Diabetic Polyneuropathy and Physical Activity in Type 1 Diabetes Mellitus: A Cross-Sectional Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Case Selection
2.2. Protocol
- -
- Biometric parameters (weight, height, BMI);
- -
- Anthropometric parameters (age, gender);
- -
- Physiological anamnesis (smoking, alcohol);
- -
- Pathological history (duration of DM, presence of DM complications, hypertension);
- -
- Clinical data (glycated haemoglobin (HbA1c), fasting glucose, total cholesterol, HDL, triglycerides, albumin-to-creatinine ratio (ACR), creatinine).
- -
- Possible sensorimotor diabetic polyneuropathy based on the presence of DPN symptoms or signs;
- -
- Probable sensorimotor diabetic polyneuropathy based on the co-presence of symptoms and signs of DPN;
- -
- Confirmed sensorimotor diabetic polyneuropathy because the patient has had abnormal findings in an abnormal nerve conduction study (defined as abnormal findings in at least two separate nerves, one of which should be the sural nerve) and a symptom or symptoms or sign or signs of DPN;
- -
- Without sensorimotor diabetic polyneuropathy due to the absence of signs, symptoms and a negative nerve conduction study.
- (1)
- Diabetics with high PA if they achieved a minimum total physical activity of 1500 MET minutes/week of vigorous-intensity activity on at least 3 days or who achieved a minimum total physical activity of 3000 MET minutes/week on 7 or more days of any combination of walking, moderate-intensity or vigorous-intensity activities;
- (2)
