Effects of a Therapeutic Exercise Protocol for Patients with Chronic Non-Specific Back Pain in Primary Health Care: A Single-Group Retrospective Cohort Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants
2.3. Measurement Outcomes
2.4. Therapeutic Exercise Protocol
2.5. Statistical Analysis
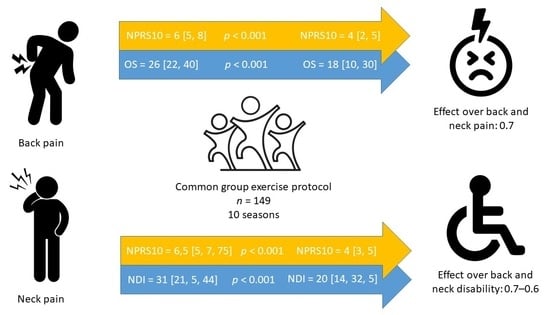
3. Results
3.1. Chronic Non-Specific Low-Back Pain Patients
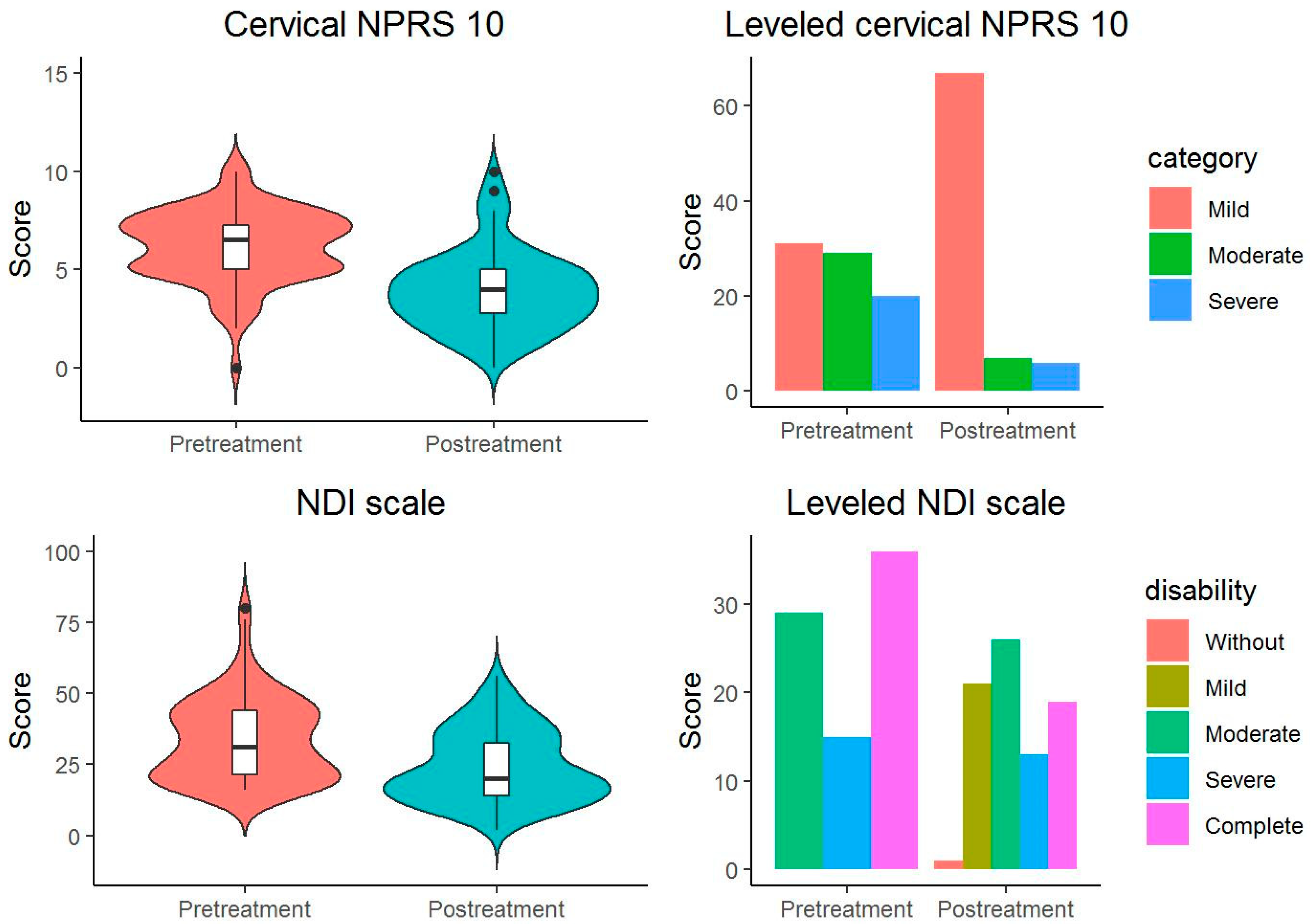
3.2. Patients with Chronic Non-Specific Neck Pain
3.3. Median Pain Intensity Between-Group Comparison
3.4. Patients with Chronic Non-Specific Low-Back Pain
3.5. Patients with Chronic Non-Specific Neck Pain
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Fett, D.; Trompeter, K.; Platen, P. Prevalence of back pain in a group of elite athletes exposed to repetitive overhead activity. PLoS ONE 2019, 14, e0210429. [Google Scholar] [CrossRef]
- Schwertner, D.S.; Oliveira, R.A.N.S.; Koerich, M.H.A.L.; Motta, A.F.; Pimenta, A.L.; Gioda, F.R. Prevalence of low back pain in young Brazilians and associated factors: Sex, physical activity, sedentary behavior, sleep and body mass index. J. Back Musculoskelet. Rehabil. 2020, 33, 233–244. [Google Scholar] [CrossRef]
- Fernández-Carnero, J.; Beltrán-Alacreu, H.; Arribas-Romano, A.; Cerezo-Téllez, E.; Cuenca-Zaldivar, J.N.; Sánchez-Romero, E.A.; Lara, S.L.; Villafañe, J.H. Prediction of Patient Satisfaction after Treatment of Chronic Neck Pain with Mulligan’s Mobilization. Life 2022, 13, 48. [Google Scholar] [CrossRef] [PubMed]
- Martin, B.I.; Deyo, R.A.; Mirza, S.K.; Turner, J.A.; Comstock, B.A.; Hollingworth, W.; Sullivan, S.D. Expenditures and health status among adults with back and neck problems. JAMA—J. Am. Med. Assoc. 2008, 299, 656–664. [Google Scholar] [CrossRef]
- Laguna, J.M.; Puhan, M.A.; Artalejo, F.R.; De Pauw, R.; Wyper, G.M.A.; Devleesschauwer, B.; Santos, J.V.; Hincapié, C.A. Certainty of the Global Burden of Disease 2019 Modelled Prevalence Estimates for Musculoskeletal Conditions: A Meta-Epidemiological Study. Int. J. Public Health 2023, 68, 1605763. [Google Scholar] [CrossRef] [PubMed]
- Deyo, R.A.; Weinstein, J.N. Low back pain. N. Engl. J. Med. 2001, 344, 363–370. [Google Scholar] [CrossRef]
- Fernández-de-las-Peñas, C.; Hernández-Barrera, V.; Alonso-Blanco, C.; Palacios-Ceña, D.; Carrasco-Garrido, P.; Jiménez-Sánchez, S.; Jiménez-García, R. Prevalence of Neck and Low Back Pain in Community-Dwelling Adults in Spain. Spine 2011, 36, E213–E219. [Google Scholar] [CrossRef] [PubMed]
- Calais-Ferreira, L.; Pozzobon, D.; Pinheiro, M.B.; Blyth, F.M.; Ordoñana, J.R.; Duncan, G.E.; Hopper, J.L.; Ferreira, P.H.; Ferreira, M.L. Sex differences in lifetime prevalence of low back pain: A multinational study of opposite-sex twin pairs. Eur. J. Pain. 2023. [Google Scholar] [CrossRef]
- Meucci, R.D.; Fassa, A.G.; Faria, N.M.X. Prevalence of chronic low back pain: Systematic review. Rev. Saude Publica 2015, 2015, 49. [Google Scholar] [CrossRef]
