Emotional Distress Caused by the Measures Taken in Assisted Reproductive Treatments during the COVID-19 Confinement in Spain
Abstract
:1. Introduction
2. Materials and Methods
2.1. Instruments
2.2. Ethical Considerations
2.3. Data Analysis Design
3. Results
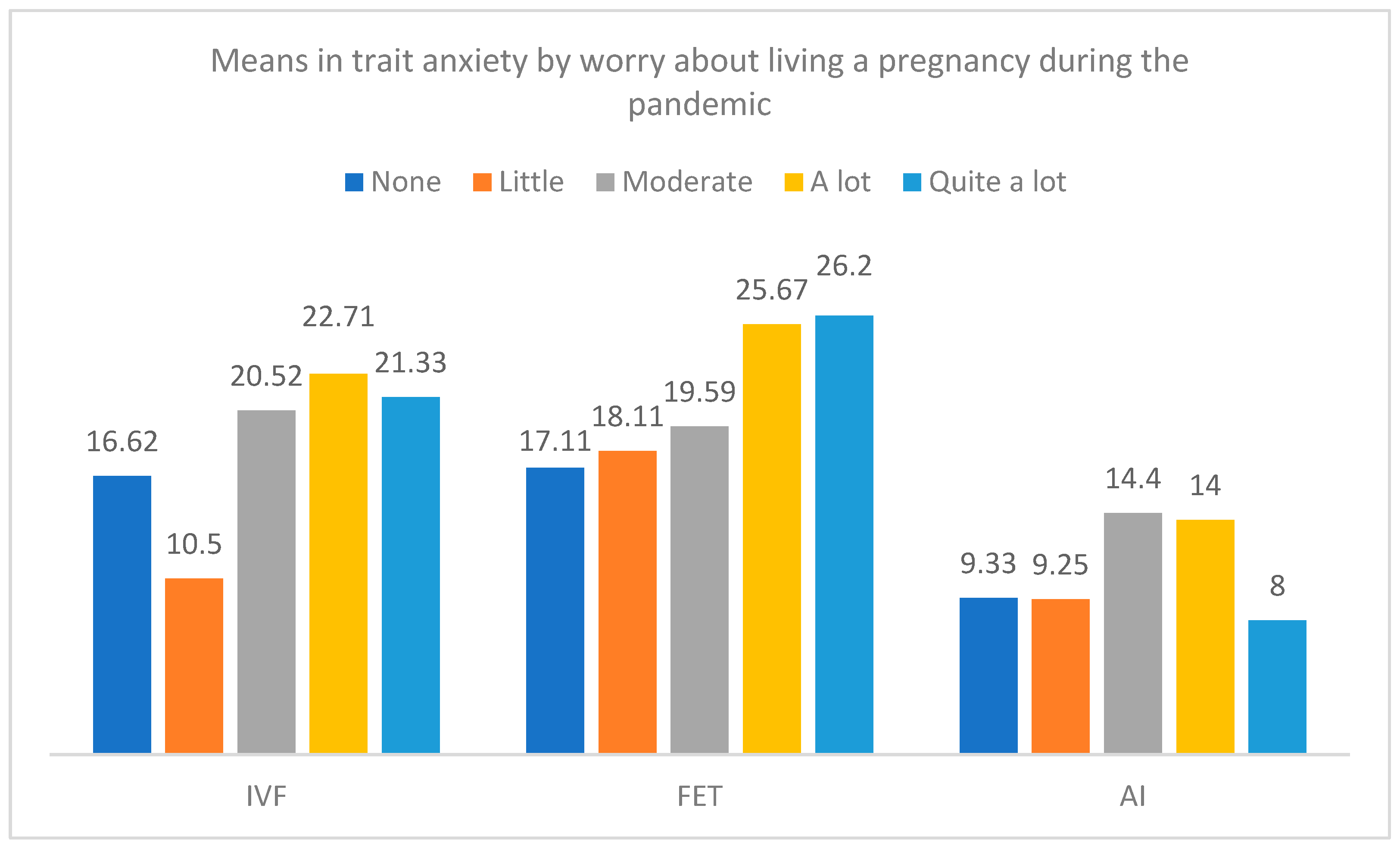
