The “Woggle” Technique for Venous Access Site Management: An Old Technique for a New Need
Abstract
1. Introduction
2. Materials and Methods
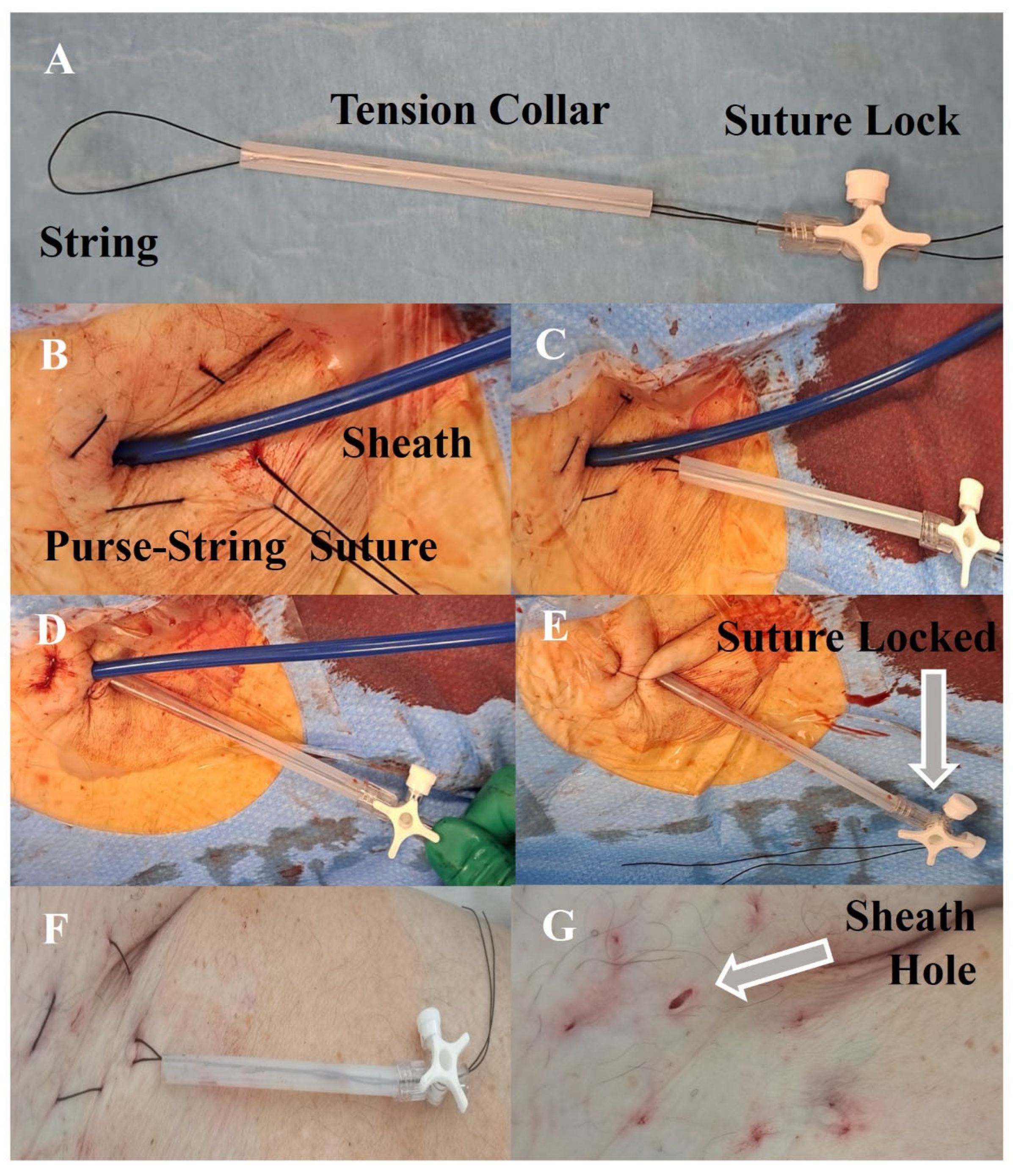
2.1. Technique
2.2. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Van Wiechen, M.P.; Ligthart, J.M.; Van Mieghem, N.M. Large-bore Vascular Closure: New Devices and Techniques. Interv. Cardiol. Rev. 2019, 14, 17–21. [Google Scholar] [CrossRef] [PubMed]
- Akkaya, E.; Soezener, K.; Rixe, J.; Tsiakou, M.; Souretis, G.; Chavakis, E.; Meyners, W.; Tanislav, C.; Gündüz, D.; Erkapic, D. Venous access closure using a purse-string suture without heparin antagonism or additional compression after MitraClip implantation. Catheter. Cardiovasc. Interv. 2020, 96, 179–186. [Google Scholar] [CrossRef]
- Steppich, B.; Stegmüller, F.; Rumpf, P.M.; Pache, J.; Sonne, C.; Lesevic, H.; Braun, D.; Hausleiter, J.; Kasel, A.M.; Ott, I. Vascular Complications after Percutaneous Mitral Valve Repair and Venous Access Closure Using Suture or Closure Device. J. Interv. Cardiol. 2018, 31, 223–229. Available online: https://onlinelibrary.wiley.com/doi/10.1111/joic.12459 (accessed on 30 August 2023). [CrossRef]
- Vesely, T.M. Use of a Purse String Suture to Close a Percutaneous Access Site after Hemodialysis Graft Interventions. J. Vasc. Interv. Radiol. 1998, 9, 447–450. Available online: https://pubmed.ncbi.nlm.nih.gov/9618104/ (accessed on 29 June 2023). [CrossRef] [PubMed]
- Zaleski, G.X.; Funaki, B.; Gentile, L.; Garofalo, R.S. Purse-String Sutures and Miniature Tourniquet to Achieve Immediate Hemostasis of Percutaneous Grafts and Fistulas: A Simple Trick with a Twist. AJR Am. J. Roentgenol. 2000, 175, 1643–1645. Available online: https://pubmed.ncbi.nlm.nih.gov/11090395/ (accessed on 21 July 2023). [CrossRef]
- Clark, T.W.; Haji-Momenian, S.; Kwak, A.; Soulen, M.C.; Stavropoulos, S.W.; Itkin, M.; Patel, A.; Mondschein, J.I.; Trerotola, S.O. Angiographic Changes Following the Use of a Purse-String Suture Hemostasis Device in Hemodialysis Access Interventions. J. Vasc. Interv. Radiol. 2009, 20, 61–65. Available online: https://pubmed.ncbi.nlm.nih.gov/19019702/ (accessed on 4 July 2023). [CrossRef]
- Park, S.J.; Chung, H.H.; Lee, S.H.; Cho, S.B.; Seo, T.S.; Song, M.G. The usefulness and feasibility of placing a clinch knot with a guidewire to achieve temporary hemostasis in arteriovenous dialysis access interventions. J. Vasc. Access 2021, 22, 606–612. [Google Scholar] [CrossRef] [PubMed]
- Ruscica, M.; Ferri, N.; Banach, M.; Sirtori, C.R.; Corsini, A. Side effects of statins: From pathophysiology and epidemiology to diagnostic and therapeutic implications. Cardiovasc. Res. 2023, 118, 3288–3304. [Google Scholar] [CrossRef] [PubMed]