- Palacios-Ceña, D.; Alonso-Blanco, C.; Hernández-Barrera, V.; Carrasco-Garrido, P.; Jiménez-García, R.; Fernández-de-las-Peñas, C. Prevalence of neck and low back pain in community-dwelling adults in Spain: An updated population-based national study. Eur. Spine J. 2015, 24, 482–492. [Google Scholar] [CrossRef]
- Øverås, C.K.; Nilsen, T.I.L.; Søgaard, K.; Mork, P.J.; Hartvigsen, J. Temporal stability in the prevalence and pattern of co-occurring musculoskeletal pain among people with persistent low back pain: Population-based data from the Norwegian HUNT Study, 1995 to 2019. Pain 2023. [Google Scholar] [CrossRef] [PubMed]
- Makris, U.E.; Weinreich, M.A.; Fraenkel, L.; Han, L.; Leo-Summers, L.; Gill, T.M. Restricting Back Pain and Subsequent Disability in Activities of Daily Living Among Community-Living Older Adults. J. Aging Health 2018, 30, 1482–1494. [Google Scholar] [CrossRef] [PubMed]
- Balagué, F.; Mannion, A.F.; Pellisé, F.; Cedraschi, C. Non-specific low back pain. Lancet 2012, 379, 482–491. [Google Scholar] [CrossRef] [PubMed]
- Sánchez Romero, E.A.; Alonso Pérez, J.L.; Muñoz Fernández, A.C.; Battaglino, A.; Castaldo, M.; Cleland, J.A.; Villafañe, J.H. Reliability of Sonography Measures of the Lumbar Multifidus and Transversus Abdominis during Static and Dynamic Activities in Subjects with Non-Specific Chronic Low Back Pain. Diagnostics 2021, 11, 632. [Google Scholar] [CrossRef]
- Joseph, L.; Vasanthan, L.; Standen, M.; Kuisma, R.; Paungmali, A.; Pirunsan, U.; Sitilertpisan, P. Causal Relationship between the Risk Factors and Work-Related Musculoskeletal Disorders Among Professional Drivers: A Systematic Review. Hum. Factors J. Hum. Factors Ergon. Soc. 2023, 65, 62–85. [Google Scholar] [CrossRef]
- Ruffilli, A.; Neri, S.; Manzetti, M.; Barile, F.; Viroli, G.; Traversari, M.; Assirelli, E.; Vita, F.; Geraci, G.; Faldini, C. Epigenetic Factors Related to Low Back Pain: A Systematic Review of the Current Literature. Int. J. Mol. Sci. 2023, 24, 1854. [Google Scholar] [CrossRef]
- Beynon, A.M.; Hebert, J.J.; Lebouef-Yde, C.; Walker, B.F. Potential risk factors and triggers for back pain in children and young adults. A scoping review, part II: Unclear or mixed types of back pain. Chiropr. Man. Ther. 2019, 27, 61. [Google Scholar] [CrossRef]
- Lu, W.; Shen, Z.; Chen, Y.; Hu, X.; Ruan, C.; Ma, W.; Jiang, W. Risk factors analysis and risk prediction model construction of non-specific low back pain: An ambidirectional cohort study. J. Orthop. Surg. Res. 2023, 18, 545. [Google Scholar] [CrossRef]
- Qaseem, A.; Wilt, T.J.; McLean, R.M.; Forciea, M.A. Noninvasive treatments for acute, subacute, and chronic low back pain: A clinical practice guideline from the American College of Physicians. Ann. Intern. Med. 2017, 166, 514–530. [Google Scholar] [CrossRef]
- Wanjau, M.N.; Möller, H.; Haigh, F.; Milat, A.; Hayek, R.; Lucas, P.; Veerman, J.L. The Potential Impact of Physical Activity on the Burden of Osteoarthritis and Low Back Pain in Australia: A Systematic Review of Reviews and Life Table Analysis. J. Phys. Act. Health 2023, 20, 690–701. [Google Scholar] [CrossRef]
