Bleeding Disorders and Dental Implants: Review and Clinical Indications
Abstract
1. Introduction
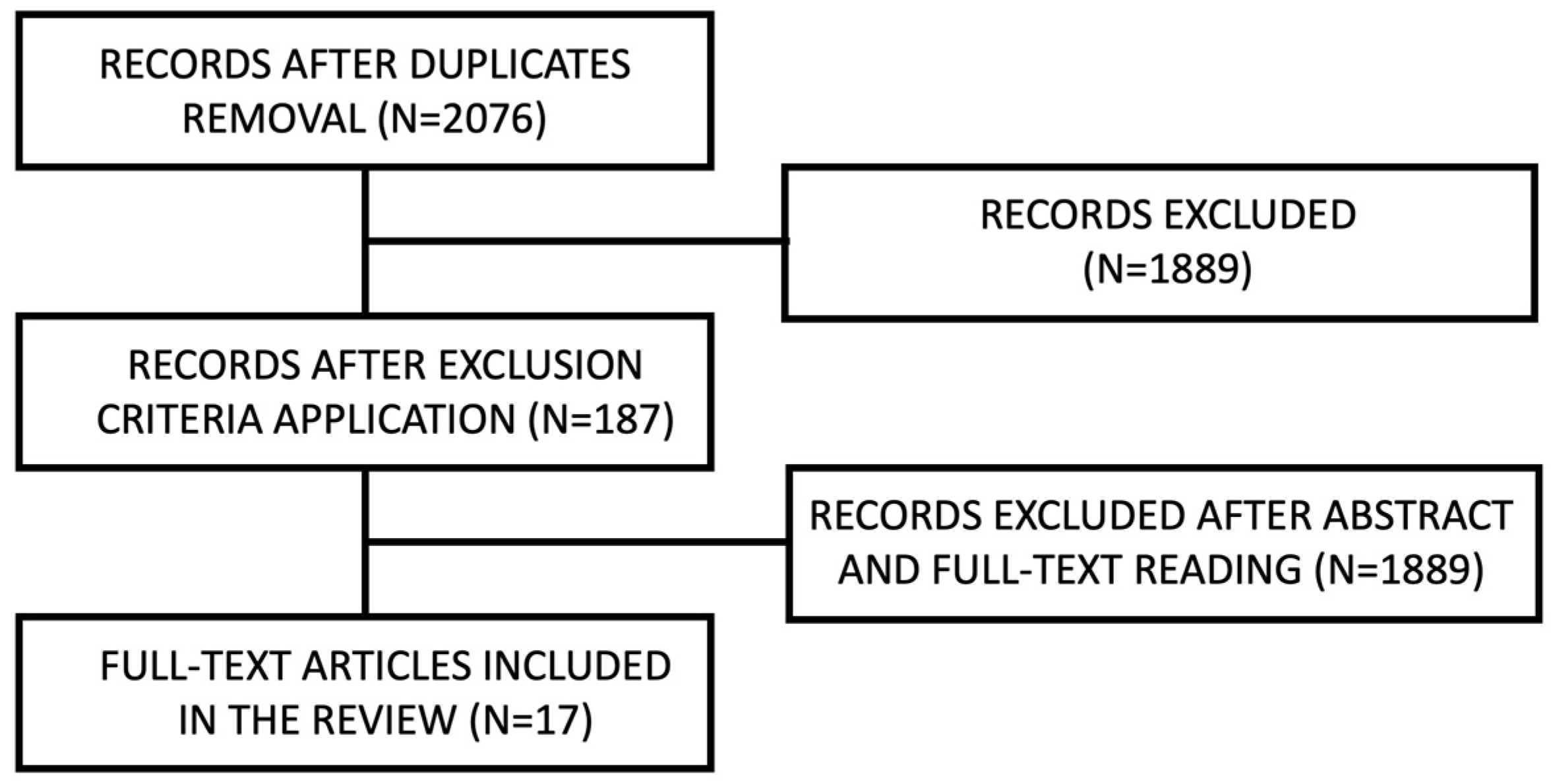
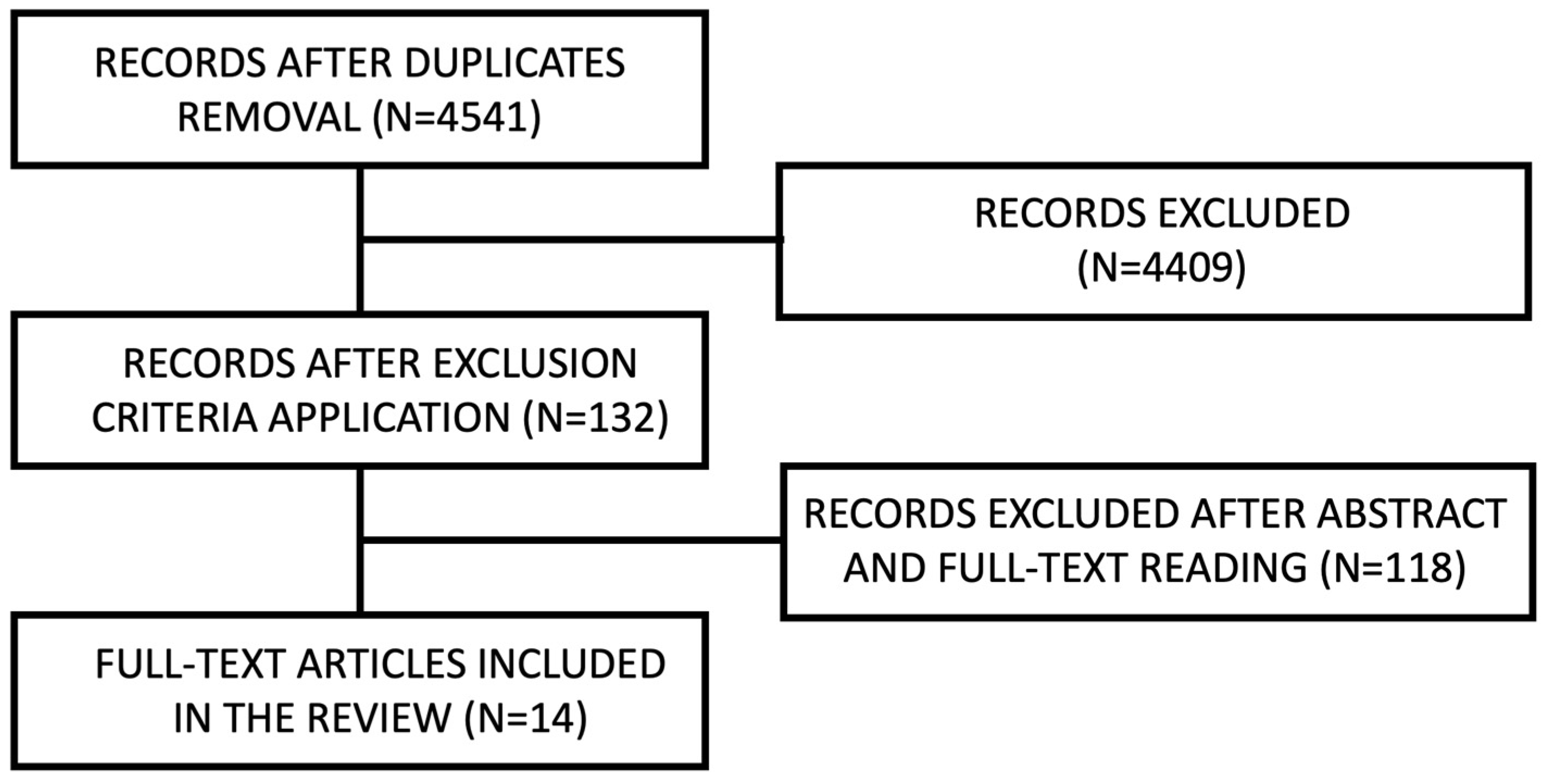
2. Materials and Methods
2.1. Search Strategy
2.2. Inclusion and Exclusion Criteria
3. Results
3.1. Congenital Coagulation Disorders (CCDs)
3.2. Antiplatelet-Induced Bleeding Disorders (APBDs)
3.3. Anticoagulant-Induced Bleeding Disorders (ACBD)
4. Discussion
5. Conclusions
Clinical Importance
- Consulting the physician who treat the patient for their bleeding disorder before implant surgery;
- Almost every study included in the present review suggests administering deficiency factor or desmopressin before the surgery in patients with congenital hemostasis disease;
- Do not withdraw antiaggregative therapy for implant surgery, even if dual; only one study suspended the antiaggregative therapy, but it was due to a concomitant anticoagulant therapy. There is no evidence for the beneficial effect of suspending antiaggregative therapy.
- Do not interrupt therapy with dicumarolics. On the contrary, clinicians should check the INR value before implant surgery and treat any bleeding complications with local hemostatic measures.
- When dealing with direct anticoagulants (DAOC) skip only one dose of the drug, the day before;
- Adopt local hemostatic measures at the end of the procedure and in case of postoperative bleeding: compressive hemostasis with gauze soaked in tranexamic acid showed excellent results in both situations. Regardless of the type of bleeding disorder, all authors agreed in suggesting the application of local hemostatic measures at the end of surgery;
- Instruct the patient about the appropriate post-operative measures: soft and cold diet for 2–3 days, avoiding vigorous rinses, physical effort and the supine position, applying gauze for 5 min in case of bleeding. If these are not enough, repeat the application of the gauze soaked with tranexamic acid. Not all articles reported postoperative instructions, but those that did agree with what is reported here.