- Diabetics with moderate PA if they are engaged in 20 min per day of vigorous activity for 3 or more days; if they engaged in 30 min per day of moderate activity or walking for 5 days or more; or, finally, if they achieved a minimum total physical activity of at least 600 MET minutes/week of walking, moderate activities or vigorous activities for 5 or more days;
- (3)
- Inactive if the patient did not meet the criteria for the previous two categories.
2.3. Statistical Analyses
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Feldman, E.L.; Callaghan, B.C.; Pop-Busui, R.; Zochodne, D.W.; Wright, D.E.; Bennett, D.L.; Bril, V.; Russell, J.W.; Viswanathan, V. Diabetic Neuropathy. Nat. Rev. Dis. Primers 2019, 5, 42. [Google Scholar] [CrossRef] [PubMed]
- Franklin, G.M.; Kahn, L.B.; Baxter, J.; Marshall, J.A.; Hamman, R.F. Sensory Neuropathy In Non-Insulin-Dependent Diabetes Mellitus. Am. J. Epidemiol. 1990, 131, 633–643. [Google Scholar] [CrossRef] [PubMed]
- Partanen, J.; Niskanen, L.; Lehtinen, J.; Mervaala, E.; Siitonen, O.; Uusitupa, M. Natural History of Peripheral Neuropathy in Patients with Non-Insulin-Dependent Diabetes Mellitus. N. Engl. J. Med. 1995, 333, 89–94. [Google Scholar] [CrossRef] [PubMed]
- Dyck, P.J.; Kratz, K.M.; Karnes, J.L.; Litchy, W.J.; Klein, R.; Pach, J.M.; Wilson, D.M.; O’Brien, P.C.; Melton, L.J. The Prevalence by Staged Severity of Various Types of Diabetic Neuropathy, Retinopathy, and Nephropathy in a Population-Based Cohort: The Rochester Diabetic Neuropathy Study. Neurology 1993, 43, 817. [Google Scholar] [CrossRef]
- Boulton, A.J.M.; Knight, G.; Drury, J.; Ward, J.D. The Prevalence of Symptomatic, Diabetic Neuropathy in an Insulin-Treated Population. Diabetes Care 1985, 8, 125–128. [Google Scholar] [CrossRef]
