Long-Term Assessment of Treatment Timing for Rapid Maxillary Expansion and Facemask Therapy Followed by Fixed Appliances: A Multicenter Retro-Prospective Study
Abstract
:1. Introduction
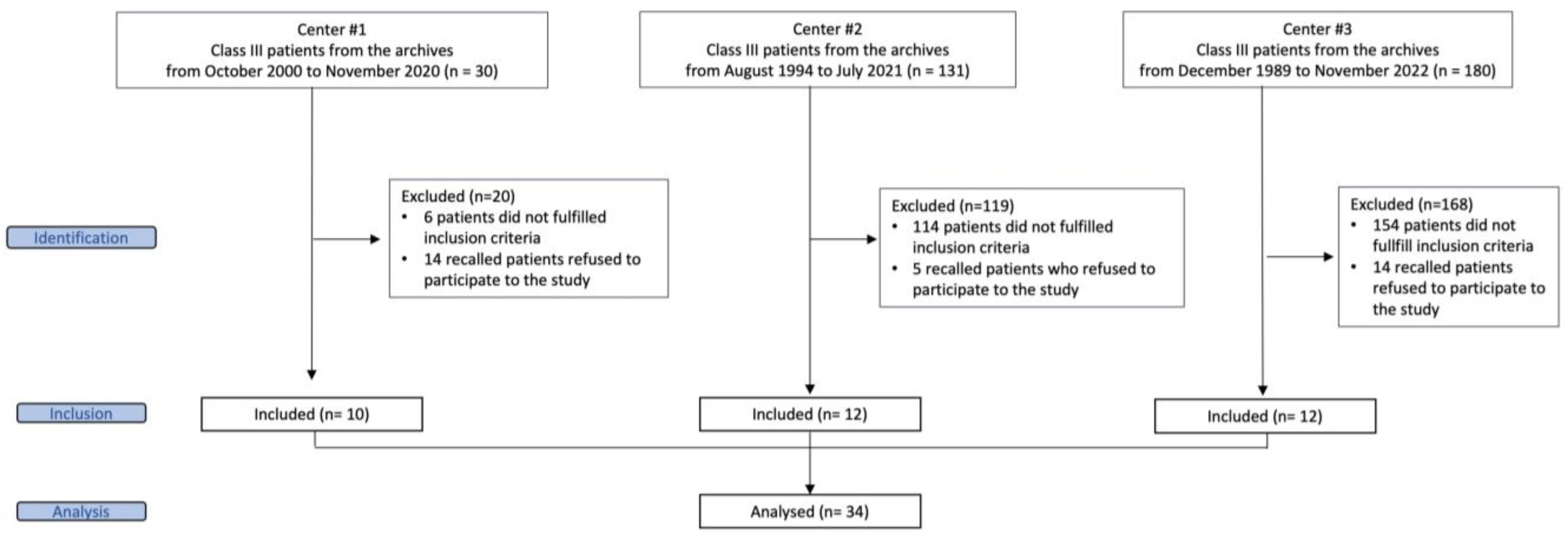
2. Materials and Methods
2.1. Study Design
2.2. Settings
2.3. Participants
- -
- Caucasian patients with Class III malocclusion who showed indications for treatment with RME/FM independently from the severity of the dento-skeletal disharmony;
- -
- Prepubertal-to-pubertal stage of maturation at the initiation of therapy (cervical vertebral maturation, CVM stages between CS1 and CS3) [22];
- -
- Availability of lateral cephalogram and panoramic radiograph before the RME/FM therapy (T0). Presence of a lateral cephalogram at a long-term follow up (T1) taken at least at 17 years of age for females and 20 years of age for males.
- -
- Patients affected by cleft lip and/or cleft palate;
- -
- Patients with craniofacial syndromes or disorders;
- -
- Patients with congenitally missing or supernumerary teeth;
- -
- For recalled patients, pregnant women were excluded.