- Mu, J.; Furlan, A.D.; Lam, W.Y.; Hsu, M.Y.; Ning, Z.; Lao, L. Acupuncture for chronic nonspecific low back pain. Cochrane Database Syst. Rev. 2020, 12, CD013814. [Google Scholar]
- Zaina, F.; Côté, P.; Cancelliere, C.; Di Felice, F.; Donzelli, S.; Rauch, A.; Verville, L.; Negrini, S.; Nordin, M. A Systematic Review of Clinical Practice Guidelines for Persons with Non-specific Low Back Pain with and without Radiculopathy: Identification of Best Evidence for Rehabilitation to Develop the WHO’s Package of Interventions for Rehabilitation. Arch. Phys. Med. Rehabil. 2023, in press. [CrossRef] [PubMed]
- Nascimento, P.R.C.; do Costa, L.O.P.; Araujo, A.C.; Poitras, S.; Bilodeau, M. Effectiveness of interventions for non-specific low back pain in older adults. A systematic review and meta-analysis. Physiotherapy 2019, 105, 147–162. [Google Scholar] [CrossRef]
- Huntoon, M.A.; Slavin, K.V.; Hagedorn, J.M.; Crosby, N.D.; Boggs, J.W. A Retrospective Review of Real-world Outcomes Following 60-day Peripheral Nerve Stimulation for the Treatment of Chronic Pain. Pain Physician 2023, 23, 273–281. [Google Scholar]
- Yang, H.; Wang, X.; Wang, X.; Yang, J.; Zhang, W.; Ding, Y.; Sang, T.; Chen, W.; Wang, W. Effect of mindfulness-based mind-body therapies in patients with non-specific low back pain—A network meta-analysis of randomized controlled trials. Front. Aging Neurosci. 2023, 15, 1148048. [Google Scholar] [CrossRef] [PubMed]
- Childress, M.A.; Stuek, S.J. Neck Pain: Initial Evaluation and Management. Am. Fam. Physician 2020, 102, 150–156. [Google Scholar]
- Pedersen, B.K.; Saltin, B. Exercise as medicine—Evidence for prescribing exercise as therapy in 26 different chronic diseases. Scand. J. Med. Sci. Sports 2015, 25, 1–72. [Google Scholar] [CrossRef]
- Steinacker, J.M.; van Mechelen, W.; Bloch, W.; Börjesson, M.; Casasco, M.; Wolfarth, B.; Knoke, C.; Papadopoulou, T.; Wendt, J.; Al Tunaiji, H.; et al. Global Alliance for the Promotion of Physical Activity: The Hamburg Declaration. BMJ Open Sport Exerc. Med. 2023, 9, e001626. [Google Scholar] [CrossRef]
- Alzahrani, H.; Mackey, M.; Stamatakis, E.; Pinheiro, M.B.; Wicks, M.; Shirley, D. The effectiveness of incidental physical activity interventions compared to other interventions in the management of people with low back pain: A systematic review and meta-analysis of randomised controlled trials. Phys. Ther. Sport 2019, 36, 34–42. [Google Scholar] [CrossRef]
- He, Y.; Sun, W.; Zhao, X.; Ma, M.; Zheng, Z.; Xu, L. Effects of core stability exercise for patients with neck pain: A protocol for systematic review and meta-analysis. Medicine 2019, 98, e17240. [Google Scholar] [CrossRef]
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. Declaración de la iniciativa STROBE (Strengthening the Reporting of Observational Studies in Epidemiology): Directrices para la comunicación de estudios observacionales. Rev. Esp. Salud Publica 2008, 82, 251–259. [Google Scholar] [CrossRef] [PubMed]
- Alcántara-Bumbiedro, S.; Flórez-García, M.T.; Echávarri-Pérez, C.; García-Pérez, F. Escala de incapacidad por dolor lumbar de Oswestry. Rehabilitacion 2006, 40, 150–158. [Google Scholar] [CrossRef]