- Tesfaye, S.; Chaturvedi, N.; Eaton, S.E.M.; Ward, J.D.; Manes, C.; Ionescu-Tirgoviste, C.; Witte, D.R.; Fuller, J.H. Vascular Risk Factors and Diabetic Neuropathy. N. Engl. J. Med. 2005, 352, 341–350. [Google Scholar] [CrossRef]
- Tesfaye, S.; Boulton, A.J.M.; Dyck, P.J.; Freeman, R.; Horowitz, M.; Kempler, P.; Lauria, G.; Malik, R.A.; Spallone, V.; Vinik, A.; et al. Diabetic Neuropathies: Update on Definitions, Diagnostic Criteria, Estimation of Severity, and Treatments. Diabetes Care 2010, 33, 2285–2293. [Google Scholar] [CrossRef]
- Dyck, P.J.; Albers, J.W.; Andersen, H.; Arezzo, J.C.; Biessels, G.-J.; Bril, V.; Feldman, E.L.; Litchy, W.J.; O’Brien, P.C.; Russell, J.W. Diabetic Polyneuropathies: Update on Research Definition, Diagnostic Criteria and Estimation of Severity. Diabetes Metab. Res. Rev. 2011, 27, 620–628. [Google Scholar] [CrossRef]
- Loprinzi, P.D.; Hager, K.K.; Ramulu, P.Y. Physical Activity, Glycemic Control, and Diabetic Peripheral Neuropathy: A National Sample. J. Diabetes Complicat. 2014, 28, 17–21. [Google Scholar] [CrossRef]
- Loprinzi, P.D.; Ramulu, P.Y. Objectively Measured Physical Activity and Inflammatory Markers Among US Adults with Diabetes: Implications for Attenuating Disease Progression. Mayo Clin. Proc. 2013, 88, 942–951. [Google Scholar] [CrossRef]
- Boulé, N.G.; Haddad, E.; Kenny, G.P.; Wells, G.A.; Sigal, R.J. Effects of Exercise on Glycemic Control and Body Mass in Type 2 Diabetes Mellitus. JAMA 2001, 286, 1218. [Google Scholar] [CrossRef]
- Sigal, R.J.; Kenny, G.P.; Wasserman, D.H.; Castaneda-Sceppa, C.; White, R.D. Physical Activity/Exercise and Type 2 Diabetes. Diabetes Care 2006, 29, 1433–1438. [Google Scholar] [CrossRef]
