.; Arnesen, E.K.; Skogen, J.C.; Fadnes, L.T. Emotional eating in relation to worries and psychological distress amid the covid-19 pandemic: A population-based survey on adults in Norway. Int. J. Environ. Res. Public Health 2021, 18, 130. [Google Scholar] [CrossRef]
- Cecchetto, C.; Aiello, M.; Gentili, C.; Ionta, S.; Osimo, S.A. Increased emotional eating during COVID-19 associated with lockdown, psychological and social distress. Appetite 2021, 160, 105122. [Google Scholar] [CrossRef]
- Braden, A.; Musher-Eizenman, D.; Watford, T.; Emley, E. Eating when depressed, anxious, bored, or happy: Are emotional eating types associated with unique psychological and physical health correlates? Appetite 2018, 125, 410–417. [Google Scholar] [CrossRef]
- Lazarevich, I.; Irigoyen Camacho, M.E.; Velázquez-Alva, M.D.C.; Zepeda Zepeda, M. Relationship among obesity, depression, and emotional eating in young adults. Appetite 2016, 107, 639–644. [Google Scholar] [CrossRef]
- Schneider, K.L.; Appelhans, B.M.; Whited, M.C.; Oleski, J.; Pagoto, S.L. Trait anxiety, but not trait anger, predisposes obese individuals to emotional eating. Appetite 2010, 55, 701–706. [Google Scholar] [CrossRef]
- Nguyen-Rodriguez, S.T.; Chou, C.-P.; Unger, J.B.; Spruijt-Metz, D. BMI as a moderator of perceived stress and emotional eating in adolescents. Eat. Behav. 2008, 9, 238–246. [Google Scholar] [CrossRef]
- Tchanturia, K.; Davies, H.; Harrison, A.; Fox, J.R.E.; Treasure, J.; Schmidt, U. Altered social hedonic processing in eating disorders. Int. J. Eat. Disord. 2012, 45, 962–969. [Google Scholar] [CrossRef] [PubMed]
- Torres, S.J.; Nowson, C.A. Relationship between stress, eating behavior, and obesity. Nutrition 2007, 23, 887–894. [Google Scholar] [CrossRef] [PubMed]
- Pink, A.E.; Lee, M.; Price, M.; Williams, C. A Serial mediation model of the relationship between alexithymia and BMI: The role of negative affect, negative urgency and emotional eating. Appetite 2019, 133, 270–278. [Google Scholar] [CrossRef]
- Tan, C.C.; Chow, C.M. Stress and emotional eating: The mediating role of eating dysregulation. Personal. Individ. Differ. 2014, 66, 1–4. [Google Scholar] [CrossRef]
- Casagrande, M.; Mingarelli, A.; Guarino, A.; Favieri, F.; Boncompagni, I.; Germanò, R.; Germanò, G.; Forte, G. Alexithymia: A facet of uncontrolled hypertension. Int. J. Psychophysiol. 2019, 146, 180–189. [Google Scholar] [CrossRef]
- Taylor, G.J.; Parker, J.D.; Bagby, R.M.; Bourke, M.P. Relationships between alexithymia and psychological characteristics associated with eating disorders. J. Psychosom. Res. 1996, 41, 561–568. [Google Scholar] [CrossRef]
- Blair, A.J.; Lewis, V.J.; Booth, D.A. Does emotional eating interfere with success in attempts at weight control? Appetite 1990, 15, 151–157. [Google Scholar] [CrossRef]
- Frayn, M.; Knäuper, B. Emotional eating and weight in adults: A review. Curr. Psychol. J. Divers. Perspect. Divers. Psychol. Issues 2018, 37, 924–933. [Google Scholar] [CrossRef]