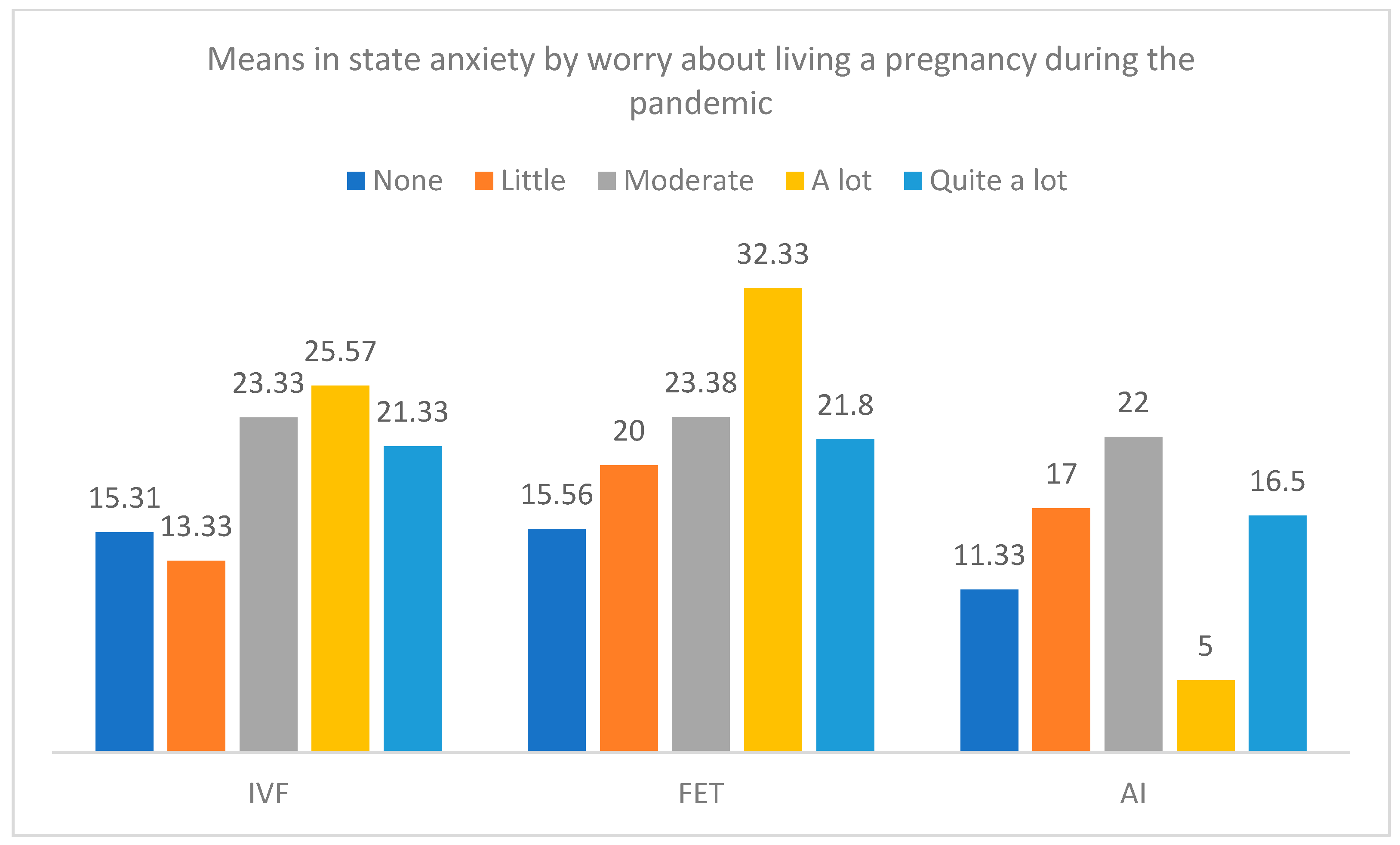
Multivariate Analyses
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- National Institute of Statistics. Fertilty Survey. 2018. Available online: https://www.ine.es/prensa/ef_2018_d.pdf (accessed on 1 August 2023).
