Male and Female Discrepancies in Anxiety, Depressive Symptoms, and Coping Strategies among Orthognathic Patients: A Cross-Sectional Analysis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Research Design and Ethical Considerations
2.2. Inclusion Criteria and Definitions
2.3. Variables
2.4. Surveys Employed
- (a)
- Disengagement: This is a form of avoidance coping, where individuals detach themselves from the stressor or the associated emotions. A higher score in this subscale might indicate that a person tends to avoid dealing with the stressor.
- (b)
- Engagement: This is an approach coping strategy, where individuals actively confront and engage with the stressor. A higher score here might mean that the individual tends to address stressors head-on.
- (c)
- Emotion Focused: This type of coping concerns managing emotional distress rather than the actual problem or situation causing the distress. Higher scores indicate that the individual frequently uses emotion-focused strategies like seeking emotional support or expressing feelings.
- (d)
- Problem Focused: This strategy is about directly addressing the problem. Higher scores on this subscale mean that the individual prefers to take direct actions to resolve the stressor.
2.5. Statistical Analysis
3. Results
4. Discussion
4.1. Important Findings and Literature Review
4.2. Study Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Khechoyan, D.Y. Orthognathic Surgery: General Considerations. Semin. Plast. Surg. 2013, 27, 133–136. [Google Scholar] [CrossRef] [PubMed]
- Seo, H.J.; Choi, Y.-K. Current trends in orthognathic surgery. Arch. Craniofac. Surg. 2021, 22, 287–295. [Google Scholar] [CrossRef]
- Robinson, R.C.; Holm, R.L. Orthognathic Surgery for Patients with Maxillofacial Deformities. AORN J. 2010, 92, 28–52. [Google Scholar] [CrossRef] [PubMed]
- Hammoudeh, J.A.; Howell, L.K.; Boutros, S.; Scott, M.A.; Urata, M.M. Current Status of Surgical Planning for Orthognathic Surgery: Traditional Methods versus 3D Surgical Planning. Plast. Reconstr. Surg. Glob. Open 2015, 3, e307. [Google Scholar] [CrossRef]