2.4. Treatment Protocol
2.4.1. Center #1
2.4.2. Center #2
2.4.3. Center #3
2.5. Variables
2.6. Methods of Collecting Data
2.7. Method Error
2.8. Bias
2.9. Ethical Permission
2.10. Study Size
2.11. Statistical Methods
3. Results
3.1. Participants
3.2. Descriptive Data and Main Results
4. Discussion
4.1. Key Results and Interpretation
4.2. Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Woon, S.C.; Thiruvenkatachari, B. Early orthodontic treatment for Class III malocclusion: A systematic review and meta-analysis. Am. J. Orthod. Dentofac. Orthop. 2017, 151, 28–52. [Google Scholar] [CrossRef] [PubMed]
- Cordasco, G.; Matarese, G.; Rustico, L.; Fastuca, S.; Caprioglio, A.; Lindauer, S.J.; Nucera, R. Efficacy of orthopedic treatment with protraction facemask on skeletal Class III malocclusion: A systematic review and meta-analysis. Orthod. Craniofacial Res. 2014, 17, 133–143. [Google Scholar] [CrossRef] [PubMed]
- Lin, Y.; Guo, R.; Hou, L.; Fu, Z.; Li, W. Stability of maxillary protraction therapy in children with Class III malocclusion: A systematic review and meta-analysis. Clin. Oral Investig. 2018, 22, 2639–2652. [Google Scholar] [CrossRef] [PubMed]
- Kakali, L.; Christopoulou, I.; Tsolakis, I.A.; Sabaziotis, D.; Alexiou, A.; Sanoudos, M.; Tsolakis, A.I. Mid-term follow up effectiveness of facemask treatment in class III malocclusion: A systematic review. Int. Orthod. 2021, 19, 365–376. [Google Scholar] [CrossRef]
- Lee, W.C.; Shieh, Y.S.; Liao, Y.F.; Lee, C.H.; Huang, C.S. Long-term maxillary anteroposterior changes following maxillary protraction with or without expansion: A meta-analysis and meta-regression. PLoS ONE 2021, 16, e0247027. [Google Scholar] [CrossRef]
- Hägg, U.; Tse, A.; Bendeus, M.; Rabie, A.B. Long-term follow-up of early treatment with reverse headgear. Eur. J. Orthod. 2003, 25, 95–102. [Google Scholar] [CrossRef]
- Wells, A.P.; Sarver, D.M.; Proffit, W.R. Long-term efficacy of reverse pull headgear therapy. Angle Orthod. 2006, 76, 915–922. [Google Scholar] [CrossRef]
- Masucci, C.; Franchi, L.; Defraia, E.; Mucedero, M.; Cozza, P.; Baccetti, T. Stability of rapid maxillary expansion and facemask therapy: A long-term controlled study. Am. J. Orthod. Dentofac. Orthop. 2011, 140, 493–500. [Google Scholar] [CrossRef]
- Wendl, B.; Stampfl, M.; Muchitsch, A.P.; Droschl, H.; Winsauer, H.; Walter, A.; Wendl, M.; Wendl, T. Long-term skeletal and dental effects of facemask versus chincup treatment in Class III patients: A retrospective study. J. Orofac. Orthop. 2017, 78, 293–299. [Google Scholar] [CrossRef]
