Abstract
Although open surgery is the conventional option for ankle arthritis, there are some reports in the literature regarding the use of the arthroscopy procedure with outstanding results. The primary purpose of this systematic review and meta-analysis was to analyze the effect of the surgery technique (open-ankle arthrodesis vs. arthroscopy) in patients with ankle osteoarthritis. Three electronic databases (PubMed, Web of Science, and Scopus) were searched until 10 April 2023. The Cochrane Collaboration’s risk-of-bias tool was used to assess the risk of bias and grading of the recommendations assessment, development, and evaluation system for each outcome. The between-study variance was estimated using a random-effects model. A total of 13 studies (including n = 994 participants) met the inclusion criteria. The meta-analysis results revealed a nom-significant (p = 0.072) odds ratio (OR) of 0.54 (0.28–1.07) for the fusion rate. Regarding operation time, a non-significant difference (p = 0.573) among both surgical techniques was found (mean differences (MD) = 3.40 min [−11.08 to 17.88]). However, hospital length stay and overall complications revealed significant differences (MD = 2.29 days [0.63 to 3.95], p = 0.017 and OR = 0.47 [0.26 to 0.83], p = 0.016), respectively. Our findings showed a non-statistically significant fusion rate. On the other hand, operation time was similar among both surgical techniques, without significant differences. Nevertheless, lower hospital stay was found in patients that were operated on with arthroscopy. Finally, for the outcome of overall complications, the ankle arthroscopy technique was a protective factor in comparison with open surgery.
1. Introduction
Osteoarthritis (OA) is a common degenerative joint disease that affects the cartilage, bone, and surrounding tissues of joints. It is also known as a degenerative joint disease or wear-and-tear osteoarthritis [1,2]. OA can occur in any joint in the body but commonly affects the knees, hips, spine, and hands [3]. The disease is thought to result from not only the aging process but also from biomechanical and biomechanical change stresses affecting the articular cartilage; however, the exact cause of osteoarthritis is not well known. Indeed, several factors contribute to its development, including age [4], genetics [5], joint injury or overuse [6], and obesity [7,8]. Several studies have identified post-traumatic etiology as the principal cause of ankle arthritis [9]. While the management of OA should be individually guided to satisfy the needs of each patient, the surgical option is reserved for more advanced OA patients and/or for patients where early treatment (i.e., patient education, weight management, and assistive devices) fails [10].
According to the definition of terms in medical subject headings, the surgical fixation of a joint by a procedure designated to accomplish the fusion of the joint surface by promoting the proliferation of the bone cell is called arthrodesis. In this regard, open-surgery arthrodesis represents the traditional option for the treatment of ankle osteoarthritis and related pathologies (i.e., chronic instability and degenerative deformity) due to its effect on pain relief and functional improvements [11]. In recent years, however, ankle replacement has gained more consideration, becoming the preferred treatment for this pathology. A meta-analysis found a greater improvement in function and range of motion when compared to ankle arthrodesis [12]. Nonetheless, the complications following lower-extremity open surgery include infections, wound issues, nerve entrapment, and delayed union and non-union, which could represent an important burden for patient quality of life [13]. On the other hand, the ankle arthroscopic technique represents a valid alternative to open surgery for patients with ankle arthrosis. Although open surgery is the traditional option for ankle osteoarthritis, there are some reports in the literature regarding the use of the arthroscopy procedure with outstanding results, including shorter operative time [14] and hospital stay [15], as well as comparable fusion rates between open vs. arthroscopic interventions [16]. For these reasons, there is still an open debate about the adequacy of which surgical technique (i.e., open vs. arthroscopic) yields better responses in patient outcomes.
The choice of surgical approach, whether arthroscopic or open, may depend on a variety of factors, including the surgeon’s preference, the patient’s condition, and the extent of the surgery required [11]. These inconsistencies and gaps in the literature establish a need for a systematic review that, with the highest scientific rigor, shows the effect of two surgery techniques (i.e., open-ankle arthrodesis vs. arthroscopy) on several clinical outcomes. To date, there are several systematic reviews and meta-analyses where this question was addressed [13,17]. However, some of them fail in study research design classification and others in the statistical analysis approach [18], which could lead to misinterpreting the conclusions obtained. Therefore, the primary purpose of this systematic review and meta-analysis was to analyze the effect of the surgery technique (open-ankle arthrodesis vs. arthroscopy) on fusion rate in patients with ankle osteoarthritis. On the other hand, the second objective of this systematic review and meta-analysis was to analyze the effect of the surgery technique on operation time and length of hospital stay. Finally, our review described the overall complications after the use of both surgical techniques described above.
2. Materials and Methods
2.1. Study Design
A systematic review and meta-analysis were developed using the Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) statement guidelines [19]. In addition, the Prisma in Exercise, Rehabilitation, Sport Medicine and Sports Science (PERSiT) was also implemented [20]. The PRISMA checklist is detailed in Supplementary File S1.