- Shi, P.; Huang, Y.; Kou, H.; Wang, T.; Chen, H. Risk Factors for Facial Appearance Dissatisfaction among Orthognathic Patients: Comparing Patients to a Non-Surgical Sample. Front. Psychol. 2019, 10, 2775. [Google Scholar] [CrossRef] [PubMed]
- Sarwer, D.B.; Siminoff, L.A.; Gardiner, H.M.; Spitzer, J.C. The psychosocial burden of visible disfigurement following traumatic injury. Front. Psychol. 2022, 13, 979574. [Google Scholar] [CrossRef] [PubMed]
- Cariati, P.; Martinez, R.; Martinez-Lara, I. Psycho-social impact of orthogathic sugery. J. Clin. Exp. Dent. 2016, 8, e540–e545. [Google Scholar] [CrossRef]
- Farhane-Medina, N.Z.; Luque, B.; Tabernero, C.; Castillo-Mayén, R. Factors associated with gender and sex differences in anxiety prevalence and comorbidity: A systematic review. Sci. Prog. 2022, 105, 368504221135469. [Google Scholar] [CrossRef]
- McLean, C.P.; Asnaani, A.; Litz, B.T.; Hofmann, S.G. Gender differences in anxiety disorders: Prevalence, course of illness, comorbidity and burden of illness. J. Psychiatr. Res. 2011, 45, 1027–1035. [Google Scholar] [CrossRef]
- Albert, P.R. Why is depression more prevalent in women? J. Psychiatry Neurosci. 2015, 40, 219–221. [Google Scholar] [CrossRef]
- Cholankeril, R.; Xiang, E.; Badr, H. Gender Differences in Coping and Psychological Adaptation during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2023, 20, 993. [Google Scholar] [CrossRef]
- Graves, B.S.; Hall, M.E.; Dias-Karch, C.; Haischer, M.H.; Apter, C. Gender differences in perceived stress and coping among college students. PLoS ONE 2021, 16, e0255634. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.-K. Complications associated with orthognathic surgery. J. Korean Assoc. Oral Maxillofac. Surg. 2017, 43, 3–15. [Google Scholar] [CrossRef] [PubMed]