- American Diabetes Association; Standards of Medical Care in Diabetes–2006. Diabetes Care 2006, 29, s4–s42. [CrossRef]
- Armstrong, D.G.; Lavery, L.A.; Holtz-Neiderer, K.; Mohler, M.J.; Wendel, C.S.; Nixon, B.P.; Boulton, A.J.M. Variability in Activity May Precede Diabetic Foot Ulceration. Diabetes Care 2004, 27, 1980–1984. [Google Scholar] [CrossRef]
- LeMaster, J.W.; Mueller, M.J.; Reiber, G.E.; Mehr, D.R.; Madsen, R.W.; Conn, V.S. Effect of Weight-Bearing Activity on Foot Ulcer Incidence in People with Diabetic Peripheral Neuropathy: Feet First Randomized Controlled Trial. Phys. Ther. 2008, 88, 1385–1398. [Google Scholar] [CrossRef]
- Balducci, S.; Iacobellis, G.; Parisi, L.; Di Biase, N.; Calandriello, E.; Leonetti, F.; Fallucca, F. Exercise Training Can Modify the Natural History of Diabetic Peripheral Neuropathy. J. Diabetes Complicat. 2006, 20, 216–223. [Google Scholar] [CrossRef]
- Allet, L.; Armand, S.; de Bie, R.A.; Golay, A.; Monnin, D.; Aminian, K.; Staal, J.B.; de Bruin, E.D. The Gait and Balance of Patients with Diabetes Can Be Improved: A Randomised Controlled Trial. Diabetologia 2010, 53, 458–466. [Google Scholar] [CrossRef] [PubMed]
- Morrison, S.; Colberg, S.R.; Parson, H.K.; Vinik, A.I. Exercise Improves Gait, Reaction Time and Postural Stability in Older Adults with Type 2 Diabetes and Neuropathy. J. Diabetes Complicat. 2014, 28, 715–722. [Google Scholar] [CrossRef] [PubMed]
- Kluding, P.M.; Pasnoor, M.; Singh, R.; Jernigan, S.; Farmer, K.; Rucker, J.; Sharma, N.K.; Wright, D.E. The Effect of Exercise on Neuropathic Symptoms, Nerve Function, and Cutaneous Innervation in People with Diabetic Peripheral Neuropathy. J. Diabetes Complicat. 2012, 26, 424–429. [Google Scholar] [CrossRef] [PubMed]