- Alfonso Andrade Ortega, J.; Damián Delgado Martínez, A.; Almécija Ruiz, R. Validación de una versión española del Índice de Discapacidad Cervical. Med. Clin. 2008, 130, 85–89. [Google Scholar] [CrossRef] [PubMed]
- Montero Ibáñez, R.; Briega, A.M. Escalas de valoración del dolor. Jano 2012, 25, 41–44. [Google Scholar]
- Young, B.A.; Walker, M.J.; Strunce, J.B.; Boyles, R.E.; Whitman, J.M.; Childs, J.D. Responsiveness of the Neck Disability Index in patients with mechanical neck disorders. Spine J. 2009, 9, 802–808. [Google Scholar] [CrossRef] [PubMed]
- Shaheen, A.A.M.; Omar, M.T.A.; Vernon, H. Cross-cultural adaptation, reliability, and validity of the arabic version of neck disability index in patients with neck pain. Spine 2013, 38, 609–615. [Google Scholar] [CrossRef]
- Hains, F.; Waalen, J.; Mior, S. Psychometric properties of the neck disability index. J. Manip. Physiol. Ther. 1998, 21, 75–80. [Google Scholar]
- Johnsen, L.G.; Hellum, C.; Nygaard, P.; Storheim, K.; Brox, J.I.; Rossvoll, I.; Leivseth, G.; Grotle, M. Comparison of the SF6D, the EQ5D, and the oswestry disability index in patients with chronic low back pain and degenerative disc disease. BMC Musculoskelet. Disord. 2013, 14, 148. [Google Scholar] [CrossRef]
- Boonstra, A.M.; Schiphorst Preuper, H.R.; Balk, G.A.; Stewart, R.E. Cut-off points for mild, moderate, and severe pain on the visual analogue scale for pain in patients with chronic musculoskeletal pain. Pain 2014, 155, 2545–2550. [Google Scholar] [CrossRef]
- Jensen, M.P.; McFarland, C.A. Increasing the reliability and validity of pain intensity measurement in chronic pain patients. Pain 1993, 55, 195–203. [Google Scholar] [CrossRef]
- Farrar, J.T.; Young, J.P.; LaMoreaux, L.; Werth, J.L.; Poole, R.M. Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. Pain 2001, 94, 149–158. [Google Scholar] [CrossRef]
- Mann, S.J.; Lam, J.C.; Singh, P. McKenzie Back Exercises; StatPearls Publishing: Treasure Island, FL, USA, 2023. [Google Scholar]
- Jonhnson, J. The Multifidus. Back Pain Solution; New Harbinger Publications Inc.: Oakland, CA, USA, 2002. [Google Scholar]
- McKenzie, R. Treat Your Own Back, 9th ed.; Orthopedic Physical Therapy Products: Waikanae, New Zealand, 2011. [Google Scholar]
- McKenzie, R. Treat Your Own Neck, 5th ed.; Orthopedic Physical Therapy Products: Raumati Beach, New Zealand, 2011. [Google Scholar]
- Li, Y.; Tse, M.Y.M. An Online Pain Education Program for Working Adults: Pilot Randomized Controlled Trial. J. Med. Internet Res. 2020, 22, e15071. [Google Scholar] [CrossRef]
- Owen, P.J.; Miller, C.T.; Mundell, N.L.; Verswijveren, S.J.; Tagliaferri, S.D.; Brisby, H.; Bowe, S.; Belavy, D.L. Which specific modes of exercise training are most effective for treating low back pain? Network meta-analysis. Br. J. Sports Med. 2020, 54, 1279–1287. [Google Scholar] [CrossRef] [PubMed]
- Lauridsen, H.H.; Hartvigsen, J.; Manniche, C.; Korsholm, L.; Grunnet-Nilsson, N. Responsiveness and minimal clinically important difference for pain and disability instruments in low back pain patients. BMC Musculoskelet. Disord. 2006, 25, 82. [Google Scholar] [CrossRef] [PubMed]