- Zamora Pascual, E. Aplicación, Evaluación y Valoración de un Programa de Intervención. Psicológica en Parejas que Acuden a una Unidad de Reproducción Humana Asistida. Ph.D. Thesis, Universidad de La Laguna, Santa Cruz de Tenerife, Spain, 2016. [Google Scholar]
- Klonoff-Cohen, H.; Chu, E.; Natarajan, L.; Sieber, W. A prospective study of stress among women undergoing in vitro fertilization or gamete intrafallopian transfer. Fertil. Steril. 2001, 76, 675–687. [Google Scholar] [CrossRef] [PubMed]
- Slade, P.; O’Neill, C.; Simpson, A.J.; Lashen, H. The relationship between perceived stigma, disclosure patterns, support and distress in new attendees at an infertility clinic. Hum. Reprod. 2007, 22, 2309–2317. [Google Scholar] [CrossRef] [PubMed]
- Gordon, J.L.; Balsom, A.A. The psychological impact of fertility treatment suspensions during the COVID-19 pandemic. PLoS ONE 2020, 15, e0239253. [Google Scholar] [CrossRef]
- Esposito, V.; Rania, E.; Lico, D.; Pedri, S.; Fiorenza, A.; Strati, M.F.; Conforti, A.; Marrone, V.; Carosso, A.; Revelli, A.; et al. Influence of COVID-19 pandemic on the psychological status of infertile couples. Eur. J. Obstet. Gynecol. Reprod. Biol. 2020, 253, 148–153. [Google Scholar] [CrossRef]
- Legro, R. The COVID-19 pandemic and reproductive health. Fertil. Steril. 2021, 115, 811–812. [Google Scholar] [CrossRef] [PubMed]
- Lawson, A.K. Psychological stress and fertility. In Fertility and Assisted Reproductive Technology (ART): Theory, Research, Policy and Practice for Healthcare Practitioners, 7th ed.; Stevenson, E.L., Hershberger, P.E., Eds.; Springer: New York, NY, USA, 2016; pp. 65–86. [Google Scholar]