- Le, B.N.H.; Goonewardene, M.; Duigou, C.; Bharat, C. The long-term efficacy of rapid maxillary expansion and facemask therapy in Class III malocclusion. Australas. Orthod. J. 2020, 36, 27–37. [Google Scholar] [CrossRef]
- Gershater, E.; Li, C.; Ha, P.; Chung, C.H.; Tanna, N.; Zou, M.; Zheng, Z. Genes and Pathways Associated with Skeletal Sagittal Malocclusions: A Systematic Review. Int. J. Mol. Sci. 2021, 22, 13037. [Google Scholar] [CrossRef] [PubMed]
- Rutili, V.; Nieri, M.; Giuntini, V.; McNamara, J.A., Jr.; Franchi, L. A multilevel analysis of craniofacial growth in subjects with untreated Class III malocclusion. Orthod. Craniofacial Res. 2020, 23, 181–191. [Google Scholar] [CrossRef] [PubMed]
- Delaire, J. Maxillary development revisited: Relevance to the orthopaedic treatment of Class III malocclusions. Eur. J. Orthod. 1997, 19, 289–311. [Google Scholar] [CrossRef] [PubMed]
- Kapust, A.J.; Sinclair, P.M.; Turley, P.K. Cephalometric effects of face mask/expansion therapy in Class III children: A comparison of three age groups. Am. J. Orthod. Dentofac. Orthop. 1998, 113, 204–212. [Google Scholar] [CrossRef]
- Saadia, M.; Torres, E. Sagittal changes after maxillary protraction with expansion in Class III patients in the primary, mixed, and late mixed dentitions: A longitudinal retrospective study. Am. J. Orthod. Dentofac. Orthop. 2000, 117, 669–680. [Google Scholar] [CrossRef]
- Franchi, L.; Baccetti, T.; McNamara, J.A., Jr. Postpubertal assessment of treatment timing for maxillary expansion and protraction therapy followed by fixed appliances. Am. J. Orthod. Dentofac. Orthop. 2004, 126, 555–568. [Google Scholar] [CrossRef]
- Chen, L.; Chen, R.; Yang, Y.; Ji, G.; Shen, G. The effects of maxillary protraction and its long-term stability-a clinical trial in Chinese adolescents. Eur. J. Orthod. 2012, 34, 88–95. [Google Scholar] [CrossRef]
- Merwin, D.; Ngan, P.; Hagg, U.; Yiu, C.; Wei, S.H. Timing for effective application of anteriorly directed orthopedic force to the maxilla. Am. J. Orthod. Dentofac. Orthop. 1997, 112, 292–299. [Google Scholar] [CrossRef]
- Yüksel, S.; Uçem, T.T.; Keykubat, A. Early and late facemask therapy. Eur. J. Orthod. 2001, 23, 559–568. [Google Scholar] [CrossRef]
- Hwang, C.J.; Kyung, S.H.; Lim, J.K. Treatment effect of protraction headgear on skeletal Class III malocclusion. Korean J. Orthod. 1994, 24, 851–860. [Google Scholar]
- Cha, K.S. Skeletal changes of maxillary protraction in patients exhibiting skeletal class III malocclusion: A comparison of three skeletal maturation groups. Angle Orthod. 2003, 73, 26–35. [Google Scholar]
- McNamara, J.A., Jr.; Franchi, L. The cervical vertebral maturation method: A user’s guide. Angle Orthod. 2018, 88, 133–143. [Google Scholar] [CrossRef]