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
Appendix A
| Study Type | Underlying Blood Disease | No. of Implants Inserted for Intervention | Flapless | Prophylaxis | Additional Drug Administered after the Procedure | Local Haemostatic Measurements | Bleeding Complications | |
|---|---|---|---|---|---|---|---|---|
| Gornitisky et al., 2005 [16] | Case report | Moderate haemophilia A | 3; 2; 1 | Unspecified | Factor VIII; Tranexamic acid per os | Factor VIII; Tranexamic acid per os | Suture | No |
| Rosen et al., 2005 [15] | Case report | Moderate haemophilia A | 3; 2; 1 | Unspecified | Unspecified | Unspecified | Unspecified | No |
| Neskoromna-Jȩdrzejczak et al., 2018 [17] | Case report | Severe haemophilia B | 2; 2 | No | Recombinant Factor IX | Recombinant Factor IX | Suture | No |
| Castellanos-Cosano et al., 2014 [13] | Case report | Severe haemophilia A; HIV; HCV | 3; 2 | No | Antibiotic; Factor VIII (FVIII), Tranexamic acid per os | Antibiotic; Factor VIII (FVIII), Tranexamic acid per os | Unspecified | No |
| Fénelon et al., 2017 [20] | Case report | Von Willebrand disease | 1 | Yes | Von Willebrand Factor (vWF) | Von Willebrand Factor (vWF); Antibiotic | Suture; fibrin glue | No |
| Kang et al., 2018 [19] | Case report | Von Willebrand disease | 1 | Yes | Desmopressin | none | Unspecified | No |
| Sung-Tak Lee et al., 2018 [23] | Case report | Porpora trombocitopenica idiopatica | 1 | Presumably not | none | none | Unspecified | Severe |
| Calvo-Guirado et al., 2019 [14] | Case report | Severe haemophilia B | 1 | No | Antibiotic; Factor IX; Tranexamic acid per os | Factor IX; Tranexamic acid per os and rinses | Suture; particulate bone graft and collagen membrane soaked in tranexamic acid; compressive hemostasis with gauze soaked in tranexamic acid | No |
| Bacci et al., 2021 [21] | Case report | Von Willebrand disease type 2B | 5 | Yes | Factor VIII + VWF; tranexamic acid | tranexamic acid per os; | Unspecified | No |
| Bacci et al., 2021 [12] | Case report | Mild haemophilia A | 1 | Yes | Factor VIII; tranexamic acid | Unspecified | Unspecified | No |
| Takashima et al., 2021 [22] | Case report | Von Willebrand disease type 1 | 6 | Unspecified | Factor VIII + VWF | Unspecified | Unspecified | Unspecified |
| Kinalsky et al., 2021 [18] | Case report | Haemophilia A | 3; 3 | Yes | Factor VIII; tranexamic acid | no | Suture | Mild |
| Study Type | Antithrombotic Treatment | Discontinuation of the Pharmacological Therapy | No. of Procedures | Post-Operative Bleeding Complications | Management of Complications | |
|---|---|---|---|---|---|---|
| Flanagan et al., 2015 [24] | Case report | Clopidogrel + ASA | No | 1 | 1 | Compressive hemostasis with sponge soaked in tranexamic acid |
| Clemm et al., 2015 [28] | Case–control study | Dicumarols (32)/bridging with LMWH (8)/Dabigatran (6)/Rivaroxaban (8)/Apixaban (2)/Antiaggregants (61) | No | 61 (antiaggregants) | 4 (1 antiaggregant; 2 dicumarols e 1 dicumarols bridged with LMWH) | Compressive hemostasis with gauze soaked in tranexamic acid/Compressive hemostasis with gauze soaked in tranexamic acid + additional suture/revision of the wound and electrocoagulation |
| Tabrizi et al., 2018 [25] | Case-crossover study | Clopidogrel/ASA | Only in the second session of the study | 41 | / | / |
| Rubino et al., 2019 [26] | Retrospective cohort study | ASA/Clopidogrel/Warfarin/DOAC/ASA + clopidogrel /Clopidogrel + warfarin/ASA + clopidogrel + warfarin/ASA + clopidogrel + DOAC/ASA + DOAC/ASA + warfarin + DOAC | Only in 4 cases, after consulting the physician | 218 | 2 (1 in ASA + warfarin; 1 in warfarin) | Cauterization and infiltration with lidocaine |
| Kaura et al., 2021 [27] | Prospective cohort study | Clopidogrel/ASA/Clopidogrel + ASA | No | 65 | 1 (in dual therapy) | / |
| Manor et al., 2021 [29] | Case–control study | Clopidogrel/ASA/DOAC/Warfarin/Combinations | No | 72 (+121 control group) | 4 (1 warfarin + DOAC; 2 Clopidogrel + ASA; 1 warfarin + clopidogrel); + 7 control group | Suture/Suture + Compressive hemostasis with sponge gauze in tranexamic acid |