- Restubog, S.L.D.; Ocampo, A.C.G.; Wang, L. Taking control amidst the chaos: Emotion regulation during the COVID-19 pandemic. J. Vocat. Behav. 2020, 119, 103440. [Google Scholar] [CrossRef]
- Wang, C.; Pan, R.; Wan, X.; Tan, Y.; Xu, L.; Ho, C.S.; Ho, R.C. Immediate Psychological Responses and Associated Factors during the Initial Stage of the 2019 Coronavirus Disease (COVID-19) Epidemic among the General Population in China. Int. J. Environ. Res. Public Health 2020, 17, 1729. [Google Scholar] [CrossRef]
- Qu, P.; Zhao, D.; Jia, P.; Dang, S.; Shi, W.; Wang, M.; Shi, J. Changes in Mental Health of Women Undergoing Assisted Reproductive Technology Treatment During the COVID-19 Pandemic Outbreak in Xi’an, China. Front. Public Health 2021, 25, 645421. [Google Scholar] [CrossRef]
- Spieberger, C.D.; Gorsuch, R.L.; Lushene, R. Manual for the State-Trait Anxiety Inventory; Consulting Psychologists Press: Palo Alto, CA, USA, 1983. [Google Scholar]
- Muñiz Fernández, J.; Fernández Hermida, J.R. La opinión de los psicólogos españoles sobre el uso de los tests. Papeles Psicólogo Rev. Col. Of. Psicólogos 2010, 31, 108–121. [Google Scholar]
- Tokgoz, V.Y.; Kaya, Y.; Tekin, A.B. The level of anxiety in infertile women whose ART cycles are postponed due to the COVID-19 outbreak. J. Psychosom. Obstet. Gynaecol. 2022, 43, 114–121. [Google Scholar] [CrossRef]
- Lablanche, O.; Salle, B.; Perie, M.A.; Labrune, E.; Langlois-Jacques, C.; Fraison, E. Psychological effect of COVID-19 pandemic among women undergoing infertility care, a French cohort–PsyCovART Psychological effect of COVID-19: PsyCovART. J. Gynecol. Obstet. Hum. Reprod. 2022, 51, 102251. [Google Scholar] [CrossRef] [PubMed]
