Mobile Solutions for Clinical Surveillance and Evaluation in Infancy—General Movement Apps
Abstract
1. Introduction
How It All Came about—From Prechtl’s First Observations of General Movements at the Bench Side to the Use of Smartphone Recordings
2. Materials and Methods
Search Engines, Inclusion Criteria, Paper Extraction, and Selection
3. Results


4. Discussion
4.1. From Different Parts of the World to a Global Endeavour and a Joint Goal
4.2. User Experience
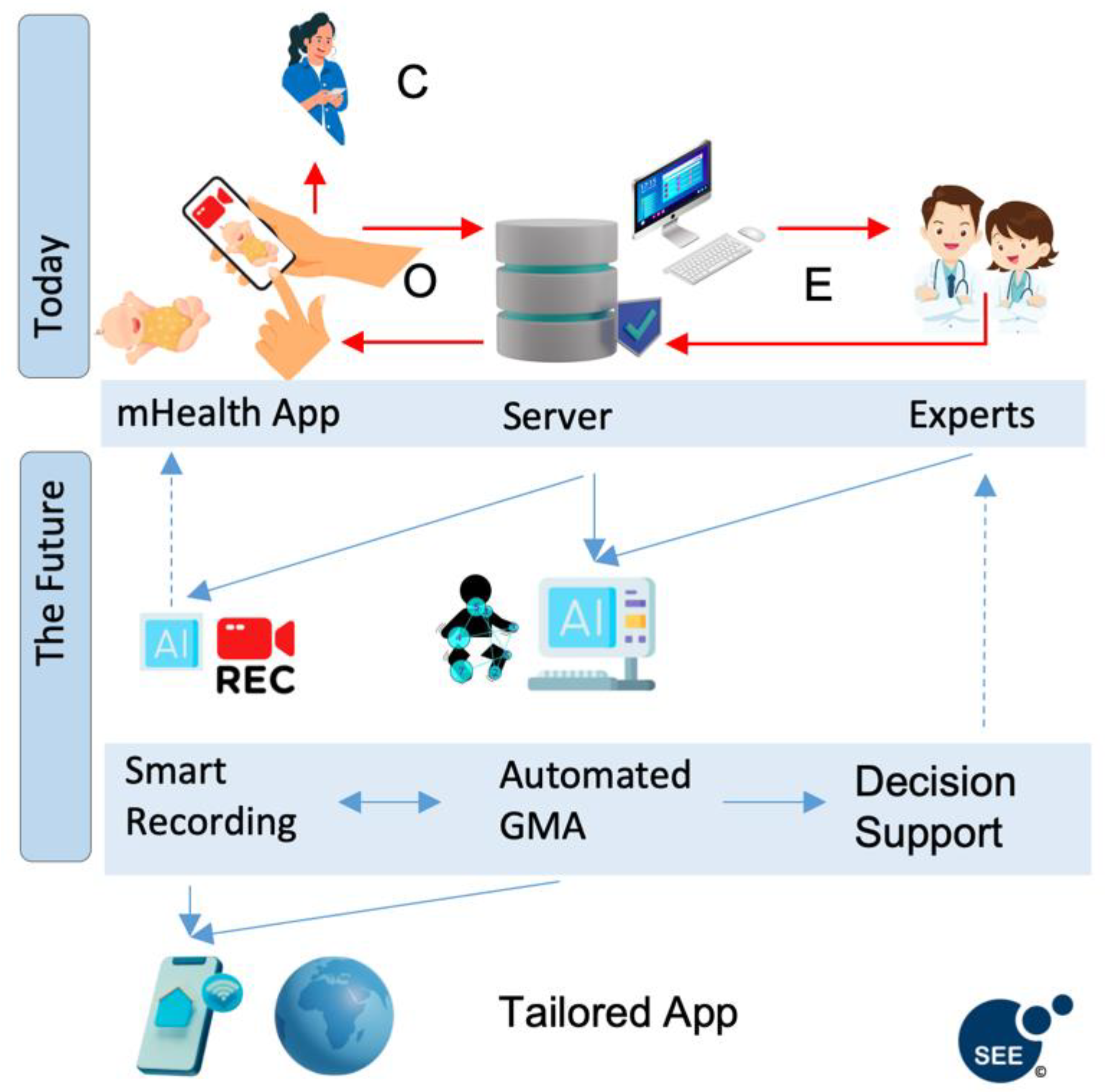
4.3. Challenges and Future Directions
4.4. What Have We Learned?
- -
- Smartphone apps for recording infant motor functions can be successfully used by most parents and healthcare providers.