2.2. Eligibility Criteria
To be included, studies had to adhere to the following criteria: (1) Type of studies: randomized or non-randomized controlled trial where the effect of the surgery technique was assessed. Only studies in English were considered. Conference abstracts were excluded. (2) Type of participant: studies included patients with osteoarthritis, including post-traumatic osteoarthritis, osteoarthritis, and end-stage osteoarthritis, or patients with ankle instability. (3) Types of interventions: open surgery for the intervention group; meanwhile, arthroscopy was the comparison group. (4) Type of outcome measures: the primary outcome of interest was fusion rate. However, in addition to that variable, operation time and length of hospital stay were collected from studies that provided this information. Finally, overall complications were also collected.
2.3. Search Strategy
A PICO strategy was used to build search criteria for electronic databases (i.e., PubMed, Web of Science, and Scopus). No restrictions were applied concerning the year of publication. The PICO consisted of terms for open-ankle arthrodesis, arthroscopy, fusion rate, and blood loss. The primary search string used for PubMed was: (“open ankle arthrodesis” [All Fields] OR “open ankle” [All Fields] OR “ankle joint/surgery” [MeSH Major Topic]) AND (“arthroscopy” [All Fields] OR “arthroscopy technique” [All Fields] OR “arthrodesis” [All Fields] OR “minimally invasive” [All Fields]) AND (“fusion rate” [All Fields] OR “Visual analogue scale (VAS)” [All Fields] OR “blood loss” [All Fields] OR “American Orthopaedic Foot and Ankle Society (AOFAS)” [All Fields]). The search strings used for other databases were adapted using the Polyglot Search Translator Tool (https://sr-accelerator.com/#/polyglot, accessed on 4 May 2023) [21] and are reported in Supplementary File S2. The final search date was performed on 10 April 2023. Forward and backward citation tracking of articles that met the eligibility criteria was performed using an online tool (citation chaser) [22].
2.4. Methodological Quality and Level of Evidence
Two researchers independently assessed the methodological quality of the studies using a modified version of the Risk of Bias 2 (RoB 2) Cochrane Bias Assessment Tool [23] In the case of disagreement between the scores provided, the primary author made the final decision. RoB 2 was considered in the interpretation of the results by applying the Grading of Recommendations Assessment, Development and Evaluation (GRADE) system. A more extensive description of the risk of bias assessment procedure and the GRADE system is found in Supplementary File S3.
2.5. Data Extraction
The following data were extracted: authors, year of publication, research design (i.e., randomized controlled trial (RCT) and non-randomized controlled trial but intervention study (nRCT)), sample size, sex (i.e., male/female), age (i.e., years), body mass index, fusion rate, follow-up period (i.e., months), hospital stay (i.e., days), and overall complications both arthroscopy and open-surgery groups. Data extraction was manually performed by two researchers. Where data were not available or insufficient information was reported, the corresponding author of the studies was contacted by email, with one reminder after 2 weeks if they did not respond to the first email. If the corresponding authors did not reply, the study was discarded.
2.6. Statistical Analysis
The sample size and means (or events), standard deviation, 95% confidence intervals (CI95%) (if applicable) of fusion rate, complications, hospital stay, and operation time were extracted independently from the included studies. Mean differences (MD) were calculated for hospital stay and operation time since all studies were reported in the same units. We first computed a change score within each group and then determined the difference between the change scores between groups using the following equation:
Finally, the variance of the MD was computed as follows [22]:
where “S2arthr” and “S2open” denote the variance of the change score for the arthroscopy and open-surgery groups, respectively.
On the other hand, for nominal variables (fusion rate and overall complications), odds ratios (ORs) and 95% of confidence intervals were calculated using the following approach [24]:
The ORs were transformed to log-OR using the natural logarithm:
Meanwhile, the standard error of the log-OR was calculated using the formula:
The consistency of the effects found was assessed using the I2 and τ2 tests, with heterogeneity (I2) being considered small (<25%), moderate (25–49%), and high (>50%). In addition, Tau-square tests (τ2) and prediction interval (PI) were included, because τ2 cannot readily point to the clinical implications of the unobserved heterogeneity [25] for ratio variables. The prediction interval allows a better clinical evaluation of the results obtained because it represents the range in which the effect size of a future study conducted on the topic will most likely be. The Egger’s test and a representation of the funnel plot were used to assess small study bias. Variance estimations between studies were calculated using a random-effects model (i.e., Hartung–Knapp/Sidik–Jakman adjustment (HKSJ)) with a 95% confidence interval (CI95%). All statistical analyses were performed using statistical software (R version 4.1.9, R Foundation for Statistical Computing, Austria, metaphor and meta-analysis package, general meta-analysis package; risk-of-bias figures were created using Robvis). The standardized mean difference (SMD) was considered trivial (<0.20), small (0.20–0.59), moderate (0.60–1.19), large (1.20–1.99), and very large (>2.00) [26]. RoB 2 figures were created using the Robvis package [26,27].
3. Results
3.1. Search Results
Figure 1 shows the PRISMA flow diagram with the different phases of the search and selection of studies included in this review. The initial search yielded 394 records. None of the records were removed before screening. After the elimination of duplicates (n = 32), another 343 studies were excluded based on abstract and another 10 studies based on full-text assessment (see Supplementary File S4 for more information regarding excluding studies). A total of 13 studies [11,14,15,16,28,29,30,31,32,33,34,35,36] were therefore included in the present review on the effectiveness of open-ankle arthrodesis vs. arthroscopy on our primary outcome (i.e., fusion rate).