- Frost, V.; Peterson, G. Psychological aspects of orthognathic surgery: How people respond to facial change. Oral Surgery, Oral Med. Oral Pathol. 1991, 71, 538–542. [Google Scholar] [CrossRef] [PubMed]
- Cunningham, S.J.; Hunt, N.P.; Feinmann, C. Psychological aspects of orthognathic surgery: A review of the literature. The Int. J. Adult Orthod. Orthognath. Surg. 1995, 10, 159–172. [Google Scholar]
- Zamboni, R.; de Moura, F.R.R.; Brew, M.C.; Rivaldo, E.G.; Braz, M.A.; Grossmann, E.; Bavaresco, C.S. Impacts of Orthognathic Surgery on Patient Satisfaction, Overall Quality of Life, and Oral Health-Related Quality of Life: A Systematic Literature Review. Int. J. Dent. 2019, 2019, 2864216. [Google Scholar] [CrossRef]
- Brunault, P.; Battini, J.; Potard, C.; Jonas, C.; Zagala-Bouquillon, B.; Chabut, A.; Mercier, J.-M.; Bedhet, N.; Réveillère, C.; Goga, D.; et al. Orthognathic surgery improves quality of life and depression, but not anxiety, and patients with higher preoperative depression scores improve less. Int. J. Oral Maxillofac. Surg. 2016, 45, 26–34. [Google Scholar] [CrossRef]
- Lin, C.H.; Chin, W.C.; Huang, Y.S.; Chen, Y.R.; Tan, P.W.; Chen, J.Y.; Yu, N.W.; Wang, C.H.; Chou, P.Y. Short-term and long-term psychological impact and quality of life of patients undergoing orthognathic surgery. Biomed. J. 2022, 45, 549–556. [Google Scholar] [CrossRef]
- Lancaster, L.; Salaita, R.D.; Swamy, C.; Shanker, S.; Kennedy, K.S.; Beck, F.M.; Johnston, W.M.; Firestone, A.R. Effects of orthognathic surgery on quality of life compared with nonsurgical controls in an American population. Am. J. Orthod. Dentofac. Orthop. 2020, 158, 555–563. [Google Scholar] [CrossRef]
- Basso, I.B.; Gonçalves, F.M.; Martins, A.A.; Schroder, A.G.D.; Taveira, K.V.M.; Stechman-Neto, J.; Santos, R.S.; Guariza-Filho, O.; de Araujo, C.M. Psychosocial changes in patients submitted to orthodontic surgery treatment: A systematic review and meta-analysis. Clin. Oral Investig. 2021, 26, 2237–2251. [Google Scholar] [CrossRef]