| Broekema et al., 2021 [30] | Case–control study | Antiaggregants/Dicumarols | No | 8 (+7 control group) | 0 | / |
| Buchbender et al., 2021 [31] | Case–control study | Antiaggregants/Dicumarols/DOACs | No | 95 (+100 control group) | 15 | Compressive hemostasis with gauze soaked in tranexamic acid |
| Study Type | Anticoagulant Therapy | No. of Patients in the Study | No. of implants | Discontinuation of the Pharmacological Therapy | Flapless | Local Hemostatic Measures | Bleeding Complications | Management of Complications | |
|---|---|---|---|---|---|---|---|---|---|
| Ferrieri et al., 2007 [8] | Cohort study | Warfarin | 3 | 7 | No | No | Suture + compressive hemostasis for 30 min with gauzed soaked in saline | No | / |
| Bacci et al., 2011 [48] | Case–control study | Warfarin | 50 | 159 | No | No | Suture + compressive hemostasis with gauze soaked in tranexamic acid for 30–60 min | 2 | Compressive hemostasis with gauze soaked in tranexamic acid for 1 h |
| Miranda et al., 2011 [40] | Case report | Warfarin | 1 | 4 | Bridged with heparin | No | Unspecified | No | / |
| Hong et al., 2012 [43] | Cohort study | Warfarin | 1 | 2 | No | Unspecified | “Poncho” of gingival former soaked with tramexamic acid | 1 | Local hemostatic measures and reinforcement of home care instructions |
| Broekema et al., 2014 [30] | Case–control study | Antiaggregants/Dicumarols | 7 | Unspecified | No | No | Unspecified | 0 | / |
| Clemm et al., 2015 [28] | Case–control study | Dicumarolici (32)/bridging with LMWH (8)/Dabigatran (6)/Rivaroxaban (8)/Apixaban (2)/Antiaggregants (61) | 117 (among them, 61 in therapy with antiaggregants) | Unspecified | No | No | Suture; electrocoagulation | 4 (1 antiaggreganti; 2 dicumarolici e 1 dicumarolici embricato con LMWH) | Compressive hemostasis with gauze soaked in tranexamic acid/Compressive hemostasis with gauze soaked in tranexamic acid + additional suture/revision of the wound and electrocoagulation |
| Gomez-Moreno 2016 [49] | Case–control study | Rivaroxaban | 18 | 43 | No | No | Suture + compressive hemostasis with gauze soaked in tranexamic acid | 1 | Compressive hemostasis with gauze soaked in tranexamic acid |
| Romero-Ruiz et al., 2015 [41] | Case report | Acenocumarolo | 1 | 12 | No | Yes | Unspecified | No | / |
| Gomez-Moreno 2018 [50] | Case–control study | Dabigatran | 29 | 67 | Yes | No | Suture + compressive hemostasis with gauze soaked in tranexamic acid for 30–60 min | 2 | Compressive hemostasis with gauze soaked in tranexamic acid |
| Kim et al., 2018 [23] | Case report | Rivaroxaban | 1 | 2 | Yes | No | Suture + compressive hemostasis for 1 h | Yes (3) | Compressive hemostasis with gauze + applying oxidized regenerated cellulose |
| Okamoto et al., 2018 [45] | Cohort study | Unspecified | 289 | Unspecified | No | Unspecified | Unspecified | 0 | / |
| Gandhi et al., 2019 [42] | Case report | Rivaroxaban (3); Apixaban (1); Dabigatran (1) | 6 | 18 | No | Yes | Unspecified | No | / |
| Rubino et al., 2019 [26] | Cohort study | Antiaggrant/Warfarin/DOAC/combinations | 176 | 218 | Only in 4 cases | Unspecified | Unspecified | 2 (1 in ASA + warfarin; 1 in warfarin) | Local hemostatic measures |
| Kwak et al., 2019 [46] | Cohort study | Dabigatran (3); Rivaroxaban (3); Apixaban (3) | 8 | Unspecified | Yes: for 24 h in 8 cases; 48 h for 1 case | No | Suture + compressive hemostasis for 1 h | 3 | Compressive hemostasis |
| Al Zoman et al., 2013 [39] | Case report | Warfarin | 1 | 1; 1 | No | Yes | Compressive hemostasis | No | / |
| Sannino et al., 2020 [47] | Case–control study | Warfarin (40) e rivaroxaban (40) | 80 | 320 | No | No | Bone wax and spongostan in the extraction site + Compressive hemostasis with gauze soaked in tranexamic acid | Gruppo warfarin: 29 mild, 11 moderate; Gruppo rivaroxavan: 37 mild, 3 moderate | Mild: Compressive hemostasis with gauze; moderate: unspecified |