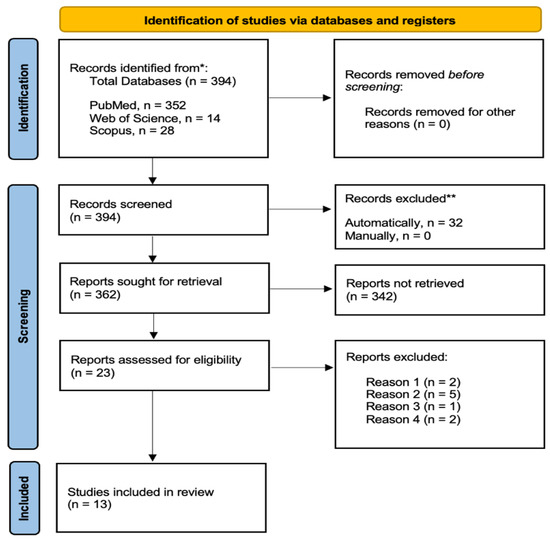
Figure 1.
PRISMA flow diagram of the literature search results. * records removed automatically using an online tool (www.sr-accelerator.com, accessed on 4 May 2023). ** records excluded according by reasons.
3.2. Risk-of-Bias Results
The risk-of-bias scores of included studies are reported in Figure 2 both traffic light and summary plots. A total of 13 studies were analyzed [11,14,15,16,28,29,30,31,32,33,34,35,36]. Figure 2A,B summarizes the risk of bias on fusion rate outcome. From a general point of view, all studies (100%) were at high risk of bias. From the 13 studies analyzed, Domain 1 (randomization procedure) in 13/13 was at high risk of bias, Domain 2 (deviations from the intended intervention) was at high risk of bias in 13/13 (100%), Domain 3 (missing outcome data) was at low risk of bias in 13/13 (100%), Domain 4 (measurement of the outcome) was at low risk of bias in 13/13 (100%), and finally, Domain 5 (selection of the reported results) was 13/13 (100%) at some concerns.
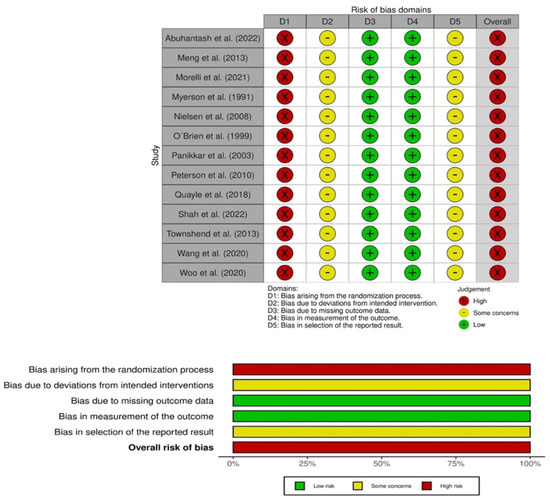
Figure 2.
Risk-of-bias assessment for fusion rate traffic light plot and and summary plot [11,14,15,16,28,29,30,31,32,33,34,35,36].
3.3. Participants Characteristics
The total sample size across all studies was n = 994 participants, where regardless of the operation technique, n = 23 (58%) and n = 383 (42%) were females and males, respectively. In two studies, the sex was not provided; for that reason, the number of participants was 909. The mean and SD of age were 57.68 ± 6.05 and 57.37 ± 6.49 years for arthroscopy and open surgery, respectively. The body mass index corresponded to 28.07 ± 2.56 and 29.31 ± 4.08 for the arthroscopy and open-surgery groups. A complete description of the patient characteristics is summarized in Table 1.

Table 1.
Baseline characteristics of the included studies.
3.4. Fusion Rate
A total of 13 studies yielded a non-significant (p = 0.072) rate of fusion of 0.54 (0.28–1.07) for arthrodesis compared with open surgery, including 540 (54%) and 454 (46%) patients for arthroscopy and open surgery, respectively. The OR score corresponded to 0.54 (0.28–1.07). The amount of heterogeneity was cataloged as low (I2 = 32%) (see Figure 3).
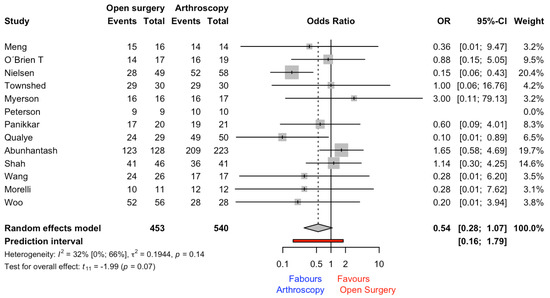
Figure 3.
Forest plot for fusion rate outcome [11,14,15,16,28,29,30,31,32,33,34,35,36].
3.5. Operation Time
This outcome was reported in a total of eight studies; however, only six studies provided the SD to calculate the MD. The meta-analysis results revealed a non-significant (p = 0.573) MD and CI95% of 3.40 min (−11.08 to 17.88) for the open-surgery group. The heterogeneity and prediction interval are shown in Figure 4.