- Lins, L.; Carvalho, F.M. SF-36 total score as a single measure of health-related quality of life: Scoping review. SAGE Open Med. 2016, 4, 2050312116671725. [Google Scholar] [CrossRef] [PubMed]
- Johnson, S.U.; Ulvenes, P.G.; Øktedalen, T.; Hoffart, A. Psychometric Properties of the General Anxiety Disorder 7-Item (GAD-7) Scale in a Heterogeneous Psychiatric Sample. Front. Psychol. 2019, 10, 1713. [Google Scholar] [CrossRef] [PubMed]
- Levis, B.; Benedetti, A.; Thombs, B.D.; DEPRESsion Screening Data (DEPRESSD) Collaboration. Accuracy of Patient Health Questionnaire-9 (PHQ-9) for screening to detect major depression: Individual participant data meta-analysis. BMJ 2019, 365, l1476, Erratum in: BMJ 2019, 365, l1781. [Google Scholar] [CrossRef] [PubMed]
- Halamová, J.; Kanovský, M.; Krizova, K.; Greškovičová, K.; Strnádelová, B.; Baránková, M. The Factor Structure and External Validity of the COPE 60 Inventory in Slovak Translation. Front. Psychol. 2022, 12, 800166. [Google Scholar] [CrossRef] [PubMed]
- Bahrami, F.; Yousefi, N. Females Are More Anxious Than Males: A Metacognitive Perspective. Iran. J. Psychiatry Behav Sci. 2011, 5, 83–90. [Google Scholar]
- Hasan, E.M.; Calma, C.L.; Tudor, A.; Vernic, C.; Palade, E.; Tudorache, E.; Oancea, C.; Papava, I. Gender Differences in Coping, Depression, and Anxiety in Patients with Non-Metastatic Lung Cancer. Cancer Manag. Res. 2022, 14, 2041–2052. [Google Scholar] [CrossRef]
- Ataro, Z.; Mengesha, M.M.; Abrham, A.; Digaffe, T. Gender Differences in Perceived Stigma and Coping Strategies Among People Living with HIV/AIDS at Jugal Hospital, Harar, Ethiopia. Psychol. Res. Behav. Manag. 2020, 13, 1191–1200. [Google Scholar] [CrossRef]
- Chudzicka-Czupała, A.; Hapon, N.; Man, R.H.C.; Li, D.-J.; Żywiołek-Szeja, M.; Karamushka, L.; Grabowski, D.; Paliga, M.; McIntyre, R.S.; Chiang, S.-K.; et al. Associations between coping strategies and psychological distress among people living in Ukraine, Poland, and Taiwan during the initial stage of the 2022 War in Ukraine. Eur. J. Psychotraumatol. 2023, 14, 2163129. [Google Scholar] [CrossRef]