- Vartanian, L.R.; Porter, A.M. Weight stigma and eating behavior: A review of the literature. Appetite 2016, 102, 3–14. [Google Scholar] [CrossRef]
- Michopoulos, V.; Powers, A.; Moore, C.; Villarreal, S.; Ressler, K.J.; Bradley, B. The mediating role of emotion dysregulation and depression on the relationship between childhood trauma exposure and emotional eating. Appetite 2015, 91, 129–136. [Google Scholar] [CrossRef] [PubMed]
- Lattimore, P. Mindfulness-based emotional eating awareness training: Taking the emotional out of eating. Eat. Weight Disord. 2020, 25, 649–657. [Google Scholar] [CrossRef] [PubMed]
- Osborne, E.L.; Ainsworth, B.; Chadwick, P.; Atkinson, M.J. The role of emotion regulation in the relationship between mindfulness and risk factors for disordered eating: A longitudinal mediation analysis. Int. J. Eat. Disord. 2023, 56, 458–463. [Google Scholar] [CrossRef]
- Grohmann, D.; Laws, K.R. Two decades of mindfulness-based interventions for binge eating: A systematic review and meta-analysis. J. Psychosom. Res. 2021, 149, 110592. [Google Scholar] [CrossRef]
- Katterman, S.N.; Kleinman, B.M.; Hood, M.M.; Nackers, L.M.; Corsica, J.A. Mindfulness meditation as an intervention for binge eating, emotional eating, and weight loss: A systematic review. Eat. Behav. 2014, 15, 197–204. [Google Scholar] [CrossRef]
- Beaulac, J.; Sandre, D.; Mercer, D. Impact on mindfulness, emotion regulation, and emotional overeating of a DBT skills training group: A pilot study. Eat. Weight Disord. 2019, 24, 373–377. [Google Scholar] [CrossRef]
- Geraets, C.N.W.; van der Stouwe, E.C.D.; Pot-Kolder, R.; Veling, W. Advances in immersive virtual reality interventions for mental disorders: A new reality? Curr. Opin. Psychol. 2021, 41, 40–45. [Google Scholar] [CrossRef]
- Colombo, D.; Díaz-García, A.; Fernandez-Álvarez, J.; Botella, C. Virtual reality for the enhancement of emotion regulation. Clin. Psychol. Psychother. 2021, 28, 519–537. [Google Scholar] [CrossRef] [PubMed]
- Brown, T.; Vogel, E.N.; Adler, S.; Bohon, C.; Bullock, K.; Nameth, K.; Riva, G.; Safer, D.L.; Runfola, C.D. Bringing virtual reality from clinical trials to clinical practice for the treatment of eating disorders: An example using virtual reality cue exposure therapy. J. Med. Internet Res. 2020, 22, e16386. [Google Scholar] [CrossRef]
- Mancini, A.; Mancini, F. Rescripting memory, redefining the self: A meta-emotional perspective on the hypothesized mechanism(s) of imagery rescripting. Front. Psychol. 2018, 9, 581. [Google Scholar] [CrossRef] [PubMed]
- Arntz, A. Imagery rescripting as a therapeutic technique: Review of clinical trials, basic studies, and research agenda. J. Exp. Psychopathol. 2012, 3, 189–208. [Google Scholar] [CrossRef]
- Ghaderi, A.; Welch, E.; Zha, C.; Holmes, E.A. Imagery rescripting for reducing body image dissatisfaction: A randomized controlled trial. Cogn. Ther. Res. 2022, 46, 721–734. [Google Scholar] [CrossRef]
- Morina, N.; Lancee, J.; Arntz, A. Imagery rescripting as a clinical intervention for aversive memories: A meta-analysis. J. Behav. Ther. Exp. Psychiatry 2017, 55, 6–15. [Google Scholar] [CrossRef]