- Feldman, E.L.; Stevens, M.J.; Thomas, P.K.; Brown, M.B.; Canal, N.; Greene, D.A. A Practical Two-Step Quantitative Clinical and Electrophysiological Assessment for the Diagnosis and Staging of Diabetic Neuropathy. Diabetes Care 1994, 17, 1281–1289. [Google Scholar] [CrossRef]
- Fedele, D.; Comi, G.; Coscelli, C.; Cucinotta, D.; Feldman, E.L.; Ghirlanda, G.; Greene, D.A.; Negrin, P.; Santeusanio, F. A Multicenter Study on the Prevalence of Diabetic Neuropathy in Italy. Italian Diabetic Neuropathy Committee. Diabetes Care 1997, 20, 836–843. [Google Scholar] [CrossRef] [PubMed]
- Mannocci, A.; Di Thiene, D.; Del Cimmuto, A.; Masala, D.; Boccia, A.; De Vito, E.; la Torre, G. International Physical Activity Questionnaire: Validation and Assessment in an Italian Sample. Ital. J. Public Health 2010, 7, 369–376. [Google Scholar]
- Vistisen, D.; Andersen, G.S.; Hansen, C.S.; Hulman, A.; Henriksen, J.E.; Bech-Nielsen, H.; Jørgensen, M.E. Prediction of First Cardiovascular Disease Event in Type 1 Diabetes Mellitus. Circulation 2016, 133, 1058–1066. [Google Scholar] [CrossRef] [PubMed]
- Colberg, S.R.; Sigal, R.J.; Yardley, J.E.; Riddell, M.C.; Dunstan, D.W.; Dempsey, P.C.; Horton, E.S.; Castorino, K.; Tate, D.F. Physical Activity/Exercise and Diabetes: A Position Statement of the American Diabetes Association. Diabetes Care 2016, 39, 2065–2079. [Google Scholar] [CrossRef]
- Herder, C.; Roden, M.; Ziegler, D. Novel Insights into Sensorimotor and Cardiovascular Autonomic Neuropathy from Recent-Onset Diabetes and Population-Based Cohorts. Trends Endocrinol. Metab. 2019, 30, 286–298. [Google Scholar] [CrossRef]