- Holahan, C.J.; Moos, R.H.; Holahan, C.K.; Brennan, P.L.; Schutte, K.K. Stress Generation, Avoidance Coping, and Depressive Symptoms: A 10-Year Model. J. Consult. Clin. Psychol. 2005, 73, 658–666. [Google Scholar] [CrossRef]
- Kok, X.L.F.; Gwilliam, J.; Sayers, M.; Jones, E.M.; Cunningham, S.J. A Cross-Sectional Study of Factors Influencing Pre-Operative Anxiety in Orthognathic Patients. J. Clin. Med. 2023, 12, 5305. [Google Scholar] [CrossRef]
- Campbell-Sills, L.; Forde, D.R.; Stein, M.B. Demographic and childhood environmental predictors of resilience in a community sample. J. Psychiatr. Res. 2009, 43, 1007–1012. [Google Scholar] [CrossRef] [PubMed]
- Helmreich, I.; Kunzler, A.; Chmitorz, A.; König, J.; Binder, H.; Wessa, M.; Lieb, K. Psychological interventions for resilience enhancement in adults. Cochrane Database Syst. Rev. 2017, 2017, CD012527. [Google Scholar] [CrossRef]
- de Groot, K.I.; Boeke, S.; van den Berge, H.J.; Duivenvoorden, H.J.; Bonke, B.; Passchier, J. The influence of psychological variables on postoperative anxiety and physical complaints in patients undergoing lumbar surgery. Pain 1997, 69, 19–25. [Google Scholar] [CrossRef] [PubMed]
- Kain, Z.N.; Sevarino, F.; Alexander, G.M.; Pincus, S.; Mayes, L.C. Preoperative anxiety and postoperative pain in women undergoing hysterectomy. A repeated-measures design. J. Psychosom. Res. 2000, 49, 417–422. [Google Scholar] [CrossRef]
- Marselle, M.R.; Warber, S.L.; Irvine, K.N. Growing Resilience through Interaction with Nature: Can Group Walks in Nature Buffer the Effects of Stressful Life Events on Mental Health? Int. J. Environ. Res. Public Health 2019, 16, 986. [Google Scholar] [CrossRef]
- McRae, K.; Ochsner, K.N.; Mauss, I.B.; Gabrieli, J.J.D.; Gross, J.J. Gender Differences in Emotion Regulation: An fMRI Study of Cognitive Reappraisal. Group Process. Intergroup Relat. 2008, 11, 143–162. [Google Scholar] [CrossRef]
| Variables | Men (n = 68) | Women (n = 59) | p-Value * |