| Galletti et al., 2020 [44] | Cohort study | Rivaroxaban | 12 | 57 | Yes (for 24 h) | No | Suture + compressive hemostasis for 30 min (+compressive hemostatis with gauze soaked with tranexamic acid for other 30 min if needed) | 3 | Compressive hemostasis with gauze soaked in tranexamic acid (+electrocauterization and additional sutures, if necessary) |
| Manor et al., 2021 [29] | Case–control study | Clopidogrel/ASA/DOAC/Warfarin/Combinations | 72 | Unspecified | No | No | Suture + gelatin sponge + Compressive hemostasis with gauze soaked in tranexamic acid for 20–30 min | 4 (1 warfarin + DOAC; 2 Clopidogrel + ASA; 1 warfarin + clopidogrel); +7 controlli | Suture/suture + compressive hemostasis with gauze soaked in tranexamic acid |
| Buchbender et al., 2021 [21] | Case–control study | Antiaggregants/Dicumarols/DOACs | 95 | Unspecified | no | Unspecified | suture + compressive hemostasis with gauze soaked in tranexamic acid | 1 | Compressive hemostasis with gauze soaked in tranexamic acid |
- Search strings for CCDs
- Search strings for APBDs
- Search strings for ACBDs
References
- Federici, A.B. Classification of Inherited von Willebrand Disease and Implications in Clinical Practice. Thromb. Res. 2009, 124, S2–S6. [Google Scholar] [CrossRef] [PubMed]
- Mazzeffi, M.A.; Stone, M.E. Perioperative Management of von Willebrand Disease: A Review for the Anesthesiologist. J. Clin. Anesth. 2011, 23, 418–426. [Google Scholar] [CrossRef]
- Peyvandi, F.; Garagiola, I.; Young, G. The Past and Future of Haemophilia: Diagnosis, Treatments, and Its Complications. Lancet 2016, 388, 187–197. [Google Scholar] [CrossRef] [PubMed]
- Sacco, R.; Sacco, M.; Carpenedo, M.; Mannucci, P.M. Oral Surgery in Patients on Oral Anticoagulant Therapy: A Randomized Comparison of Different Intensity Targets. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontol. 2007, 104, e18–e21. [Google Scholar] [CrossRef] [PubMed]
- Zimmerman, B.; Valentino, L.A. Hemophilia: In Review. Pediatr. Rev. 2013, 34, 289–295. [Google Scholar] [CrossRef]
- Baron, T.H.; Kamath, P.S.; McBane, R.D. Management of Antithrombotic Therapy in Patients Undergoing Invasive Procedures. N. Engl. J. Med. 2013, 368, 2113–2124. [Google Scholar] [CrossRef]
- Schaefer, J.K.; McBane, R.D.; Wysokinski, W.E. How to Choose Appropriate Direct Oral Anticoagulant for Patient with Nonvalvular Atrial Fibrillation. Ann. Hematol. 2016, 95, 437–449. [Google Scholar] [CrossRef]
- Ferrieri, G.B.; Castiglioni, S.; Carmagnola, D.; Cargnel, M.; Strohmenger, L.; Abati, S. Oral Surgery in Patients on Anticoagulant Treatment Without Therapy Interruption. J. Oral Maxillofac. Surg. 2007, 65, 1149–1154. [Google Scholar] [CrossRef]
- Schulman, S.; Kearon, C.; Kakkar, A.K.; Schellong, S.; Eriksson, H.; Baanstra, D.; Kvamme, A.M.; Friedman, J.; Mismetti, P.; Goldhaber, S.Z. Extended Use of Dabigatran, Warfarin, or Placebo in Venous Thromboembolism. N. Engl. J. Med. 2013, 368, 709–718. [Google Scholar] [CrossRef]
- Szumita, R.P.; Szumita, P.M. (Eds.) Hemostasis in Dentistry; Springer International Publishing: Cham, Switzerland, 2018; ISBN 978-3-319-71239-0. [Google Scholar]
- Sbricoli, L.; Bazzi, E.; Stellini, E.; Bacci, C. Systemic Diseases and Biological Dental Implant Complications: A Narrative Review. Dent. J. 2022, 11, 10. [Google Scholar] [CrossRef]
- Bacci, C.; Cerrato, A.; Zanette, G.; Pasca, S.; Zanon, E. Regenerative Surgery with Dental Implant Rehabilitation in a Haemophiliac Patient. TH Open 2021, 5, e104–e106. [Google Scholar] [CrossRef] [PubMed]
- Castellanos-Cosano, L.; Núñez-Vázquez, R.-J.; Segura-Egea, J.-J.; Torres-Lagares, D.; Corcuera-Flores, J.-R.; Machuca-Portillo, G. Protocol for Oral Implant Rehabilitation in a Hemophilic HIV-Positive Patient With Type C Hepatitis. Implant Dent. 2014, 23, 622–625. [Google Scholar] [CrossRef] [PubMed]