- Lawson, A.K.; McQueen, D.B.; Swanson, A.C.; Confino, R.; Feinberg, E.C.; Pavone, M.E. Psychological distress and postponed fertility care during the COVID-19 pandemic. J. Assist. Reprod. Genet. 2021, 38, 333–341. [Google Scholar] [CrossRef] [PubMed]
- Marom Haham, L.; Youngster, M.; Kuperman Shani, A.; Yee, S.; Ben-Kimhy, R.; Medina-Artom, T.R.; Hourvitz, A.; Kedem, A.; Librach, C. Suspension of fertility treatment during the COVID-19 pandemic: Views, emotional reactions and psychological distress among women undergoing fertility treatment. Reprod. Biomed. Online 2021, 42, 849–858. [Google Scholar] [CrossRef] [PubMed]
- Vaughan, D.A.; Shah, J.S.; Penzias, A.S.; Domar, A.D.; Toth, T.L. Infertility remains a top stressor despite the COVID-19 pandemic. Reprod. Biomed. Online 2020, 41, 425–427. [Google Scholar] [CrossRef] [PubMed]
- Turocy, J.M.; Robles, A.; Hercz, D.; D’Alton, M.; Forman, E.J.; Williams, Z. The emotional impact of the ASRM guidelines on fertility patients during the COVID-19 pandemic. Fertil. Steril. 2020, 114, e63. [Google Scholar] [CrossRef]
- Ben-Kimhy, R.; Youngster, M.; Medina-Artom, T.R.; Avraham, S.; Gat, I.; Haham, L.M.; Hourvitz, A.; Kedem, A. Fertility patients under COVID-19: Attitudes, perceptions and psychological reactions. Hum. Reprod. 2020, 35, 2774–2783. [Google Scholar] [CrossRef]