|---|---|---|---|
| Age, years (mean ± SD) ** | 32.8 ± 12.5 | 33.5 ± 14.1 | 0.767 |
| Obesity (n, %) | 14 (20.6%) | 12 (20.3%) | 0.972 |
| Currently smoking | 15 (22.1%) | 7 (11.9%) | 0.130 |
| Alcohol use (occasionally) | 23 (33.8%) | 18 (30.5%) | 0.690 |
| Place of origin (urban) | 38 (55.9%) | 36 (61.0%) | 0.558 |
| Education | |||
| High school | 21 (30.9%) | 19 (32.2%) | 0.880 |
| College | 24 (35.3%) | 22 (37.3%) | 0.815 |
| University | 23 (33.8%) | 18 (30.5%) | 0.724 |
| CCI > 2 | 6 (8.8%) | 4 (6.8%) | 0.669 |
| Relationship status (single) | 25 (36.8%) | 29 (49.2%) | 0.159 |
| Unemployed (n, %) | 11 (16.2%) | 8 (13.6%) | 0.683 |
| Malocclusion type | 0.706 | ||
| I | 10 (14.7%) | 11 (18.6%) | |
| II | 33 (48.5%) | 30 (50.8%) | |
| III | 25 (36.8%) | 18 (30.5%) | |
| Surgery type | 0.651 | ||
| Single jaw | 35 (51.5%) | 28 (47.5%) | |
| Bimaxillary | 33 (48.5%) | 31 (52.5%) |
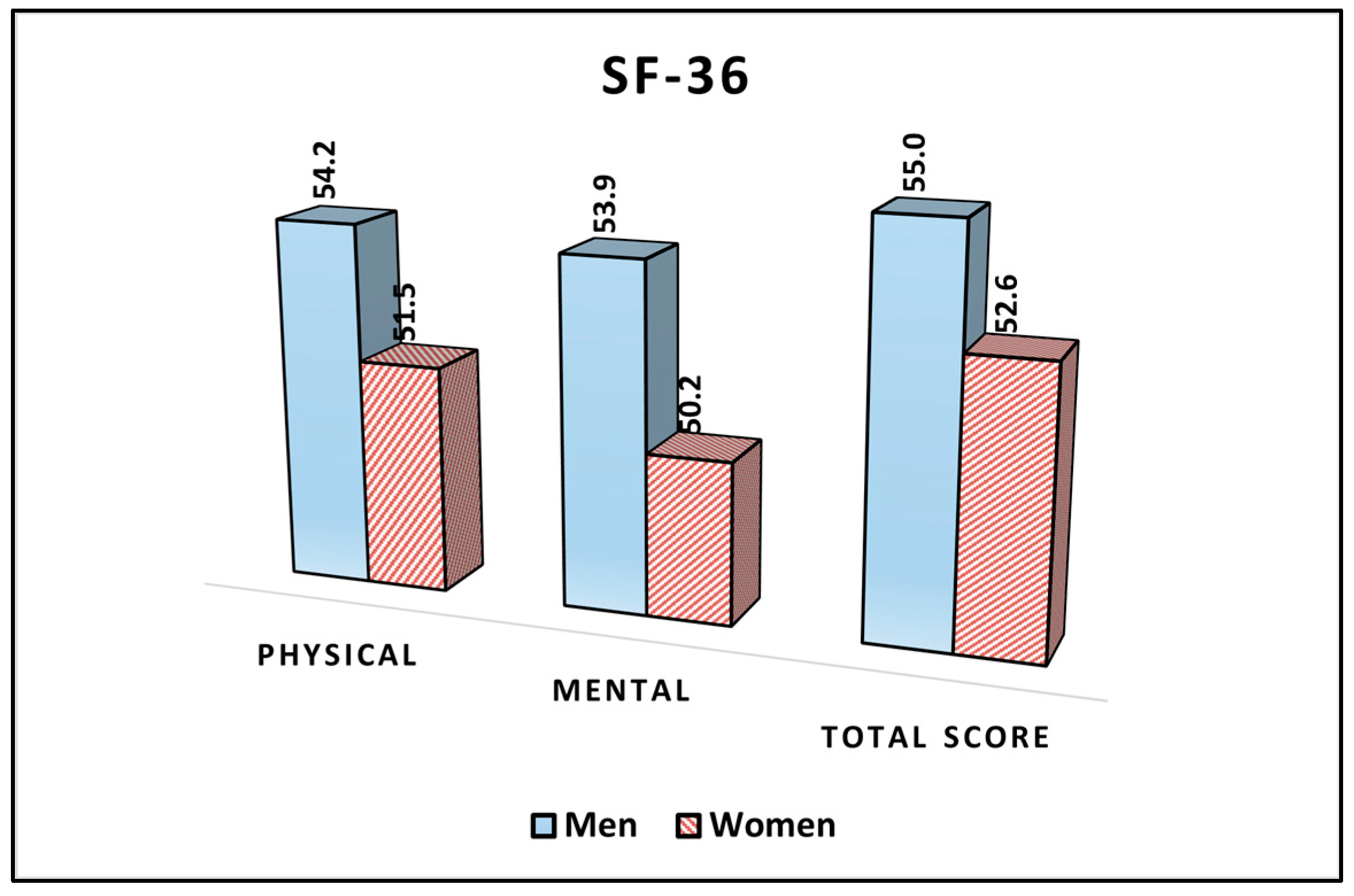
| SF-36 (Mean ± SD) | Men (n = 68) | Women (n = 59) | p-Value * |
|---|---|---|---|
| Physical | 54.2 ± 7.0 | 51.5 ± 8.3 | 0.049 |
| Mental | 53.9 ± 6.6 | 50.2 ± 6.9 | 0.003 |
| Total score | 55.0 ± 8.1 | 52.6 ± 7.3 | 0.083 |
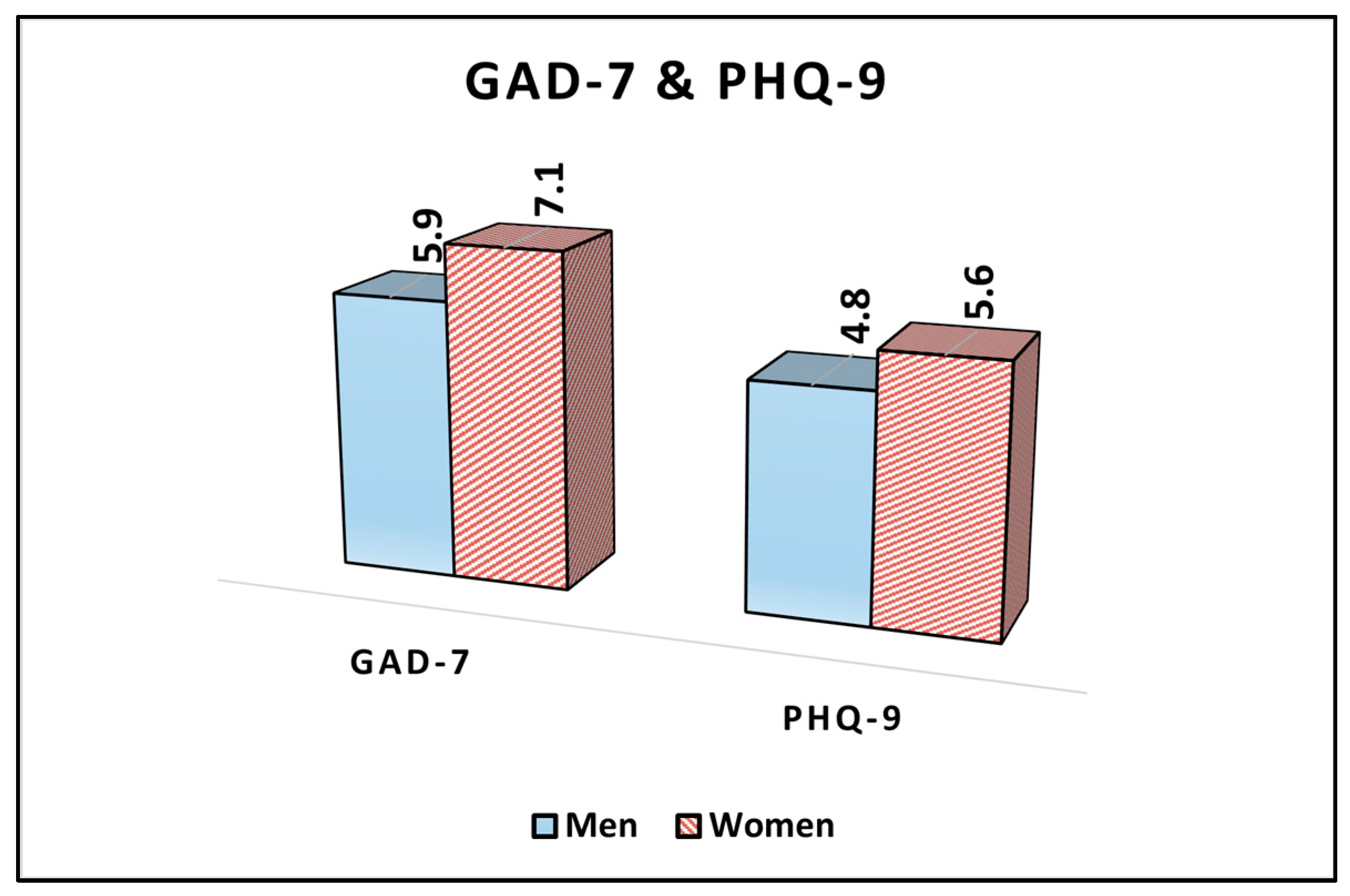
| Variables (Mean ± SD) | Men (n = 68) | Women (n = 59) | p-Value * |
|---|---|---|---|
| GAD-7 | 5.9 ± 3.3 | 7.1 ± 3.1 | 0.037 |
| PHQ-9 | 4.8 ± 2.5 | 5.6 ± 2.8 | 0.091 |
| Variables (% of Scores above Median) | Men (n = 68) | Women (n = 59) | p-Value * |
|---|---|---|---|
| Disengagement | 42 (61.8%) | 26 (44.1%) | 0.046 |
| Engagement | 18 (26.5%) | 30 (50.8%) | 0.004 |
| Emotion Focused | 16 (23.5%) | 35 (59.3%) | <0.001 |
| Problem Focused | 24 (35.3%) | 17 (28.8%) | 0.435 |
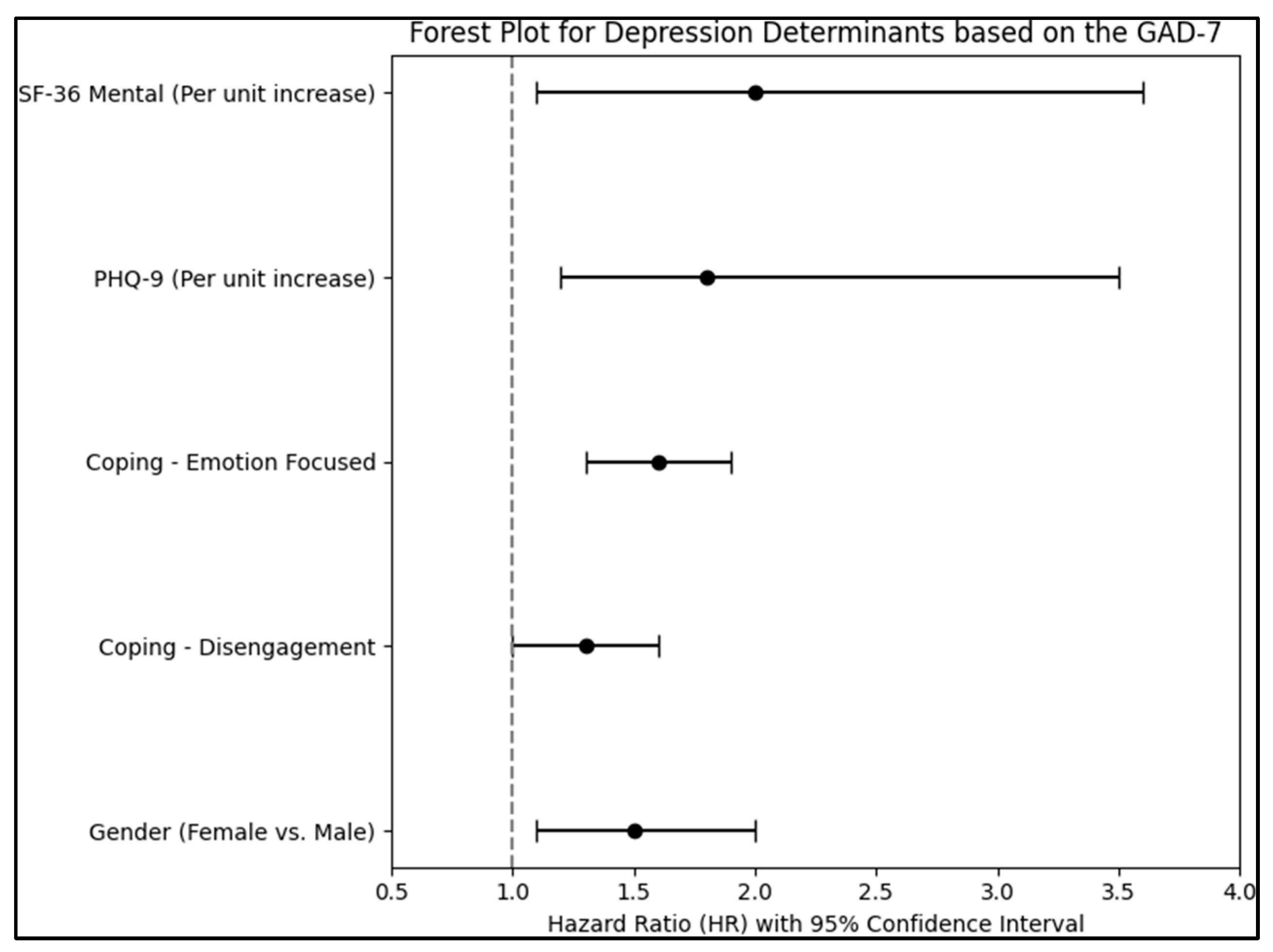
| Independent Variables | HR–Exp(B) | 95% CI | p-Value |
|---|---|---|---|
| Sex (Female vs. Male) | 1.5 | 1.1–2.0 | 0.014 |
| Age (Per year increase) | 1.02 | 0.97–1.19 | 0.132 |
| Coping–Disengagement | 1.3 | 1.0–1.6 | 0.049 |