- -
- Lower maternal education, limited language skills, and reliance on government financial support were related to poorer engagement.
- -
- The reliability of GMA was assessed using traditional GM methodology and smartphone applications.
- -
- The use of smartphone apps has enabled the collection of large data sets in research trials across varied clinical/diagnostic populations.
4.5. Considerations for the Future
- -
- Collaboration to reduce duplication and progress the field;
- -
- Apps that can be altered to the local context;
- -
- Ethical regulations;
- -
- Data protection guidelines;
- -
- Continuous software updating;
- -
- Sustainable IT structures and privacy preserving ML/AI capabilities;
- -
- Involvement of specialised organisations (e.g., GM Trust, CP Alliance).
4.6. How Would Heinz Prechtl Comment on These Developments?
5. Conclusions
Author Contributions
Funding
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Prechtl, H.F. Qualitative changes of spontaneous movements in fetus and preterm infant are a marker of neurological dysfunction. Early Hum. Dev. 1990, 23, 151–158. [Google Scholar] [CrossRef]
- Prechtl, H.F.R.; Einspieler, C.; Cioni, G.; Bos, A.F.; Ferrari, F.; Sontheimer, D. An early marker for neurological deficits after perinatal brain lesions. Lancet 1997, 349, 1361–1363. [Google Scholar] [CrossRef]
- Einspieler, C.; Prechtl, H.; Bos, A.; Ferrari, F.; Cioni, G. Prechtl’s Method on the Qualitative Assessment of General Movements in Preterm, Term and Young Infants; Mac Keith Press: London, UK, 2004. [Google Scholar]
- Einspieler, C.; Marschik, P.B.; Prechtl, H.F.R. Human motor behavior. Z. Für Psychol./J. Psychol. 2008, 216, 147–153. [Google Scholar] [CrossRef]
- Einspieler, C.; Prayer, D.; Marschik, P.B. Fetal movements: The origin of human behaviour. Dev. Med. Child Neurol. 2021, 63, 1142–1148. [Google Scholar] [CrossRef]
- Einspieler, C.; Prechtl, H.F.R. Prechtl’s assessment of general movements: A diagnostic tool for the functional assessment of the young nervous system. Ment. Retard. Dev. Disabil. Res. Rev. 2005, 11, 61–67. [Google Scholar] [CrossRef] [PubMed]
- Einspieler, C.; Peharz, R.; Marschik, P.B. Fidgety movements-tiny in appearance, but huge in impact. J. Pediatr. (Rio J.) 2016, 92, S64–S70. [Google Scholar] [CrossRef]
- Bölte, S.; Neufeld, J.; Marschik, P.B.; Williams, Z.J.; Gallagher, L.; Lai, M.C. Sex and gender in neurodevelopmental conditions. Nat. Rev. Neurol. 2023, 19, 136–159. [Google Scholar] [CrossRef] [PubMed]
- Einspieler, C.; Utsch, F.; Brasil, P.; Panvequio Aizawa, C.Y.; Peyton, C.; Hydee Hasue, R.; Francoso Genovesi, F.; Damasceno, L.; Moreira, M.E.; Adachi, K.; et al. Association of infants exposed to prenatal zika virus infection with their clinical, neurologic, and developmental status evaluated via the general movement assessment tool. JAMA Netw. Open 2019, 2, e187235. [Google Scholar] [CrossRef]
- Hadders-Algra, M. Early human motor development: From variation to the ability to vary and adapt. Neurosci. Biobehav. Rev. 2018, 90, 411–427. [Google Scholar] [CrossRef]
- Valentin, T.; Uhl, K.; Einspieler, C. The effectiveness of training in Prechtl’s method on the qualitative assessment of general movements. Early Hum. Dev. 2005, 81, 623–627. [Google Scholar] [CrossRef] [PubMed]