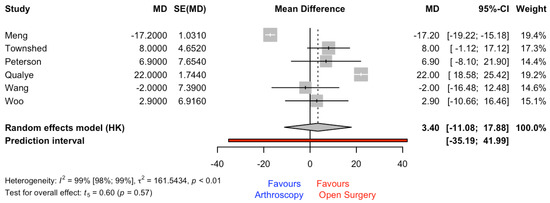
Figure 4.
Forest plot for mean difference (MD) (min) for operation time outcome. SE = standard error [14,15,28,33,35,36].
3.6. Length of Hospital Stay
This outcome was reported in a total of 10 studies; however, only 6 studies provided the SD to calculate the MD. The meta-analysis results revealed a significant (p = 0.017) MD and CI95% of 2.29 days (0.63 to 3.95) for the open-surgery group. The heterogeneity and prediction interval are shown in Figure 5.
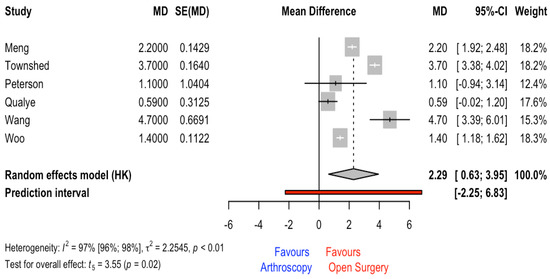
Figure 5.
Forest plot for hospital length stay [14,15,28,33,35,36].
3.7. Post-Operative Overall Complications
A total of 9 studies, including 43 and 66 patients for arthroscopy and open surgery, respectively, reported the number of complications. The meta-analysis results revealed a statistically significant OR and CI95% of 0.40 (0.20 to 0.82) (p = 0.012), favoring the arthroscopy surgical technique. The heterogeneity was low (I2 = 17%) (see Figure 6).
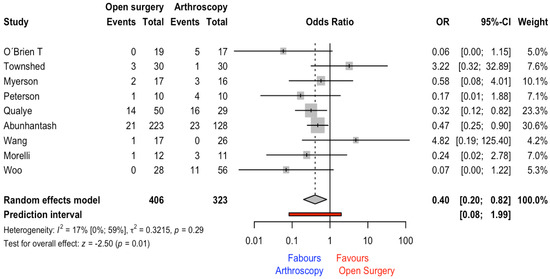
Figure 6.
Forest plot for post-operative complications outcome [11,14,16,28,29,30,33,35,36].
On the one hand, regarding overall complications, the most common complications described were delayed union, wound infection, non-union, deep infection, tibial entrapment, subtalar osteoarthritis, and tarsal tunnel syndrome in the open-surgery group. On the other hand, non-union, malunion, deep infection, and delayed wound healing were reported for the arthroscopy group.
3.8. Heterogeneity Analysis and Publication Bias
Visual analysis of the counter-enhanced funnel plot did not show the presence of publications’ bias fusion rate (A) and overall complications (B) (Figure 7). This was confirmed analyzing Egger’s test for both outcomes (fusion rate intercept = −0.031, CI95% = −1.75 to −1.69, t = −0.036, p = 0.972, and overall complications intercept = −0.046, CI95% = −1.30 to −1.21, t = −0.072, p = 0.944).
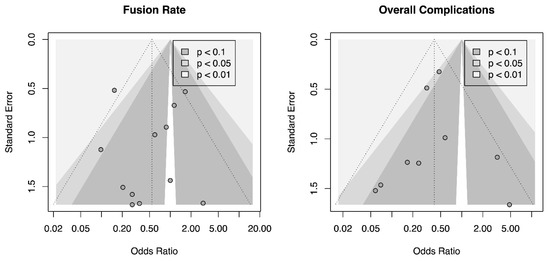
Figure 7.
Counter-enhanced funnel plot for fusion rate and overall complications.
Table 2 summarizes the GRADE evaluation system for the outcomes included in the present systematic review and meta-analysis.

Table 2.
Grading of Recommendations Assessment, Development and Evaluation system (GRADE) on fusion rate, operation time, hospital stay, and overall complications.
4. Discussion
The main aim of this systematic review and meta-analysis was to analyze the effect of the surgery technique (i.e., open surgery vs. arthroscopy) on fusion rate in patients with ankle osteoarthritis. Evidence coming from studies with some concerns or high risk of bias showed that the arthroscopy technique had a non-statistical benefit in comparison to open-ankle surgery. The quality of evidence synthesis was rated as low. On the other hand, when operation time was compared among surgical techniques, the meta-analysis results revealed non-significant differences (3.40 min [11.08 to −17.88]). However, significant differences with an MD of 2.29 days (0.63 to 3.95) favoring the open-surgery group were found. In patients that were operated on with the open-surgery technique, the stance in the hospital was higher in comparison to the arthroscopy group. Finally, regarding overall complications, the meta-analysis results revealed that arthroscopy was a protective factor (OR = 0.47 [0.26 to 0.84]) in comparison with open surgery. In the absence of the homogeneity of studies in the outcomes provided, the preferential use of one of these techniques should be guided by other indicators such as patient characteristics or surgical preferences.