- Kim, H.; Kim, C.S.; Lee, J.M.; Lee, J.J.; Lee, J.; Kim, J.S.; Choi, S.H. Prediction of Fishman’s skeletal maturity indicators using artificial intelligence. Sci. Rep. 2023, 13, 5870. [Google Scholar] [CrossRef] [PubMed]
- Garib, D.; Lauris, R.C.; Calil, L.R.; Alves, A.C.; Janson, G.; De Almeida, A.M.; Cevidanes, L.H.; Lauris, J.R. Dentoskeletal outcomes of a rapid maxillary expander with differential opening in patients with bilateral cleft lip and palate: A prospective clinical trial. Am. J. Orthod. Dentofac. Orthop. 2016, 150, 564–574. [Google Scholar] [CrossRef]
- Majanni, A.M.; Hajeer, M.Y. The removable mandibular retractor vs the bone-anchored intermaxillary traction in the correction of skeletal Class III malocclusion in children: A randomized controlled trial. J. Contemp. Dent. Pract. 2016, 17, 361–371. [Google Scholar] [PubMed]
- dos Santos, B.M.; Stuani, A.S.; Stuani, A.S.; Faria, G.; Quintão, C.C.; Stuani, M.B. Soft tissue profile changes after rapid maxillary expansion with a bonded expander. Eur. J. Orthod. 2012, 34, 367–373. [Google Scholar] [CrossRef]
- Paddenberg, E.; Proff, P.; Kirschneck, C. Floating norms for individualising the ANB angle and the WITS appraisal in orthodontic cephalometric analysis based on guiding variables. J. Orofac. Orthop. 2023, 84, 10–18. [Google Scholar] [CrossRef] [PubMed]
- Souki, B.Q.; Nieri, M.; Pavoni, C.; Pavan Barros, H.M.; Junqueira Pereira, T.; Giuntini, V.; Cozza, P.; Franchi, L. Development and validation of a prediction model for long-term unsuccess of early treatment of Class III malocclusion. Eur. J. Orthod. 2020, 42, 200–205. [Google Scholar] [CrossRef]
- Koo, T.K.; Li, M.Y. A Guideline of selecting and reporting intraclass correlation coefficients for reliability research. J. Chiropr. Med. 2016, 15, 155–163. [Google Scholar] [CrossRef]
- Ngan, P. Early treatment of Class III malocclusion: Is it worth the burden? Am. J. Orthod. Dentofac. Orthop. 2006, 129, S82–S85. [Google Scholar] [CrossRef]
- Melsen, B.; Melsen, F. The postnatal development of the palatomaxillary region studied on human autopsy material. Am. J. Orthod. 1982, 82, 329–342. [Google Scholar] [CrossRef] [PubMed]


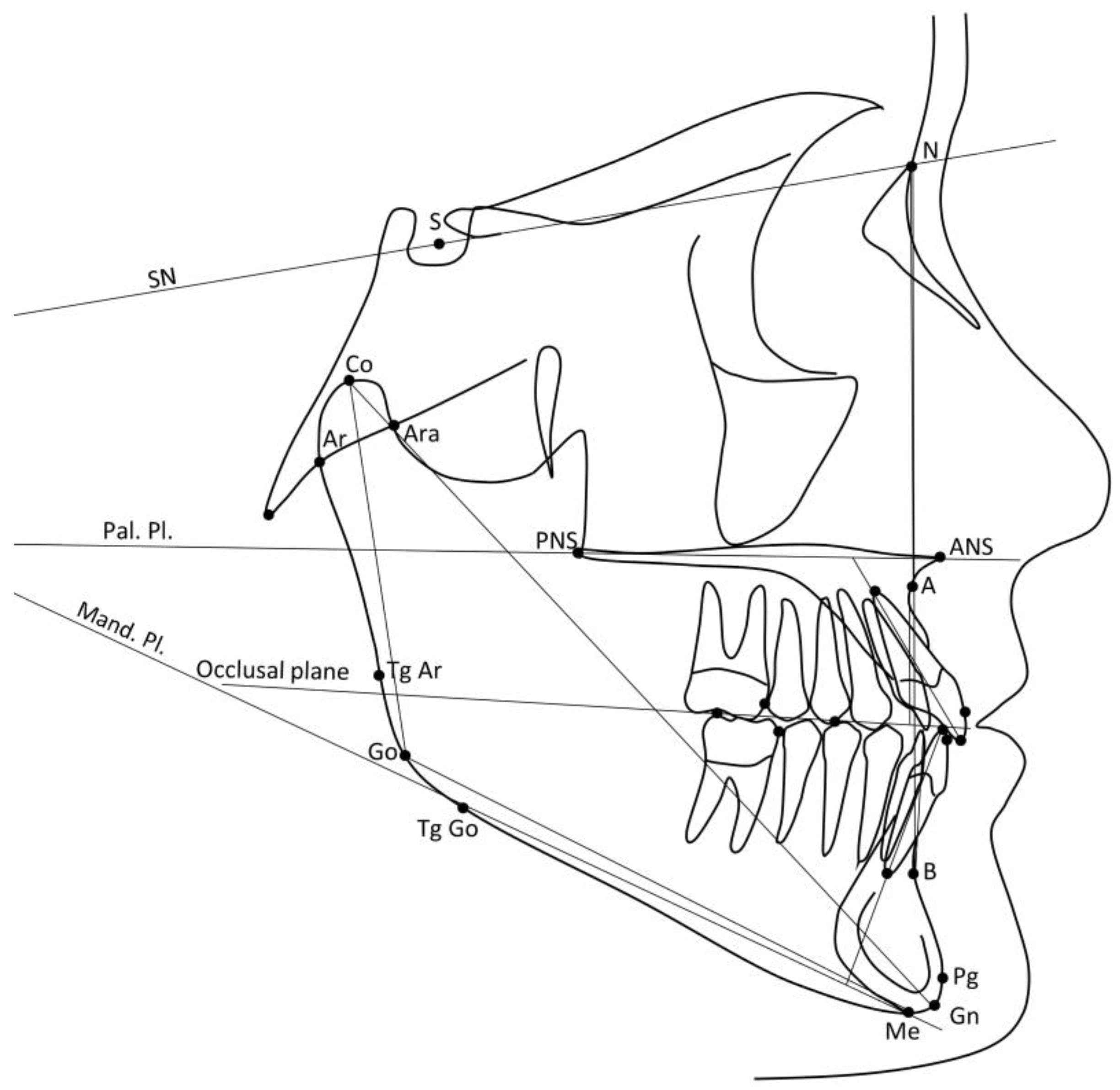
| Variable | Definition |
|---|---|
| NSBa° | Cranial base angle Nasion–Sella–Basion |
| SNA° | Angle between the SN line and A point |
| SNB° | Angle between the SN line and B point |
| ANB° | Angle between the A point, Nasion, and B point |
| Wits mm | Linear distance between the perpendicular projections of point A and point B on the occlusal plane |