- Levey, A.S.; Stevens, L.A.; Schmid, C.H.; Zhang, Y.; Castro, A.F.; Feldman, H.I.; Kusek, J.W.; Eggers, P.; Van Lente, F.; CKD-EPI (Chronic Kidney Disease Epidemiology Collaboration); et al. A New Equation to Estimate Glomerular Filtration Rate. Ann. Intern. Med. 2009, 150, 604–612. [Google Scholar] [CrossRef] [PubMed]
- Mehran, R.; Rao, S.V.; Bhatt, D.L.; Gibson, C.M.; Caixeta, A.; Eikelboom, J.; Kaul, S.; Wiviott, S.D.; Menon, V.; White, H.; et al. Special Report Standardized Bleeding Definitions for Cardiovascular Clinical Trials a Consensus Report from the Bleeding Academic Research Consortium. Circulation 2011, 123, 2736–2747. Available online: http://circ.ahajournals.org (accessed on 21 July 2023). [CrossRef] [PubMed]
- Casu, G.; Gulizia, M.M.; Molon, G.; Mazzone, P.; Audo, A.; Casolo, G.; Di Lorenzo, E.; Portoghese, M.; Pristipino, C.; Di Bartolomeo, R.; et al. ANMCO/AIAC/SICI-GISE/SIC/SICCH Consensus Document: Percutaneous Occlusion of the Left Atrial Appendage in Non-Valvular Atrial Fibrillation Patients: Indications, Patient Selection, Staff Skills, Organisation, and Training. Eur. Heart J. Suppl. 2017, 19 (Suppl. D), D333–D353. Available online: https://pubmed-ncbi-nlm-nih-gov.bvsp.idm.oclc.org/28751849/ (accessed on 30 August 2023). [CrossRef] [PubMed]
- Pristipino, C.; Sievert, H.; D’Ascenzo, F.; Louis Mas, J.; Meier, B.; Scacciatella, P.; Hildick-Smith, P.; Gaita, F.; Toni, D.; European Association of Percutaneous Cardiovascular Interventions (EAPCI); et al. European Position Paper on the Management of Patients with Patent Foramen Ovale. General Approach and Left Circulation Thromboembolism. Eur. Heart J. 2019, 40, 3182–3195. Available online: https://pubmed-ncbi-nlm-nih-gov.bvsp.idm.oclc.org/30358849/ (accessed on 30 August 2023). [CrossRef] [PubMed]
- Mlekusch, W.; Mlekusch, I.; Sabeti-Sandor, S. Vascular puncture site complications—Diagnosis, therapy, and prognosis. Vasa Eur. J. Vasc. Med. 2016, 45, 461–469. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Akkaya, E.; Berkowitsch, A.; Zaltsberg, S.; Deubner, N.; Greiss, H.; Hain, A.; Hamm, C.W.; Sperzel, J.; Neumann, T.; Kuniss, M. Safety and Feasibility of Percutaneous Skin Closure Using Purse-String Suture Compared with Compression Bandage after Pulmonary Vein Isolation. J. Cardiovasc. Electrophysiol. 2017, 28, 1048–1057. Available online: https://pubmed-ncbi-nlm-nih-gov.bvsp.idm.oclc.org/28608980/ (accessed on 17 September 2023). [CrossRef] [PubMed]
| Clinical Characteristics | (n = 45) |
|---|---|
| Age | 57.6 ± 16.5 |
| Male sex (%) | 28 (62) |
| BMI (Kg/m2) | 20.9 ± 3.8 |
| Hypertension (%) | 21 (46) |
| Active smokers (%) | 4 (9) |
| Hypercholesterolemia (%) | 16 (35) |
| Diabetes (%) | 6 (13) |
| Family history of CAD (%) | 6 (13) |
| Previous stroke (%) | 31 (69) |
| Atrial fibrillation (%) | 14 (31) |
| Dialysis (%) | 5 (11) |
| Previous hemorrhage (%) | 1 (10) |
| Left ventricular ejection fraction (%) | 58 ± 8 |