- Petersen, T.; Larsen, K.; Nordsteen, J.; Olsen, S.; Fournier, G.; Jacobsen, S. The McKenzie method compared with manipulation when used adjunctive to information and advice in low back pain patients presenting with centralization or peripheralization: A randomized controlled trial. Spine 2011, 36, 1999–2010. [Google Scholar] [CrossRef] [PubMed]
- Garcia, A.N.; Costa, L.D.C.M.; Hancock, M.J.; De Souza, F.S.; de Oliveira Gomes, G.V.F.; De Almeida, M.O.; Costa, L.O.P. McKenzie Method of Mechanical Diagnosis and Therapy was slightly more effective than placebo for pain, but not for disability, in patients with chronic non-specific low back pain: A randomised placebo controlled trial with short and longer term follow-up. Br. J. Sports Med. 2018, 52, 594–598. [Google Scholar] [CrossRef]
- Paatelma, M.; Kilpikoski, S.; Simonen, R.; Heinonen, A.; Alen, M.; Videman, T. Orthopaedic manual therapy, Mckenzie method or advice only for low back pain in working adults: A randomized controlled trial with one year follow-up. J. Rehabil. Med. 2008, 40, 858–863. [Google Scholar] [CrossRef]
- Garcia, A.N.; Costa, L.d.C.M.; da Silva, T.M.; Gondo, F.L.B.; Cyrillo, F.N.; Costa, R.A.; Costa, L.O.P. Effectiveness of back school versus McKenzie exercises in patients with chronic nonspecific low back pain: A randomized controlled trial. Phys. Ther. 2013, 93, 729–747. [Google Scholar] [CrossRef]
- Luetchford, S.; Declich, M.; Tavella, R.; Zaninelli, D.; May, S. Diagnosis of cervical and thoracic musculoskeletal spinal pain receptive to mechanical movement strategies: A multicenter observational study. J. Man. Manip. Ther. 2018, 26, 292–300. [Google Scholar] [CrossRef]
- Yarznbowicz, R.; Tao, M.; Wlodarski, M.; Dolutan, J. Pain pattern classification and directional preference for patients with neck pain. J. Man. Manip. Ther. 2018, 26, 230–236. [Google Scholar] [CrossRef]
- Baumann, A.N.; Orellana, K.; Landis, L.; Oleson, C.J.; Rogers, H.; Curtis, D.P.; Baldwin, K.D.; Crawford, M.T. The McKenzie Method Is an Effective Rehabilitation Paradigm for Treating Adults with Moderate-to-Severe Neck Pain: A Systematic Review with Meta-Analysis. Cureus 2023, 15, e39218. [Google Scholar] [CrossRef] [PubMed]
- Almeida, M.O.; Narciso Garcia, A.; Menezes Costa, L.C.; van Tulder, M.W.; Lin, C.W.C.; Machado, L.A. The McKenzie method for (sub)acute non-specific low back pain. Cochrane Database Syst. Rev. 2023, 4, CD009711. [Google Scholar] [PubMed]
- Wang, X.-Q.; Zheng, J.-J.; Yu, Z.-W.; Bi, X.; Lou, S.-J.; Liu, J.; Cai, B.; Hua, Y.-H.; Wu, M.; Wei, M.-L.; et al. A Meta-Analysis of Core Stability Exercise versus General Exercise for Chronic Low Back Pain. Eldabe S, editor. PLoS ONE 2012, 7, e52082. [Google Scholar]
- Coulombe, B.J.; Games, K.E.; Neil, E.R.; Eberman, L.E. Core Stability Exercise Versus General Exercise for Chronic Low Back Pain. J. Athl. Train. 2017, 52, 71–72. [Google Scholar] [CrossRef]