- Einspieler, C.; Prechtl, H.F.; Ferrari, F.; Cioni, G.; Bos, A.F. The qualitative assessment of general movements in preterm, term and young infants—Review of the methodology. Early Hum. Dev. 1997, 50, 47–60. [Google Scholar] [CrossRef]
- Einspieler, C.; Yang, H.; Bartl-Pokorny, K.D.; Chi, X.; Zang, F.F.; Marschik, P.B.; Guzzetta, A.; Ferrari, F.; Bos, A.F.; Cioni, G. Are sporadic fidgety movements as clinically relevant as is their absence? Early Hum. Dev. 2015, 91, 247–252. [Google Scholar] [CrossRef] [PubMed]
- Cioni, G.; Bos, A.F.; Einspieler, C.; Ferrari, F.; Martijn, A.; Paolicelli, P.B.; Rapisardi, G.; Roversi, M.F.; Prechtl, H.F. Early neurological signs in preterm infants with unilateral intraparenchymal echodensity. Neuropediatrics 2000, 31, 240–251. [Google Scholar] [CrossRef] [PubMed]
- Guzzetta, A.; Mercuri, E.; Rapisardi, G.; Ferrari, F.; Roversi, M.F.; Cowan, F.; Rutherford, M.; Paolicelli, P.B.; Einspieler, C.; Boldrini, A.; et al. General movements detect early signs of hemiplegia in term infants with neonatal cerebral infarction. Neuropediatrics 2003, 34, 61–66. [Google Scholar] [CrossRef] [PubMed]
- Peyton, C.; Pascal, A.; Boswell, L.; de Regnier, R.; Fjørtoft, T.; Støen, R.; Adde, L. Inter-observer reliability using the General Movement Assessment is influenced by rater experience. Early Hum. Dev. 2021, 161, 105436. [Google Scholar] [CrossRef]
- Crowle, C.; Galea, C.; Morgan, C.; Novak, I.; Walker, K.; Badawi, N. Inter-observer agreement of the General Movements Assessment with infants following surgery. Early Hum. Dev. 2017, 104, 17–21. [Google Scholar] [CrossRef] [PubMed]
- Fjørtoft, T.; Einspieler, C.; Adde, L.; Strand, L.I. Inter-observer reliability of the “Assessment of Motor Repertoire--3 to 5 Months” based on video recordings of infants. Early Hum. Dev. 2009, 85, 297–302. [Google Scholar] [CrossRef]
- Örtqvist, M.; Marschik, P.B.; Toldo, M.; Zhang, D.; Fajardo-Martinez, V.; Nielsen-Saines, K.; Ådén, U.; Einspieler, C. Reliability of the Motor Optimality Score-Revised: A study of infants at elevated likelihood for adverse neurological outcomes. Acta Paediatr. 2023, 112, 1259–1265. [Google Scholar] [CrossRef]
- Einspieler, C.; Marschik, P.B.; Pansy, J.; Scheuchenegger, A.; Krieber, M.; Yang, H.; Kornacka, M.K.; Rowinska, E.; Soloveichick, M.; Bos, A.F. The general movement optimality score: A detailed assessment of general movements during preterm and term age. Dev. Med. Child Neurol. 2016, 58, 361–368. [Google Scholar] [CrossRef]
- Einspieler, C.; Bos, A.F.; Krieber-Tomantschger, M.; Alvarado, E.; Barbosa, V.M.; Bertoncelli, N.; Burger, M.; Chorna, O.; Del Secco, S.; DeRegnier, R.A.; et al. Cerebral palsy: Early markers of clinical phenotype and functional outcome. J. Clin. Med. 2019, 8, 1616. [Google Scholar] [CrossRef]
- Barbosa, V.M.; Einspieler, C.; Smith, E.; Bos, A.F.; Cioni, G.; Ferrari, F.; Yang, H.; Urlesberger, B.; Marschik, P.B.; Zhang, D. Clinical implications of the General Movement Optimality Score: Beyond the classes of Rasch analysis. J. Clin. Med. 2021, 10, 1069. [Google Scholar] [CrossRef] [PubMed]
- Irshad, M.T.; Nisar, M.A.; Gouverneur, P.; Rapp, M.; Grzegorzek, M. AI approaches towards Prechtl’s assessment of general movements: A systematic literature review. Sensors 2020, 20, 5321. [Google Scholar] [CrossRef] [PubMed]
- Silva, N.; Zhang, D.; Kulvicius, T.; Gail, A.; Barreiros, C.; Lindstaedt, S.; Kraft, M.; Bölte, S.; Poustka, L.; Nielsen-Saines, K.; et al. The future of general movement assessment: The role of computer vision and machine learning—A scoping review. Res. Dev. Disabil. 2021, 110, 103854. [Google Scholar] [CrossRef] [PubMed]