- Riva, G. The key to unlocking the virtual body: Virtual reality in the treatment of obesity and eating disorders. J. Diabetes Sci. Technol. 2011, 5, 283–292. [Google Scholar] [CrossRef] [PubMed]
- Wilson, M. Six views of embodied cognition. Psychon. Bull. Rev. 2002, 9, 625–636. [Google Scholar] [CrossRef] [PubMed]
- Riva, G. The neuroscience of body memory: From the self through the space to the others. Cortex 2018, 104, 241–260. [Google Scholar] [CrossRef] [PubMed]
- Barrett, L.F. The theory of constructed emotion: An active inference account of interoception and categorization. Soc. Cogn. Affect. Neurosci. 2017, 12, 1–23. [Google Scholar] [CrossRef] [PubMed]
- Barrett-Cheetham, E.; Williams, L.A.; Bednall, T.C. A differentiated approach to the link between positive emotion, motivation, and eudaimonic well-being. J. Posit. Psychol. 2016, 11, 595–608. [Google Scholar] [CrossRef]
- Damasio, A. Self Comes to Mind: Constructing the Conscious Brain; Pantheon/Random House: New York, NY, USA, 2010; p. 367. ISBN 978-0-307-37875-0. [Google Scholar]
- Damasio, A.; Carvalho, G.B. The nature of feelings: Evolutionary and neurobiological origins. Nat. Rev. Neurosci. 2013, 14, 143–152. [Google Scholar] [CrossRef]
- Malighetti, C.; Schnitzer, C.; Potter, G.; Nameth, K.; Brown, T.; Vogel, E.; Riva, G.; Runfola, C.D.; Safer, D.L. Rescripting emotional eating with virtual reality: A case study. Annu. Rev. Cyberther. Telemed. 2021, 19, 117–121. [Google Scholar]
- Malighetti, C.; Bernardelli, L.; Pancini, E.; Riva, G.; Villani, D. Promoting emotional and psychological well-being during COVID-19 pandemic: A self-help virtual reality intervention for university students. Cyberpsychol. Behav. Soc. Netw. 2023, 26, 309–317. [Google Scholar] [CrossRef] [PubMed]
- Riva, G.; Bernardelli, L.; Castelnuovo, G.; Di Lernia, D.; Tuena, C.; Clementi, A.; Pedroli, E.; Malighetti, C.; Sforza, F.; Wiederhold, B.K.; et al. A virtual reality-based self-help intervention for dealing with the psychological distress associated with the COVID-19 lockdown: An effectiveness study with a two-week follow-up. Int. J. Environ. Res. Public Health 2021, 18, 8188. [Google Scholar] [CrossRef]
- Meyer, D.; Van Rheenen, T.E.; Neill, E.; Phillipou, A.; Tan, E.J.; Toh, W.L.; Sumner, P.J.; Rossell, S.L. Surviving the COVID-19 pandemic: An examination of adaptive coping strategies. Heliyon 2022, 8, e09508. [Google Scholar] [CrossRef] [PubMed]
- Farahimanesh, S.; Serino, S.; Tuena, C.; Di Lernia, D.; Wiederhold, B.K.; Bernardelli, L.; Riva, G.; Moradi, A. Effectiveness of a virtual-reality-based self-help intervention for lowering the psychological burden during the COVID-19 pandemic: Results from a randomized controlled trial in Iran. J. Clin. Med. 2023, 12, 2006. [Google Scholar] [CrossRef] [PubMed]
- Leon, A.C.; Davis, L.L.; Kraemer, H.C. The role and interpretation of pilot studies in clinical research. J. Psychiatr. Res. 2011, 45, 626–629. [Google Scholar] [CrossRef] [PubMed]