- Muhaidat, N.; Alshrouf, M.A.; Karam, A.M.; Elfalah, M. Infertility Management Disruption During the COVID-19 Outbreak in a Middle-Income Country: Patients’ Choices, Attitudes, and Concerns. Patient Prefer. Adherence 2021, 15, 2279–2288. [Google Scholar] [CrossRef]
- Cirillo, M.; Rizzello, F.; Badolato, L.; De Angelis, D.; Evangelisti, P.; Coccia, M.E.; Fatini, C. The effects of COVID-19 lockdown on lifestyle and emotional state in women undergoing assisted reproductive technology: Results of an Italian survey. J. Gynecol. Obstet. Hum. Reprod. 2021, 50, 102079. [Google Scholar] [CrossRef]
- Bernard, A.L.; Barbour, A.K.; Meernik, C.; Madeira, J.L.; Lindheim, S.R.; Goodman, L.R. The impact of an interactive multimedia educational platform on patient comprehension and anxiety during fertility treatment: A randomized controlled trial. FS Rep. 2022, 1, 214–222. [Google Scholar] [CrossRef]
- Martinelli, N.; Gil, S.; Belletier, C.; Chevalère, J.; Dezecache, G.; Huguet, P.; Droit-Volet, S. Time and emotion during lockdown and the COVID-19 epidemic: Determinants of our experience of time? Front. Psychol. 2021, 11, 616169. [Google Scholar] [CrossRef]
- Biviá-Roig, G.; Boldó-Roda, A.; Blasco-Sanz, R.; Serrano-Raya, L.; DelaFuente-Díez, E.; Múzquiz-Barberá, P.; Lisón, J.F. Impact of the COVID-19 pandemic on the lifestyles and quality of life of women with fertility problems: A cross-sectional study. Front. Public Health 2021, 19, 686115. [Google Scholar] [CrossRef] [PubMed]


| Anguish | Frustration | Sadness | Loneliness | ||
|---|---|---|---|---|---|
| What did you feel when you were told that you had to postpone your treatment? | 10.2 | 32.7 | 54.1 | 3.1 | |
| Relief | Tranquility | Relaxation | Acceptance | ||