- Reich, S.; Zhang, D.; Kulvicius, T.; Bölte, S.; Nielsen-Saines, K.; Pokorny, F.B.; Peharz, R.; Poustka, L.; Wörgötter, F.; Einspieler, C.; et al. Novel AI driven approach to classify infant motor functions. Sci. Rep. 2021, 11, 9888. [Google Scholar] [CrossRef]
- Tsuji, T.; Nakashima, S.; Hayashi, H.; Soh, Z.; Furui, A.; Shibanoki, T.; Shima, K.; Shimatani, K. Markerless measurement and evaluation of general movements in infants. Sci. Rep. 2020, 10, 1422. [Google Scholar] [CrossRef] [PubMed]
- Kulvicius, T.; Zhang, D.; Nielsen-Saines, K.; Bölte, S.; Kraft, M.; Einspieler, C.; Poustka, L.; Wörgötter, F.; Marschik, P.B. Infant movement classification through pressure distribution analysis-added value for research and clinical implementation. arXiv 2022, arXiv:2208.00884. [Google Scholar]
- Schroeder, A.S.; Hesse, N.; Weinberger, R.; Tacke, U.; Gerstl, L.; Hilgendorff, A.; Heinen, F.; Arens, M.; Dijkstra, L.J.; Pujades Rocamora, S.; et al. General Movement Assessment from videos of computed 3D infant body models is equally effective compared to conventional RGB video rating. Early Hum. Dev. 2020, 144, 104967. [Google Scholar] [CrossRef]
- Groos, D.; Adde, L.; Aubert, S.; Boswell, L.; de Regnier, R.A.; Fjørtoft, T.; Gaebler-Spira, D.; Haukeland, A.; Loennecken, M.; Msall, M.; et al. Development and validation of a deep learning method to predict cerebral palsy from spontaneous movements in infants at high risk. JAMA Netw. Open 2022, 5, e2221325. [Google Scholar] [CrossRef] [PubMed]
- Marchi, V.; Belmonti, V.; Cecchi, F.; Coluccini, M.; Ghirri, P.; Grassi, A.; Sabatini, A.M.; Guzzetta, A. Movement analysis in early infancy: Towards a motion biomarker of age. Early Hum. Dev. 2020, 142, 104942. [Google Scholar] [CrossRef]
- Marcroft, C.; Khan, A.; Embleton, N.D.; Trenell, M.; Plotz, T. Movement recognition technology as a method of assessing spontaneous general movements in high risk infants. Front. Neurol. 2014, 5, 284. [Google Scholar] [CrossRef] [PubMed]
- Marschik, P.B.; Pokorny, F.B.; Peharz, R.; Zhang, D.; O’Muircheartaigh, J.; Roeyers, H.; Bölte, S.; Spittle, A.J.; Urlesberger, B.; Schuller, B.; et al. A novel way to measure and predict development: A heuristic approach to facilitate the early detection of neurodevelopmental disorders. Curr. Neurol. Neurosci. Rep. 2017, 17, 43. [Google Scholar] [CrossRef] [PubMed]
- Marschik, P.B.; Kulvicius, T.; Flügge, S.; Widmann, C.; Nielsen-Saines, K.; Schulte-Rüther, M.; Hüning, B.; Bölte, S.; Poustka, L.; Sigafoos, J.; et al. Open video data sharing in developmental science and clinical practice. iScience 2023, 26, 106348. [Google Scholar] [CrossRef] [PubMed]
- Orlandi, S.; Raghuram, K.; Smith, C.R.; Mansueto, D.; Church, P.; Shah, V.; Luther, M.; Chau, T. Detection of Atypical and Typical Infant Movements using Computer-based Video Analysis. In Proceedings of the 2018 40th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Honolulu, HI, USA, 18–21 July 2018. [Google Scholar] [CrossRef]
- Adde, L.; Brown, A.; van den Broeck, C.; DeCoen, K.; Eriksen, B.H.; Fjørtoft, T.; Groos, D.; Ihlen, E.A.F.; Osland, S.; Pascal, A.; et al. In-Motion-App for remote General Movement Assessment: A multi-site observational study. BMJ Open 2021, 11, e042147. [Google Scholar] [CrossRef] [PubMed]