- Falla, D.; Hodges, P.W. Individualized Exercise Interventions for Spinal Pain. Exerc. Sport Sci. Rev. 2017, 45, 105–115. [Google Scholar] [CrossRef]
- Naugle, K.M.; Naugle, K.E.; Fillingim, R.B.; Samuels, B.; Riley, J.L. Intensity thresholds for aerobic exercise-induced hypoalgesia. Med. Sci. Sports Exerc. 2014, 46, 817–825. [Google Scholar] [CrossRef]
- Black, C.D.; Huber, J.K.; Ellingson, L.D.; Ade, C.J.; Taylor, E.L.; Griffeth, E.M.; Janzen, N.R.; Sutterfield, S.L. Exercise-Induced Hypoalgesia Is Not Influenced by Physical Activity Type and Amount. Med. Sci. Sports Exerc. 2017, 49, 975–982. [Google Scholar] [CrossRef]
- Sánchez-Romero, E.A.; de-Pedro, M.; Fernández-Carnero, J. Editorial to the Special Issue The Effect of Exercise Intensity and Psychological Intervention on Musculoskeletal Disorders. Int. J. Environ. Res. Public Health 2023, 20, 5777. [Google Scholar] [CrossRef]
- Alonso Pérez, J.L.; Martín Pérez, S.; Battaglino, A.; Villafañe, J.H.; Alonso-Sal, A.; Sánchez Romero, E.A. An Up-Date of the Muscle Strengthening Exercise Effectiveness in Postmenopausal Women with Osteoporosis: A Qualitative Systematic Review. J. Clin. Med. 2021, 10, 2229. [Google Scholar] [CrossRef]
- Hayden, J.A.; Van Tulder, M.W.; Tomlinson, G. Systematic review: Strategies for using exercise therapy to improve outcomes in chronic low back pain. Ann. Intern. Med. 2005, 142, 776–785. [Google Scholar] [CrossRef]
- Good, M. A comparison of the effects of jaw relaxation and music on postoperative pain. Nurs. Res. 1995, 44, 52–57. [Google Scholar] [CrossRef]
- Salt, E.; Wright, C.; Kelly, S.; Dean, A. A systematic literature review on the effectiveness of non-invasive therapy for cervicobrachial pain. Man. Ther. 2011, 16, 53–65. [Google Scholar] [CrossRef]
- Hidalgo, B.; Hall, T.; Bossert, J.; Dugeny, A.; Cagnie, B.; Pitance, L. The efficacy of manual therapy and exercise for treating non-specific neck pain: A systematic review. J. Back Musculoskelet. Rehabil. 2017, 30, 1149–1169. [Google Scholar] [CrossRef] [PubMed]
- Gross, A.; Paquin, J.; Dupont, G.; Blanchette, S.; Lalonde, P.; Cristie, T.; Graham, N.; Kay, T.; Burnie, S.; Gelley, G.; et al. Exercises for mechanical neck disorders: A Cochrane review update. Man. Ther. 2016, 24, 25–45. [Google Scholar] [CrossRef] [PubMed]
- Gross, A.; Kay, T.M.; Paquin, J.P.; Blanchette, S.; Lalonde, P.; Christie, T.; Dupont, G.; Graham, N.; Burnie, S.J.; Gelley, G.; et al. Exercises for Mechanical Neck Disorders. Cochrane Database Syst. Rev. 2015, 1, CD004250. [Google Scholar] [CrossRef]
- Leaver, A.M.; Refshauge, K.M.; Maher, C.G.; McAuley, J.H. Conservative interventions provide short-term relief for non-specific neck pain: A systematic review. J. Physiother. 2010, 56, 73–85. [Google Scholar] [CrossRef] [PubMed]
- Gross, A.; Miller, J.; D’sylva, J.; Burnie, S.J.; Goldsmith, C.H.; Graham, N.; Haines, T.; Brønfort, G.; Hoving, J.L. Manipulation or mobilisation for neck pain: A Cochrane Review. Man. Ther. 2010, 15, 315–333. [Google Scholar] [CrossRef]
- Gumuscu, B.H.; Kisa, E.P.; Kara Kaya, B.; Muammer, R. Comparison of three different exercise trainings in patients with chronic neck pain: A randomized controlled study. Korean J. Pain 2023, 36, 242–252. [Google Scholar] [CrossRef] [PubMed]