Regarding our primary outcome (i.e., fusion rate), the meta-analysis results revealed that although the arthroscopy surgical technique seems to have acted as a protection factor, no significant differences were found when data were compared with the open-ankle surgery technique. In addition, the GRADE evaluation system cataloged fusion rate and operation time as low and very low overall quality, respectively. This result differs from a recent meta-analysis by Bai et al. [17]. On the one hand, new studies were included in our meta-analysis, such as the study by Abuhantasth et al. [11], where a total of 351 patients were treated (n = 223 for arthroscopy and n = 128 for open surgery). On the other hand, there are several studies that were included in the study of Bai et al. [17], where it was not possible to find the references (impossible to access Chinese electronic databases), which represents a problem of replicability.
Arthroscopy, in comparison with open surgery, requires only small incisions, which means there is less soft-tissue damage and scarring. This can lead to less pain and a faster recovery time. Our results showed that the use of arthroscopy was more beneficial than open surgery (OR = 0.54), but non-significant differences were found in fusion rate (see Figure 3) and in operation time (see Figure 4). It is important to highlight that these results came from studies with high risk of bias in the first domain (i.e., bias arising from the randomization process). It should be considered that, in all studies included in the present systematic review and meta-analysis, the patient division across groups was made according to a specific criterion (i.e., surgeon preferences or other factors). For example, in the study conducted by Woo et al. [36], the decision of which surgical procedure was performed was based on surgeon preference, as well as the study by Abuhantasth et al. [11], which revealed that the surgeon decided on which operation technique to employ on the basis of the anatomy, deformity, and patient comorbidities. These facts could affect the fusion rate and the operation time. The surgeon’s expertise could have an effect on operation time and on fusion rate outcomes.
The total number of complications across groups was 43 and 66 for the arthroscopy and open-surgery groups, respectively. However, when this result was adjusted by the total number of patients, the mean and SD of overall complications were 12% ± 0.08 and 27% ± 0.18 (OR = 0.47, see Figure 6). However, deep infection was reported in both surgical techniques; in this sense, Shah et al. [34] concluded that for patients with a remote history of infection, open-ankle arthrodesis may be preferable.
Based on the primary findings of this study, when the fusion rate outcome was analyzed, there was a beneficial use of the arthroscopy surgical technique in comparison with open surgery. However, it is important to highlight that non-significant differences were found between these surgical techniques. Overall, the use of arthroscopy in ankle arthrodesis can provide several advantages over traditional open surgery, resulting in a faster, less painful recovery with fewer complications. However, as with any surgical procedure, the choice of approach should be made in consultation with the patient’s surgeon, taking into account individual factors such as the patient’s medical history, level of physical activity, and overall health. While arthroscopic ankle arthrodesis offers several advantages over open surgery, there are also some potential disadvantages to consider, for instance, limited visualization; technical difficulty; limited accessibility; risk of complications, such as infection, nerve damage, and blood vessel injury; and limited weight-bearing capacity. However, arthroscopic ankle arthrodesis has demonstrated its advantages, and it is important to highlight that ankle joint replacement is currently the gold standard for ankle osteoarthritis. Ankle arthrodesis is technically less demanding, but patients have limited function. Whereas joint replacement showed better function and range of motion compared with ankle arthrodesis, patient satisfaction showed no difference [12].
There are some limitations in the present systematic review that need to be carefully addressed before interpreting the results obtained. Firstly, there was a large heterogeneity of outcomes across the included studies; meanwhile, some studies included functional scales and pain assessment while other studies did not. The lack of agreement regarding the outcomes assessed creates the necessity for a clinical guideline to be systematic in the outcomes reported. On the other hand, the risk-of-bias analysis of the included studies in this meta-analysis revealed the necessity for studies with a randomization process and an assessor blinded to the patient groups. Finally, arthroscopic ankle arthrodesis is often recommended for well-aligned cases, whereas open fusion is indicated to treat malaligned arthritic ankles. This fact may introduce bias in the interpretation of the results, as the lower complication rate may be attributed to less complex cases and not to the surgical approach itself. In addition, it should be mentioned that the studies do not report on the implants used for fixation, which may also have influenced the results. These major findings could affect the primary outcomes.
5. Conclusions
While both arthroscopic and open surgery can be effective for ankle arthrodesis, the evidence found suggests that arthroscopic surgery may produce similar or even better outcomes with several potential advantages over open surgery (i.e., fewer overall complications). In conclusion, our findings show that studies with some concerns or high risk of bias provided a better but non-statistically significant fusion rate in patients that underwent arthroscopic arthrodesis in comparison with open surgery. The quality of evidence was rated as low. On the other hand, operation time was not different among surgical techniques, although a lower hospital stay was found in patients that were operated on with arthroscopy. Finally, for the outcome of overall complications, the ankle arthroscopy technique was a protective factor in comparison with open surgery. For these reasons, the choice of surgical approach should be based on the careful consideration of the individual patient’s condition and the surgeon’s experience and preference.