- Redd, C.B.; Karunanithi, M.; Boyd, R.N.; Barber, L.A. Technology-assisted quantification of movement to predict infants at high risk of motor disability: A systematic review. Res. Dev. Disabil. 2021, 118, 104071. [Google Scholar] [CrossRef]
- Raghuram, K.; Orlandi, S.; Church, P.; Chau, T.; Uleryk, E.; Pechlivanoglou, P.; Shah, V. Automated movement recognition to predict motor impairment in high-risk infants: A systematic review of diagnostic test accuracy and meta-analysis. Dev. Med. Child Neurol. 2021, 63, 637–648. [Google Scholar] [CrossRef]
- Spittle, A.J.; Olsen, J.; Kwong, A.; Doyle, L.W.; Marschik, P.B.; Einspieler, C.; Cheong, J. The Baby Moves prospective cohort study protocol: Using a smartphone application with the General Movements Assessment to predict neurodevelopmental outcomes at age 2 years for extremely preterm or extremely low birthweight infants. BMJ Open 2016, 6, e013446. [Google Scholar] [CrossRef]
- Svensson, K.A.; Örtqvist, M.; Bos, A.F.; Eliasson, A.C.; Sundelin, H.E. Usability and inter-rater reliability of the NeuroMotion app: A tool in General Movements Assessments. Eur. J. Paediatr. Neurol. 2021, 33, 29–35. [Google Scholar] [CrossRef] [PubMed]
- Kwong, A.K.; Eeles, A.L.; Olsen, J.E.; Cheong, J.L.; Doyle, L.W.; Spittle, A.J. The Baby Moves smartphone app for General Movements Assessment: Engagement amongst extremely preterm and term-born infants in a state-wide geographical study. J. Paediatr. Child Health 2019, 55, 548–554. [Google Scholar] [CrossRef]
- Elliott, C.; Alexander, C.; Salt, A.; Spittle, A.J.; Boyd, R.N.; Badawi, N.; Morgan, C.; Silva, D.; Geelhoed, E.; Ware, R.S.; et al. Early Moves: A protocol for a population-based prospective cohort study to establish general movements as an early biomarker of cognitive impairment in infants. BMJ Open 2021, 11, e041695. [Google Scholar] [CrossRef]
- Peyton, C.; Millman, R.; Rodriguez, S.; Boswell, L.; Naber, M.; Spittle, A.; de Regnier, R.; Barbosa, V.M.; Sukal-Moulton, T. Motor Optimality Scores are significantly lower in a population of high-risk infants than in infants born moderate-late preterm. Early Hum. Dev. 2022, 174, 105684. [Google Scholar] [CrossRef]
- Pouppirt, N.R.; Martin, V.; Pagnotto-Hammitt, L.; Spittle, A.J.; Flibotte, J.; DeMauro, S.B. The General Movements Assessment in neonates with hypoxic ischemic encephalopathy. J. Child Neurol. 2021, 36, 601–609. [Google Scholar] [CrossRef] [PubMed]
- Kwong, A.K.L.; Fitzgerald, T.L.; Doyle, L.W.; Cheong, J.L.Y.; Spittle, A.J. Predictive validity of spontaneous early infant movement for later cerebral palsy: A systematic review. Dev. Med. Child Neurol. 2018, 60, 480–489. [Google Scholar] [CrossRef] [PubMed]
- Kwong, A.K.L.; Boyd, R.; Chatfield, M.; Ware, R.; Colditz, P.; George, J. Early motor repertoire of very preterm infants and relationships with 2-year neurodevelopment. J. Clin. Med. 2022, 11, 1833. [Google Scholar] [CrossRef] [PubMed]
- Kwong, A.K.L.; Doyle, L.; Olsen, J.; Eeles, A.; Lee, K.; Cheong, J.; Spittle, A. Early motor repertoire and neurodevelopment at 2 years in infants born extremely preterm or extremely-low-birthweight. Dev. Med. Child Neurol. 2022, 64, 855–862. [Google Scholar] [CrossRef]
- Luke, C.R.; Benfer, K.; Mick-Ramsamy, L.; Ware, R.S.; Reid, N.; Bos, A.F.; Bosanquet, M.; Boyd, R.N. Early detection of Australian Aboriginal and Torres Strait Islander infants at high risk of adverse neurodevelopmental outcomes at 12 months corrected age: LEAP-CP prospective cohort study protocol. BMJ Open 2022, 12, e053646. [Google Scholar] [CrossRef] [PubMed]