| Procedural characteristics | |
| LAAO (%) | 15 (33) |
| PFO-c (%) | 30 (66) |
| Success rate (%) | 45 (100) |
| ASA during procedure (%) | 40 (89) |
| DAPT during procedure (%) | 26 (58) |
| French sheath | 11.6 ± 1.2 |
| French sheath 12–14 (%) | 20 (44) |
| Procedural time (min) | 63 ± 35 |
| Heparin (UI/Kg) | 92 ± 22 |
| Woggle technique | |
| Number of releases | 1.04 ± 0.20 |
| Single release (%) | 43 (95) |
| Final time (minutes) | 302–83 |
| Therapy discharge | |
| No antithrombotic therapy | 4 (8.8) |
| SAPT (%) | 4 (8.8) |
| DAPT (%) | 36 (80) |
| DOAC (%) | 1 (2.2) |
| In-hospital outcome | |
| Days of hospitalization after procedure | 2 ± 1.4 |
| In hospital MACE (%) | 0 (0) |
| In-hospital all-cause death (%) | 0 (0) |
| Bleeding (BARC > 2) (%) | 0 (0) |
| Bleeding requiring action (%) | 0 (0) |
| Transfusion (%) | 1 (2) |
| Local hematoma (%) | 1 (2) |
| Biochemistry | Pre Procedure | Post Procedure | p-Value |
|---|---|---|---|
| Hemoglobin (g/dL) | 12.8 ± 2.2 | 12.4 ± 2.1 | 0.01 |
| Serum creatinine (mg/dL) | 1.47 ± 1.69 | 1.69 ± 2.17 | ns |
| Sheath | 8–11 F | 12–14 F | p-Value |
|---|---|---|---|
| n | 25 | 20 | |
| Hematoma (%) | 1 (4) | 0 | ns |
| DAPT during procedure (%) | 18 (72) | 8 (40) | 0.03 |
| Delta hemoglobin (g/dL) | −0.4 [0.8] | −0.55 [1.0] | ns |
| Clinical Characteristics | Pre Procedure | Post Procedure | p-Value |
|---|---|---|---|
| Sheath 8–11 hemoglobin | 13.8 [3.05] | 13.6 [3.0] | ns |
| Sheath 12–14 hemoglobin | 12.6 [4.75] | 11.7 [4.4] | 0.039 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tumminello, G.; Barbieri, L.; Avallone, C.; Bellissimo, N.; Mircoli, L.; Colombo, F.; Vicenzi, M.; Ruscica, M.; Carugo, S. The “Woggle” Technique for Venous Access Site Management: An Old Technique for a New Need. J. Clin. Med. 2023, 12, 6087. https://doi.org/10.3390/jcm12186087
Tumminello G, Barbieri L, Avallone C, Bellissimo N, Mircoli L, Colombo F, Vicenzi M, Ruscica M, Carugo S. The “Woggle” Technique for Venous Access Site Management: An Old Technique for a New Need. Journal of Clinical Medicine. 2023; 12(18):6087. https://doi.org/10.3390/jcm12186087
Chicago/Turabian StyleTumminello, Gabriele, Lucia Barbieri, Carlo Avallone, Nello Bellissimo, Luca Mircoli, Federico Colombo, Marco Vicenzi, Massimiliano Ruscica, and Stefano Carugo. 2023. "The “Woggle” Technique for Venous Access Site Management: An Old Technique for a New Need" Journal of Clinical Medicine 12, no. 18: 6087. https://doi.org/10.3390/jcm12186087
APA StyleTumminello, G., Barbieri, L., Avallone, C., Bellissimo, N., Mircoli, L., Colombo, F., Vicenzi, M., Ruscica, M., & Carugo, S. (2023). The “Woggle” Technique for Venous Access Site Management: An Old Technique for a New Need. Journal of Clinical Medicine, 12(18), 6087. https://doi.org/10.3390/jcm12186087