- Ahn, S.; Song, R. Effects of Tai Chi Exercise on Glucose Control, Neuropathy Scores, Balance, and Quality of Life in Patients with Type 2 Diabetes and Neuropathy. J. Altern. Complement. Med. 2012, 18, 1172–1178. [Google Scholar] [CrossRef]
- Streckmann, F.; Zopf, E.M.; Lehmann, H.C.; May, K.; Rizza, J.; Zimmer, P.; Gollhofer, A.; Bloch, W.; Baumann, F.T. Exercise Intervention Studies in Patients with Peripheral Neuropathy: A Systematic Review. Sports Med. 2014, 44, 1289–1304. [Google Scholar] [CrossRef]
- Riddell, M.C.; Gallen, I.W.; Smart, C.E.; Taplin, C.E.; Adolfsson, P.; Lumb, A.N.; Kowalski, A.; Rabasa-Lhoret, R.; McCrimmon, R.J.; Hume, C.; et al. Exercise Management in Type 1 Diabetes: A Consensus Statement. Lancet Diabetes Endocrinol. 2017, 5, 377–390. [Google Scholar] [CrossRef]
- Alves, A.J.; Viana, J.L.; Cavalcante, S.L.; Oliveira, N.L.; Duarte, J.A.; Mota, J.; Oliveira, J.; Ribeiro, F. Physical Activity in Primary and Secondary Prevention of Cardiovascular Disease: Overview Updated. World J. Cardiol. 2016, 8, 575. [Google Scholar] [CrossRef]
| Variables | Physical Activity | p Value | |||
|---|---|---|---|---|---|
| Low 19 (21.1%) | Moderate 37 (41.1%) | High 34 (37.8%) | |||
| Age (years) | 49.0 (41.0–55.8) | 51.0 (47.0–60.5) | 51.0 (39.0–56.0) | 46.0 (38.0–50.0) | 0.125 |
| Sex n (%) | male 47 (52.2) | 9 (10.0) | 24 (26.7) | 14 (15.6) | 0.122 |
| female 43 (47.8) | 10 (11.1) | 13 (14.4) | 20 (22.2) | ||
| BMI (kg/m2) | 23.6 (21.8–25.9) | 23.4 (20.9–24.9) | 25.0 (22.9–28.5) | 22.6 (21.3–23.9) | 0.053 |