- Passmore, E.; Kwong, A.K.L.; Olsen, J.E.; Eeles, A.L.; Cheong, J.; Spittle, A.; Ball, G. Deep learning for automated pose estimation of infants at home from smart phone videos. Gait Posture 2020, 81, 261–262. [Google Scholar] [CrossRef]
- Rodriguez, S.H.; Blair, M.P.; Timtim, E.; Millman, R.; Si, Z.; Wroblewski, K.; Andrews, B.; Msall, M.E.; Peyton, C. Smartphone application links severity of retinopathy of prematurity to early motor behavior in a cohort of high-risk preterm infants. J. Am. Assoc. Pediatr. Ophthalmol. Strabismus 2023, 27, 12.e11–12.e17. [Google Scholar] [CrossRef]
- Kwong, A.K.L.; Doyle, L.W.; Olsen, J.E.; Eeles, A.L.; Zannino, D.; Mainzer, R.M.; Cheong, J.L.Y.; Spittle, A.J. Parent-recorded videos of infant spontaneous movement: Comparisons at 3-4 months and relationships with 2-year developmental outcomes in extremely preterm, extremely low birthweight and term-born infants. Paediatr. Perinat. Epidemiol. 2022, 36, 673–682. [Google Scholar] [CrossRef]
- Kwong, A.K.L.; Olsen, J.E.; Eeles, A.L.; Einspieler, C.; Lee, K.J.; Doyle, L.W.; Cheong, J.L.Y.; Spittle, A.J. Occurrence of and temporal trends in fidgety general movements in infants born extremely preterm/extremely low birthweight and term-born controls. Early Hum. Dev. 2019, 135, 11–15. [Google Scholar] [CrossRef]
- Buen, C.Ø. Implementation of a Mobileapplication for Diagnosis of Cerebral Palsy [NTNU]. 2016. Available online: https://ntnuopen.ntnu.no/ntnu-xmlui/handle/11250/2404027 (accessed on 15 May 2023).
- Katusiime, J.; Pinkwart, N. A review of privacy and usability issues in mobile health systems: Role of external factors. Health Inform. J. 2019, 25, 935–950. [Google Scholar] [CrossRef]
- Schuller, B.W.; Steidl, S.; Batliner, A.; Marschik, P.B.; Baumeister, H.; Dong, F.; Hantke, S.; Pokorny, F.B.; Rathner, E.; Bartl-Pokorny, K.D.; et al. The INTERSPEECH 2018 computational paralinguistics challenge: Atypical & self-assessed affect, crying & heart beats. In Proceedings of the Interspeech 2018, Hyderabad, India, 2–6 September 2018; pp. 122–126. [Google Scholar]
- Novak, I.; Morgan, C.; Adde, L.; Blackman, J.; Boyd, R.N.; Brunstrom-Hernandez, J.; Cioni, G.; Damiano, D.; Darrah, J.; Eliasson, A.C.; et al. Early, accurate diagnosis and early intervention in cerebral palsy: Advances in diagnosis and treatment. JAMA Pediatr. 2017, 171, 897–907. [Google Scholar] [CrossRef] [PubMed]
- Wu, X.; Xiao, L.; Sun, Y.; Zhang, J.; Ma, T.; He, L. A survey of human-in-the-loop for machine learning. Future Gener. Comput. Syst. 2022, 135, 364–381. [Google Scholar] [CrossRef]
- Wilkinson, M.D.; Dumontier, M.; Aalbersberg, I.J.; Appleton, G.; Axton, M.; Baak, A.; Blomberg, N.; Boiten, J.-W.; da Silva Santos, L.B.; Bourne, P.E.; et al. The FAIR Guiding Principles for scientific data management and stewardship. Sci. Data 2016, 3, 160018. [Google Scholar] [CrossRef] [PubMed]
- Gillan, C.M.; Rutledge, R.B. Smartphones and the neuroscience of mental health. Annu. Rev. Neurosci. 2021, 44, 129–151. [Google Scholar] [CrossRef] [PubMed]
- Einspieler, C.; Marschik, P.B.; Bos, A.F.; Ferrari, F.; Cioni, G. Heinz F. R. Prechtl, 1927–2014 crossing the borders. Dev. Psychobiol. 2014, 56, 1609–1611. [Google Scholar] [CrossRef]