Supplementary Materials
The following are available online at https://www.mdpi.com/article/10.3390/jcm12103574/s1, File S1: Prisma Checklist. File S2: Search strings. File S3: Risk of Bias and Grading of Recommendation Assessment, Development and Evaluation system. File S4: Excluded studies with reasons. References [19,37,38,39,40,41,42,43,44,45,46] are cited in Supplementary Materials.
Author Contributions
G.M. is the corresponding author for this article. Contributor roles: conceptualization, A.L., L.P., P.P., I.J.B., G.M., C.B. and R.L.; data curation A.L., L.P., P.P., I.J.B., G.M., C.B. and R.L.; formal analysis, A.L., L.P., P.P., I.J.B., G.M., C.B. and R.L.; investigation, A.L., L.P., P.P., I.J.B., G.M., C.B. and R.L.; methodology, A.L., L.P., P.P., I.J.B., G.M., C.B. and R.L.; project administration, A.L. and R.L.; software, A.L., I.J.B. and G.M.; supervision, R.L.; validation, A.L., L.P., P.P., I.J.B., G.M., C.B. and R.L.; visualization, A.L., L.P., P.P., I.J.B., G.M., C.B. and R.L.; writing original draft, A.L., L.P., P.P., I.J.B., G.M., C.B. and R.L.; writing–review and editing, A.L., L.P., P.P., I.J.B., G.M., C.B. and R.L. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This study is a meta-analysis, and no ethics committee approval is required.
Informed Consent Statement
Not applicable.
Data Availability Statement
All data generated or analyzed during this study are included in this published article (and its Supplementary Materials).
Conflicts of Interest
The authors declare no competing interests.
References
- Khlopas, H.; Khlopas, A.; Samuel, L.T.; Ohliger, E.; Sultan, A.A.; Chughtai, M.; Mont, M.A. Current concepts in osteoarthritis of the ankle. Surg. Technol. Int. 2019, 35, 280–294. [Google Scholar] [PubMed]
- Glazebrook, M.; Daniels, T.; Younger, A.; Foote, C.J.; Penner, M.; Wing, K.; Lau, J.; Leighton, R.; Dunbar, M. Comparison of health-related quality of life between patients with end-stage ankle and hip arthrosis. J. Bone Joint Surg. Am. 2008, 90, 499–505. [Google Scholar] [CrossRef] [PubMed]
- Migliorini, F.; Torsiello, E.; La Padula, G.; Oliva, F.; Maffulli, N. The Association Between Sex and Osteoarthritis in the Physically Active Population: A Systematic Review. Sports Med. Arthrosc. Rev. 2022, 30, 87–91. [Google Scholar] [CrossRef] [PubMed]
- Baal, J.D.; Cecil, K.L.; Patel, R.; O’Brien, M.; McGill, K.; Link, T.M. Imaging of Overuse Injuries of the Hip. Radiol. Clin. North Am. 2023, 61, 191–201. [Google Scholar] [CrossRef]
- Liu, H.; Yan, L.; Li, X.; Li, D.; Wang, G.; Shen, N.-N.; Li, J.J.; Wang, B. MicroRNA expression in osteoarthritis: A meta-analysis. Clin. Exp. Med. 2023. [Google Scholar] [CrossRef]
- Morasiewicz, P.; Dejnek, M.; Kulej, M.; Dragan, S.Ł.; Konieczny, G.; Krawczyk, A.; Urbański, W.; Orzechowski, W.; Dragan, S.F.; Pawik, Ł. Sport and physical activity after ankle arthrodesis with Ilizarov fixation and internal fixation. Adv. Clin. Exp. Med. 2019, 28, 609–614. [Google Scholar] [CrossRef]
- Li, X.; Wang, Y.; Zhang, Y.; Ma, Y.; Pan, F.; Laslett, L.; Cai, G. Longitudinal associations of body mass index and abdominal circumference with back pain among community-dwelling adults: Data from the Osteoarthritis Initiative. Spine. J. 2023, in press. [Google Scholar] [CrossRef]
- Kuş, G.; Yasaci, Z.; Boz, C.; Türkmen, E. Association of Osteoarthritis Prevalence with Age and Obesity Factors in OECD Countries: Panel Regression Model. Am. J. Phys. Med. Rehabil. 2023, 2013, 71. [Google Scholar] [CrossRef]
- Weatherall, J.M.; Mroczek, K.; McLaurin, T.; Ding, B.; Tejwani, N. Post-traumatic ankle arthritis. Bull. Hosp. Jt. Dis. 2013, 71, 104–112. [Google Scholar]
- Mann, R.A.; Rongstad, K.M. Arthrodesis of the ankle: A critical analysis. Foot Ankle. Int. 1998, 19, 3–9. [Google Scholar] [CrossRef]
- Abuhantash, M.; Veljkovic, A.; Wing, K.; Gagne, O.; Qian, H.; Wong, H.; Sadr, H.; Penner, M.; Younger, A. Arthroscopic vs. Open Ankle Arthrodesis: A 5-Year Follow Up. J. Bone Joint Surg. Am. 2022, 104, 1197–1203. [Google Scholar] [CrossRef] [PubMed]