| SN-Pal. Pl.° | Angle between the SN line and palatal plane (plane passing through the ANS and PNS points) |
| SN-Mand. Pl.° | Angle between the SN line and the mandibular plane (passing through the Menton point and tangent to the lower border of the mandibular corpus in the gonial region) |
| Pal. Pl.-Mand. Pl.° | Angle between the palatal plane and mandibular plane |
| Co-Gn mm | Total mandibular length |
| CoGoMe° | Mandibular angle |
| OVJ mm | Horizontal distance measured from the incisal margin of the upper central incisor to the incisal third of the lower central incisor |
| OVB mm | Vertical distance between the incisal edges of the upper and lower central incisors |
| Mol. Rel. mm | The distance between the mesial contact heights of contour on the maxillary and mandibular first molars, measured along the occlusal plane. |
| Upper Inc.-Pal. Pl° | Angle between the long axis of the upper central incisor and the palatal plane |
| Lower Inc. Mand. Pl.° | Angle between the long axis of the lower central incisor and the mandibular plane |
| EPG N = 17 (SD) | LPG N = 17 (SD) | Diff. | 95% CI | p Value (t-Test) | |
|---|---|---|---|---|---|
| Age (years) | 5.8 (0.7) Range 4.3–6.9 | 10.1 (0.8) Range 9.0–11.1 | 4.3 | 3.7; 4.3 | <0.001 |
| Females | 14 (82%) | 8 (47%) | 0.071 (FET) | ||
| CVM≥ 3 | 0 (0%) | 1 (6%) | 0.999 (FET) | ||
| NSBa° | 131.3 (6.0) | 132.1 (5.5) | 0.7 | −3.3; 4.8 | 0.711 |
| SNA° | 78.7 (3.6) | 78.8 (2.7) | 0.2 | −2.1; 2.4 | 0.885 |
| SNB° | 77.9 (3.2) | 77.8 (2.7) | −0.2 | −2.2; 1.9 | 0.881 |
| ANB° | 0.8 (1.9) | 1.1 (1.7) | 0.3 | −1.0; 1.6 | 0.612 |
| Wits mm | −4.6 (4.0) | −4.8 (2.4) | −0.3 | −2.6; 2.0 | 0.815 |
| SN-Pal. Pl.° | 9.0 (3.3) | 9.5 (2.4) | 0.5 | −1.5; 2.5 | 0.581 |
| SN-Mand. Pl.° | 36.1 (4.7) | 37.1 (3.5) | 1.0 | −1.9; 3.9 | 0.486 |
| Pal. Pl.-Mand. Pl.° | 27.1 (5.2) | 27.6 (3.2) | 0.5 | −2.5; 3.5 | 0.476 |
| Co-Gn mm | 91.6 (4.2) | 102.8 (4.5) | 11.3 | 8.2; 14.3 | <0.001 |
| CoGoMe° | 128.3 (5.1) | 128.2 (4.0) | −0.1 | −3.3; 3.1 | 0.938 |
| OVJ mm | −2.6 (2.0) | 0.2 (1.8) | 2.7 | 1.4; 4.0 | <0.001 |
| OVB mm | 0.6 (2.1) | 0.9 (1.4) | 0.4 | −0.9; 1.6 | 0.565 |
| Mol. Rel. mm | 2.8 (2.3) | 2.2 (1.2) | −0.6 | −1.9; 0.7 | 0.338 |
| Upper Inc.-Pal. Pl° | 96.6 (5.5) | 111.3 (7.0) | 14.7 | −10.3; 19.1 | <0.001 |
| Lower Inc.-Mand. Pl.° | 83.4 (9.1) | 87.3 (5.5) | 3.9 | −1.4; 9.1 | 0.145 |
| EPG N = 17 (SD) | LPG N = 17 (SD) | Diff. | 95% CI | p Value (t-Test) | |
|---|---|---|---|---|---|
| Age (years) | 19.8 (1.0) Range 18.4–21.7 | 21.0 (2.1) Range 17.1–24.4 | 1.2 | 0.1; 2.4 | 0.037 |
| Unsuccessful | 3 (18%) | 5 (29%) | 1.94 (Odds ratio) | 0.38; 9.88 | 0.688 |