- Larsen, D.L.; Attkisson, C.C.; Hargreaves, W.A.; Nguyen, T.D. Assessment of client/patient satisfaction: Development of a general scale. Eval. Program Plan. 1979, 2, 197–207. [Google Scholar] [CrossRef]
- Gratz, K.L.; Roemer, L. Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and initial validation of the difficulties in emotion regulation scale. J. Psychopathol. Behav. Assess. 2004, 26, 41–54. [Google Scholar] [CrossRef]
- Harrison, A.; Sullivan, S.; Tchanturia, K.; Treasure, J. Emotional functioning in eating disorders: Attentional bias, emotion recognition and emotion regulation. Psychol. Med. 2010, 40, 1887–1897. [Google Scholar] [CrossRef]
- Hallion, L.S.; Steinman, S.A.; Tolin, D.F.; Diefenbach, G.J. Psychometric properties of the difficulties in emotion regulation scale (DERS) and its short forms in adults with emotional disorders. Front. Psychol. 2018, 9, 539. [Google Scholar] [CrossRef]
- Van Strien, T.; Frijters, J.E.; Bergers, G.P.; Defares, P.B. The Dutch eating behavior questionnaire (DEBQ) for assessment of restrained, emotional, and external eating behavior. Int. J. Eat. Disord. 1986, 5, 295–315. [Google Scholar] [CrossRef]
- De Carvalho, M.V.; Cardoso, A.G.d.A.; Feuerstein, S.C.; de Sousa, R.R.; Collese, T.S.; Torres-Leal, F.L.; Nascimento-Ferreira, M.V.; De Moraes, A.C.F. Reliability and validity of the dutch eating behavior questionnaire in an online format for university students from low-income regions in a pandemic context: A 24 hour MESYN study. Front. Epidemiol. 2023, 2, 1036631. [Google Scholar] [CrossRef]
- Tyndall, I.; Waldeck, D.; Pancani, L.; Whelan, R.; Roche, B.; Dawson, D.L. The acceptance and action questionnaire-II (AAQ-II) as a measure of experiential avoidance: Concerns over discriminant validity. J. Context. Behav. Sci. 2019, 12, 278–284. [Google Scholar] [CrossRef]
- Navidian, A. Reliability and validity of the weight efficacy lifestyle questionnaire in overweight and obese individuals. Int. J. Behav. Sci. 2009, 3, 217–222. [Google Scholar]
- Brownley, K.A.; Berkman, N.D.; Peat, C.M.; Lohr, K.N.; Cullen, K.E.; Bann, C.M.; Bulik, C.M. Binge-eating disorder in adults: A systematic review and meta-analysis. Ann. Intern. Med. 2016, 165, 409–420. [Google Scholar] [CrossRef] [PubMed]
- De Zwaan, M.; Herpertz, S.; Zipfel, S.; Svaldi, J.; Friederich, H.-C.; Schmidt, F.; Mayr, A.; Lam, T.; Schade-Brittinger, C.; Hilbert, A. Effect of internet-based guided self-help vs individual face-to-face treatment on full or subsyndromal binge eating disorder in overweight or obese patients: The INTERBED randomized clinical trial. JAMA Psychiatry 2017, 74, 987–995. [Google Scholar] [CrossRef]
- Runfola, C.D.; Kirby, J.S.; Baucom, D.H.; Fischer, M.S.; Baucom, B.R.W.; Matherne, C.E.; Pentel, K.Z.; Bulik, C.M. A pilot open trial of UNITE-BED: A couple-based intervention for binge-eating disorder. Int. J. Eat. Disord. 2018, 51, 1107–1112. [Google Scholar] [CrossRef] [PubMed]
- Safer, D.L.; Robinson, A.H.; Jo, B. Outcome from a randomized controlled trial of group therapy for binge eating disorder: Comparing dialectical behavior therapy adapted for binge eating to an active comparison group therapy. Behav. Ther. 2010, 41, 106–120. [Google Scholar] [CrossRef]