- Shih, C.L.; Chen, S.J.; Huang, P.J. Clinical Outcomes of Total Ankle Arthroplasty vs. Ankle Arthrodesis for the Treatment of End-Stage Ankle Arthritis in the Last Decade: A Systematic Review and Meta-analysis. J. Foot Ankle. Surg. 2020, 59, 1032–1039. [Google Scholar] [CrossRef] [PubMed]
- Park, J.H.; Kim, H.J.; Suh, D.H.; Lee, J.W.; Kim, H.J.; Oh, M.J.; Choi, G.W. Arthroscopic vs. Open Ankle Arthrodesis: A Systematic Review. Arthroscopy. 2018, 34, 988–997. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Xu, C.; Li, M.; Li, H.; Wang, L.; Zhong, D.; Liu, H. Arthroscopic ankle fusion only has a limited advantage over the open operation if osseous operation type is the same: A retrospective comparative study. J. Orthop. Surg. Res. 2020, 15, 80. [Google Scholar] [CrossRef]
- Quayle, J.; Shafafy, R.; Khan, M.A.; Ghosh, K.; Sakellariou, A.; Gougoulias, N. Arthroscopic vs. open ankle arthrodesis. Foot Ankle Surg. 2018, 24, 137–142. [Google Scholar] [CrossRef] [PubMed]
- O’Brien, T.S.; Hart, T.S.; Shereff, M.J.; Stone, J.; Johnson, J. Open vs. arthroscopic ankle arthrodesis: A comparative study. Foot Ankle Int. 1999, 20, 368–374. [Google Scholar] [CrossRef]
- Bai, Z.; Yang, Y.; Chen, S.; Dong, Y.; Cao, X.; Qin, W.; Sun, W. Clinical effectiveness of arthroscopic vs open ankle arthrodesis for advanced ankle arthritis: A systematic review and meta-analysis. Medicine 2021, 100, e24998. [Google Scholar] [CrossRef]
- Mok, T.N.; He, Q.; Panneerselavam, S.; Wang, H.; Hou, H.; Zheng, X.; Pan, J.; Li, J. Open vs. arthroscopic ankle arthrodesis: A systematic review and meta-analysis. Orthop. Surg. Res. 2020, 15, 187. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Ardern, C.L.; Büttner, F.; Andrade, R.; Weir, A.; Ashe, M.C.; Holden, S.; Impellizzeri, F.M.; Delahunt, E.; Dijkstra, H.P.; Mathieson, S.; et al. Implementing the 27 PRISMA 2020 statement items for systematic reviews in the sport and exercise medicine, musculoskeletal rehabilitation and sports science fields: The persist (implementing Prisma in exercise, rehabilitation, sport medicine and sports science) guidance. British journal of sports medicine. Br. J. Sports Med. 2022, 56, 175–195. [Google Scholar]
- Clark, J.M.; Sanders, S.; Carter, M.; Honeyman, D.; Cleo, G.; Auld, Y.; Booth, D.; Condron, P.; Dalais, C.; Bateup, S.; et al. Improving the translation of search strategies using the Polyglot Search Translator: A randomized controlled trial. J. Med. Libr. Assoc. 2020, 108, 195–207. [Google Scholar] [CrossRef] [PubMed]
- Haddaway, N.R.; Grainger, M.J.; Gray, C.T. An R package and Shiny app for forward and backward citations chasing in academic searching. Zenodo 2021, 16. [Google Scholar]
- Higgins, J.P.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J. Cochrane Handbook for Systematic Reviews of Interventions; John Wiley & Sons: Hoboken, NJ, USA, 2019. [Google Scholar]
- Cooper, H.; Hedges, L.V.; Valentine, J.C. The Handbook of Research Synthesis and Meta-Analysis; Russell Sage Foundation: New York, NY, USA, 2019. [Google Scholar]
- IntHout, J.; Ioannidis, J.P.; Rovers, M.M.; Goeman, J.J. Plea for routinely presenting prediction intervals in meta-analysis. BMJ. Open. 2016, 6, e010247. [Google Scholar] [CrossRef] [PubMed]
- Hopkins, W.G. A scale of magnitudes for effect statistics. A new view of statistics. Auckland 2002, 502, 411. [Google Scholar]
- McGuinness, L.A.; Higgins, J.P.T. Risk-of-bias VISualization (robvis): An R package and Shiny web app for visualizing risk-of-bias assessments. Res. Synth. Methods 2021, 12, 55–61. [Google Scholar] [CrossRef]
- Meng, Q.; Yu, T.; Yu, L.; Zhao, X.; Qi, C. Effectiveness comparison between arthroscopic and open ankle arthrodeses. Zhongguo. Xiu. Fu. Chong. Jian. Wai. Ke. Za. Zhi 2013, 27, 288–291. [Google Scholar]
- Morelli, F.; Princi, G.; Cantagalli, M.R.; Rossini, M.; Caperna, L.; Mazza, D.; Ferreti, A. Arthroscopic vs open ankle arthrodesis: A prospective case series with seven years follow-up. World J. Orthop. 2021, 12, 1016–1025. [Google Scholar] [CrossRef]