| Authors | App | Study/Article Type | Participants |
|---|---|---|---|
| Spittle et al., 2016 [38] | Baby Moves | Protocol, app description | Extremely preterm infants, term control infants |
| Kwong et al., 2018 [40] | Baby Moves | Prospective cohort | Extremely preterm infants (n = 204), term control infants (n = 212) |
| Elliott et al., 2021 [41] | Baby Moves | Protocol | General population prospective cohort (aim: 3000 infants) |
| Marschik et al., 2017 [32] | GMApp | Protocol, project-related website, app description | Neurotypical cohort, convenience sample of preterm infants (aim: 50 infants longitudinally in biweekly intervals) |
| Svensson et al., 2021 [39] | NeuroMotion | Prospective cohort, app description | Infants at heightened risk for adverse neurological outcome (n = 52; 95 parents) |
| Adde et al., 2021 [35] | In-Motion | Prospective cohort, app description | Infants at high risk for cerebral palsy (n = 86) |
| App/Name | Original App Description | Platform | Users | Reminders/Functionality | Video Upload | Recording Aids |
|---|---|---|---|---|---|---|
| Baby Moves | Spittle et al., 2016 [38] | iOS, Android | Parents | Filming start reminder (push notification) | Server upload to REDCap |
|
| GMApp | Marschik et al., 2017 * [32] | iOS, Android | Healthcare professionals | -Filming start date reminder function -OEOC- feedback loop/video feedback to healthcare providers and caregivers -Case management for the assessment of multiple infants -Statistics and overview about patients | Server upload/cloud system as GMApp has been used in different continents and countries |
|
| NeuroMotion | Svensson et al., 2021 [39] | iOS, Android | Parents | -Filming start date recording reminder (push notification) | Server upload to REDCap |
|
| In-Motion-App | Adde et al., 2021 [35] | iOS, Android | Parents | -One-week prior reminder -Filming start date reminder -Visual recording timeline | Server upload (server at St. Olavs Hospital, Norway) |
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Marschik, P.B.; Kwong, A.K.L.; Silva, N.; Olsen, J.E.; Schulte-Rüther, M.; Bölte, S.; Örtqvist, M.; Eeles, A.; Poustka, L.; Einspieler, C.; et al. Mobile Solutions for Clinical Surveillance and Evaluation in Infancy—General Movement Apps. J. Clin. Med. 2023, 12, 3576. https://doi.org/10.3390/jcm12103576
Marschik PB, Kwong AKL, Silva N, Olsen JE, Schulte-Rüther M, Bölte S, Örtqvist M, Eeles A, Poustka L, Einspieler C, et al. Mobile Solutions for Clinical Surveillance and Evaluation in Infancy—General Movement Apps. Journal of Clinical Medicine. 2023; 12(10):3576. https://doi.org/10.3390/jcm12103576
Chicago/Turabian StyleMarschik, Peter B., Amanda K. L. Kwong, Nelson Silva, Joy E. Olsen, Martin Schulte-Rüther, Sven Bölte, Maria Örtqvist, Abbey Eeles, Luise Poustka, Christa Einspieler, and et al. 2023. "Mobile Solutions for Clinical Surveillance and Evaluation in Infancy—General Movement Apps" Journal of Clinical Medicine 12, no. 10: 3576. https://doi.org/10.3390/jcm12103576
APA StyleMarschik, P. B., Kwong, A. K. L., Silva, N., Olsen, J. E., Schulte-Rüther, M., Bölte, S., Örtqvist, M., Eeles, A., Poustka, L., Einspieler, C., Nielsen-Saines, K., Zhang, D., & Spittle, A. J. (2023). Mobile Solutions for Clinical Surveillance and Evaluation in Infancy—General Movement Apps. Journal of Clinical Medicine, 12(10), 3576. https://doi.org/10.3390/jcm12103576