| How did you experience it? | 5.2 | 26.1 | 3.5 | 65.2 | |
| None | Little | Moderate | A lot | Quite a lot | |
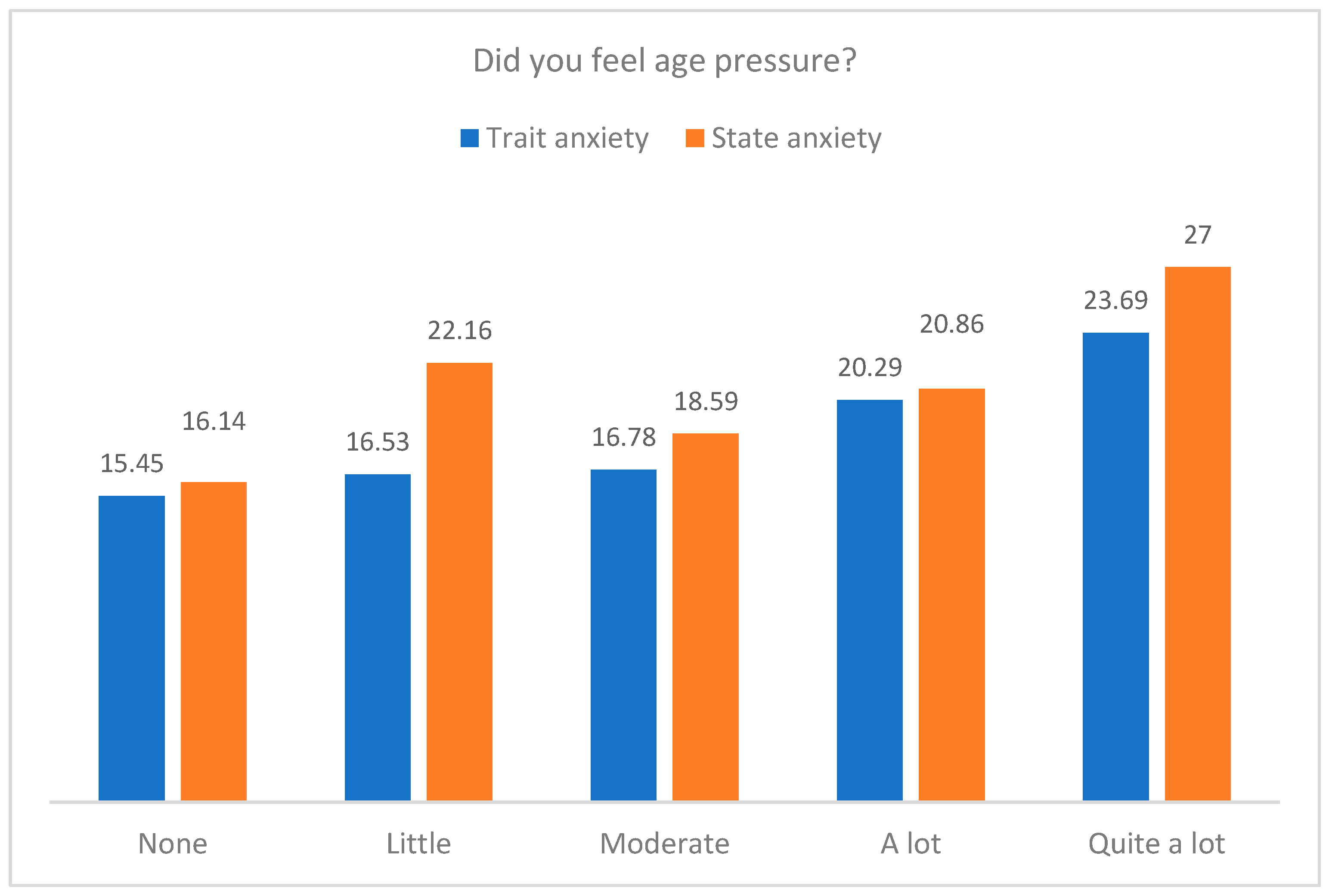
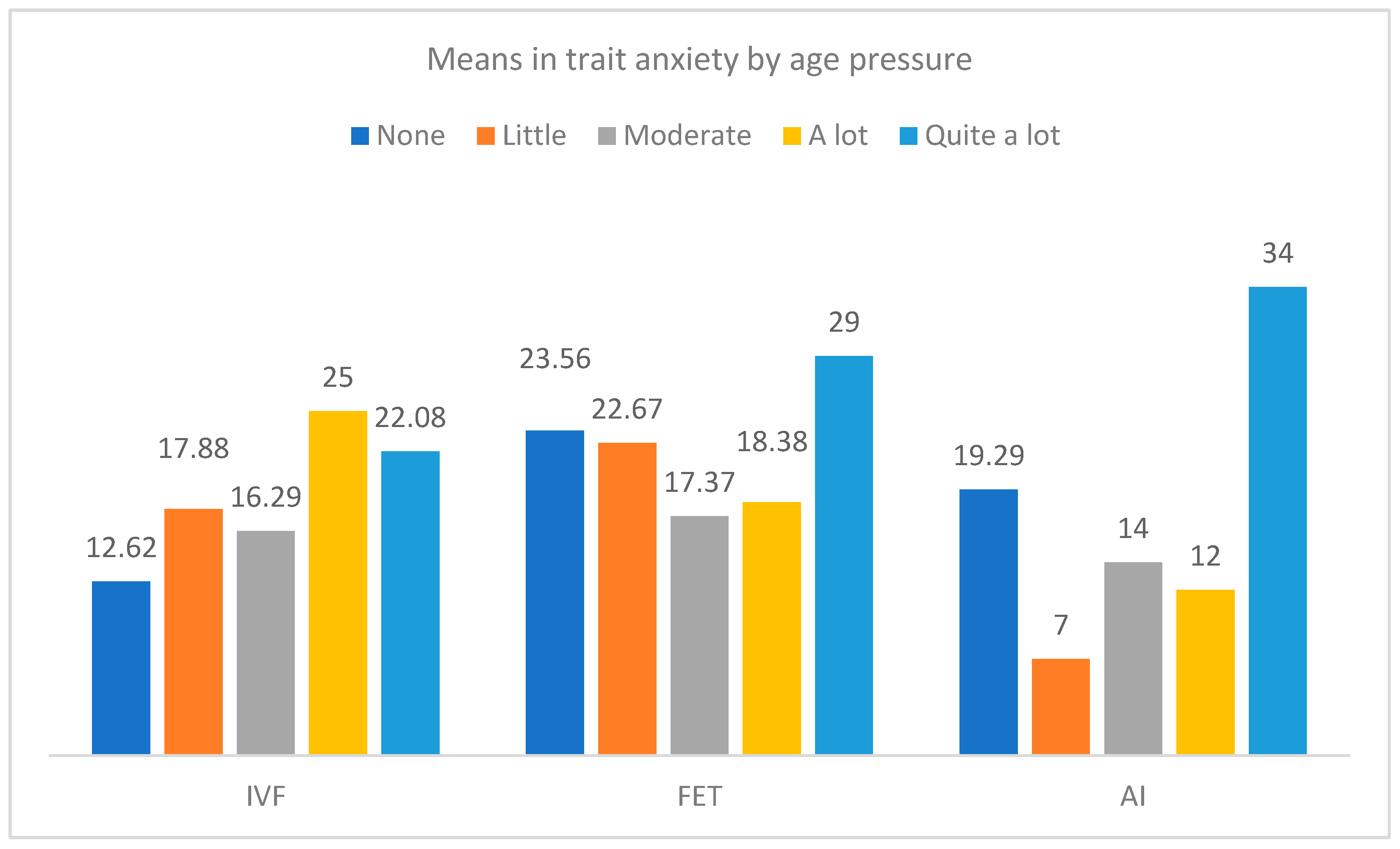
| Did you feel age pressure? | 25.2 | 16.5 | 32.2 | 12.2 | 13.9 |
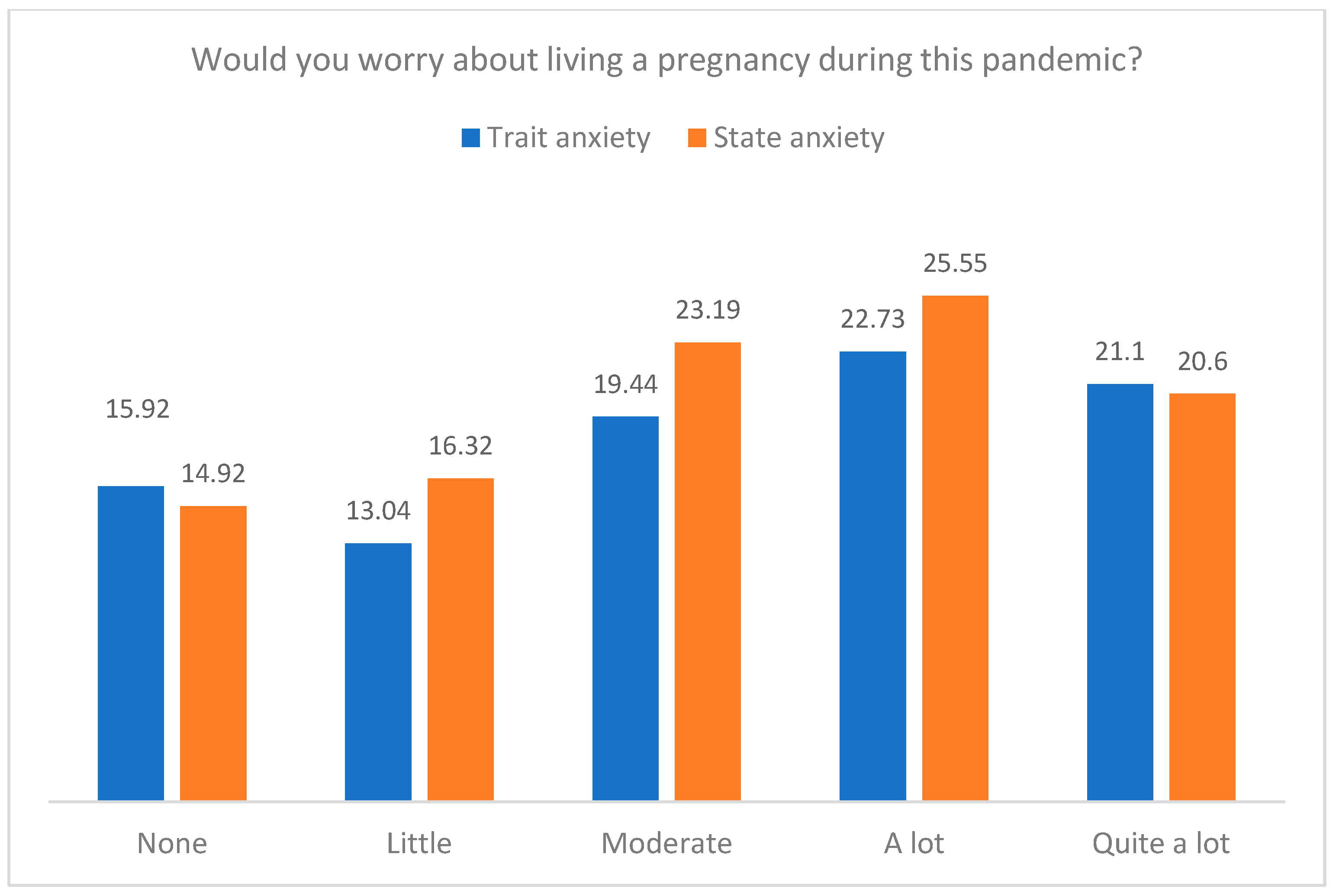
| Would you worry about pregnancy during this pandemic? | 21.9 | 21.9 | 37.7 | 9.6 | 8.8 |
| No matter what happens, I will continue. | I wonder if it is convenient to continue. | I take the good advice of professionals. | I abandon because it is a sign that I should not continue. | ||
| When a setback arises regarding your goal… | 13 | 11.3 | 75.7 | 0 | |
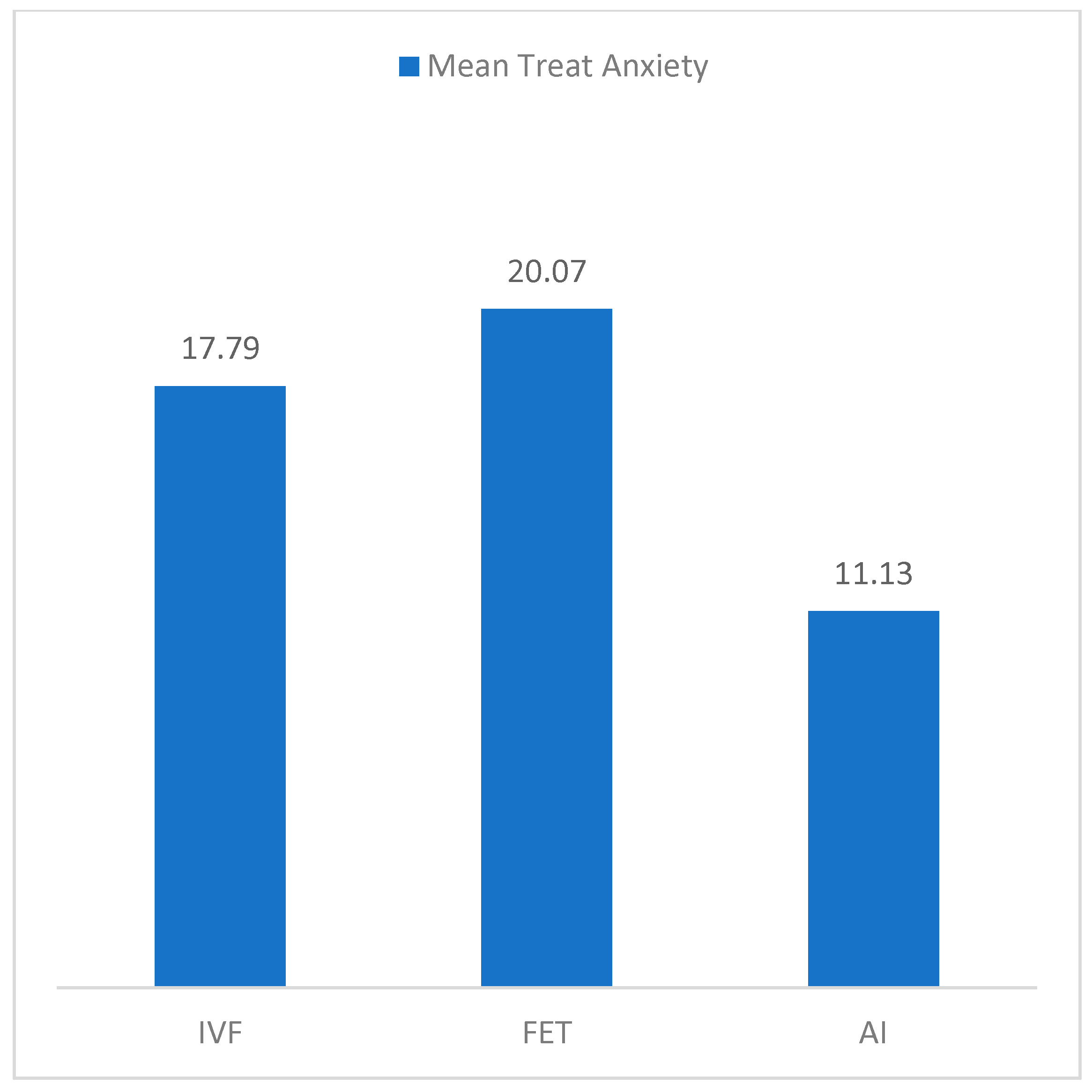
| Type of Treatment | n | Trait Anxiety Quantile | State Anxiety Quantile | ||
|---|---|---|---|---|---|
| IVF-ICSI | 56 | 41.27 | ±25.54 | 61.39 | ±18.53 |
| FET | 44 | 16.93 | ±17.05 | 19.91 | ±15.71 |
| AI | 15 | 37.73 | ±28.26 | 55.33 | ±11.10 |
| Total | 115 | 31.5 | ±25.62 | 44.73 | ±25.75 |
| Dependent Variable: State Anxiety | Dependent Variable: Trait Anxiety | |||||||
|---|---|---|---|---|---|---|---|---|
| F | R2 | t | β | F | R2 | t | β | |
| 4.51 *** | 0.24 | 4.07 ** | 0.21 | |||||
| Treatment | 0.98 | 0.10 | 0.71 | 0.97 | ||||
| Sterility time | −1.03 | −0.11 | −0.67 | −0.07 | ||||
| What did you feel when you were told that you had to postpone your treatment? | 0.72 | 0.07 | 0.84 | 0.09 | ||||
| How did you experience it? | −0.14 | −0.01 | −1.38 | −0.14 | ||||
| Did you feel age pressure? | 2.84 | 0.31 ** | 2.59 | 0.28 * | ||||