| Smoking n (%) | 24 (26.7) | 7 (7.8) | 8 (8.9) | 9 (10) | 0.475 |
| Alcohol n (%) | 70 (77.8) | 14 (15.6) | 30 (33.3) | 26 (28.9) | 0.798 |
| Educational level n (%) | lower middle school 7 (7.8) | 1 (1.1) | 2 (2.2) | 4 (4.4) | |
| high school 50 (55.6) | 10 (11.1) | 19 (21.1) | 21 (23.3) | 0.549 | |
| university 33 (36.7) | 8 (8.9) | 16 (17.8) | 9 (10.0) | ||
| DM duration (years) | 21.0 (14.3–34.0) | 23.0 (13.0–34.5) | 24.0 (15.0–40.0) | 19.5 (15.0–26.0) | 0.250 |
| DM therapy n (%) | CSII 58 (64.4) | 14 (15.6) | 21 (23.3) | 23 (25.6) | |
| Insulin basal-bolus 32 (35.6) | 5 (5.6) | 16 (17.8) | 11 (12.2) | 0.404 | |
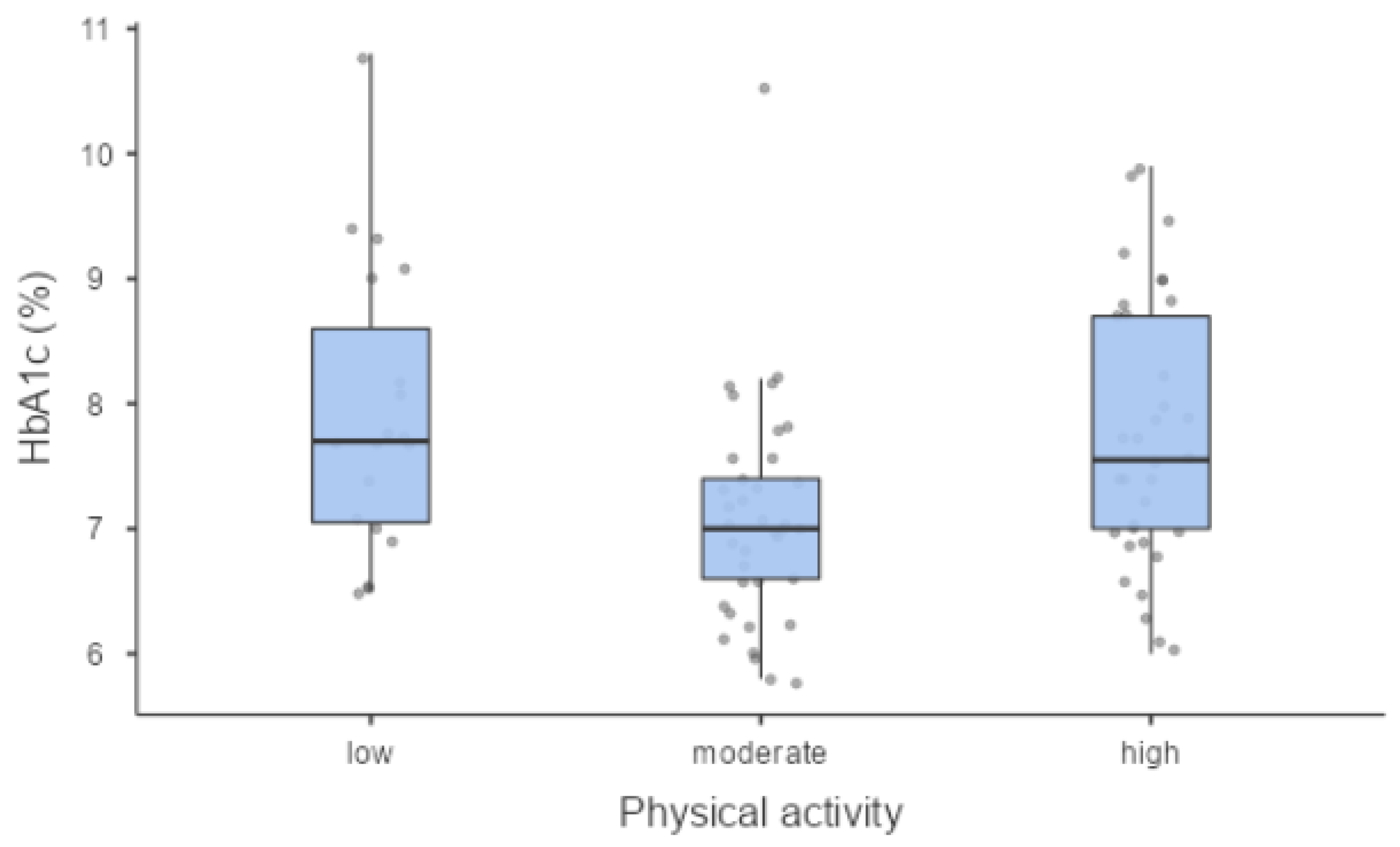
| HbA1c % (mmol/mol) | 7.35 (57) (6.82–8.07 (51–65)) | 7.70 (61) (7.05–8.60 (54–70)) | 7.00 (53) (6.60–7.40 (49–57)) | 7.55 (59) (7.00–8.70 (53–72)) | 0.004 |
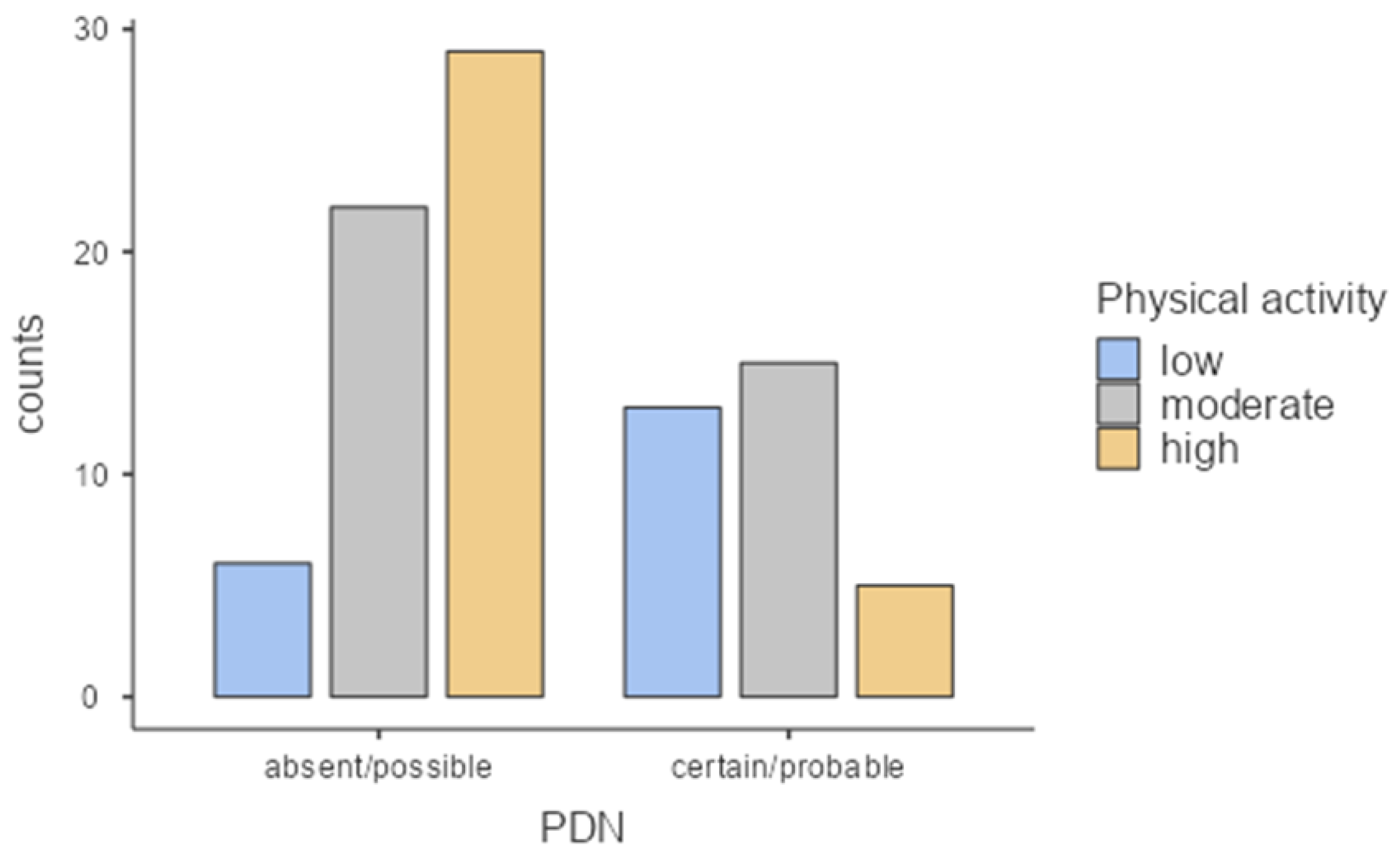
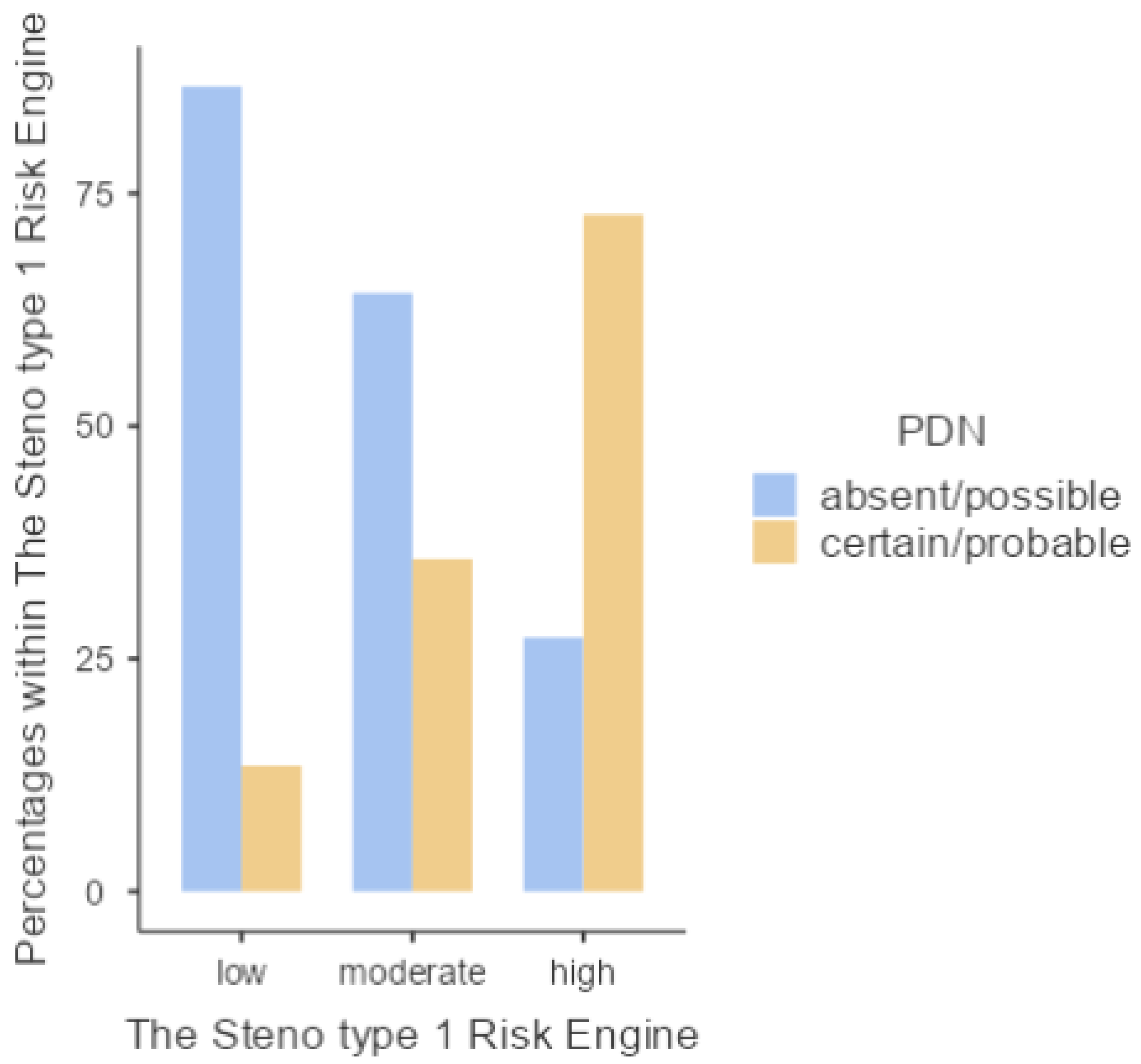
| DM complications n (%) | PDN absent/possible 57 (63.3) | 6 (6.7) | 22 (24.4) | 29 (32.2) | <0.001 |
| certain/probable 33 (36.7) | 13 (14.4) | 15 (16.7) | 5 (5.6) | ||
| Retinopathy 26 (28.9) | 8 (8.9) | 11 (12.2) | 7 (7.8) | 0.251 | |
| Nephropathy 10 (11.1) | 2 (2.2) | 6 (6.7) | 2 (2.2) | 0.382 | |
| Myocardial Infarction 3 (3.3) | |||||
| Carotid artery atheromasia 16 (17.8) | 4 (4.4) | 8 (8.9) | 4 (4.4) | 0.508 | |
| Hypertension n (%) | 24 (26.7) | 7 (7.8) | 12 (13.3) | 5 (5.6) | 0.127 |
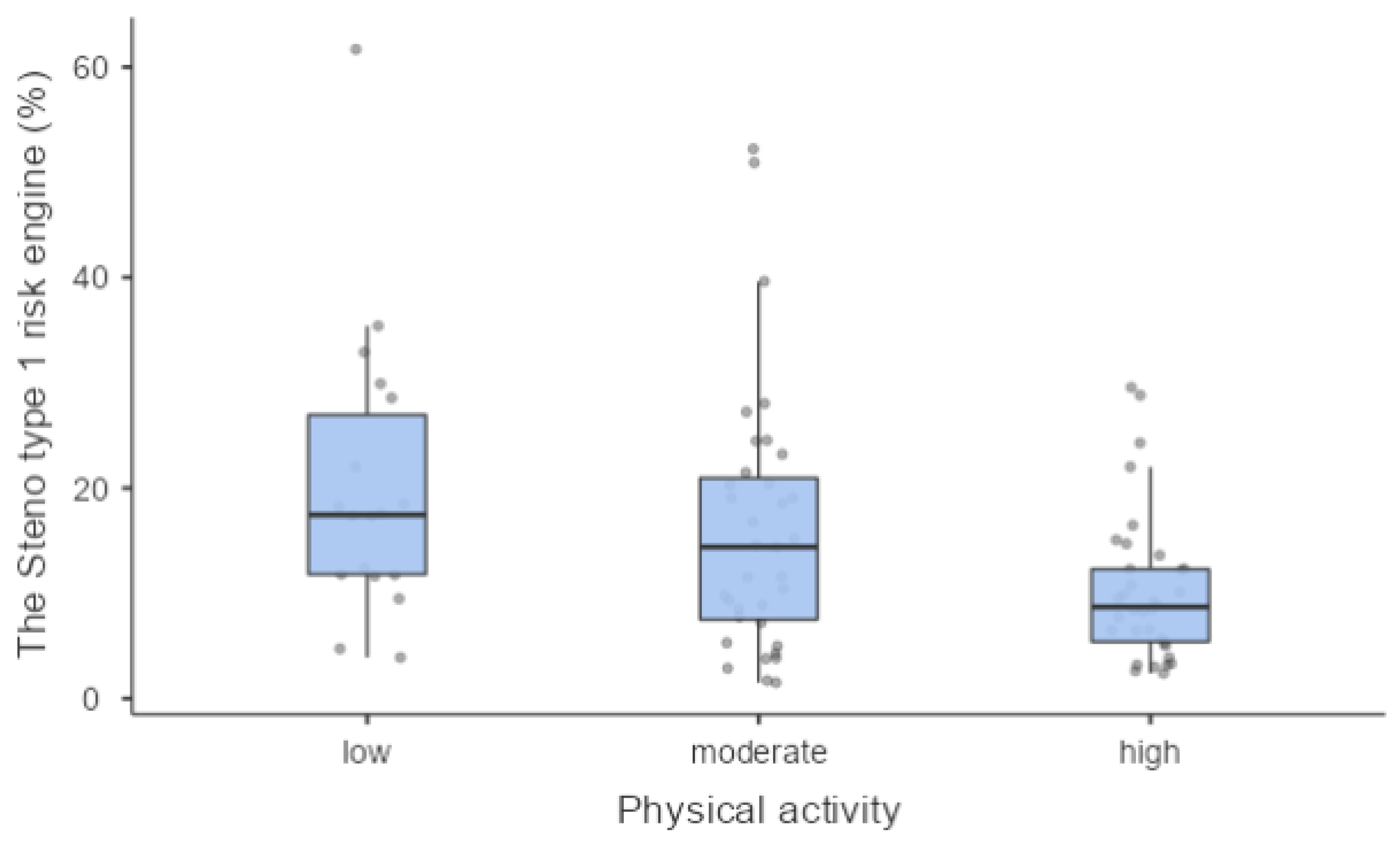
| Steno type 1 risk engine n (%) | low 37 (42.5) | 3 (3.4) | 14 (16.1) | 20 (23) | |
| moderate 28 (32.2) | 9 (10.3) | 10 (11.5) | 9 (10.3) | 0.045 | |
| high 22 (25.3) | 6 (6.9) | 11 (12.6) | 5 (5.7) |
| Physical Activity | |
|---|---|