- Calvo-Guirado, J.L.; Romanos, G.E.; Delgado-Ruiz, R.A. Infected Tooth Extraction, Bone Grafting, Immediate Implant Placement and Immediate Temporary Crown Insertion in a Patient with Severe Type-B Hemophilia. BMJ Case Rep. 2019, 12, e229204. [Google Scholar] [CrossRef]
- Rosen, H.; Gornitsky, M. Cementable Implant-Supported Prosthesis, Serial Extraction, and Serial Implant Installation: Case Report. Implant Dent. 2004, 13, 322–327. [Google Scholar] [CrossRef]
- Gornitsky, M.; Hammouda, W.; Rosen, H. Rehabilitation of a Hemophiliac With Implants: A Medical Perspective and Case Report. J. Oral Maxillofac. Surg. 2005, 63, 592–597. [Google Scholar] [CrossRef] [PubMed]
- Neskoromna-Jędrzejczak, A.; Bogusiak, K.; Chojnowski, K.; Robak, M.; Treliński, J. Implantoprosthetic Rehabilitation of a Patient with Severe Form of Hemophilia B: A Case Report. Acta Haematol. Pol. 2018, 49, 33–36. [Google Scholar] [CrossRef]
- De Azevedo Kinalski, M.; Brondani, L.P.; De Mattos Carpena, A.L.M.; Dos Santos, M.B.F. Delayed Bleeding in a Hemophilic Patient After Sinus Floor Elevation and Multiple Implant Placements: A Case Report. J. Oral Implantol. 2022, 48, 133–138. [Google Scholar] [CrossRef]
- Kang, M.; Kang, P. Dental Implant Therapy on a Patient With von Willebrand Disease: A Case Study. Implant Dent. 2018, 27, 599–601. [Google Scholar] [CrossRef]
- Fénelon, M.; Castet, S.; Fricain, J.-C.; Catros, S. Guided Implant Surgery to Reduce Morbidity in Von Willebrand Disease Patients: A Case Report. Open Dent. J. 2018, 12, 80–86. [Google Scholar] [CrossRef]
- Bacci, C.; Cerrato, A.; Zanette, G.; Pampaloni, L.; Grigoletto, A.; Zanon, E. Riabilitazione Implantare Nel Morbo Di Von Willebrand: Un Caso Resistente Alla Desmopressina. Dent. Cadmos 2021, 89, 632. [Google Scholar] [CrossRef]
- Takashima, H.; Sato (Boku), A.; Miyamoro, H.; Kato, S.; Furuno, S.; Shibuya, Y. Perioperative Management of von Willebrand Patients at the Time of Implant Placement: Case Report. Clin. Case Rep. 2021, 9, e04755. [Google Scholar] [CrossRef]
- Lee, S.-T.; Kim, J.-W.; Kwon, T.-G. Life-Threating Outcomes after Dental Implantation in Patient with Idiopathic Thrombocytopenic Purpura: A Case Report and Review of Literature. Maxillofac. Plast. Reconstr. Surg. 2018, 40, 39. [Google Scholar] [CrossRef] [PubMed]
- Flanagan, D. Tranexamic Acid Tamponade to Control Postoperative Surgical Hemorrhage. J. Oral Implantol. 2015, 41, e82–e89. [Google Scholar] [CrossRef] [PubMed]
- Tabrizi, R.; Khaheshi, I.; Hoseinzadeh, A.; Rezvanpour, B.; Shafie, S. Do Antiplatelet Drugs Increase the Risk of Bleeding After Dental Implant Surgery? A Case-and-Crossover Study. J. Oral Maxillofac. Surg. 2018, 76, 2092–2096. [Google Scholar] [CrossRef]
- Rubino, R.T.; Dawson, D.R.; Kryscio, R.J.; Al-Sabbagh, M.; Miller, C.S. Postoperative Bleeding Associated with Antiplatelet and Anticoagulant Drugs: A Retrospective Study. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2019, 128, 243–249. [Google Scholar] [CrossRef] [PubMed]
- Kaura, S.; Rai, R.; Satia, G.; Budhiraja, N.; Mohan, B. Assessment of Bleeding in Patients on Antiplatelets Undergoing Dental Implants. J. Maxillofac. Oral Surg. 2022, 21, 260–264. [Google Scholar] [CrossRef]
- Clemm, R.; Neukam, F.W.; Rusche, B.; Bauersachs, A.; Musazada, S.; Schmitt, C.M. Management of Anticoagulated Patients in Implant Therapy: A Clinical Comparative Study. Clin. Oral Implants Res. 2016, 27, 1274–1282. [Google Scholar] [CrossRef] [PubMed]
- Manor, Y.; Peleg, O.; Mijiritsky, E.; Manor, A.; Reiter, S. A Retrospective Analysis of Dental Implantation under Anticoagulant Treatment. Clin. Oral Investig. 2021, 25, 1001–1009. [Google Scholar] [CrossRef]
- Broekema, F.I.; Van Minnen, B.; Jansma, J.; Bos, R.R.M. Risk of Bleeding after Dentoalveolar Surgery in Patients Taking Anticoagulants. Br. J. Oral Maxillofac. Surg. 2014, 52, e15–e19. [Google Scholar] [CrossRef]
- Buchbender, M.; Schlee, N.; Kesting, M.R.; Grimm, J.; Fehlhofer, J.; Rau, A. A Prospective Comparative Study to Assess the Risk of Postoperative Bleeding after Dental Surgery While on Medication with Direct Oral Anticoagulants, Antiplatelet Agents, or Vitamin K Antagonists. BMC Oral Health 2021, 21, 504. [Google Scholar] [CrossRef]