- Areeudomwong, P.; Buttagat, V. Comparison of Core Stabilisation Exercise and Proprioceptive Neuromuscular Facilitation Training on Pain-related and Neuromuscular Response Outcomes for Chronic Low Back Pain: A Randomised Controlled Trial. Malays. J. Med. Sci. 2019, 26, 77–89. [Google Scholar] [CrossRef]
- Niederer, D.; Mueller, J. Sustainability effects of motor control stabilisation exercises on pain and function in chronic nonspecific low back pain patients: A systematic review with meta-analysis and meta-regression. PLoS ONE 2020, 15, e0227423. [Google Scholar] [CrossRef]
- Bloxham, S.R.; Layden, J.; Jane, B.; Peers, C.; Scragg, S. The longitudinal effects of a physical activity programme on the physical fitness and disability of back pain patients: Service evaluation. J. Back Musculoskelet. Rehabil. 2020, 33, 7–13. [Google Scholar] [CrossRef] [PubMed]
- Gordon, R.; Bloxham, S. A Systematic Review of the Effects of Exercise and Physical Activity on Non-Specific Chronic Low Back Pain. Healthcare 2016, 4, 22. [Google Scholar] [CrossRef]
- Babatunde, O.O.; Jordan, J.L.; Van Der Windt, D.A.; Hill, J.C.; Foster, N.E.; Protheroe, J. Effective treatment options for musculoskeletal pain in primary care: A systematic overview of current evidence. PLoS ONE 2017, 12, e0178621. [Google Scholar] [CrossRef] [PubMed]
- Martínez-Pozas, O.; Sánchez-Romero, E.A.; Beltran-Alacreu, H.; Arribas-Romano, A.; Cuenca-Martínez, F.; Villafañe, J.H.; Fernández-Carnero, J. Effects of Orthopedic Manual Therapy on Pain Sensitization in Patients with Chronic Musculoskeletal Pain. Am. J. Phys. Med. Rehabil. 2023, 102, 879–885. [Google Scholar] [CrossRef] [PubMed]
- Ballestra, E.; Battaglino, A.; Cotella, D.; Rossettini, G.; Sanchez-Romero, E.A.; Villafane, J.H. Do patients’ expectations influence conservative treatment in Chronic Low Back Pain? A Narrative Review. Retos 2022, 46, 395–403. [Google Scholar] [CrossRef]
- Pinto, E.M.; Neves, J.R.; Laranjeira, M.; Reis, J. The importance of inflammatory biomarkers in non-specific acute and chronic low back pain: A systematic review. Eur. Spine J. 2023, 32, 3230–3244. [Google Scholar] [CrossRef]

| n | 149 | |
|---|---|---|
| Turn | Afternoon | 58 (38.9%) |
| Morning | 91 (61.1%) | |
| Age | 60 [50, 69] | |
| Leveled age | Young | 17 (11.4%) |
| Middle age | 84 (56.4%) | |
| Older | 48 (32.2%) | |
| Gender | Female | 117 (78.5%) |
| Male | 32 (21.5%) | |
| Non-specific neck pain/Low back pain | Non-specific neck pain | 28 (18.8%) |
| Non-specific low back | 69 (46.3%) | |
| Non-specific neck and low back pain | 52 (34.9%) | |
| Non-specific dorsal pain | No | 126 (84.6%) |
| Yes | 23 (15.4%) |
| Initial | Final | Difference (Median 95% CI) | p | r (95% CI) | ||
|---|---|---|---|---|---|---|
| Oswestry | 26 [22, 40] | 18 [10, 30] | 8 (12 [9, 13]) | <0.001 a | 0.759, (0.651, 0.837) | |
| Cohen’s g (95% CI) | ||||||
| 0.025 a | 0.375 (0.167, 0.5) | |||||
| Minimum | - | 72 (59.5%) | ||||