| Coping–Emotion Focused | 1.6 | 1.3–1.9 | <0.001 |
| Coping–Problem Focused | 0.9 | 0.7–1.1 | 0.345 |
| Smoking (Yes vs. No) | 1.2 | 0.9–1.6 | 0.212 |
| Place of origin (Urban) | 1.1 | 0.8–1.4 | 0.621 |
| Relationship status (Single) | 1.3 | 1.0–1.7 | 0.056 |
| PHQ-9 (Per unit increase) | 1.8 | 1.2–3.5 | <0.001 |
| SF-36 Physical (Per unit increase) | 1.1 | 0.9–1.8 | 0.086 |
| SF-36 Mental (Per unit increase) | 2.0 | 1.1–3.6 | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Avramut, R.; Talpos, S.; Szuhanek, C.; Pricop, M.; Talpos, R.; Hajaj, T.; Nikolajevic-Stoican, N.; Maracineanu, R.; Ghircau-Radu, R.; Popa, M. Male and Female Discrepancies in Anxiety, Depressive Symptoms, and Coping Strategies among Orthognathic Patients: A Cross-Sectional Analysis. J. Clin. Med. 2023, 12, 7161. https://doi.org/10.3390/jcm12227161
Avramut R, Talpos S, Szuhanek C, Pricop M, Talpos R, Hajaj T, Nikolajevic-Stoican N, Maracineanu R, Ghircau-Radu R, Popa M. Male and Female Discrepancies in Anxiety, Depressive Symptoms, and Coping Strategies among Orthognathic Patients: A Cross-Sectional Analysis. Journal of Clinical Medicine. 2023; 12(22):7161. https://doi.org/10.3390/jcm12227161
Chicago/Turabian StyleAvramut, Robert, Serban Talpos, Camelia Szuhanek, Marius Pricop, Roxana Talpos, Tareq Hajaj, Nicoleta Nikolajevic-Stoican, Raluca Maracineanu, Roxana Ghircau-Radu, and Malina Popa. 2023. "Male and Female Discrepancies in Anxiety, Depressive Symptoms, and Coping Strategies among Orthognathic Patients: A Cross-Sectional Analysis" Journal of Clinical Medicine 12, no. 22: 7161. https://doi.org/10.3390/jcm12227161
APA StyleAvramut, R., Talpos, S., Szuhanek, C., Pricop, M., Talpos, R., Hajaj, T., Nikolajevic-Stoican, N., Maracineanu, R., Ghircau-Radu, R., & Popa, M. (2023). Male and Female Discrepancies in Anxiety, Depressive Symptoms, and Coping Strategies among Orthognathic Patients: A Cross-Sectional Analysis. Journal of Clinical Medicine, 12(22), 7161. https://doi.org/10.3390/jcm12227161