- Lillis, T.; Veis, A.; Sakellaridis, N.; Tsirlis, A.; Dailiana, Z. Effect of Clopidogrel in Bone Healing-Experimental Study in Rabbits. World J. Orthop. 2019, 10, 434–445. [Google Scholar] [CrossRef] [PubMed]
- Lupepsa, A.C.; Vargas-Sanchez, P.; Moro, M.G.; Mecca, L.E.A.; Claudino, M.; Soares, P.B.F.; Fischborn, A.R.; Andreis, J.D.; Franco, G.C.N. Effects of Low-Dose Aspirin on the Osseointegration Process in Rats. Int. J. Implant Dent. 2021, 7, 3. [Google Scholar] [CrossRef] [PubMed]
- Bajkin, B.V.; Wahl, M.J.; Miller, C.S. Dental Implant Surgery and Risk of Bleeding in Patients on Antithrombotic Medications: A Review of the Literature. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2020, 130, 522–532. [Google Scholar] [CrossRef]
- Miziara, L.N.B.; Sendyk, W.R.; Ortega, K.L.; Gallottini, M.; Sendyk, D.I.; Martins, F. Risk of Bleeding during Implant Surgery in Patients Taking Antithrombotics: A Systematic Review. Semin. Thromb. Hemost. 2021, 47, 702–708. [Google Scholar] [CrossRef] [PubMed]
- Cervino, G.; Fiorillo, L.; Monte, I.P.; De Stefano, R.; Laino, L.; Crimi, S.; Bianchi, A.; Herford, A.S.; Biondi, A.; Cicciù, M. Advances in Antiplatelet Therapy for Dentofacial Surgery Patients: Focus on Past and Present Strategies. Materials 2019, 12, 1524. [Google Scholar] [CrossRef] [PubMed]
- Apostu, D.; Lucaciu, O.; Lucaciu, G.D.O.; Crisan, B.; Crisan, L.; Baciut, M.; Onisor, F.; Baciut, G.; Câmpian, R.S.; Bran, S. Systemic Drugs That Influence Titanium Implant Osseointegration. Drug Metab. Rev. 2017, 49, 92–104. [Google Scholar] [CrossRef]
- Kim, C.; Dam, C.; Jeong, J.; Kwak, E.-J.; Park, W. Delayed Bleeding after Implant Surgery in Patients Taking Novel Oral Anticoagulants: A Case Report. J. Dent. Anesth. Pain Med. 2017, 17, 143. [Google Scholar] [CrossRef]
- Zoman, H.A.; Jetaily, S.A.; Robert, A.A.; Baskaradoss, J.K.; Al-Suwyed, A.; Ciancio, S.; Mubarak, S.A. Flapless Dental Implant Surgery for Patients on Oral Anticoagulants—The “WarLess Procedure”: A Report of 2 Cases. J. Oral Implantol. 2013, 39, 264–270. [Google Scholar] [CrossRef]
- Miranda, M. Implant Surgery and Oral Anticoagulant Therapy: Case Report. Oral Implantol. 2014, 7, 51. [Google Scholar] [CrossRef]
- Romero-Ruiz, M.; Mosquera-Perez, R.; Gutierrez-Perez, J.; Torres-Lagares, D. Flapless Implant Surgery: A Review of the Literature and 3 Case Reports. J. Clin. Exp. Dent. 2015, 7, e146–e152. [Google Scholar] [CrossRef]
- Gandhi, Y.; Bhatavdekar, N. MIDAS (Minimally Invasive Drilling And Styptic) Protocol—A Modified Approach to Treating Patients under Therapeutic Anticoagulants. J. Oral Biol. Craniofacial Res. 2019, 9, 208–211. [Google Scholar] [CrossRef]
- Hong, C.; Napenas, J.J.; Brennan, M.; Furney, S.; Lockhart, P. Risk of Postoperative Bleeding after Dental Procedures in Patients on Warfarin: A Retrospective Study. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2012, 114, 464–468. [Google Scholar] [CrossRef]
- Galletti, G.; Alfonsi, F.; Raffaele, A.; Valente, N.A.; Chatelain, S.; Kolerman, R.; Cinquini, C.; Romeggio, S.; Iezzi, G.; Barone, A. Implant Placement in Patients under Treatment with Rivaroxaban: A Retrospective Clinical Study. Int. J. Environ. Res. Public Health 2020, 17, 4607. [Google Scholar] [CrossRef] [PubMed]
- Okamoto, T.; Hoshi, K.; Fukada, K.; Kataoka, T.; Kumasaka, A.; Kaibuchi, N.; Fukuzawa, S.; Ando, T. Factors Affecting the Occurrence of Complications in the Early Stages After Dental Implant Placement: A Retrospective Cohort Study. Implant Dent. 2018, 27, 221–225. [Google Scholar] [CrossRef] [PubMed]
- Kwak, E.-J.; Nam, S.; Park, K.; Kim, S.; Huh, J.; Park, W. Bleeding Related to Dental Treatment in Patients Taking Novel Oral Anticoagulants (NOACs): A Retrospective Study. Clin. Oral Investig. 2019, 23, 477–484. [Google Scholar] [CrossRef] [PubMed]