| Would you worry about pregnancy within this pandemic? | 3.04 | 0.32 ** | 3.08 | 0.33 ** | ||||
| When a setback arises in regard to your goal… | 1.91 | 0.20 | 1.48 | 0.16 | ||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Correa Rancel, M.; Sosa Comino, E.; Leon-Larios, F.; Suárez Hernández, Y.; Carballo Lorenzo, J.; Gomez-Baya, D.; Baez Quintana, D. Emotional Distress Caused by the Measures Taken in Assisted Reproductive Treatments during the COVID-19 Confinement in Spain. J. Clin. Med. 2023, 12, 7069. https://doi.org/10.3390/jcm12227069
Correa Rancel M, Sosa Comino E, Leon-Larios F, Suárez Hernández Y, Carballo Lorenzo J, Gomez-Baya D, Baez Quintana D. Emotional Distress Caused by the Measures Taken in Assisted Reproductive Treatments during the COVID-19 Confinement in Spain. Journal of Clinical Medicine. 2023; 12(22):7069. https://doi.org/10.3390/jcm12227069
Chicago/Turabian StyleCorrea Rancel, Marta, Elena Sosa Comino, Fatima Leon-Larios, Yaiza Suárez Hernández, Janet Carballo Lorenzo, Diego Gomez-Baya, and Delia Baez Quintana. 2023. "Emotional Distress Caused by the Measures Taken in Assisted Reproductive Treatments during the COVID-19 Confinement in Spain" Journal of Clinical Medicine 12, no. 22: 7069. https://doi.org/10.3390/jcm12227069
APA StyleCorrea Rancel, M., Sosa Comino, E., Leon-Larios, F., Suárez Hernández, Y., Carballo Lorenzo, J., Gomez-Baya, D., & Baez Quintana, D. (2023). Emotional Distress Caused by the Measures Taken in Assisted Reproductive Treatments during the COVID-19 Confinement in Spain. Journal of Clinical Medicine, 12(22), 7069. https://doi.org/10.3390/jcm12227069