- Myerson, M.S.; Quill, G. Ankle arthrodesis. A comparison of an arthroscopic and an open method of treatment. Clin. Orthop. Relat. Res. 1991, 268, 84–95. [Google Scholar]
- Nielsen, K.K.; Linde, F.; Jensen, N.C. The outcome of arthroscopic and open surgery ankle arthrodesis: A comparative retrospective study on 107 patients. Foot Ankle Surg. 2008, 14, 153–157. [Google Scholar] [CrossRef]
- Panikkar, K.V.; Taylor, A.; Kamath, S.; Henry, A.P.J. A comparison of open and arthroscopic ankle fusion. Foot Ankle Surg. 2003, 9, 169–172. [Google Scholar] [CrossRef]
- Peterson, K.S.; Lee, M.S.; Buddecke, D.E. Arthroscopic vs. open ankle arthrodesis: A retrospective cost analysis. J. Foot Ankle Surg. 2010, 49, 242–247. [Google Scholar] [CrossRef] [PubMed]
- Shah, A.B.; Davis, W.; Littlefield, Z.L.; Young, S.; Alexander, B.; Andrews, N.A.; Khurana, A.; Cage, B.; Sinha, T.; McGwin, G.; et al. Patient and Surgical Factors Affecting Fusion Rates After Arthroscopic and Open Ankle Fusion: A Review of a High-Risk Cohort. Indian J. Orthop. 2022, 56, 1217–1226. [Google Scholar] [CrossRef] [PubMed]
- Townshend, D.; Di Silvestro, M.; Krause, F.; Penner, M.; Younger, A.; Glazebrook, M.; Wing, K. Arthroscopic vs. open ankle arthrodesis: A multicenter comparative case series. J. Bone Joint Surg. Am. 2013, 95, 98–102. [Google Scholar] [CrossRef] [PubMed]
- Woo, B.J.; Lai, M.C.; Ng, S.; Rikhraj, I.S.; Koo, K. Clinical outcomes comparing arthroscopic vs open ankle arthrodesis. Foot Ankle Surg. 2020, 26, 530–534. [Google Scholar] [CrossRef]
- Lopes, R.; Andrieu, M.; Cordier, G.; Molinier, F.; Benoist, J.; Colin, F.; Thès, A.; Elkaïm, M.; Boniface, O.; Guillo, S.; et al. Arthroscopic treatment of chronic ankle instability: Prospective study of outcomes in 286 patients. Orthop. Traumatol. Surg. Res. 2018, 104, S199–S205. [Google Scholar] [CrossRef]
- Murawski, C.D.; Kennedy, J.G. Anteromedial impingement in the ankle joint: Outcomes following arthroscopy. Am. J. Sport. Med. 2010, 38, 2017–2024. [Google Scholar] [CrossRef]
- DeVries, J.G.; Scharer, B.M.; Romdenne, T.A. Ankle stabilization with arthroscopic versus open with suture tape augmentation techniques. J. Foot Ankle Surg. 2019, 58, 57–61. [Google Scholar] [CrossRef]
- Schmid, T.; Krause, F.; Penner, M.J.; Veljkovic, A.; Younger, A.S.; Wing, K. Effect of preoperative deformity on arthroscopic and open ankle fusion outcomes. Foot Ankle Int. 2017, 38, 1301–1310. [Google Scholar] [CrossRef]
- Xu, C.; Li, M.; Wang, C.; Liu, H. A comparison between arthroscopic and open surgery for treatment outcomes of chronic lateral ankle instability accompanied by osteochondral lesions of the talus. J. Orthop. Surg. Res. 2020, 15, 113. [Google Scholar] [CrossRef]
- Cottom, J.M.; Baker, J.; Plemmons, B.S. Analysis of Two Different Arthroscopic Broström Repair Constructs for Treatment of Chronic Lateral Ankle Instability in 110 Patients: A Retrospective Cohort Study. J. Foot Ankle Surg. Off. Publ. Am. Coll. Foot Ankle Surg. 2018, 57, 31–37. [Google Scholar] [CrossRef]
- Rigby, R.B.; Cottom, J.M. A comparison of the ‘All-Inside’ arthroscopic Broström procedure with the traditional open modified Broström-Gould technique: A review of 62 patients. Foot Ankle Surg. J. Eur. Soc. Foot Ankle Surg. 2019, 25, 31–36. [Google Scholar] [CrossRef] [PubMed]
- Dujela, M.D.; Hyer, C.F. Ankle Arthrodesis: Open Anterior and Arthroscopic Approaches. In Essential Foot and Ankle Surgical Techniques: A Multidisciplinary Approach; Springer: Berlin/Heidelberg, Germany, 2016; pp. 275–290. [Google Scholar]
- Anderson, T.; Maxander, P.; Rydholm, U.; Besjakov, J.; Carlsson, A. Ankle arthrodesis by compression screws in rheumatoid arthritis: Primary nonunion in 9/35 patients. Acta Orthop. 2005, 76, 884–890. [Google Scholar] [CrossRef] [PubMed]
- Holt, E.S.; Hansen, S.T.; Mayo, K.A.; Sangeorzan, B.J. Ankle arthrodesis using internal screw fixation. Clin. Orthop. Relat. Res. 1991, 268, 21–28. [Google Scholar]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).