- Sannino, G.; Capparé, P.; Montemezzi, P.; Alfieri, O.; Pantaleo, G.; Gherlone, E. Postoperative Bleeding in Patients Taking Oral Anticoagulation Therapy after “All-on-Four” Rehabilitation: A Case-Control Study. Int. J. Oral Implantol. Berl. Ger. 2020, 13, 77–87. [Google Scholar]
- Bacci, C.; Berengo, M.; Favero, L.; Zanon, E. Safety of Dental Implant Surgery in Patients Undergoing Anticoagulation Therapy: A Prospective Case-Control Study: Dental Implant Therapy in Anticoagulated Patients. Clin. Oral Implants Res. 2011, 22, 151–156. [Google Scholar] [CrossRef]
- Gómez-Moreno, G.; Aguilar-Salvatierra, A.; Fernández-Cejas, E.; Delgado-Ruiz, R.A.; Markovic, A.; Calvo-Guirado, J.L. Dental Implant Surgery in Patients in Treatment with the Anticoagulant Oral Rivaroxaban. Clin. Oral Implants Res. 2016, 27, 730–733. [Google Scholar] [CrossRef]
- Gómez-Moreno, G.; Fernández-Cejas, E.; Aguilar-Salvatierra, A.; De Carlos, F.; Delgado-Ruiz, R.A.; Calvo-Guirado, J.L. Dental Implant Surgery in Patients in Treatment by Dabigatran. Clin. Oral Implants Res. 2018, 29, 644–648. [Google Scholar] [CrossRef]
- Madrid, C.; Sanz, M. What Influence Do Anticoagulants Have on Oral Implant Therapy? A Systematic Review. Clin. Oral Implants Res. 2009, 20, 96–106. [Google Scholar] [CrossRef]
- Sivolella, S.; De Biagi, M.; Brunello, G.; Berengo, M.; Pengo, V. Managing Dentoalveolar Surgical Procedures in Patients Taking New Oral Anticoagulants. Odontology 2015, 103, 258–263. [Google Scholar] [CrossRef] [PubMed]
- Pirlog, C.D.; Pirlog, A.M.; Maghiar, T. A Systematic Review of Hemorrhage Risk in Patients on the New Oral Anticoagulant Therapy Postdental Implant Placement. World J. Dent. 2019, 10, 154–157. [Google Scholar] [CrossRef]
- Fortier, K.; Shroff, D.; Reebye, U.N. Review: An Overview and Analysis of Novel Oral Anticoagulants and Their Dental Implications. Gerodontology 2018, 35, 78–86. [Google Scholar] [CrossRef] [PubMed]
- Shi, Q.; Xu, J.; Zhang, T.; Zhang, B.; Liu, H. Post-Operative Bleeding Risk in Dental Surgery for Patients on Oral Anticoagulant Therapy: A Meta-Analysis of Observational Studies. Front. Pharmacol. 2017, 8, 58. [Google Scholar] [CrossRef]
- Donos, N.; Calciolari, E. Dental Implants in Patients Affected by Systemic Diseases. Br. Dent. J. 2014, 217, 425–430. [Google Scholar] [CrossRef] [PubMed]
- Diz, P.; Scully, C.; Sanz, M. Dental Implants in the Medically Compromised Patient. J. Dent. 2013, 41, 195–206. [Google Scholar] [CrossRef] [PubMed]
- Hewson, I.; Daly, J.; Hallett, K.; Liberali, S.; Scott, C.; Spaile, G.; Widmer, R.; Winters, J. Consensus Statement by Hospital Based Dentists Providing Dental Treatment for Patients with Inherited Bleeding Disorders*: Dental Care for Inherited Bleeding Disorder Patients. Aust. Dent. J. 2011, 56, 221–226. [Google Scholar] [CrossRef]
- Hwang, D.; Wang, H.-L. Medical Contraindications to Implant Therapy: Part I: Absolute Contraindications. Implant Dent. 2006, 15, 353–360. [Google Scholar] [CrossRef]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bacci, C.; Schiazzano, C.; Zanon, E.; Stellini, E.; Sbricoli, L. Bleeding Disorders and Dental Implants: Review and Clinical Indications. J. Clin. Med. 2023, 12, 4757. https://doi.org/10.3390/jcm12144757
Bacci C, Schiazzano C, Zanon E, Stellini E, Sbricoli L. Bleeding Disorders and Dental Implants: Review and Clinical Indications. Journal of Clinical Medicine. 2023; 12(14):4757. https://doi.org/10.3390/jcm12144757
Chicago/Turabian StyleBacci, Christian, Claudia Schiazzano, Ezio Zanon, Edoardo Stellini, and Luca Sbricoli. 2023. "Bleeding Disorders and Dental Implants: Review and Clinical Indications" Journal of Clinical Medicine 12, no. 14: 4757. https://doi.org/10.3390/jcm12144757
APA StyleBacci, C., Schiazzano, C., Zanon, E., Stellini, E., & Sbricoli, L. (2023). Bleeding Disorders and Dental Implants: Review and Clinical Indications. Journal of Clinical Medicine, 12(14), 4757. https://doi.org/10.3390/jcm12144757