- De Carvalho, M.R.; Dias, T.R.d.S.; Duchesne, M.; Nardi, A.E.; Appolinario, J.C. Virtual reality as a promising strategy in the assessment and treatment of bulimia nervosa and binge eating disorder: A systematic review. Behav. Sci. 2017, 7, 43. [Google Scholar] [CrossRef]
- Zaitsoff, S.; Pullmer, R.; Cyr, M.; Aime, H. The role of the therapeutic alliance in eating disorder treatment outcomes: A systematic review. Eat. Disord. 2015, 23, 99–114. [Google Scholar] [CrossRef]
- Dingemans, A.; Danner, U.; Parks, M. Emotion regulation in binge eating disorder: A review. Nutrients 2017, 9, 1274. [Google Scholar] [CrossRef]
- Surmay, C.; Vo, M.; Derenne, J.; Sherman, D. Virtual reality mindfulness therapy for anxiety and pain management in adolescent and young adult patients with eating disorders. J. Adolesc. Health 2020, 66, S62–S63. [Google Scholar] [CrossRef]
- Ma, J.; Zhao, D.; Xu, N.; Yang, J. The effectiveness of immersive virtual reality (VR) based mindfulness training on improvement mental-health in adults: A narrative systematic review. Explore 2023, 19, 310–318. [Google Scholar] [CrossRef]
- Stepanova, E.; Quesnel, D.; Riecke, B. Understanding AWE: Can a virtual journey, inspired by the overview effect, lead to an increased sense of interconnectedness? Front. Digit. Humanit. 2019, 6, 9. [Google Scholar] [CrossRef]
- Bond, F.W.; Hayes, S.C.; Baer, R.A.; Carpenter, K.M.; Guenole, N.; Orcutt, H.K.; Waltz, T.; Zettle, R.D. Preliminary psychometric properties of the acceptance and action questionnaire-II: A revised measure of psychological inflexibility and experiential avoidance. Behav. Ther. 2011, 42, 676–688. [Google Scholar] [CrossRef] [PubMed]
| Measures | VE-ER Group n = 10 | TAU Group n = 11 | t | Sign |
|---|---|---|---|---|
| Mean ± SD | Mean ± SD | |||
| DERS_TOT | 109.80 ± 22.90 | 108.64 ± 22.47 | 0.117 | 0.908 |
| DEBQ-R | 3.09 ± 0.79 | 2.78 ± 0.50 | 1.064 | 0.301 |
| DEBQ-E | 4.12 ± 0.49 | 3.55 ± 1 | 1.634 | 0.119 |
| DEBQ-EXT | 3.35 ± 0.88 | 2.99 ± 0.60 | 1.093 | 0.288 |
| AAQ_II | 33.40 ± 6.50 | 30.82 ± 5.98 | 0.948 | 0.355 |
| WELSQ_NE | 9.90 ± 6.80 | 15.73 ± 6.21 | −2.051 | 0.054 |
| WELSQ_AV | 16.40 ± 8.50 | 19.18 ± 8.32 | −0.757 | 0.458 |
| WELSQ_SP | 16.70 ± 8.23 | 21.36 ± 6.21 | 0.351 | 0.157 |
| WELSQ_PD | 17.20 ± 9.36 | 20.18 ± 6.94 | −0.834 | 0.414 |
| WELSQ_PA | 22 ± 5.59 | 24.45 ± 4.84 | −1.092 | 0.288 |
| #OBES | 1.50 ± 1.50 | 0.73 ± 1.47 | 0.748 | 0.984 |
| #SBES | 1.70 ± 1.98 | 3.43 ± 2.57 | −1.962 | 0.951 |
| #PURGES | 0.60 ± 1.35 | 0.64 ± 2.11 | −0.047 | 0.75 |
| #EE | 3.40 ± 1.07 | 2.92 ± 0.90 | 1.26 | 0.222 |
| VE-ER Group (n = 10) | TAU Group (n = 11) | Anova | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Measures | Pre | Post | Pre | Post | Time | Group × Time | |||
| Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | F | Sig. | F | Sig. | η2 | |
| #EE | 3.40 ± 1.07 | 1.90 ± 0.73 | 2.92 ± 0.90 | 2 ± 0.60 | 13.07 | 0.002 * | 4.95 | 0.038 * | 0.39 |