| NSBa° | 131.2 (7.6) | 131.5 (6.1) | 0.3 | −4.5; 5.1 | 0.902 |
| SNA° | 80.5 (3.4) | 80.2 (3.0) | −0.3 | −2.5; 2.0 | 0.798 |
| SNB° | 79.4 (4.5) | 79.4 (3.4) | 0.0 | −2.8; 2.8 | 1.0 |
| ANB° | 1.1 (3.2) | 0.8 (2.9) | −0.3 | −2.4; 1.9 | 0.803 |
| Wits mm | −3.7 (3.7) | −4.2 (2.6) | −0.6 | −2.8; 1.7 | 0.616 |
| SN-Pal. Pl.° | 8.8 (3.9) | 9.8 (2.6) | 1.0 | −1.3; 3.3 | 0.388 |
| SN-Mand. Pl.° | 32.8 (7.0) | 35.0 (5.3) | 2.2 | −2.1; 6.5 | 0.303 |
| Pal. Pl.-Mand. Pl.° | 24.0 (6.8) | 25.2 (4.8) | 1.2 | −2.9; 5.4 | 0.550 |
| Co-Gn mm | 115.7 (7.9) | 117.5 (6.3) | 1.8 | −3.2; 6.8 | 0.464 |
| CoGoMe° | 122.7 (5.8) | 125.0 (5.8) | 2.3 | −1.8; 6.3 | 0.264 |
| OVJ mm | 1.8 (1.5) | 1.1 (2.6) | −0.7 | −2.2; 0.8 | 0.348 |
| OVB mm | 1.5 (1.3) | 1.3 (1.7) | −0.2 | −1.2; 0.9 | 0.747 |
| Mol. Rel. mm | 2.2 (1.9) | 3.2 (2.6) | 1.0 | −0.6; 2.5 | 0.220 |
| Upper Inc.-Pal. Pl.° | 116.4 (6.2) | 116.8 (4.7) | 0.4 | −3.4; 4.3 | 0.826 |
| Lower Inc.-Mand. Pl.° | 91.0 (9.7) | 90.2 (7.6) | −0.8 | −6.9; 5.3 | 0.784 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rutili, V.; Quiroga Souki, B.; Nieri, M.; Farnese Morais Carlos, A.L.; Pavoni, C.; Cozza, P.; McNamara, J.A., Jr.; Giuntini, V.; Franchi, L. Long-Term Assessment of Treatment Timing for Rapid Maxillary Expansion and Facemask Therapy Followed by Fixed Appliances: A Multicenter Retro-Prospective Study. J. Clin. Med. 2023, 12, 6930. https://doi.org/10.3390/jcm12216930
Rutili V, Quiroga Souki B, Nieri M, Farnese Morais Carlos AL, Pavoni C, Cozza P, McNamara JA Jr., Giuntini V, Franchi L. Long-Term Assessment of Treatment Timing for Rapid Maxillary Expansion and Facemask Therapy Followed by Fixed Appliances: A Multicenter Retro-Prospective Study. Journal of Clinical Medicine. 2023; 12(21):6930. https://doi.org/10.3390/jcm12216930
Chicago/Turabian StyleRutili, Valentina, Bernardo Quiroga Souki, Michele Nieri, Ana Luiza Farnese Morais Carlos, Chiara Pavoni, Paola Cozza, James A. McNamara, Jr., Veronica Giuntini, and Lorenzo Franchi. 2023. "Long-Term Assessment of Treatment Timing for Rapid Maxillary Expansion and Facemask Therapy Followed by Fixed Appliances: A Multicenter Retro-Prospective Study" Journal of Clinical Medicine 12, no. 21: 6930. https://doi.org/10.3390/jcm12216930
APA StyleRutili, V., Quiroga Souki, B., Nieri, M., Farnese Morais Carlos, A. L., Pavoni, C., Cozza, P., McNamara, J. A., Jr., Giuntini, V., & Franchi, L. (2023). Long-Term Assessment of Treatment Timing for Rapid Maxillary Expansion and Facemask Therapy Followed by Fixed Appliances: A Multicenter Retro-Prospective Study. Journal of Clinical Medicine, 12(21), 6930. https://doi.org/10.3390/jcm12216930