| Moderate | 98 (81%) | 38 (31.4%) | 0.038 a | 0.333 (0.1, 0.5) | ||
| Intense | 17 (14%) | 9 (7.4%) | 0.038 a | 0.333 (0.1, 0.5) | ||
| Disability | 5 (4.1%) | 2 (1.7%) | ||||
| Maximum | 1 (0.8%) | - | ||||
| r (95% CI) | ||||||
| NPRS 10 | 6 [5, 8] | 4 [2, 5] | 2 [2 (2, 3)] | <0.001 a | 0.731 (0.622, 0.812) | |
| Cohen´s g (95% IC) | ||||||
| <0.001 a | 0.411 (0.336, 0.481) | |||||
| Mild | 50 (41.3%) | 94 (77.7%) | <0.001 a | 0.423 (0.3, 0.5), | ||
| Moderate | 34 (28.1%) | 14 (11.6%) | <0.001 a | 0.423 (0.3, 0.5), | ||
| Severe | 37 (30.6%) | 13 (10.7%) | <0.001 a | 0.423 (0.3, 0.5). |
| Initial | Final | Difference (Median 95% CI)] | p | r (95% CI) | ||
|---|---|---|---|---|---|---|
| NDI | 31 [21.5, 44] | 20 [14, 32.5] | 11 [8 (6, 11)] | <0.001 a | 0.658 (0.52, 0.779) | |
| Cohen´s g (95% CI) | ||||||
| 0.008 a | 0.293 (0.18, 0.433)] | |||||
| No disability | - | 1 (1.2%) | ||||
| Mild | - | 21 (26.2%) | ||||
| Moderate | 29 (36.2%) | 26 (32.5%) | 0.01 a | 0.423 (0.25, 0.5) | ||
| Severe | 15 (18.8%) | 13 (16.2%) | ||||
| Complete disability | 36 (45%) | 19 (23.8%) | 0.01 a | 0.423 (0.25, 0.5) | ||
| r (95% CI) | ||||||
| NPRS 10 | 6.5 [5, 7.75] | 4 [3, 5] | 2.5 [3 (2, 3)] | <0.001 | 0.761 (0.641, 0.842) | |
| Cohen´s g | ||||||
| <0.001 a | 0.5 | |||||
| Mild | 31 (38.8%) | 65 (81.2%) | <0.001 a | 0.5 | ||
| Moderate | 27 (33.8%) | 7 (8.8%) | <0.001 a | 0.5 | ||
| Severe | 20 (25%) | 6 (7.5%) | <0.001 a | 0.5 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cuenca-Zaldívar, J.N.; Fernández-Carnero, J.; Sánchez-Romero, E.A.; Álvarez-Gonzalo, V.; Conde-Rodríguez, R.; Rodríguez-Sanz, D.; Calvo-Lobo, C. Effects of a Therapeutic Exercise Protocol for Patients with Chronic Non-Specific Back Pain in Primary Health Care: A Single-Group Retrospective Cohort Study. J. Clin. Med. 2023, 12, 6478. https://doi.org/10.3390/jcm12206478
Cuenca-Zaldívar JN, Fernández-Carnero J, Sánchez-Romero EA, Álvarez-Gonzalo V, Conde-Rodríguez R, Rodríguez-Sanz D, Calvo-Lobo C. Effects of a Therapeutic Exercise Protocol for Patients with Chronic Non-Specific Back Pain in Primary Health Care: A Single-Group Retrospective Cohort Study. Journal of Clinical Medicine. 2023; 12(20):6478. https://doi.org/10.3390/jcm12206478
Chicago/Turabian StyleCuenca-Zaldívar, Juan Nicolás, Josué Fernández-Carnero, Eleuterio A. Sánchez-Romero, Verónica Álvarez-Gonzalo, Rocío Conde-Rodríguez, David Rodríguez-Sanz, and César Calvo-Lobo. 2023. "Effects of a Therapeutic Exercise Protocol for Patients with Chronic Non-Specific Back Pain in Primary Health Care: A Single-Group Retrospective Cohort Study" Journal of Clinical Medicine 12, no. 20: 6478. https://doi.org/10.3390/jcm12206478
APA StyleCuenca-Zaldívar, J. N., Fernández-Carnero, J., Sánchez-Romero, E. A., Álvarez-Gonzalo, V., Conde-Rodríguez, R., Rodríguez-Sanz, D., & Calvo-Lobo, C. (2023). Effects of a Therapeutic Exercise Protocol for Patients with Chronic Non-Specific Back Pain in Primary Health Care: A Single-Group Retrospective Cohort Study. Journal of Clinical Medicine, 12(20), 6478. https://doi.org/10.3390/jcm12206478