| DPN absent/possible n. 57 (63.3%) | low n. 6 (6.7%) |
| moderate n. 22 (24.4%) | |
| high n. 29 (32.2%) | |
| DPN certain/probable n. 33 (36.7%) | low n. 13 (14.4%) |
| moderate n. 15 (16.7%) | |
| high n. 5 (5.6%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zaccaria, S.; Di Perna, P.; Giurato, L.; Pecchioli, C.; Sperti, P.; Arciprete, F.; Del Grande, A.; Nardone, I.; Wolde Sellasie, S.; Iani, C.; et al. Diabetic Polyneuropathy and Physical Activity in Type 1 Diabetes Mellitus: A Cross-Sectional Study. J. Clin. Med. 2023, 12, 6597. https://doi.org/10.3390/jcm12206597
Zaccaria S, Di Perna P, Giurato L, Pecchioli C, Sperti P, Arciprete F, Del Grande A, Nardone I, Wolde Sellasie S, Iani C, et al. Diabetic Polyneuropathy and Physical Activity in Type 1 Diabetes Mellitus: A Cross-Sectional Study. Journal of Clinical Medicine. 2023; 12(20):6597. https://doi.org/10.3390/jcm12206597
Chicago/Turabian StyleZaccaria, Simona, Pasquale Di Perna, Laura Giurato, Chiara Pecchioli, Patrizia Sperti, Flavio Arciprete, Alessandra Del Grande, Isabella Nardone, Sium Wolde Sellasie, Cesare Iani, and et al. 2023. "Diabetic Polyneuropathy and Physical Activity in Type 1 Diabetes Mellitus: A Cross-Sectional Study" Journal of Clinical Medicine 12, no. 20: 6597. https://doi.org/10.3390/jcm12206597
APA StyleZaccaria, S., Di Perna, P., Giurato, L., Pecchioli, C., Sperti, P., Arciprete, F., Del Grande, A., Nardone, I., Wolde Sellasie, S., Iani, C., & Uccioli, L. (2023). Diabetic Polyneuropathy and Physical Activity in Type 1 Diabetes Mellitus: A Cross-Sectional Study. Journal of Clinical Medicine, 12(20), 6597. https://doi.org/10.3390/jcm12206597