| #SBES | 1.70 ± 1.98 | 0.80 ± 1.13 | 3.43 ± 2.57 | 1.42 ± 1.24 | 9.29 | 0.007 * | 2.69 | 0.117 | 0.13 |
| #Purge | 0.60 ± 1.35 | 0 ± 0.00 | 0.64 ± 2.11 | 0.45 ± 1.50 | 3.03 | 0.098 | 0.869 | 0.363 | 0.32 |
| #OBES | 1.50 ± 1.50 | 0.80 ± 1.13 | 0.73 ± 1.47 | 0.55 ± 0.88 | 7.61 | 0.012 * | 0.005 | 0.947 | 0.27 |
| VE-ER Group | TAU Group | |||||||
|---|---|---|---|---|---|---|---|---|
| Pre n = 10 | Post n = 5 | Pre n = 11 | Post n = 11 | |||||
| Measures | Mean ± SD | Mean ± SD | z | Sign | Mean ± SD | Mean ± SD | z | Sign |
| DERS_TOT | 109.80 ± 22.90 | 86 ± 26.46 | −2.032 | 0.042 * | 108.64 ± 22.47 | 102.09 ± 20.62 | −1.07 | 0.284 |
| DEBQ-R | 3.09 ± 0.79 | 2.66 ± 0.95 | −0.674 | 0.500 | 2.78 ± 0.50 | 2.76 ± 0.72 | 0.089 | 0.929 |
| DEBQ-E | 4.12 ± 0.49 | 3.20 ± 0.67 | −1.753 | 0.060 | 3.55 ± 1 | 3.38 ± 0.92 | −0.561 | 0.575 |
| DEBQ-EXT | 3.35 ± 0.88 | 3.10 ± 0.99 | −1.604 | 0.109 | 2.99 ± 0.60 | 2.97 ± 0.49 | −0.102 | 0.919 |
| AAQ_II | 33.40 ± 6.50 | 30.20 ± 10.68 | −1.095 | 0.273 | 30.82 ± 5.98 | 29.91 ± 7.36 | −0.66 | 0.504 |
| WELSQ_NE | 9.90 ± 6.80 | 18.80 ± 5.63 | −1.753 | 0.070 | 15.73 ± 6.21 | 15 ± 5.86 | −0.67 | 0.501 |
| WELSQ_AV | 16.40 ± 8.50 | 20.80 ± 9.49 | −944 | 0.354 | 19.18 ± 8.32 | 16.82 ± 8.08 | −0.66 | −505 |
| WELSQ_SP | 16.70 ± 8.23 | 23.40 ± 7.05 | −1.214 | 0.225 | 21.36 ± 6.21 | 19 ± 11.27 | −81 | 0.413 |
| WELSQ_PD | 17.20 ± 9.36 | 23.40 ± 8.26 | 0.000 | 1 | 20.18 ± 6.94 | 20.18 ± 5.28 | −0.35 | 0.720 |
| WELSQ_PA | 22.99 ± 5.59 | 23.40 ± 7.12 | −0.406 | 0.684 | 24.45 ± 4.69 | 22.36 ± 6.57 | −0.75 | 0.449 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Malighetti, C.; Schnitzer, C.K.; YorkWilliams, S.L.; Bernardelli, L.; Runfola, C.D.; Riva, G.; Safer, D.L. A Pilot Multisensory Approach for Emotional Eating: Pivoting from Virtual Reality to a 2-D Telemedicine Intervention during the COVID-19 Pandemic. J. Clin. Med. 2023, 12, 7402. https://doi.org/10.3390/jcm12237402
Malighetti C, Schnitzer CK, YorkWilliams SL, Bernardelli L, Runfola CD, Riva G, Safer DL. A Pilot Multisensory Approach for Emotional Eating: Pivoting from Virtual Reality to a 2-D Telemedicine Intervention during the COVID-19 Pandemic. Journal of Clinical Medicine. 2023; 12(23):7402. https://doi.org/10.3390/jcm12237402
Chicago/Turabian StyleMalighetti, Clelia, Ciara Kelly Schnitzer, Sophie Lou YorkWilliams, Luca Bernardelli, Cristin D. Runfola, Giuseppe Riva, and Debra L. Safer. 2023. "A Pilot Multisensory Approach for Emotional Eating: Pivoting from Virtual Reality to a 2-D Telemedicine Intervention during the COVID-19 Pandemic" Journal of Clinical Medicine 12, no. 23: 7402. https://doi.org/10.3390/jcm12237402
APA StyleMalighetti, C., Schnitzer, C. K., YorkWilliams, S. L., Bernardelli, L., Runfola, C. D., Riva, G., & Safer, D. L. (2023). A Pilot Multisensory Approach for Emotional Eating: Pivoting from Virtual Reality to a 2-D Telemedicine Intervention during the COVID-19 Pandemic. Journal of Clinical Medicine, 12(23), 7402. https://doi.org/10.3390/jcm12237402







